Abstract
Objectives
Use of complementary and alternative medicine (CAM) has increased over the past two decades, and a growing body of evidence suggests that some CAM modalities may be useful in addressing gastrointestinal (GI) conditions. However, the overall patterns of CAM use for GI conditions remains unknown. We sought to elucidate the prevalence and patterns of CAM use among U.S. adults with GI conditions.
Methods
We used the 2012 National Health Interview Survey (n=34,525), a nationally representative survey of the civilian, non-institutionalized U.S. population, to estimate the prevalence of CAM use among adults with GI conditions (abdominal pain, acid reflux/heartburn, digestive allergy, liver condition, nausea and/or vomiting, stomach or intestinal illness, ulcer). We also examined the reasons for CAM use, perceived helpfulness, and disclosure of use to health care providers among individuals who specifically used CAM to address a GI condition. Prevalence estimates were weighted to reflect the complex sampling design of the survey.
Results
Of 13,505 respondents with a GI condition in the past year, 42% (n=5629) used CAM in the past year and 3% (n=407) used at least one CAM modality to address a GI condition. The top 3 modalities among those using CAM to address GI conditions were herbs and supplements, mind body therapies, and manipulative therapies. Of those using CAM to address a GI condition, 47% used 3 or more CAM therapies, and over 80% felt that it was helpful in addressing a GI condition and was important in maintaining health and well-being. Respondents told their health care provider about use of these therapies 70% of the time.
Conclusions
CAM was used by 42% of respondents with a GI condition in the past year. A small proportion use CAM specifically to address their GI condition, but the majority who do find it helpful. The most commonly used modalities in this group are herbs and supplements, mind body, and manipulative therapies.
Introduction
Use of complementary and alternative medicine (CAM) has increased in the U.S. over the past two decades (1, 2). Evidence suggests that specific modalities may be effective for addressing certain gastrointestinal (GI) conditions (3–6). However, the prevalence, patterns, and effectiveness of CAM for GI conditions remains incompletely characterized.
Among patients with Crohn’s disease and ulcerative colitis CAM use ranges from 11–40% (7, 8), depending upon the population, year, and the modalities included in the definition of CAM. Other studies of convenience samples of patients with liver disease, functional bowel disorders, and other GI conditions found ranges of 20–52% (9–12). No large, nationally-representative studies have been published on CAM use among patients with GI conditions in the U.S.
The National Health Interview Survey (NHIS) gathers health-related data on the U.S. population and has previously been used to characterize CAM use among U.S. adults with several non-GI medical conditions (13–15). We used the 2012 NHIS data to examine the prevalence and patterns of CAM use among U.S. adults with GI conditions. We also examined disclosure to healthcare providers, reasons for use, and perceived helpfulness among adults specifically using CAM to address a GI condition.
Methods
Data Source
The National Health Interview Survey (NHIS) is a cross-sectional, face-to-face, survey conducted annually by the National Center for Health Statistics (NCHS) and the Centers for Disease Control (CDC) that gathers health-related data on the civilian, non-institutionalized U.S. population. The survey uses a complex, multi-stage sampling design and oversamples minorities to achieve population representation. Sampling weights are subsequently applied to the data to obtain statistically accurate estimates for the U.S. population. Every five years, the survey includes questions about CAM use. The 2012 NHIS includes 34,525 U.S. adults with a conditional response rate of 79.7% (16). The 2012 CAM supplement serially asked participants whether they saw a practitioner for, or used, a given CAM modality within the past 12 months. Respondents were asked to rank their top three CAM modalities and state whether they used these modalities to address one or more symptoms or health conditions. For each of the top three CAM modalities, the survey also asked about disclosure to healthcare providers, use of medical treatments, sources of information about CAM, and the reasons, motivations, perceived benefits, and perceived helpfulness of CAM use.
Study Population
We defined adults with a GI condition as everyone who indicated the occurrence of one or more of the following on either the sample adult or CAM portions of the survey within the past 12 months: abdominal pain, acid reflux or heartburn, digestive allergy, liver condition, nausea and/or vomiting, ulcer, and stomach or intestinal illness. Each of these conditions was asked of all survey respondents except for the last category (stomach or intestinal illness) which was only asked of individuals using a CAM modality to address a health-related condition. We also identified a subpopulation of 407 adults who had used one or more of their top three CAM modalities specifically to address one or more of the GI conditions listed above.
Population Characteristics
The sociodemographic characteristics that we examined included sex, age, race, ethnicity, region of residence, education, marital status, income, and insurance status. We also examined perceived health status, BMI, and health behaviors such as smoking status, alcohol use, and physical activity (17). For the comorbidity score, subjects were given a point for heart disease (coronary heart disease, ever had a heart attack, other heart condition), hypertension, pulmonary disease (emphysema, COPD, asthma, or chronic bronchitis), mental health concern in the last 12 months (depression, anxiety, other mental health disorder), neurological issues (recurring headache, memory loss, stroke, other neurological problem), weak/failing kidneys, or ever diagnosed with cancer, diabetes, or arthritis.
Outcomes
Use of a CAM modality was defined as a positive response to use of a specific modality and/or visit to a practitioner of that modality within the past 12 months. Modalities were categorized into one of the following groups: herbs and non-vitamin non-mineral supplements, manipulative therapies (chiropractic, osteopathic manipulation, massage, craniosacral therapy), mind body therapies (hypnosis, biofeedback, meditation, imagery, progressive relaxation, and mind body exercise [yoga, tai chi, qi gong]), special diets (vegetarian or vegan, macrobiotic, Atkins diet, Pritikin diet, Ornish diet, or saw a practitioner for dietary counseling), movement therapies (Feldenkrais, Alexander technique, Pilates, Trager psychological integration), and other CAM modalities (acupuncture, ayurveda, chelation, energy healing, homeopathy, naturopathy, traditional healers). Use of vitamin and mineral supplements was excluded due to the high prevalence of use; teas were also not included. To sum the total number of CAM modalities used by each respondent we counted herb and supplement use only once; meditation, imagery, and progressive relaxation comprised a single category; mind body exercises were one category; and any special diets were counted only once.
We also assessed the reasons, motivations, perceived benefits, and perceived helpfulness of CAM use; disclosure to healthcare providers; and sources of information about CAM among individuals using these modalities to specifically address a GI condition. To determine whether having a GI condition was independently associated with CAM use, we conducted a logistic regression analysis adjusting for all of the sociodemographic and health factors in Table 1.
Table 1.
Characteristics of adults with and without GI conditions
| No GI condition, n=21020, n(%)^ |
Any GI condition, n=13,505, n(%)^ |
Chi square p value |
|
|---|---|---|---|
| Estimated U.S. Population Size* | N=143,408,789 | N=91,511,881 | |
| Sex | <.0001 | ||
| Female | 11005 (48.3%) | 8247 (57.5%) | |
| Male | 10015 (51.7%) | 5258 (42.5%) | |
| Age | 0.0008 | ||
| 18–29 | 3956 (22.1%) | 2464 (20.8%) | |
| 30–44 | 5540 (26.2%) | 3330 (24.7%) | |
| 45–64 | 7008 (34.0%) | 4845 (36.3%) | |
| ≥ 65 | 4516 (17.6%) | 2866 (18.2%) | |
| Race | <.0001 | ||
| White | 15265 (77.7%) | 10674 (84.0%) | |
| Black | 3530 (13.4%) | 1789 (9.5%) | |
| American Indian/Alaskan Native | 204 (0.8%) | 145 (0.9%) | |
| Asian | 1644 (6.7%) | 539 (3.2%) | |
| Other | 377 (1.5%) | 358 (2.3%) | |
| Hispanic | 4036 (16.9%) | 1823 (11.7%) | <.0001 |
| Region | <.0001 | ||
| Northeast | 3719 (19.7%) | 2055 (15.9%) | |
| Midwest | 4185 (21.3%) | 3008 (25.0%) | |
| South | 7658 (36.6%) | 4878 (36.2%) | |
| West | 5458 (22.5%) | 3564 (22.9%) | |
| Marital Status | <.0001 | ||
| Married/Living with Partner | 10376 (59.8%) | 6677 (61.0%) | |
| Widowed | 1937 (5.7%) | 1348 (6.5%) | |
| Divorced | 3393 (10.7%) | 2446 (12.3%) | |
| Never Married | 5259 (23.7%) | 3011 (20.2%) | |
| Education | 0.32 | ||
| < High School | 3389 (14.1%) | 2098 (13.6%) | |
| High School or equivalent | 5516 (26.3%) | 3422 (26.0%) | |
| > High School | 12009 (59.0%) | 7938 (60.0%) | |
| Family Income | <.0001 | ||
| < $34,999 | 8392 (30.1%) | 5960 (34.0%) | |
| $35,000 – $74,999 | 6039 (29.6%) | 3879 (30.6%) | |
| $75,000 – $99,999 | 2071 (12.1%) | 1179 (10.6%) | |
| ≥$100,000 | 3206 (21.6%) | 1873 (19.7%) | |
| Unknown/Undefined | 1312 (6.6%) | 614 (5.1%) | |
| Insurance Status | <.0001 | ||
| Uninsured | 3994 (17.9) | 2162 (15.3) | |
| Medicare | 4733 (18.3) | 3488 (22.2) | |
| Medicaid | 1395 (6.0) | 1125 (7.2) | |
| Private | 10155 (54.5) | 6122 (51.0) | |
| Other | 667 (3.0) | 572 (4.0) | |
| Perceived Health Status | <.0001 | ||
| Excellent | 6432 (33.1) | 2426 (20.4) | |
| Very Good | 6872 (33.3) | 3872 (30.4) | |
| Good | 5532 (25.0) | 4104 (29.4) | |
| Fair | 1790 (7.1) | 2209 (13.9) | |
| Poor | 385 (1.6) | 885 (5.7) | |
| BMI | <.0001 | ||
| < 20 | 1156 (5.5) | 681 (5.1) | |
| 20–25 | 6653 (32.0) | 3630 (26.7) | |
| 25–30 | 7131 (33.8) | 4346 (32.8) | |
| 30–35 | 3303 (15.7) | 2411 (17.8) | |
| > 35 | 1939 (8.7) | 1920 (13.9) | |
| Unknown | 838 (4.2) | 517 (3.7) | |
| Smoking Status | <.0001 | ||
| Current | 3560 (16.0) | 2876 (20.9) | |
| Former | 4220 (20.1) | 3364 (25.0) | |
| Never | 13081 (63.1) | 7155 (53.4) | |
| Unknown | 159 (0.8) | 110 (0.8) | |
| Alcohol Use | <.0001 | ||
| None | 8002 (35.6) | 4849 (33.6) | |
| Light | 8485 (42.2) | 5782 (44.5) | |
| Moderate | 3062 (15.4) | 1854 (14.6) | |
| Heavy | 998 (4.5) | 761 (5.5) | |
| Unknown | 473 (2.3) | 259 (1.8) | |
| Physical Activity | <.0001 | ||
| Low | 7122 (31.5) | 4783 (33.4) | |
| Moderate | 3586 (17.6) | 2644 (20.3) | |
| High | 10090 (49.7) | 5942 (45.3) | |
| Unknown | 222 (1.2) | 136 (1.0) | |
| Comorbidity Score | <.0001 | ||
| 0 | 10060 (50.3) | 2979 (24.0) | |
| 1 | 5443(26.0) | 3152 (24.6) | |
| 2–3 | 4434(19.6) | 4747 (34.5) | |
| 4+ | 1083 (4.2) | 2627 (16.9) |
n=number of individuals responding in the survey; (%) = weighted percent estimate for the U.S. population
The complex sampling design of the NHIS allows for estimation of the U.S. population
Statistical analyses
We used SAS v9.2, proc surveyfreq, and the population weights provided by the NCHS (16) to account for the complex sampling design of the survey and to obtain stastistically accurate estimates of percentages for the civilian, non-institutionalized U.S. population. Chi-square tests for differences in proportions were conducted. Logistic regression analysis was performed using SAS-callable SUDAAN v11.0. Following the recommendations of the NCHS, estimates with relative standard errors greater than 30% were suppressed due to their likely unreliability. We conducted a sensitivity analysis excluding nausea and/or vomiting from our definition of GI condition as this was one of the largest categories of respondents and may represent an acute illness or be construed as more of a symptom than an actual condition. This study was reviewed and granted exempted status by the Beth Israel Deaconess Medical Center Committee on Clinical Investigations as all data were de-identified.
Results
Sample Characteristics
Overall, 13,505 (39%) of the 34,525 adults surveyed reported at least one GI condition within the past year. The sociodemographic characteristics and health behaviors of adults with and without GI conditions differed significantly (Table 1). Compared to those without GI conditions, adults with GI conditions were more likely to be female, white, non-Hispanic, have a poorer perception of health status, a current or former smoker, have lower levels of physical activity, and greater illness burden.
CAM Use Among Adults With and Without GI Conditions
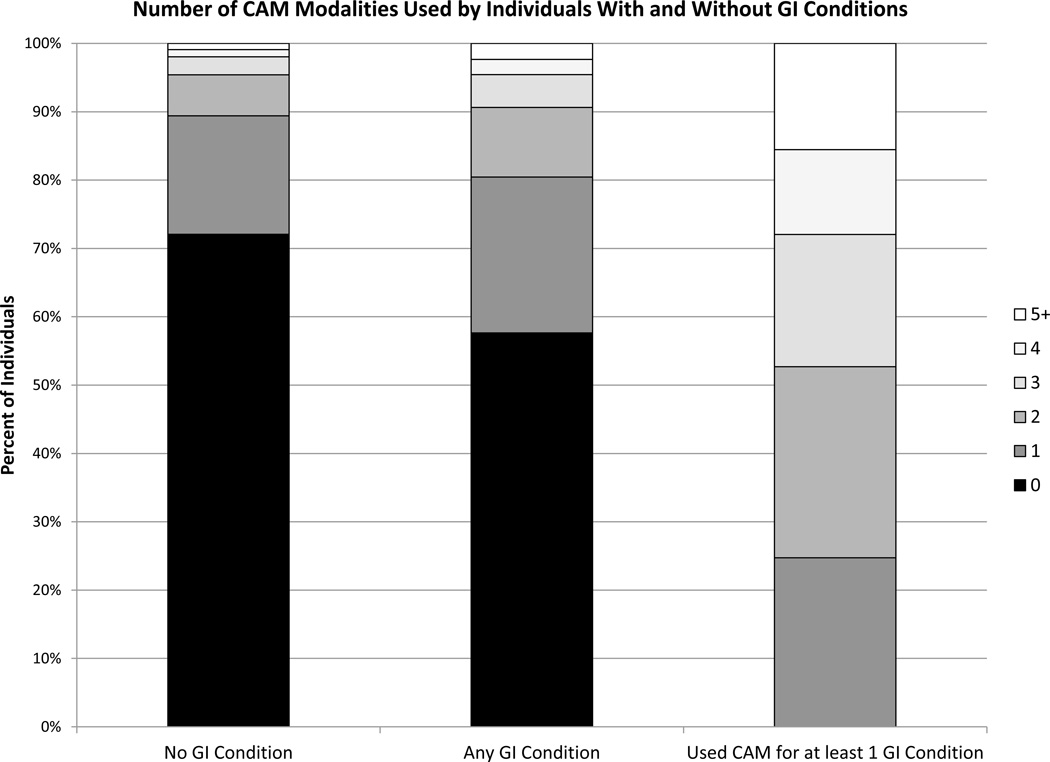
Of 13,505 respondents with a GI condition in the past year, 42% (n=5629) used CAM in the past year and 3% (n=407) used at least one CAM modality to address a GI condition. CAM use was prevalent across each of the GI conditions examined (Table 2), ranging from 38%–51%. For all conditions, the most commonly used CAM modality was herbs and dietary supplements (20–31%), followed by manipulative (15–25%) and mind body (11–23%) therapies. Each of the individual CAM modalities examined was used more often among adults with a GI condition compared to those without a GI condition (Table 3). The total number of CAM modalities used by U.S. adults within the past year varied widely, from 0–12 (Figure 1). Among those who used CAM specifically to address a GI condition, 47% used 3 or more CAM modalities. After adjusting for sociodemorgraphic and health factors, the odds ratio for CAM use among those who have a GI condition was 1.69 (95% CI 1.57 – 1.81; data not shown). We also performed a sensitivity analysis excluding nausea and/or vomiting from our definition of GI condition, and our results did not substantially change (data not shown).
Table 2.
GI conditions and frequency of modalities used
| Herbs & Supplements# |
Manipulative Therapy |
Mind Body | Special Diet |
Movement Therapy |
Other | Any CAM | |
|---|---|---|---|---|---|---|---|
| GI Condition (n)^ | n(%)^ | n(%)^ | n(%)^ | n(%)^ | n(%)^ | n(%)^ | n(%)^ |
| Abdominal Pain (n=3516) | 826 (24.3) | 686 (19.6) | 628 (18.7) | 169 (5.1) | 99 (2.9) | 293 (8.6) | 1540 (44.8) |
| Acid Reflux / Heartburn (n=7903) | 1689 (21.5) | 1392 (17.5) | 967 (12.4) | 265 (3.4) | 124 (1.7) | 454 (5.5) | 3055 (38.8) |
| Digestive Allergy (n=1425) | 416 (30.7) | 337 (25.2) | 308 (23.1) | 94 (7.5) | 59 (5.3) | 172 (12.4) | 708 (50.9) |
| Liver Condition (n=513) | 111 (21.7) | 73 (14.8) | 69 (11.1) | 20 (3.2) | * | 39 (7.7) | 196 (38.1) |
| Nausea/Vomiting (n=6741) | 1602 (24.2) | 1394 (20.6) | 1372 (20.2) | 312 (4.5) | 226 (3.5) | 486 (6.9) | 3113 (46.6) |
| Ulcer (n=676) | 130 (19.5) | 118 (18.2) | 101 (15.6) | 22 (3.1) | * | 46 (7.4) | 262 (39.6) |
Does not include vitamin or mineral supplements
n=number of individuals responding in the survey; (%) = weighted percent estimate for the U.S. population
Number suppressed because relative standard error is over 30% and estimate is unreliable
Table 3.
Most commonly used modalities for individuals with and without GI conditions
| Modality | No GI condition, n=21020, n(%)^ |
Any GI condition, n=13505, n(%)^ |
Used CAM for GI condition, n=407, n(%)^* |
|---|---|---|---|
| Any CAM | 5887 (27.9) | 5629 (42.4) | 407 (100) |
| Herbs & Supplements# | 2922 (13.6) | 3052 (23.0) | 316 (79.5) |
| Meditation/Imagery/Progressive Relaxation | 643 (2.9) | 972 (7.2) | 138 (35.8) |
| Mind Body Exercise | 1678 (8.1) | 1527 (11.7) | 125 (30.4) |
| Massage | 1429 (6.7) | 1522 (11.3) | 107 (27.5) |
| Chiropractic/Osteopathic Manipulation | 1492 (7.3) | 1501 (11.2) | 113 (25.8) |
| Homeopathy | 308 (1.5) | 410 (3.2) | 90 (25.9) |
| Special Diet | 489 (2.2) | 538 (4.0) | 81 (18.8) |
| Naturopathy | 98 (0.4) | 178 (1.2) | 46 (11.6) |
| Acupuncture | 285 (1.2) | 319 (2.2) | 35 (7.7) |
| Movement Therapy | 353 (1.7) | 325 (2.6) | 31 (7.9) |
n=number of individuals responding in the survey; (%) = weighted percent estimate for the U.S. population
Explicitly used at least one of their top three CAM modalities for at least 1 GI condition
Does not include vitamin or mineral supplements
Figure 1.
Number of CAM modalities used by individuals with and without GI conditions. The stacked bar graph illustrates the percentage of survey respondents who used 0, 1, 2, 3, 4, or 5 or more CAM modalities. The three populations shown are those individuals with no GI condition (n=21020), individuals with one or more GI conditions (n=13505), and individuals who used at least one of their top three CAM modalities to address a GI condition (n=407).
As herbs and other non-vitamin, non-mineral dietary supplements are the most commonly used CAM modality by the U.S. population, we examined the patterns of use of the most common dietary supplements (Table 4). Consistent with our findings in Table 3, adults with GI conditions were more likely to use both GI-specific (e.g., probiotics, digestive enzymes) and non-GI-specific (e.g., glucosamine, cranberry) supplements.
Table 4.
Herbs andsupplements most commonly used by individuals with and without GI conditions#
| Herbs & Supplements | No GI condition, n=21020, n(%)^ |
Any GI condition, n=13505, n(%)^ |
Used CAM for GI condition, n=407, n(%)^* |
|---|---|---|---|
| Fish Oil | 1884 (8.9) | 1882 (14.3) | 182 (47.2) |
| Probiotics or Prebiotics | 348 (1.6) | 546 (4.3) | 165 (45.3) |
| Digestive Enzymes (Lactaid) | 135 (0.6) | 304 (2.1) | 108 (26.1) |
| Other Herbs and Supplements# | 599 (2.7) | 689 (5.2) | 102 (24.9) |
| Glucosamine | 585 (2.7) | 583 (4.6) | 54 (16.7) |
| Cranberry | 230 (1.0) | 375 (2.6) | 53 (13.4) |
| Echinacea | 417 (1.9) | 458 (3.3) | 52 (13.1) |
| Melatonin | 321 (1.5) | 469 (3.4) | 46 (13.1) |
| Ginseng | 312 (1.3) | 360 (2.6) | 52 (12.7) |
| CoQ10 | 327 (1.5) | 338 (2.5) | 49 (12.4) |
| Garlic | 269 (1.1) | 294 (2.0) | 42 (11.2) |
| Milk Thistle (Silymarin) | 130 (0.6) | 178 (1.2) | 41 (10.6) |
| Bee Pollen | 170 (0.8) | 157 (1.2) | 33 (9.6) |
| Chondroitin | 287 (1.4) | 315 (2.4) | 32 (9.5) |
| Green Tea | 202 (0.9) | 265 (1.9) | 37 (8.5) |
| Ginkgo | 253 (1.0) | 250 (1.8) | 31 (7.1) |
n=number of individuals responding in the survey; (%) = weighted percent estimate for the U.S. population
Explicitly used at least one of their top three CAM modalities for at least 1 GI condition.
Does not include vitamin or mineral supplements
CAM Use Among Those Specifically Addressing a GI Condition
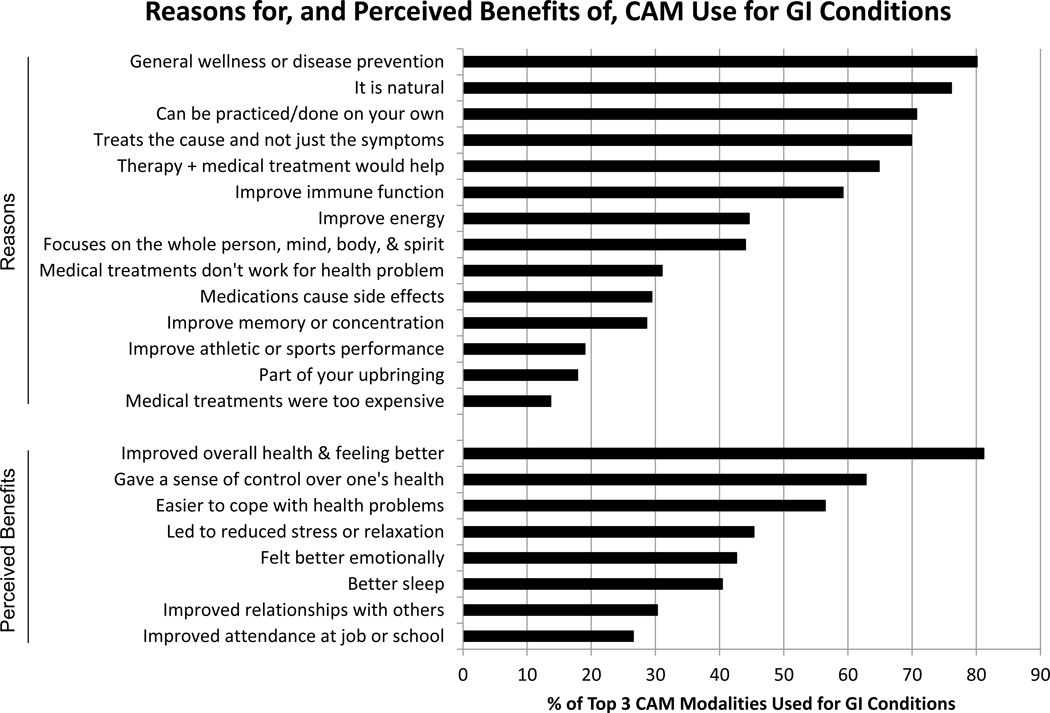
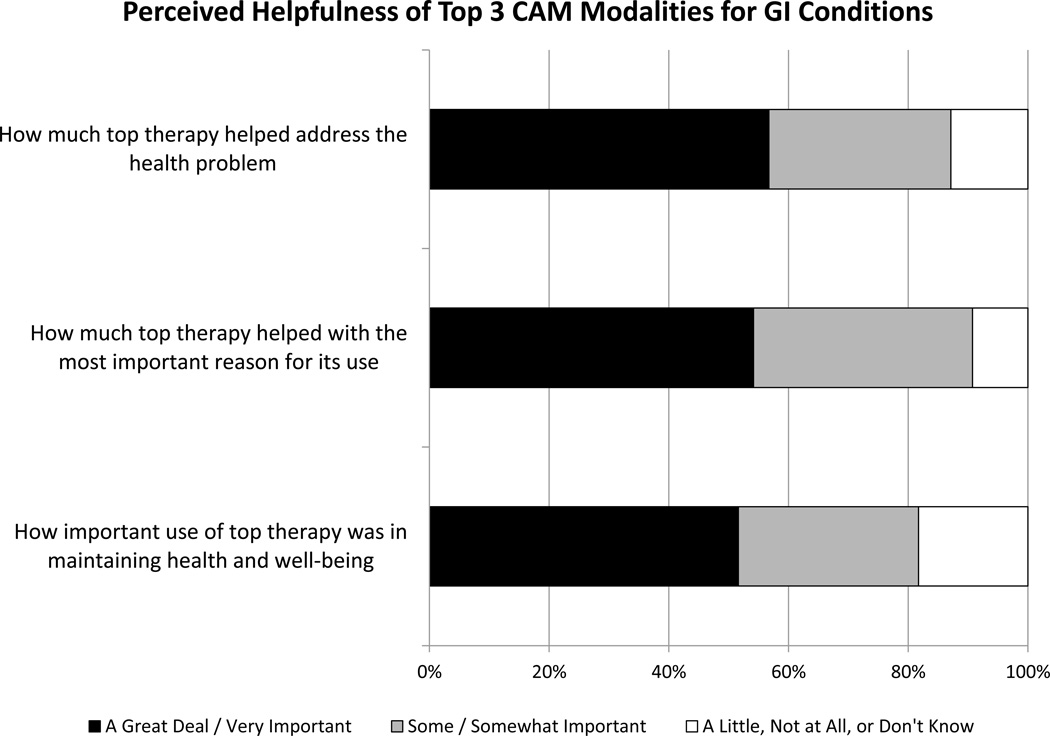
Figure 2 illustrates the reasons for, and perceived benefits of, CAM use for GI conditions. Over 80% of respondents using CAM to address a GI condition felt that it was helpful in addressing the GI-related problem and in maintaining health and well-being (Figure 3).
Figure 2.
Reasons for, and perceived benefits of, CAM use for GI conditions. Shown in descending order are the percent of the top 3 CAM modalities used to address GI conditions that were used for the reasons cited, or benefits experienced, by respondents (n=407).
Figure 3.
Perceived helpfulness of Top 3 CAM modalities for GI Conditions. Survey respondents (n=407) were asked 1) How much did the therapy help address the health problem, 2) How much did the therapy help with the most important reason for its use, and 3) How important was use of the therapy in maintaining health and well-being. Most important reasons for use included 18 possible choices (general wellness/disease prevention; improve energy, immune function, athletic performance, memory or concentration; eat healthier, more organic foods; cut back or stop drinking alcohol, smoking cigarettes; exercise more regularly; and the 8 perceived benefits listed in Figure 2).
In addition to using CAM, many respondents in this population also received prescription (48%) and/or over-the-counter (47%) medications to address one of their top three most important health conditions. Respondents told their personal health care provider about 70% of the top three CAM modalities that they were using for GI conditions. Among those who did not disclose CAM use, the most common reasons were that the provider didn’t ask (51%) and that they didn’t think the provider needed to know (44%).
CAM modalities for GI conditions were most frequently recommended by family (38%), physicians (33%), and friends (30%) and the most common sources of information on these therapies were print material such as books, magazines, and newspapers (35%) and the internet (34%).
Discussion
CAM use is more common among adults with GI conditions (42%) compared to adults without GI conditions (28%). The adjusted odds ratio for CAM use among adults with GI conditions was 1.69. The most commonly used modalities among U.S. adults with GI conditions include herbs and supplements, manipulative therapies, and mind body therapies. Moreover, 47% of those who specifically used at least one of their top three CAM modalities to address a GI condition used three or more modalities. The majority felt that CAM was helpful in addressing a GI condition and in maintaining health and well-being.
An increased frequency of CAM use among U.S. adults with medical conditions has also been found for adults with arthritis (13) and neurological conditions (15), but not for adults with cardiovascular disease (14). Prior studies have found an association between CAM use and female gender, higher levels of education and income, and the presence of other medical conditions (2, 11). While these associations were also present in our population, after adjusting for these and other factors, having a GI condition was still significantly associated with CAM use.
We found the prevalence of CAM use among U.S. adults with GI conditions is similar to prior reports (7, 8, 10, 11), however, given that we did not include the use of prayer or vitamins and minerals in our analysis as several prior reports do, our estimates likely reflect a somewhat higher prevalence of CAM use in comparison. Nonetheless, the majority of CAM use among U.S. adults with GI conditions is not specifically targeted to address GI conditions.
A novel feature of our analysis is that we identified a subpopulation of individuals who specifically used CAM to address a GI condition. Within this population, the most common reasons for, and perceived benefits of, CAM use were related to general health and well-being and to a sense of self-efficacy.
Our study has several limitations. NHIS data are based upon self-report and thus subject to misclassification and recall bias. Our definition of GI conditions is limited to those that were included in the survey. Thus, we may be missing a substantial number of individuals with small or large bowel disease, such as inflammatory bowel diseases and irritable bowel syndrome, chronic pancreatitis, and biliary diseases who did not respond to the questions about abdominal pain or nausea and/or vomiting. Furthermore, the severity and duration of GI-related disease could not be ascertained in this population, those using CAM to cope with symptoms related to a GI condition or side effects of a medication for a GI condition (e.g., depression, fatigue) are not captured, and NHIS only assesses in more detail the top three CAM modalities used by respondents. These factors may have resulted in an underestimation of both the overall use and condition–specific use of CAM among adults with GI conditions. However, we also cannot distinguish one-time CAM users from frequent users. In addition, there are a variety of special diets that are now popular among some GI patients (e.g., gluten-free, low FODMAP) that are not assessed on the NHIS. We tried to capture these populations by including visits to practitioners for special diets, which may also include visits to traditional nutritionists. Nonetheless, we may still have underestimated the prevalence of use of special diets in this population.
In conclusion, we found that 42% of adults with a GI condition who completed the survey used CAM within the past year, and at least 7% of them used CAM to specifically address a GI condition. In the latter population, 47% used three or more CAM modalities in the past year and over 80% of CAM therapies used for GI conditions were perceived to be helpful. Further study of this population may provide clues for promising therapies worthy of further study, while enhancing communication between doctors and patients on this topic may promote better clinical use of evidence-based CAM therapies.
Acknowledgement
We thank Dr. Suzanne Bertisch for NHIS insights and contributions to SAS demographics code.
Guarantor of the article: Michelle L. Dossett, MD, PhD, MPH.
Study Support
Financial support: M.L.D was supported by an institutional National Research Service Award #T32AT000051 from the National Center for Complementary and Alternative Medicine (NCCAM) at the NIH and by the Division of General Medicine and Primary Care at Beth Israel Deaconess Medical Center. This work was conducted with support from Harvard Catalyst, The Harvard Clinical and Translational Science Center (NIH Award 1UL1 TR001102-01 and financial contributions from Harvard University and its affiliated academic health care centers). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
Footnotes
Conflict of Interest
Potential competing interests: None.
Specific author contributions: M.L.D.: conceived the study, performed data analysis and interpretation, drafted the manuscript. R.B.D.: data analysis and interpretation, critically reviewed the manuscript. A.J.L. and G.Y. contributed to study design, data interpretation, critically reviewed the manuscript.
References
- 1.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the united states, 1990–1997: Results of a follow-up national survey. JAMA. 1998 Nov 11;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United states, 2007. Natl Health Stat Report. 2008 Dec 10;(12)(12):1–23. [PubMed] [Google Scholar]
- 3.Gaylord SA, Palsson OS, Garland EL, Faurot KR, Coble RS, Mann JD, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. Am J Gastroenterol. 2011 Sep;106(9):1678–1688. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanai H, Iida T, Takeuchi K, Watanabe F, Maruyama Y, Andoh A, et al. Curcumin maintenance therapy for ulcerative colitis: Randomized, multicenter, double-blind, placebo-controlled trial. Clin Gastroenterol Hepatol. 2006 Dec;4(12):1502–1506. doi: 10.1016/j.cgh.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Dickman R, Schiff E, Holland A, Wright C, Sarela SR, Han B, et al. Clinical trial: Acupuncture vs. doubling the proton pump inhibitor dose in refractory heartburn. Aliment Pharmacol Ther. 2007 Nov 15;26(10):1333–1344. doi: 10.1111/j.1365-2036.2007.03520.x. [DOI] [PubMed] [Google Scholar]
- 6.Guarner F, Khan AG, Garisch J, Eliakim R, Gangl A, Thomson A, et al. World gastroenterology organisation global guidelines: Probiotics and prebiotics october 2011. J Clin Gastroenterol. 2012 Jul;46(6):468–481. doi: 10.1097/MCG.0b013e3182549092. [DOI] [PubMed] [Google Scholar]
- 7.Hilsden RJ, Verhoef MJ, Rasmussen H, Porcino A, DeBruyn JC. Use of complementary and alternative medicine by patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011 Feb;17(2):655–662. doi: 10.1002/ibd.21360. [DOI] [PubMed] [Google Scholar]
- 8.Rawsthorne P, Clara I, Graff LA, Bernstein KI, Carr R, Walker JR, et al. The manitoba inflammatory bowel disease cohort study: A prospective longitudinal evaluation of the use of complementary and alternative medicine services and products. Gut. 2012 Apr;61(4):521–527. doi: 10.1136/gutjnl-2011-300219. [DOI] [PubMed] [Google Scholar]
- 9.Strader DB, Bacon BR, Lindsay KL, La Brecque DR, Morgan T, Wright EC, et al. Use of complementary and alternative medicine in patients with liver disease. Am J Gastroenterol. 2002 Sep;97(9):2391–2397. doi: 10.1111/j.1572-0241.2002.05993.x. [DOI] [PubMed] [Google Scholar]
- 10.van Tilburg MA, Palsson OS, Levy RL, Feld AD, Turner MJ, Drossman DA, et al. Complementary and alternative medicine use and cost in functional bowel disorders: A six month prospective study in a large HMO. BMC Complement Altern Med. 2008 Jul 24;8 doi: 10.1186/1472-6882-8-46. 46,6882-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ganguli SC, Cawdron R, Irvine EJ. Alternative medicine use by canadian ambulatory gastroenterology patients: Secular trend or epidemic? Am J Gastroenterol. 2004 Feb;99(2):319–326. doi: 10.1111/j.1572-0241.2004.04046.x. [DOI] [PubMed] [Google Scholar]
- 12.Kong SC, Hurlstone DP, Pocock CY, Walkington LA, Farquharson NR, Bramble MG, et al. The incidence of self-prescribed oral complementary and alternative medicine use by patients with gastrointestinal diseases. J Clin Gastroenterol. 2005 Feb;39(2):138–141. [PubMed] [Google Scholar]
- 13.Quandt SA, Chen H, Grzywacz JG, Bell RA, Lang W, Arcury TA. Use of complementary and alternative medicine by persons with arthritis: Results of the national health interview survey. Arthritis Rheum. 2005 Oct 15;53(5):748–755. doi: 10.1002/art.21443. [DOI] [PubMed] [Google Scholar]
- 14.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006 Sep 1;98(5):673–680. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 15.Wells RE, Phillips RS, Schachter SC, McCarthy EP. Complementary and alternative medicine use among US adults with common neurological conditions. J Neurol. 2010 Nov;257(11):1822–1831. doi: 10.1007/s00415-010-5616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Division of Health Interview Statistics, National Center for Health Statistics. NHIS survey description [Internet] Hyattsville, Maryland: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 17.Kushi LH, Fee RM, Folsom AR, Mink PJ, Anderson KE, Sellers TA. Physical activity and mortality in postmenopausal women. JAMA. 1997 Apr 23–30;277(16):1287–1292. [PubMed] [Google Scholar]