Lesson
We report a polytrauma case requiring simultaneous neurosurgery and laparotomy. Upon abdominal closure, raised intracranial pressure occurred. This illustrates the important physiological interplay between body compartments in critical care patients.
Keywords: Traumatic brain injury, intracranial hypertension, decompressive laparotomy, multiple compartment syndrome
Case presentation
A 20-year-old Caucasian male was admitted to a London major trauma centre following a motorcycle collision. On arrival to hospital, examination revealed a Glasgow Coma Scale score of 3/15, pupils sized 2 mm and equal and hypovolaemic shock (blood pressure, 65/23 mmHg; heart rate, 140/min). He was immediately intubated. Focused Assessment with Sonography for Trauma was positive for intraabdominal fluid. The patient was transfused with two units of packed red cells, and his systolic blood pressure increased to 116 mmHg. An immediate computed tomography (CT) scan demonstrated an acute right-sided subdural haematoma with midline shift and effacement of the lateral ventricle and suprasellar cisterns, a Grade 4 splenic laceration with active bleeding, a Grade 3 renal injury with no active bleeding and multiple bony injuries.
He was transferred directly to the theatre where he underwent simultaneous craniotomy with evacuation of subdural haematoma and laparotomy with emergency splenectomy.
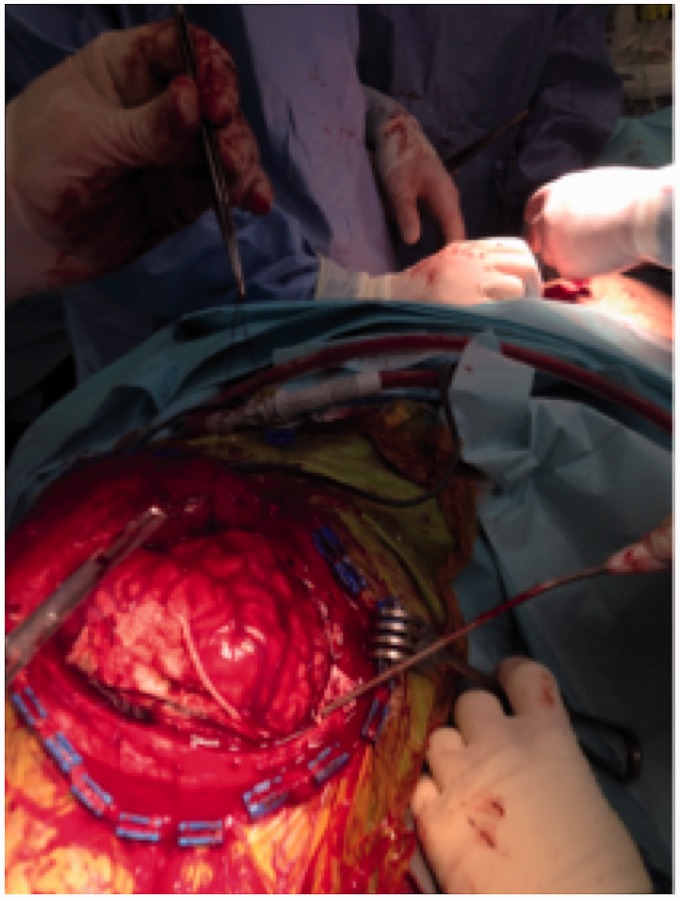
Initially, during the craniotomy, the brain appeared pulsating and non-oedematous, and the subdural haematoma was evacuated without complications. Upon closure of the abdominal fascia after completion of the splenectomy, the brain herniated from the craniotomy; this was accompanied by significant bleeding from the right transverse sinus (see Figure 1). Loosening the tension of the abdominal sutures arrested the venous bleeding in the cranium, which recurred on retightening. Sinus wall defect haemostasis required Flo-Seal™, Surgicell™ and tonsil swab packing, and the bone flap was not replaced. Post-operative CT scan with venogram and arteriogram confirmed significant fracture overlying the right transverse sinus, further supporting the supposition that the intraoperative ooze had originated from this site. No venous sinus thrombosis was seen on the post-operative CT scan.
Figure 1.
An intraoperative photograph of the patient’s brain herniating through the craniotomy on abdominal fascia closure.
Four months post-injury, the patient’s Glasgow Coma Scale is 9/10 (eyes open spontaneously, spontaneous ventilation through a tracheostomy and localises to pain). He has no motor activity on his left side and has required multiple re-admissions to the Intensive Treatment Unit for a variety of reasons, including hospital-acquired pneumonia, acute kidney injury exacerbated by pre-existing renal disease and post-cranioplasty, development of significant hygroma requiring insertion of a ventriculo-peritoneal shunt.
Discussion
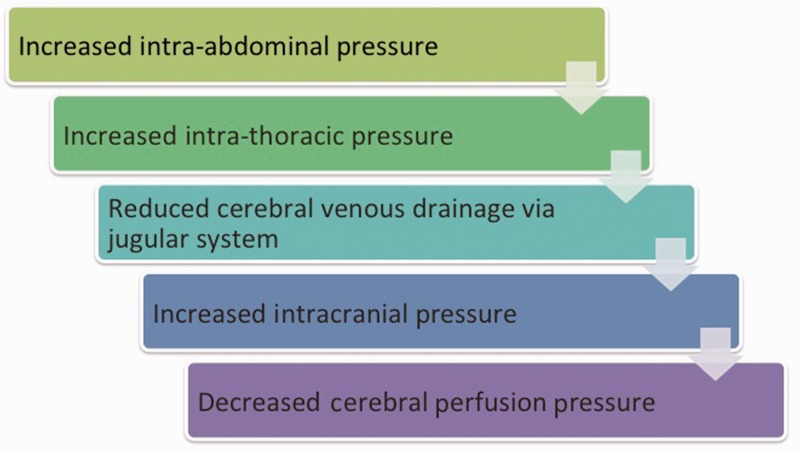
In this case, intracranial pressure was directly observed to rise significantly upon closure of the abdominal fascia. A number of small studies in the literature describe a close relationship between intraabdominal (IAP), intrathoracic (ITP) and intracranial (ICP) pressure in patients with traumatic brain injury (TBI).1
In a swine model, artificially increasing IAP caused a transmitted increase in ITP, impeding cerebral venous outflow and subsequently increasing ICP. In the same study, swine models with a median thoracotomy and pleuropericardotomy had no significant change in intracranial pressure upon increasing IAP2 (see Figure 2).
Figure 2.
Flowchart illustrating the interplay between pressure compartments in patients with traumatic brain injury.
Prospective studies have confirmed that induced abdominal compartment syndrome raises ICP in TBI patients. By positioning a weight on the abdomen of the Intensive Treatment Unit-based patients with a head injury, Citerio et al.3 demonstrated an increase in IAP which was associated with a significant increase in ICP (from 12.0 ± 4.2 to 15.5 ± 4.4 mmHg; p < 0.01). In this paper, Citerio’s group raise the possibility of routine measurement of IAP in a subset of patients in order to identify remediable causes of raised ICP.
Work by Scalea’s group has demonstrated considerable reductions in ICP with decompressive laparotomy (DL) in patients with refractory intracranial hypertension following TBI. In one paper, 17 out of 17 patients without abdominal compartment syndrome benefitted from a reduction in ICP (mean 27.5–17.5 mmHg), although in six patients (all of whom subsequently died) this fall was transient.4 Following two successful cases in 2000 in which DL improved ICP and led to good neurological recovery, Scalea’s group began routine measurement of IAP in patients with high ICP measurements. They have found DL to be lifesaving in some cases and recommend DL to be performed before obvious signs of abdominal compartment syndrome are manifest.
Scalea’s group also suggest that treatment decisions in TBI patients designed to treat one physiological system may be detrimental to others. For example, aggressive fluid resuscitation and ventilatory manoeuvres can increase IAP and ITP, respectively, thereby further increasing ICP.5 Here, Scalea studies patients with multiple compartment syndrome who underwent either decompressive craniectomy (DC) or DL or both. Results showed that in 24 patients, although ICP was initially significantly reduced (p < 0.05), it increased steadily during the subsequent 24 to 72 h. This cohort of patients was also noted to have a significantly higher Injury Severity Score and fluid requirement in the first seven days after admission compared to patients who had only DC.
Conclusions
With the advent of major trauma networks in the UK, major trauma centres will frequently encounter severe polytrauma cases. It is well known that pressure compartments in the body are interdependent, and we re-iterate the importance of considering that interplay in polytrauma patients here. As described, Scalea’s group have found some success in performing decompressive laparotomies to treat refractory intracranial hypertension. However, the decision to undertake DL must be weighed against the possible risk of infection, enterocutaneous fistulae and abdominal wall hernia in an already compromised cohort.4 Routine IAP measurements may assist clinicians in observing trends between IAP & ICP and assessing the potential benefit of DL. This is a potentially exciting and novel treatment for refractory intracranial hypertension which may be increasingly considered as an option in the UK. However, it is of paramount importance to continue to consider simple measures of reducing body compartment pressures (and thereby ICP), such as loosening tightly fitted C-spine collars, cautious administration of intravenous fluids and mindful use of positive pressure ventilation.
This case clearly illustrates the complex interplay between body compartments in critical care patients in the context of trauma. In this case, although the patient’s head injury was severe and his potential for neurological recovery was poor, delayed closure of the laparotomy incision may have been beneficial.
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
The patient was unable to provide written informed consent so this has been provided by his next of kin for the publication of this case report.
Guarantor
MW
Contributorship
All authors were directly involved with the care of the patient. SH and LC contributed to the writing of the case report. MW was the primary surgeon and reviewed and edited the manuscript.
Acknowledgements
The patient and his family are gratefully acknowledged.
Provenance
Not commissioned; peer-reviewed by Peter Hutchinson
References
- 1.Lauerman MH, Stein DM. Multicompartment management of patients with severe traumatic brain injury. Curr Opin Anaesthesiol 2014; 27: 219–224. [DOI] [PubMed] [Google Scholar]
- 2.Bloomfield G, Ridings P, Blocher C, et al. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. J Trauma 1997; 25: 496–503. [DOI] [PubMed] [Google Scholar]
- 3.Citerio G, Vascatto E, Villa F, et al. Induced abdominal compartment syndrome increases intracranial pressures in neurotrauma patients. Crit Care Med 2001; 297: 1466–1471. [DOI] [PubMed] [Google Scholar]
- 4.Joseph DK, Dutton RP, Aarabi B, Scalea TM. Decompressive laparotomy to treat intractable intracranial hypertension after traumatic brain injury. J Trauma 2004; 57: 687–693 discussion 693–695. [DOI] [PubMed] [Google Scholar]
- 5.Scalea TM, Bochicchio GV, Habashi N, McCunn M, Shih D, McQuillan K, et al. Increased intra-abdominal, intrathoracic, and intracranial pressure after severe brain injury: multiple compartment syndrome. J Trauma 2007; 62: 647–656 discussion 656. [DOI] [PubMed] [Google Scholar]