Abstract
Backgrounds/Aims
Combined hepatocellular carcinoma and cholangiocarcinoma (cHCC-CC) is an uncommon subtype of primary liver cancer that has rarely been reported in detail. This study was performed in order to evaluate the clinicopathological characteristics and prognostic factors of cHCC-CC in single center.
Methods
The clinicopathological features of patients diagnosed and operated with cHCC-CC at Chonbuk National Hospital between July 1998 and July 2007 were retrospectively studied by comparing them with patients with only hepatocellular carcinoma (HCC) who had undergone a hepatic resection during the same period.
Results
Ten out of 152 patients who had undergone a hepatic resection were diagnosed with cHCC-CC and thus included in this study (M : F=8 : 2, median age: 52±11.1 years). According to the parameters of the 7th American Joint Committee on Cancer T staging, there were 76 (50.0%), 44 (28.9%), 9 (5.9%), 18 (11.8%) and 5 (3.3%) patients with T stages 1, 2, 3a, 3b and 4, respectively. The overall survival period was longer in the HCC only group (68±40.4 months) than in the combined cHCC-CC group (23±40.1 months) (p<0.0001). The 5-year survival rate was 10% in the cHCC-CC group and 60% in the HCC group (p<0.0001). The disease free survival for patients with cHCC-HCC and HCC were 16±37.4 and 51±44.3 months, respectively (p<0.0001). Univariate analysis revealed that age, gender, transarterial chemoembolization (TACE), and T stage were statistically significant in terms of patient's overall survival. However, there were no significant clinicopathological factors identified by the multivariate analysis.
Conclusions
Even after the hepatic resection in the HCC, the prognosis is poorer if the patient has cholangiocellular components compared to the usual HCC.
Keywords: Combined hepatocellular cholangiocarcinoma, Survival rate, Prognostic factors
INTRODUCTION
Combined hepatocellular carcinoma and cholangiocarcinoma (cHCC-CC) is a rare subtype of liver cancer displaying components of both hepatocellular and cholangiocellular carcinoma. The World Health Organization (WHO) classification defines combined HCC-CC, classical type as a tumor containing unequivocal elements of both hepatocellular carcinoma (HCC) and cholangiocarcinoma (CC), which are intimately admixed; this tumor should be distinguished from separate HCC and CC arising in the same liver.1
Primary liver cancer is a major worldwide health problem. Most primary cancers of the liver are classified into two major types: hepatocellular carcinoma (HCC), which originates in the hepatocytes, and cholangiocarcinoma (CC), which originates from the epithelial cells in the bile duct. Many reports have examined the clinical features, survival outcomes or prognostic factors of cHCC-CC.2-4 To define the clinicopathologic features and clinical out-comes more fully, we compared patients with combined tumors to those with pure HCC.
METHODS
Patients
A total of 152 patients with primary liver cancer, except CC, underwent hepatic resection between July 1, 1998 and July 31, 2007 at Chonbuk National University Hospital.
They were comprised of 10 patients with a histopathologic diagnosis of combined tumor (cHCC-CC group) and 142 patients with HCC (HCC group).
Methods
A retrospective review of a database provided information on the total number of patients. The variables that were used to evaluate our series included the following: clinical variables of age, sex, laboratory data, alpha-fetoprotein (AFP), Hepatitis B (HBV) and hepatitis C (HCV) viral markers, which included the HBV surface antigen, operative type and pre or postoperative transarterial chemoembolization (TACE).
Pathologically, all tumors were staged based on T staging of the AJCC (American Joint Committee on Cancer) 7th edition staging system.
Statistical analysis
Student's t-tests and χ2-tests were used for statistical analysis. To identify predictors of survival, a univariate analysis was performed using the Kaplan-Meier method and compared with the log-lank test. A multivariate analysis was performed using the Cox regression hazards model in order to identify the independent prognostic factors. All statistical analyses were made using SPSS 18.0 for Windows (SPSS Inc. Chicago, III). A p-value less than 0.05 was considered as statistically significant.
RESULTS
Clinicopathological characteristics
In the HCC (n=142) group, the median age was 55 years (22-75); there were 120 men (84.5%) and 22 women (15.5%) (p=0.003). The prevalence of the hepatitis B surface antigen was found in 58 (40.8%) patients; positive serology for hepatitis C infection was found in 5 (3.5%) patients. Alcoholic liver cirrhosis was found in 10 (7%) patients. The hepatitis B surface antigen with alcoholic liver cirrhosis was found in 1 (0.7%) patient (Table 1).
Table 1.
Clinicopathological characteristics of patients with HCC and cHCC-CC

HBV, hepatitis B virus; HCV, hepatitis C virus; AST, aspartate aminotransferase; ALT, alanine aminotransferase; AFP, alpha-fetoprotein; TACE, transarterial chemoembolization
The median level of AFP was 2,997 ng/ml (1.6-875,000). In terms of the operative method, segmentectomy was performed in 70 (49.3%) patients. Wedge resection, hemihepatectomy, mass enucleation and liver transplantation were performed in 44 (31%), 16 (11.3%), 10 (7%), and 2 (1.4%) patients, respectively. Pre- and post-operative TACE were performed in 1 (0.7%) and 89 (62.7%) patients, respectively. There were 74 (52.1%), 41 (28.9%), 8 (5.6%), 15 (10.6%) and 4 (2.8%) patients with T stages 1, 2, 3a, 3b and 4, respectively.
In the cHCC-CC (n=10) group, the median age was 52 years (39-70); there were 8 men (80%) and 2 women (20%). The prevalence of the hepatitis B surface antigen was 8 (80%).
The median level of AFP was 9,361 ng/ml (5.4-75680). Postoperative TACE was conducted in 3 (30%) patients. There were 2 (20.0%), 3 (30.0%), 1 (10%), 3(30%) and 1 (10%) patients with T stages 1, 2, 3a, 3b and 4, respectively.
There was no significant difference between the HCC and cHCC-CC group based on the clinicopathological factors.
Overall and disease-free survival rate of patients with HCC and cHCC-CC
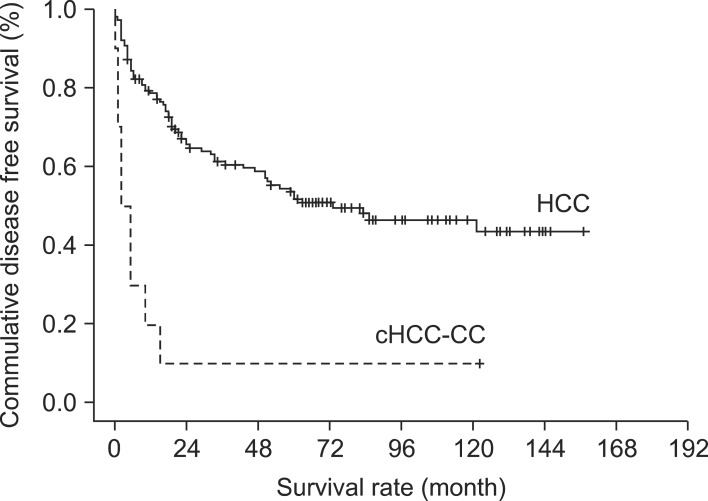
The 1-year overall survival rate was 82%, the 3-year overall survival rate was 73%, and the 5-year overall survival rate was 60% in the HCC group. On the other hand, the cHCC-CC group showed that the 1-year overall survival rate was 20%, the 3-year overall survival rate was 20%, and the 5-year overall survival rate was 10% (p=0.000). Median survival periods in the HCC and cHCC-CC groups were 68±40.4 and 23±40.1 months, respectively (Fig. 1).
Fig. 1.
Overall survival of patients with HCC and cHCC-CC. The overall survival of the cHCC-CC group was lower than the HCC group (p<0.0001). 1-year, 3-year and 5-year survival rates in the HCC group were 82%, 73% and 60%, respectively. On the other hand, the cHCC-CC group showed downward results with 1-year, 3-year and 5-year survival rates at 20%, 20% and 10%, respectively. (p<0.000) Mean survival period in the HCC and cHCC-CC groups were 68±40.4 and 23±40.1 months, respectively.
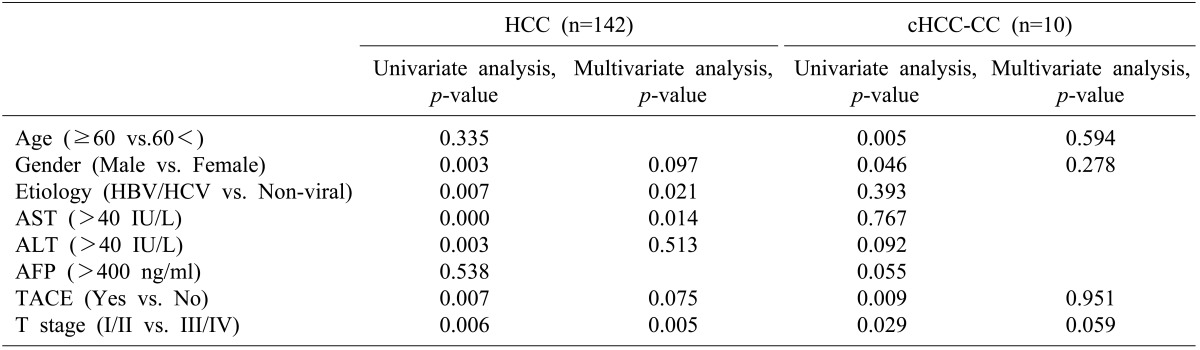
In the HCC group, the 1-year disease free survival rate was 67%, the 3-year disease free survival rate was 59%, and the 5-year disease free survival rate was 50%. On the other hand, the cHCC-CC group indicated that the 1-year disease free survival rate was 10%, the 3-year disease free survival rate was 10%, and the 5-year disease free survival rate was 10% (p<0.0001).
Except for 1 case in which the patient survived for 122 months at the T1 stage, most patients in the cHCC-CC group died or experienced recurrence within 1 year (Fig. 2). According to the overall survival rate, significant prognostic factors in the cHCC-CC group were age (p=0.005), sex (p=0.046), TACE (p=0.009) and T stage (p=0.029) in the univariate analysis, but not in the multivariate analysis (Table 2).
Fig. 2.
Disease free survival of patients with HCC and cHCC-CC. The disease free survival of the cHCC-CC group was lower than the HCC group (p<0.0001). 1-year, 3-year and 5-year disease free survival rates in the HCC group were 67%, 59% and 50%, respectively. On the other hand, the cHCC-CC group showed 1-year, 3-year and 5-year survival rates of 10%, 10% and 10%, respectively (p<0.0001).
Table 2.
Prognostic factors of overall survival in HCC and cHCC-CC
AST, aspartate aminotransferase; ALT, alanine aminotransferase; AFP, alpha-fetoprotein,; TACE, transarterial chemoembolization; HBV, hepatitis B virus; HCV, hepatitis C virus
According to the disease free survival rate, significant prognostic factors in the cHCC-CC group were age (p=0.006), sex (p=0.046), preoperative alanine transaminase (ALT) (p=0.03) and T stage (p=0.005) in the univariate analysis, but not in the multivariate analysis (Table 3).
Table 3.
Prognostic factors of disease free survival in HCC and cHCC-CC
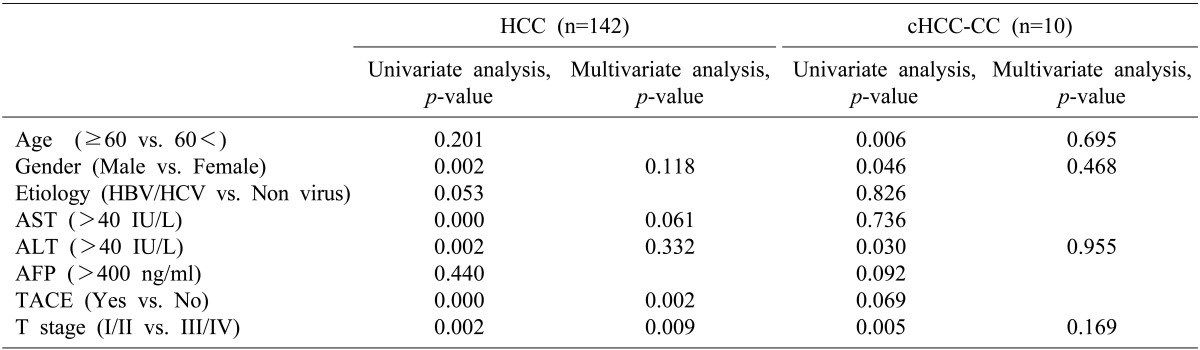
AST, aspartate aminotransferase; ALT, alanine aminotransferase; AFP, alpha-fetoprotein; TACE, transarterial chemoembolization; HBV, hepatitis B virus; HCV, hepatitis C virus
DISCUSSION
cHCC-CC is an uncommon liver malignancy with distinctive features compared with HCC and CC in respect to its clinicopathologic changes and prognosis. The incidence of cHCC-CC varies widely, from a rate of 2.4% to 14.2%.2 In our study, the incidence of cHCC-CC was 6.6%. Generally, the clinicopathological features of cHCC-CC were similar to those of HCC.5,8
Most cHCC-CC patients in our series were men with a high prevalence of HBV, suggesting that HBV infection is a main cause for both HCC and cHCC-CC in Asia. According to AFP, the elevation of AFP was found in both groups. Some authors reported that high elevation of the AFP level (≥400 IU/L) was an independent prognostic factor in cHCC-CC.5,7 On the other hand, Jarnagin et al. reported that the level of AFP in cHCC-CC was lower than that in HCC, but had no significant difference.10 In our study, there was no significant difference in the AFP levels as well as in the statistical relationship with a survival rate between the HCC-CC group and the HCC group.
The number of tumor and UICC stage in cHCC-CC were predictive factors of the overall survival rate.2 Our study demonstrated that the T stage was related to a significant difference in the survival rate in the univariate analysis, but not in multivariate analysis.
cHCC-CC patients had poorer prognosis compared to HCC patients, and CC had a relatively unfavorable prognosis compared with cHCC-CC and HCC.5,9 In our study, the cHCC-CC group had significantly poorer prognosis than the HCC patients. Okuda12 reported that patient prognosis with cHCC-CC was poorer than that of HCC because lymph node metastasis occurred more frequently. In our study, the disease free survival rate was 16 months and T stage was a significant prognostic factor.
TACE is indicated for patients with non-resectable or recurrent HCC for palliative purposes because it has been proved to increase the survival of these patients. However, the therapeutic effect of TACE for cHCC-CCs remains unclear. Compared with HCC, many cHCC-CCs are less vascular than HCC and thus, may poorly respond to TACE. Other reports showed that patients in advancedstage disease cases who had received TACE treatment had a significantly longer 6-month survival than patients who received supportive treatment.8,13,14
Our 3 patients who underwent TACE showed a significant improvement in the survival rate. Some studies reported radiation treatment attempts to patients with non-resectable or local recurrent tumor for a better survival rate.15
There are some limitations in our study. First, this study was retrospective and could have been affected by any and all of the limitations of this investigational design.
Second, both HCC and cHCC-CC were compared without CC.
In conclusion, most reports have indicated that surgical intervention was an effective treatment for cHCC-CC. However, patients with cHCC-CC have a significantly poorer survival outcome after hepatic resection than do patients with HCC. Further studies on effective treatment modalities and clinical predictors for cHCC-CC are required in order to prolong the survival of these patients.
References
- 1.Theise ND, Nakashima O, Park YN, Nakanuma Y. Combined hepatocellular-cholangiocarcinoma. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon, France: IARC; 2010. pp. 225–227. [Google Scholar]
- 2.Koh KC, Lee H, Choi MS, et al. Clinicopathologic features and prognosis of combined hepatocellular cholangiocarcinoma. Am J Surg. 2005;189:120–125. doi: 10.1016/j.amjsurg.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 3.Goodman ZD, Ishak KG, Langloss JM, et al. Combined hepatocellular-cholangiocarcinoma. A histologic and immunohistochemical study. Cancer. 1985;55:124–135. doi: 10.1002/1097-0142(19850101)55:1<124::aid-cncr2820550120>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 4.Kim DK, Lee SM, Hong SW. Combined hepatocellular-cholangiocarcinoma. Korean J Hepatobiliary Pancreat Surg. 1998;2:171–176. [Google Scholar]
- 5.Yano Y, Yamamoto J, Kosuge T, et al. Combined hepatocellular and cholangiocarcinoma: a clinicopathologic study of 26 resected cases. Jpn J Clin Oncol. 2003;33:283–287. doi: 10.1093/jjco/hyg056. [DOI] [PubMed] [Google Scholar]
- 6.Liu CL, Fan ST, Lo CM, et al. Hepatic resection for combined hepatocellular and cholangiocarcinoma. Arch Surg. 2003;138:86–90. [PubMed] [Google Scholar]
- 7.Park HS, Bae JS, Jang KY, et al. Clinicopathologic study on combined hepatocellular carcinoma and cholangiocarcinoma: with emphasis on the intermediate cell morphology. J Korean Med Sci. 2011;26:1023–1030. doi: 10.3346/jkms.2011.26.8.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yin X, Zhang BH, Qiu SJ, et al. Combined hepatocellular carcinoma and cholangiocarcinoma: clinical features, treatment modalities, and prognosis. Ann Surg Oncol. 2012;19:2869–2876. doi: 10.1245/s10434-012-2328-0. [DOI] [PubMed] [Google Scholar]
- 9.Maeda T, Adachi E, Kajiyama K, et al. Combined hepatocellular and cholangiocarcinoma: proposed criteria according to cytokeratin expression and analysis of clinicopathologic features. Hum Pathol. 1995;26:956–964. doi: 10.1016/0046-8177(95)90084-5. [DOI] [PubMed] [Google Scholar]
- 10.Jarnagin WR, Weber S, Tickoo SK, et al. Combined hepatocellular and cholangiocarcinoma: demographic, clinical, and prognostic factors. Cancer. 2002;94:2040–2046. doi: 10.1002/cncr.10392. [DOI] [PubMed] [Google Scholar]
- 11.Park H, Choi KH, Choi SB, et al. Clinicopathological characteristics in combined hepatocellular-cholangiocarcinoma: a single center study in Korea. Yonsei Med J. 2011;52:753–760. doi: 10.3349/ymj.2011.52.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okuda K. Natural history of hepatocellular carcinoma including fibrolamellar and hepato-cholangiocarcinoma variants. J Gastroenterol Hepatol. 2002;17:401–405. doi: 10.1046/j.1440-1746.2002.02734.x. [DOI] [PubMed] [Google Scholar]
- 13.Poon RT, Ngan H, Lo CM, et al. Transarterial chemoembolization for inoperable hepatocellular carcinoma and postresection intrahepatic recurrence. J Surg Oncol. 2000;73:109–114. doi: 10.1002/(sici)1096-9098(200002)73:2<109::aid-jso10>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 14.Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 15.Ibarra RA, Rojas D, Snyder L, et al. Multicenter results of stereotactic body radiotherapy (SBRT) for non-resectable primary liver tumors. Acta Oncol. 2012;51:575–583. doi: 10.3109/0284186X.2011.652736. [DOI] [PubMed] [Google Scholar]