Abstract
Background
An increasing number of clinics offer complementary or integrative medicine services; however, clear guidance about how complementary medicine could be successfully and efficiently integrated into conventional health care settings is still lacking. Combining conventional and complementary medicine into integrative medicine can be regarded as a kind of merger. In a merger, two or more organizations − usually companies − are combined into one in order to strengthen the companies financially and strategically. The corporate culture of both merger partners has an important influence on the integration.
Purpose
The aim of this project was to transfer the concept of corporate culture in mergers to the merging of two medical systems.
Methods
A two-step approach (literature analyses and expert consensus procedure) was used to develop practical guidance for the development of a cultural basis for integrative medicine, based on the framework of corporate culture in “mergers,” which could be used to build an integrative medicine department or integrative medicine service.
Results
Results include recommendations for general strategic dimensions (definition of the medical model, motivation for integration, clarification of the available resources, development of the integration team, and development of a communication strategy), and recommendations to overcome cultural differences (the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine).
Conclusion
The framework of mergers in corporate culture provides an understanding of the difficulties involved in integrative medicine projects. The specific recommendations provide a good basis for more efficient implementation.
Keywords: integrative medicine, mergers, corporate culture
Introduction
In Germany and the US, complementary medicine is increasingly provided by conventional medical institutions.1–6 Furthermore, new terms – particularly the term “integrative medicine”7,8 – have been introduced to capture the increasing implementation of complementary medicine into conventional medicine (mainstream medicine).
Complementary medicine is an umbrella term, which represents a heterogeneous field with disparate beliefs and practices that can vary considerably.9,10 According to the National Institutes of Health in the US, “complementary” generally refers to using a non-mainstream approach together with conventional medicine.11
To date, few theoretical models and frameworks for describing and evaluating complementary medicine services have been published12,13 and clear guidance about how complementary medicine could be successfully and efficiently integrated into conventional health care settings is lacking. This so-called “integrative medicine” has been defined by the Consortium of Academic Health Centers for integrative medicine in the US as
[…] the practice of medicine that reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic approaches, health care professionals, and disciplines to achieve optimal health and healing.14
A previous semi-structured interview study with leading experts of academic integrative medicine was performed. In addition to recommendations that include creating common goals, networking, and establishing well-functioning research teams,15 the interviewees made it clear that for the successful development of integrative medicine, familiarity with the different cultures of conventional and complementary medicine plays an important role.
Combining conventional and complementary medicine into integrative medicine can be regarded as a kind of merger. In a merger, two or more organizations − usually companies − are combined into one in order to strengthen the companies financially and strategically. Merging organizations have the opportunity to adapt quickly to new or changing markets by fostering a more rapid transformation of the organization that will not occur with either organization alone.16
The careful selection of the merger partners is extremely important for success. Not only must the acquirer consider the likelihood of success of combining financial and strategic aspects of both companies, it must also consider the likelihood of success of combining the corporate cultures.17 It is well known that a failure to negotiate the cultural differences between the merger partners can contribute to merger failure.17,18
The corporate culture of an organization may be expressed as “the way we do things around here,” and this sentiment includes values, beliefs, attitudes, assumptions, norms, mission statements, aims, personal interests, behaviors, and management styles. In general, two merging organizations may not necessarily have the same corporate culture, but they should be able to act together.17 In practice, several cultures (ie, microcultures) often coexist within one organization. According to Sherwin,19 medical schools and teaching hospitals are under pressure to change from academic institutions to corporate organizations. In the hospital environment today, different departments often start to develop their own operational norms. These are influenced by multiple factors, including medical specialization, country, type of hospital, leadership, and employees. In general, many problems in cooperation, communication, teamwork, and acceptance of treatments can be attributed to cultural differences. In corporate mergers, organizations that once offered mutually exclusive and competitive products and services in the marketplace face challenges to become uniform and integrated.
Transferring the theoretical frameworks that have been developed for merging organizations to the two distinctive medical approaches of conventional medicine and complementary medicine might be helpful for a better understanding and further development of integrative medicine. The underlying aim for a corporate merger is to arrive at positive synergy, meaning that the final outcome of the merged system is greater than the sum of its constituent parts. Similarly, integrative medicine wants to reach synergistic therapeutic effects that lead to a better treatment outcome for patients by combining conventional and complementary medicine.8
The impact of the merger on the corporate culture of both organizations is strongly influenced by the employed integration type. According to Kummer,20 different degrees of integration are possible during a merger. Developing an integrative medicine referral service would be characterized as a “linking” type of integration, which allows conventional and complementary medicine to work together while maintaining their respective and independent identities; in this case, at least a mutual understanding of both cultures is needed. The creation of a new department for integrative medicine with a joint team of conventional and complementary medicine professionals would be called “the best of both worlds” integration type; here, the development of a new corporate culture is necessary.
The aim of this project was to develop practical guidance for the development of a cultural basis for integrative medicine. This guidance is based on the framework of corporate culture in “mergers” and could be used to build an integrative medicine department or integrative medicine service.
Methods
A two-step approach, including a literature analysis and expert consensus procedure, was used. The preparation of the symposium was based on a literature analysis and brief narrative telephone interviews with merger experts as well as with professionals working in integrative medicine. Relevant information on merger theory and corporate culture, as well as information on corporate culture aspects of both conventional and complementary medicine, were summarized in a written document and synthesized into a presentation for the workshop. Furthermore, integrative oncology, a growing field within integrative medicine, was identified as a good example. Workshop participants from Germany and the US were identified and invited to participate in a 2-day interdisciplinary consensus symposium. The symposium took place at the Robert Bosch Foundation in Stuttgart, Germany on October 22–23, 2012.14 The 14 participants came from different backgrounds and included two leading experts on corporate culture in mergers, a hospital manager with experience in establishing an integrative medicine department in Germany, a nurse who established one of the leading integrative medicine programs in the US, four chief medical doctors from integrative medicine departments (one from Germany; three from the US), four researchers with experience in integrative medicine research from a variety of backgrounds (business, history of medicine, medical anthropology, and epidemiology), and two representatives of the supporting foundations (Robert Bosch Stiftung and The Institute for Integrative Health). The workshop included introductory lectures on mergers and corporate culture and case studies from integrative oncology, which were complemented by breakout sessions in which two interdisciplinary groups with seven participants each worked in parallel discussing the same topics over the course of 2 days. These topics included reasons for building an integrative medicine department or integrative medicine service, identifying the most relevant aspects of cultural differences between conventional and complementary medicine, and developing practical recommendations to guide the development of an integrative medicine department or integrative medicine service.
Results from the two working groups were presented in a plenary session and synthesized through a consensus discussion. In addition to written Delphi rounds, all workshop participants and those who were not able to join the workshop were asked to comment on the manuscript until final consensus was reached after the third round.
Three additional experts (one patient advocate, one chief medical doctor, and the principal investigator of a large collaborative research project on integrative oncology) – who were invited, but unable to participate in the workshop – joined the post-symposium Delphi process.
Results
From the symposium and Delphi process, some general comments and insights were derived. When building an integrative medicine department or offering an integrative medicine service, the primary aim was viewed as the achievement of positive synergy between conventional and complementary medicine and the improvement of hospital outcomes, including health care. Positive synergy was viewed as the integration of the two approaches to medicine (conventional and complementary) leading to better patient outcomes as well as to better clinic outcomes (eg, patient numbers, revenue) than either approach could achieve alone. Because several definitions exist for the terms complementary medicine and integrative medicine, it was decided that the term “integrative medicine” would be used to denote a combination of conventional medicine and complementary medicine that creates positive synergy. Providers play an important role and cultural differences between conventional health care providers and complementary medicine providers were discussed during the symposium as a threat resulting in a possible cultural clash. This would have a negative impact on synergy as well as on each provider group itself. This impact may include conflict, low morale, low productivity, poorer quality care, and turnover among key individuals and groups.21
It became clear that in each hospital or department a mosaic of different perspectives generally exists (eg, medical doctors, nurses, administration, pharmacists) and that both conventional medicine and complementary medicine have many microcultures depending on their respective specialties or modalities. However, although both are heterogeneous on the microculture level, it was assumed that each has an overall macroculture. On a macro level, conventional medicine appeared to have a more uniform and sharply delineated culture with clear norms and values, whereas the macroculture of complementary medicine seemed to be more heterogeneous and strongly influenced by the different treatment modality philosophies (eg, Chinese medicine). Although conventional medicine also includes a broad variety of disciplines with heterogeneous microcultures, these were commonly seen to be highly respected in society and share a similar scientific basis, whereas complementary medicine was viewed as less respected and less scientific. Furthermore, different financial models for conventional and complementary medicine in health care were discussed, which vary between countries and states. Third party coverage is more common for conventional medicine overall, whereas complementary medicine is more often based on fee-for-service models or philanthropic support.
It became clear that providers of complementary medicine vary depending on the country in which complementary medicine is delivered, as well as national and local regulation. In Germany, for example, complementary medicine is more often provided by conventional medical doctors,22 whereas in the US, it is mainly provided by non-medical doctors. Some of the recommendations below, for example, using a common language and terminology, are more relevant when conventional medical doctors and non-medical doctor complementary medicine practitioners work together.
During the discussion it became obvious that when integrating conventional and complementary medical providers, it is very likely that more than two cultures will be brought together, potentially exacerbating the challenges discussed above.
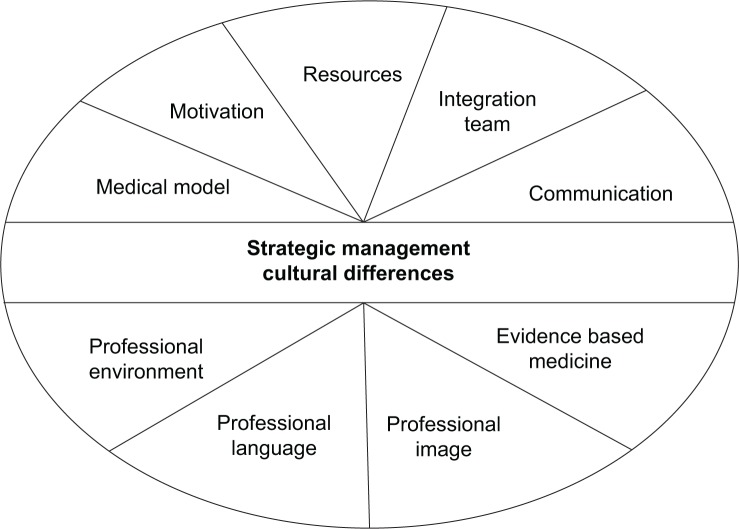
The following recommendations were developed for practical guidance to support the development of a cultural basis for integrative medicine, which could be used to build an integrative medicine department. They are divided into recommendations for general integration management and recommendations for dealing with cultural differences (Figure 1).
Figure 1.
Recommendation areas for general integration management and for dealing with cultural differences.
Recommendations for general integration management
The recommendations center on five general strategic dimensions of integration management. These include the definition of the medical model, motivation for integration, clarification of the available resources, development of the integration team, and development of a communication strategy.
Definition of the medical model
It is important to choose a medical model that suits the needs of patients, the clinic, and its other relevant stakeholders. The medical model includes the type of integration (eg, integrative medicine department which needs the development of a new shared culture or an integrative medicine referral service where a mutual understanding of both cultures is needed); the complementary medicine modalities to be offered, with attention to their safety and credibility (eg, starting with the more known and accepted modalities); and the degree of specialization (eg, How much specialization is reasonable and necessary to be competent and effective without losing the patient-centered and holistic approach?). The benefit to the patient should play a key role when defining the medical model.
Motivation for integration
The motivation of the administration and the providers from both sides (complementary and conventional medicine) should be succinct, explicit, and transparent for the integration and subsequent collaboration when treating patients. Both intrinsic (eg, seeing the benefit of integration for the patient) and extrinsic (eg, financial incentives) motivators should be communicated and accepted by all parties involved.
Clarification of available resources
The available resources should be defined and reasonable, including space, staff, training, and consumables, as well as time and incentives for those involved in the planning and implementation.
Building the integration team
The team should consist of visible “champions,” with interpersonal, social, and emotional skills, who can act as door openers or liaisons between administrators and practitioners from both medical approaches. However, to support sustainability, it is important not to depend on a single person. The “champions” should understand the aims, share the overall vision, and be able to work together as a team. This teamwork requires building mutual respect and belief in the validity of both approaches to medicine. The team ideally includes: 1) a conventional medical doctor in a leadership position who is highly respected in the clinic, has political savvy, and is able to compromise; 2) an administrator who is in a leading position; 3) a complementary medicine practitioner who is respected in his/her field, with good leadership and clinical skills, and who has high visibility, and brings value to the organization beyond complementary medicine; and 4) a nurse who is visible and highly respected to encourage bridging between complementary and conventional medicine as well as bridging to patients.
Communication strategy
The concept of the integrative medicine department or referral service should be over-communicated. This communication should emphasize the project’s aims, as well as describing exactly what integrative medicine services are anticipated. Strategies should be developed to increase the knowledge and understanding of integrative medicine (eg, joint events in which physicians and practitioners might socialize and bond such as conferences and trainings). Furthermore, the impact of the new service/department on the different stakeholders should be clearly communicated.23,24
Recommendations for overcoming cultural differences
Four cultural differences have been identified that could lead to a clash of cultures when developing and implementing an integrative medicine department or referral service: the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine. For each, the cultural difference, potential implications, and recommendations to mitigate cultural differences are outlined in Table 1.
Table 1.
Identified cultural differences that could lead to a clash of cultures when developing and implementing an integrative medicine department or referral service
| Cultural differences | Possible consequences of cultural differences | Recommendations to mitigate cultural differences | |
|---|---|---|---|
| The integrative medicine environment (inpatient or outpatient clinic usually as part of a hospital) | A complementary medicine practitioner is most commonly an entrepreneur working in his/her own business, and will have to adapt to a new role in the clinic as an employee who works as part of a team. Most complementary medicine practitioners are unfamiliar with the structures, the type of patients, and working in interdisciplinary teams typical of conventional medicine. Conventional health care providers (eg, medical doctors and nurses) have been trained to work within this environment. | Cultural differences influence the attitudes, communications, and working style within the professional team, as well as patient care (eg, patient–practitioner interaction and communication). Differences can have a negative impact on outcomes, especially on patient satisfaction and provider productivity. | a) In general, team and meeting structures in conventional medicine are already changing to take into account the need for multidisciplinary teams. Complementary medicine could be viewed as one discipline within such a team. It is important to enforce less hierarchical structures, but to have clearly defined roles and responsibilities in the teams. Furthermore, the responsibility for the medical diagnosis – including legal liability – has to be clarified within the team. b) Complementary medicine practitioners have an entrepreneurial background and might have a fresh perspective on the given structures. In terms of continuous improvement, the administration should be open to their innovative ideas (eg, employee idea system). c) Training and education should be provided for complementary medicine practitioners in these areas: 1) team development/exposure training (including materials, group exercises and team building, and conflict resolution pathways), 2) special training in organizational structure (eg, reporting guidelines, record keeping, safety), and 3) education in the medical specialty (eg, breast cancer) and typical safety aspects. |
| Professional image (part of the personality and includes aspects such as appearance, behavior, habits, and communication style) | The professional image of many complementary medicine practitioners can differ from that of conventional health professionals. The institutions that provide the relevant training, the peers, and the underlying treatment philosophies have an influence on respective professional images. | Cultural difference influences attitudes and communication in the professional team, as well as attitudes toward and communication with the patient. It especially affects corporate philosophy, because complementary medicine practitioners often don’t fit the corporate identity of a conventional medicine organization. | a) For the complementary medicine practitioners, the “social norm” in the integrative medicine institution must be clearly defined. Aspects such as having a clear strategy for complementary medicine providers’ visibility as a marketing tool might be taken into account. b) In the staff selection process, considering both clinical skills and professional image will be useful. As noted earlier, complementary medicine includes practitioners with many different modalities (eg, acupuncture, massage therapy) with a wide variety of cultural variances among them as well. The within-modality differences should be considered as much as the differences between complementary and conventional medicine. |
| Professional language (a profession is identified in part by its use of a shared – but often specialized – language) | For all conventional health care professionals, a shared basic medical language exists, and it is more detailed in the different specialties. By contrast, the professional language of complementary medicine practitioners is very heterogeneous across the different modalities. Language is also influenced by the different modalities’ respective philosophical groundings. | Different professional languages are problematic for communication with patients and for communication within the professional team. Misunderstandings affect the quality of care and may result in reduced patient safety and patient satisfaction, and can have a negative effect on job satisfaction and productivity. | a) Short-term recommendations include: 1) training of complementary medicine practitioners in the basic medical language, and the provision of details needed for the specialty in which they work, 2) the development of a clear and comprehensive safety triage system, which could also be applied by complementary medicine practitioners (eg, when a cancer patient gets a new headache, imaging would be needed to check for brain tumor), 3) training of conventional health professionals in the basics of the applied complementary medicine methods for a better understanding for appropriate referrals, and 4) increasing respect and mutual understanding in an overall multidisciplinary team structure by avoiding abbreviations and explaining special terms. b) Long-term recommendations include: 1) the inclusion of basic conventional medicine medical terminology |
| Implementation of EBM (is a conscientious use of current best evidence in making decisions about the care of individual patients or the delivery of health services22) | Currently, EBM is much more established in conventional medicine than in complementary medicine. | Misunderstandings about EBM have a critical influence on the communication within the professional team, and can reduce productivity and job satisfaction. Because EBM has an influence on strategy, its relevance and the acceptable EBM level should be defined as part of the medical model. | a) Short-term recommendations include: 1) empowering complementary medicine practitioners in research literacy with trainings that focus on their treatment modalities including literature search, critical appraisal, the relevance of EBM, a better understanding for clinically meaningful effects in studies, and the relevance and potential of context effects in overall medicine for patient outcomes, 2) educating both conventional health care professionals and complementary medicine practitioners to understand EBM as evidence that includes three pillars (practitioners’ experience, norms and values of the patient, and evidence from clinical research), that evidence can exist on different levels, and that they should be familiar with the available evidence of both conventional and complementary medicine interventions in their field. b) The long-term recommendations include more research literacy in the complementary medicine training of conventional medicine practitioners. |
Abbreviation: EBM, evidence-based medicine.
Discussion
The framework of corporate culture in mergers provides perspectives that allow for an understanding of the difficulties involved in integrative medicine projects. Five key actions have been identified as important in the strategy for development of an integrative medicine department or referral service: definition of the medical model, clarification of the motivation for integration, clarification of available resources, development of the integration team, and development of a communication strategy. Four cultural differences that are relevant for integrative medicine were able to be identified: the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine. Furthermore, recommendations to mitigate these cultural differences were provided.
The recommendations were based on a literature analysis and systematic multidisciplinary expert experience. One limitation is that in the symposium participants represented only two countries, Germany and the US. These countries were selected because both had strong development in the field of integrative medicine within medical schools and teaching hospitals in recent years, but have very different health care systems. The recommendations might have differed had experts from other countries such as China or India participated, where the culture of traditional medicine has long been the predominant medical approach and is still widely available. One further limitation is that patients’ barriers to integrative medicine were not discussed. However, it was recommended that it is important to choose a medical model that suits the needs of patients, and to make this possible, patients should be fully integrated into the development process of the integrative medicine department or integrative medicine service.
Furthermore, integrative medicine is a broad and heterogeneous field and the recommendations provided here should be viewed as general guidance. When putting these recommendations into practice, it will be necessary to take many details of the actual context into account. The structure of the health care system and reimbursement guidelines will have an especially strong influence on the choice of the medical model. In the US and Germany, the reimbursement of integrative medicine could be various based on the policy. Due to this, not all integrative medicine services will be economically self-sustainable. It is important to allow enough time and resources for the strategic planning phase of the proposed integrative medicine department. Sometimes the best decision may be to not pursue implementation of the integrative medicine department project, because it will be neither accepted nor sustainable. The integration project might even lose money and reduce the productivity of the organization as a whole. It is noteworthy to mention that the integration of complementary and alternative medicine into a mainstream hospital is only possible if the hospital is financially viable.
A new integrative medicine department that is based on the integration type “best of both worlds” needs the development of a “new,” shared culture,20 a process that can be resource intensive. For a successful and efficient integrative medicine referral service that is based on the integration type of “linking,” corporate culture also plays an important role, but the focus might be better directed toward developing mutual respect and an understanding of cultural differences than at the development of a completely “new” culture. Such mutual respect and understanding would be based not only on a shared professional language, but also on an appropriate orientation to and familiarity with the professional environment. Moreover, sensitivity to incentive systems is critical, especially in environments where complementary medicine and conventional medicine may not be viewed or valued the same. Without these, patient safety and productivity might be negatively affected. Overall, the integration might be less resource intensive and easier in Germany than in the US, because in Germany complementary medicine is often provided by conventionally trained medical doctors who know the conventional environment and speak the professional language. However, independent of their professional backgrounds, the “champions” from the complementary medicine field need strong leadership skills and the ability to work in a team in addition to their clinical skills. Currently, in both Germany and the US, there is a shortage of complementary medicine practitioners with extensive skills and experience in leading multidisciplinary teams. Leadership in integrative medicine is an area that needs development, and should include clear definitions of the necessary competencies, motivation incentives, and training in leadership competencies.
Acknowledgments
The authors thank Iris Bartsch and Hildegard Micko for their assistance in organizing the symposium.
The symposium was funded by the Robert Bosch Stiftung. Marion Pérard received a scholarship from The Institute for Integrative Health. Claudia Witt’s work, in her role as Chair of Complementary Medicine Research, was funded by the Carstens Foundation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Horrigan B, Lewis S, Abrams D, Pechura C. Integrative Medicine in America: How Integrative Medicine is Being Practiced in Clinical Centers Across the United States. Minneapolis, MN: The Bravewell Collaborative; 2012. [Accessed August 27, 2014]. Available from: http://www.bravewell.org/content/Downlaods/IMinAm.pdf. [Google Scholar]
- 2.Maizes V, Rakel D, Niemiec C. Integrative medicine and patient-centered care. Explore (NY) 2009;5(5):277–289. doi: 10.1016/j.explore.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Ruggie M. Mainstreaming complementary therapies: new directions in health care. Health Aff (Millwood) 2005;24(4):980–990. doi: 10.1377/hlthaff.24.4.980. [DOI] [PubMed] [Google Scholar]
- 4.Dobos GJ, Voiss P, Schwidde I, et al. Integrative oncology for breast cancer patients: introduction of an expert-based model. BMC Cancer. 2012;12:539. doi: 10.1186/1471-2407-12-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knutson L, Johnson PJ, Sidebottom A, Fyfe-Johnson A. Development of a hospital-based integrative healthcare program. J Nurs Adm. 2013;43(2):101–107. doi: 10.1097/NNA.0b013e31827f2229. [DOI] [PubMed] [Google Scholar]
- 6.Lauche R, Cramer H, Moebus S, et al. Results of a 2-week inpatient stay at the department for internal and integrative medicine: an observational study. Evid Based Complement Alternat Med. 2012;2012:875874. doi: 10.1155/2012/875874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmberg C, Brinkhaus B, Witt C. Experts’ opinions on terminology for complementary and integrative medicine – a qualitative study with leading experts. BMC Complement Altern Med. 2012;12:218. doi: 10.1186/1472-6882-12-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dobos G. Integrative medicine – medicine of the future or “old wine in new skins”? Eur J Integr Med. 2009;1(3):109–115. [Google Scholar]
- 9.Gevitz N. Alternative medicine and the orthodox canon. Mt Sinai J Med. 1995;62(2):127–131. [PubMed] [Google Scholar]
- 10.Jütte R. Alternative medicine and medico-historical semantics. In: Jütte R, Eklöf M, Nelson MC, editors. Historical Aspects of Unconventional Medicine: Approaches, Concepts, Case Studies. Sheffield: European Association for the History of Medicine and Health; 2001. pp. 11–26. [Google Scholar]
- 11.Complementary, alternative, or integrative health: what’s in a name? [webpage on the Internet] Bethesda, MD: National Center for Complementary and Alternative Medicine (NCCAM); 2008. [Accessed June 6, 2014]. [updated July 2014]. Available from: http://nccam.nih.gov/health/whatiscam. [Google Scholar]
- 12.Boon H, Verhoef M, O’Hara D, Findlay B. From parallel practice to integrative health care: a conceptual framework. BMC Health Serv Res. 2004;4(1):15. doi: 10.1186/1472-6963-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leckridge B. The future of complementary and alternative medicine – models of integration. J Altern Complement Med. 2004;10(2):413–416. doi: 10.1089/107555304323062446. [DOI] [PubMed] [Google Scholar]
- 14.About us: definition of integrative medicine [webpage on the Internet] Minneapolis, MN: Consortium of Academic Health Centers for Integrative Medicine; 2004. [Accessed June 6, 2014]. [edited November 2009]. Available from: http://www.imconsortium.org/about/ [Google Scholar]
- 15.Witt CM, Holmberg C. Changing academic medicine: strategies used by academic leaders of integrative medicine – a qualitative study. Evid Based Complement Alternat Med. 2012;2012:652546. doi: 10.1155/2012/652546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahern KR, Weston JF. M&As: the good, the bad, and the ugly. Journal of Applied Finance. 2007;17(1):5–20. [Google Scholar]
- 17.Cartwright S, Cooper CL. Managing Mergers, Acquisitions and Strategic Alliances Integrating People and Cultures. Oxford: Butter-worth-Heinemann; 1996. [Google Scholar]
- 18.Chatterjee S, Lubatkin M, Schweiger D, Weber Y. Cultural differences and shareholder value: explaining the variability in the performance of related merger. Strategic Management Journal. 1992;13(5):319–334. [Google Scholar]
- 19.Sherwin J. Changing culture, changing process: academic medicine’s own work in progress [webpage on the Internet] Washington, DC: Association of American Medical Colleges; 2011. [Accessed May 12, 2013]. [cited October 18, 2011]. Available from: https://www.aamc.org/newsroom/reporter/october2011/262456/changingculture.html. [Google Scholar]
- 20.Kummer C. Overcoming the challenges and issues of post-merger integration: putting PMI in the driver’s seat in the M&A process. In: Ganesh C, editor. Mergers and Acquisitions – Issues and Perspectives from the Asia–Pacific Region. Tokyo: Asian Productivity Organization; 2012. pp. 133–147. [Google Scholar]
- 21.Lubatkin M, Schweiger DM, Weber Y. Top management turnover in related M&A’s: an additional test of the theory of relative standing. J Manage. 1999;25(1):55–73. [Google Scholar]
- 22.Joos S, Musselmann B, Miksch A, Rosemann T, Szecsenyi J. The role of complementary and alternative medicine (CAM) in Germany – a focus group study of GPs. BMC Health Serv Res. 2008;8:127. doi: 10.1186/1472-6963-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schweiger DM, DeNisi AS. Communication with employees following a merger: a longitudinal field experiment. Acad Manage J. 1991;34(1):110–135. [Google Scholar]
- 24.Schweiger DM. M&A Integration: A Framework for Executives and Managers. New York, NY: McGraw Hill; 2002. [Google Scholar]