Abstract
The Gram-negative Burkholderia mallei is a zoonotic pathogen and the causative agent of glanders disease. Because the bacteria maintain the potential to be used as a biothreat agent, vaccine strategies are required for human glanders prophylaxis. A rhesus macaque (Macaca mulatta) model of pneumonic (inhalational) glanders was established and the protective properties of a nanoparticle glycoconjugate vaccine composed of B. thailandensis LPS conjugated to FliC was evaluated. An aerosol challenge dose of ~1×104 CFU B. mallei produced mortality in 50% of naïve animals (n = 2/4), 2–3 days post-exposure. Although survival benefit was not observed by vaccination with a glycoconjugate glanders vaccine (p=0.42), serum LPS-specific IgG titres were significantly higher on day 80 in 3 vaccinated animals who survived compared with 3 vaccinated animals who died. Furthermore, B. mallei was isolated from multiple organs of both non-vaccinated survivors, but not from any organs of 3 vaccinated survivors at 30 days post-challenge. Taken together, this is the first time a candidate vaccine has been evaluated in a non-human primate aerosol model of glanders and represents the initial step for consideration in pre-clinical studies.
Keywords: Nanoparticles, glycoconjugate, glanders, macaques, Burkholderia mallei, aerosol
1. Introduction
Burkholderia mallei strains are the causative agent of glanders, an endemic disease in many parts of the world, including the Middle East and Asia [1]. B. mallei is primarily a disease of solipeds, but human infections have occurred sporadically among laboratory workers and those in direct contact with infected animals [2]. Although glanders has been eradicated from many parts of the world, the threat of B. mallei being used as a weapon is very real and it is considered one of the first biological warfare agents used in the 20th century [3]. Though human glanders case information is limited, and clinical symptoms in humans are often nonspecific, a clinical definition of human pulmonary glanders infection has been recently proposed [4]. Because current treatment for glanders includes acute parenteral treatment and a long-term oral eradicative antibiotic regimen that is associated with a number of side effects and poor adherence [4, 5], and the case fatality rate in acute cases is about 40% even with treatment [4, 5], the need for a prophylactic or therapeutic vaccine is critical.
Several strategies have been used to identify immunogenic antigens that can be included in the development of an effective glanders vaccine [6]. The B. mallei polysaccharides (e.g. lipopolysaccharide [LPS]) are important virulence factors and they are major targets of the immune response to infection, and often make excellent vaccines [7, 8]. Polysaccharides are often conjugated to proteins to enhance the immunogenicity of vaccines. For example, the B. pseudomallei LPS has been conjugated to proteins and passive transfer of LPS-specific antibody from immunized into naive mice provided protection against a subsequent challenge [9]. Further, a conjugate consisting of B. pseudomallei flagellin and O-antigen has been described [10]; this conjugate induced IgG responses and protection in diabetic rats.
Significant advances in nanotechnology have had a significant impact in vaccine development, particularly the use of solid nanoparticles that can be taken up by host cells [11, 12]. Gold nanoparticles (AuNPs) are promising candidates for various biological applications due to their unique physical properties (size and shape dependent), biocompatibility, ease of synthesis and bioconjugation, and their utility for vaccine design and delivery using diverse immunization routes [13]. For example, AuNPs have also been used widely for the epidermal delivery of DNA vaccines, eliciting humoral and cellular immune responses and becoming successful approaches to DNA vaccine delivery [14].
We have recently utilized AuNPs as components of a glycoconjugate vaccine against glanders [15]. AuNPs were covalently coupled with one of three different protein carriers (including flagellin protein FliC) followed by conjugation to LPS purified from a non-virulent B. thailandensis strain and tested for their protective capacity against B. mallei strain ATCC 23344 challenge in BALB/c mice. When we compared with LPS alone, the glycoconjugated LPS was found to generate significantly higher antibody titers, induced immunoglobulin class-switching, reduce bacterial burden and subsequently improve protection of mice against a lethal inhalation B. mallei challenge [15]. In this study we have evaluated the protective efficacy of a nanoparticle-linked glycoconjugate vaccine in a non-human primate aerosol model of glanders.
2. Materials and Methods
2.1 Nanoparticle synthesis and protein purification
AuNPs were synthesized as previously described [15]. Briefly, a colloidal solution of gold (III) chloride trihydrate and sodium citrate dihydrate was prepared and stored in the dark until use. Nanoparticle tracking analysis (NanoSight NS500) was used to determine the concentration of AuNPs. FliC (BPSL3319; amino acids 175 - 297) gene was amplified from B. pseudomallei genomic DNA by PCR and cloned in frame with an N-terminal tag (vector pET15b; Novagen) as previously described [15]. E. coli (λDE3) Rosetta harbouring the plasmid was cultured for 18–20 h prior to harvesting by centrifugation and sonication. Supernatant of the cell lysate was added to 1 mL of washed Ni2+-NTA agarose resin (Qiagen). The protein was released from the column with elution buffer (Lysis buffer [50 mM NaH2PO4, 300 mM NaCl, pH 8.0] containing 250 mM imidazole) through Poly-Prep chromatography columns (Bio-Rad) and further purified by size exclusion chromatography using a Hiload 16/60 Superdex 200 preparatory grade column (GE Healthcare). Protein concentration was calculated using the BCA assay.
2.2 LPS purification and antigen coupling to AuNPs
LPS was extracted from B. thailandensis E264 using a modified hot-phenol extraction method [15]. Briefly, bacteria were lysed and treated with DNase I, RNase I and Proteinase K, then 90% (w/v) aqueous phenol was added and the bacterial suspension heated to 70°C for 30 min. The mixture was dialyzed, the lyophilized sample digested with Proteinase K, and then ultracentrifuged at 100,000 × g for 3 h. The dry LPS was re-suspended in dH2O, aliquoted and the quality of the purified LPS verified using SDS-PAGE and silver-staining (Bio-Rad).
Recombinant carrier protein was immobilized onto AuNPs using carbodiimide chemistry using an AuNP suspension and 0.1 mM 16-mercaptohexadecanoic acid (MHDA) followed by 0.1% (v/v) Triton® X-100. The mixture was centrifuged and the pellet re-suspended in PBS prior to the addition of N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (Sigma), N-hydroxysuccinimide (Sigma), and 20 µg/mL of the carrier protein. The solution was incubated at room temperature for 2 h and after centrifugation; the conjugated AuNPs was re-suspended in PBS.
To make a 1 mL solution of AuNPs linked to LPS, the AuNPs coupled with a protein carrier of choice was suspended in potassium phosphate buffer (pH 7.5), followed by the addition of S-acetylthioglycolic acid N-hydroxysuccinimide ester (Sigma) [15]. Hydroxylamine and EDTA were then added to the AuNP solution to quench the reaction, centrifuged, and then re-suspended into the LPS solution for incubation at room temperature for 4 h. The conjugation reaction was quenched with 5 mM N-ethylmaleimide and the final nanoglycoconjugates re-suspended in PBS with or without 0.26% (w/v) alhydrogel. Glycoconjugate was quantified as previously described previously [15].
2.3 Animal use
Rhesus macaques (Macaca mulatta) of similar age (>3 yr) and weighing 3–6 kg, were used. Animals were housed in animal biosafety level 2 (immunization phase) and level 3 (challenge phase) facilities at the Tulane National Primate Research Center and were monitored throughout the study for physical health, food consumption, body weight, temperature, complete blood count, respiratory mechanics, and serum chemistry. Eight of the twelve animals were implanted with radiotelemetry devices and were continuously monitored for physiological changes in body temperature, heart rate and respiratory rate. The study was approved by the Institutional Animal Care and Use Committee at Tulane University, and all animals were handled in accordance with guidance from the American Association for Accreditation of Laboratory Animal Care.
2.4 Bacterial strain and bacterial preparation
B. mallei strain ATCC 23344 was obtained from BEI Resources (Manassas, VA, USA) and was grown overnight at 37°C in Luria-Bertani (LB) media containing 4% glycerol (LBG). 5.0 × 109 CFU/mL B. mallei aliquots of overnight growth were prepared and stored at −80°C. For aerosol exposures, a freshly grown stock of B. mallei was incubated in LBG for 18 h, then adjusted to approximately 5.0 × 109 CFU/mL for the challenge inoculum.
2.5 Aerosol exposure
A total of 12 macaques were used in the study. In the aerosol-exposure glanders model characterization (n=4) or in the vaccination study (6 vaccines and 6 controls) (Supplemental Fig. 1), anesthetized macaques were challenged with wild type B. mallei strain ATCC 23344 aerosols using a inhalation exposure system as described previously [16], and monitored for 30 days. In order to reduce the number of animals used in the study and to even up the vaccine and control groups, the NHPs used in the aerosol-exposure glanders model were included as negative control animals in the vaccination study. Inductive plethsymography, which measures the tidal volume of each individual animal per minute, was performed just before the exposure. Briefly, the animals were placed in a Class III BSC with the head only in a sealed exposure chamber. B. mallei inoculums in media were adjusted in the generator to the concentration appropriate to deliver the target dose. The B. mallei aerosols were generated directly in the head-only chamber using a Collision three jet-nebulizer (BGI Inc., Waltham, MA) with fully automated management control system (Biaera Technologies, Hagerstown, MD). Air samples were continuously obtained during the exposure and the bacterial concentrations of these samples were determined by culture for determination of aerosol concentration generated for each animal. Individual inhaled dose of B. mallei was calculated by multiplying the empirically determined aerosol exposure concentration (CFU/l air) in the chamber by volume of air estimated to have been breathed by the animal during the 10 minute exposure period. The LD50 dose was calculated from the average of inhaled CFU per animal.
2.6 Telemetry
Subcutaneous radiotelemetry transmitters combined with sensors capable of detecting biopotential signals of an electrocardiogram as well as thermistor type sensors capable of detecting temperature signals (T34G-8; Konigsberg Instruments [KI], Inc., Monrovia, CA) were surgically implanted, under aseptic conditions in eight of the twelve study animals several months prior to vaccination. Following surgical implantation, animals were housed in rooms and cages specifically designed with cage-mounted antennas (TR38-1FG; KI Inc.) configured to receive and transmit signals to a KI data acquisition base station. Telemetry data was continuously recorded using the Notocord-hem Acquisition System (Notocord Inc, Paris, France) and reported as hourly averages for 1-h observation intervals, with each animal serving as its own control. Baseline control data averages were generated from each subject for a minimum of 6 days prior to vaccination. Control data were aligned by the time of day over a 24-h period and averaged for hourly means to establish detection thresholds for each animal. These thresholds of detection of significant events were defined to be >1.5 times the maximum standard deviation of the control averages. Individual post-exposure data were then aligned by time and compared against control values for each animal. An assessment of fever (hyperthermia) hours and fever intensity was then performed for each animal.
2.7 Vaccine and vaccination
The AuNP glycoconjugate vaccine contained the FliC protein and the B. thailandensis LPS [15]. In this study, animals (n=6/group) were vaccinated with AuNP-LPS-FliC or PBS diluent, both containing 0.26% alhydrogel. All animals were vaccinated three times at 30 days intervals, receiving 20 µg of antigen in 400 µL subcutaneously in the upper deltoid and observed for signs of an adverse response after vaccination. Animals were bled on days 0, 10, 20, 30, 40, 50, 60, 70 and 80 days during vaccination and bronchoalveolar lavages (BALs) were performed at days 0 and 80. Following aerosol challenge, tissue samples were also collected from all animals either when they succumbed to infection or 30 days after challenge when the experiment was terminated.
2.8 Bacterial burden
Samples of BALs were plated on LBG and incubated at 37°C for 72 h to detect bacteria in the alveolar spaces. Tissue samples from the lung, liver, spleen, and bronchial lymph nodes were aseptically collected at necropsy and cultured for bacteria. Each tissue sample of approximately 0.25 to 1.0 g was homogenized and plated on LBG to quantify bacterial burden.
2.9 Gross pathology and histopathology
A full necropsy was performed on all animals by a board-certified veterinary pathologist. Lung, liver, spleen, and bronchial lymph nodes were collected from all NHPs, immersed in 10% neutral buffered formalin and submitted for histopathology. Tissue sections were trimmed at 5- to 6-µm thickness and stained with hematoxylin and eosin.
2.10 Antibody determination
Indirect ELISA was used to detect IgG antibodies against LPS and FliC in sera and BALs from both vaccinated and control animals. Titration analysis was performed to optimize the concentration of recombinant proteins and serum dilution to be used. An ELISA plate (Corning) was coated with 50µl of the antigens (0.5 µg/ml) in PBS overnight at 4°C. Plates were washed with PBS-Tween (pH 7.2) and blocked with 200 µl of 1% BSA for 2 h at 37°C. Sera were diluted 1:200 for LPS and 1:400 for FliC; BALs were diluted 1:8 and 1:4 for LPS and FliC, respectively, in PBS-T containing 0.1% BSA and incubated overnight at 4°C. Goat anti-monkey (IgG) antibodies conjugated to HRP (Fitzgerald), diluted 1:2,000, were added and incubated for 2 h at room temperature. ELISA was developed for 20 min with 50 µl/well of TMB microwell substrate (eBioscience) and following addition of 50 µl/well stop solution (1M H2SO4). A450 was determined.
3. Results and Discussion
3.1 Establishing inhalation glanders model in rhesus macaques
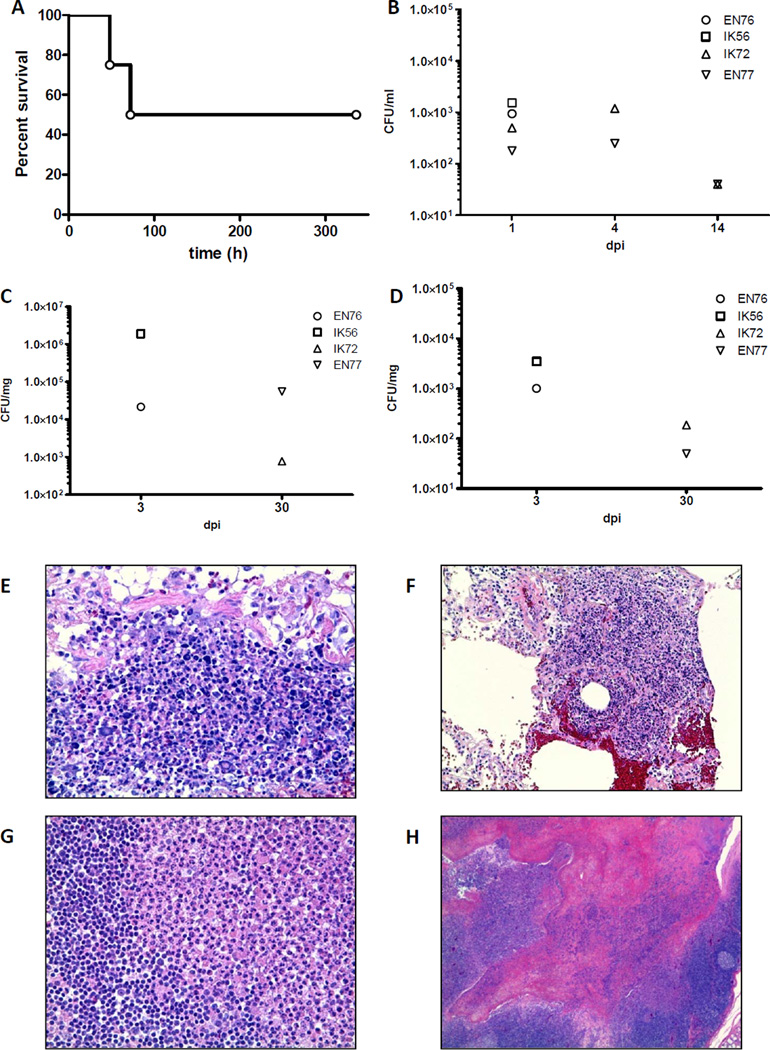
The inhalational glanders model in Rhesus macaques has not ever been reported so we began by determining the LD50 dose and characterizing the model in non-human primates (NHPs). Four Rhesus macaques were exposed to aerosolized B. mallei ATCC 23344 and the inhaled CFU dose per animal was calculated to be 1.4 × 104 ± 3.8 × 103. Half (2/4) NHPs became moribund and succumbed to infection between days 2–3 while the other two animals survived throughout all the 30-day observation period (Fig. 1A). All animals received a similar challenge dose (Supplemental Fig. 2) and displayed clinical signs of infection after day 2; however, two animals improved and survived the infection. Since we had 50% surviving rate at the end of this experiment, the LD50 could be approximated at 1.4 × 104 and subsequently served as a target challenge dose for our vaccine evaluation experiment.
Figure 1. Inhalation glanders NHP model.
(A) LD50 analysis of B. mallei ATCC 23344 in Rhesus macaques (n=4) infected via aerosol delivery, and with the percentage of survivals indicated. Bacterial burden in the bronchoalveolar lavage (B), lung (C) and spleen (D) is depicted. The symbols represent individual animals. Histological analysis of lungs (E and F), bronchial lymph nodes (G) and tonsil (H). Representative images of hematoxylin and eosin stained tissue sections from B. mallei-infected NHPs. Magnification 40x.
Because glanders commonly presents with fever, we monitored the progression of the febrile response utilizing biotelemetry and found it to be one of the primary indicators of disease and lethality (Supplemental Fig. 3). Non-surviving animals (EN76 and IK56) developed a sustained fever above control temperature within six hours of exposure and exhibited a complete loss of a natural diurnal rhythm. In contrast, the surviving animals (IK72 and EN77) displayed different episodes of fever; both early and through the course of the infection. The surviving animals, however, maintained a diurnal pattern of temperature changes. Blood parameters post-exposure were evaluated and in general, there was an increase in the blood parameters (RBC, WBC) early during infection and then a gradual decrease in animals that survived (data not shown).
To evaluate presence of B. mallei in the alveolar spaces, BALs cultures were performed at days 1, 4 and 14 post-infection. At day 1, the 4 NHPs showed ~ 1 × 103 CFU/mL and bacteria remained in the infected lungs of surviving animals (Fig. 1B). Additionally, quantitative bacterial cultures of the lungs, spleen, bronchial lymph nodes and liver were performed in the 2 non-surviving NHPs at day 3 post-infection and at day 30 in the surviving animals. The presence of B. mallei was detected in all the organs evaluated; however, organs from animals succumbing to infection had higher CFU counts than those from surviving animals (Fig 1C and D and data not shown).
Pulmonary lesions were the most common pathology finding in non-surviving NHPs. Gross examination of NHPs lungs demonstrated the presence of surface abscesses (data not shown). Foci of granuloma necrosis and granuloma hemorrhage were apparent in animals that became moribund 2–3 days post-infection (Fig. 1E and F). In the case of the surviving NHPs, bronchial lymph node abscesses were commonly observed (Fig. 1G). Interestingly, these animals displayed spleen sinusoids full of cells and tonsil crypt abscesses (Fig. 1H and data not shown), pathology which has been reported in human cases [4].
3.2 Evaluation of the protective properties of the AuNP glycoconjugate glanders vaccine
Next, we tested whether the AuNP glycoconjugate vaccine, which has been proven to be immunogenic and protective in the murine model [15], was effective in protecting NHP from aerosolized B. mallei. We used the AuNP-LPS-FliC vaccine because LPS O-antigen provides epitopes for the development of antigen-specific antibodies and the lipid A region is a potent agonist for TLR4 and evokes a strong immune response [17]. FliC, the structural flagellar protein, has a high affinity for TLR5 which plays a fundamental role in activating innate immunity [18]. Whilst B. mallei does not express a flagellum, and is therefore non- motile, it does contain the fliC gene [19]. Moreover, the addition of FliC as a protein carrier provides antigenic epitopes for recognition by CD4+ T cells to support B cell activation and differentiation [20].
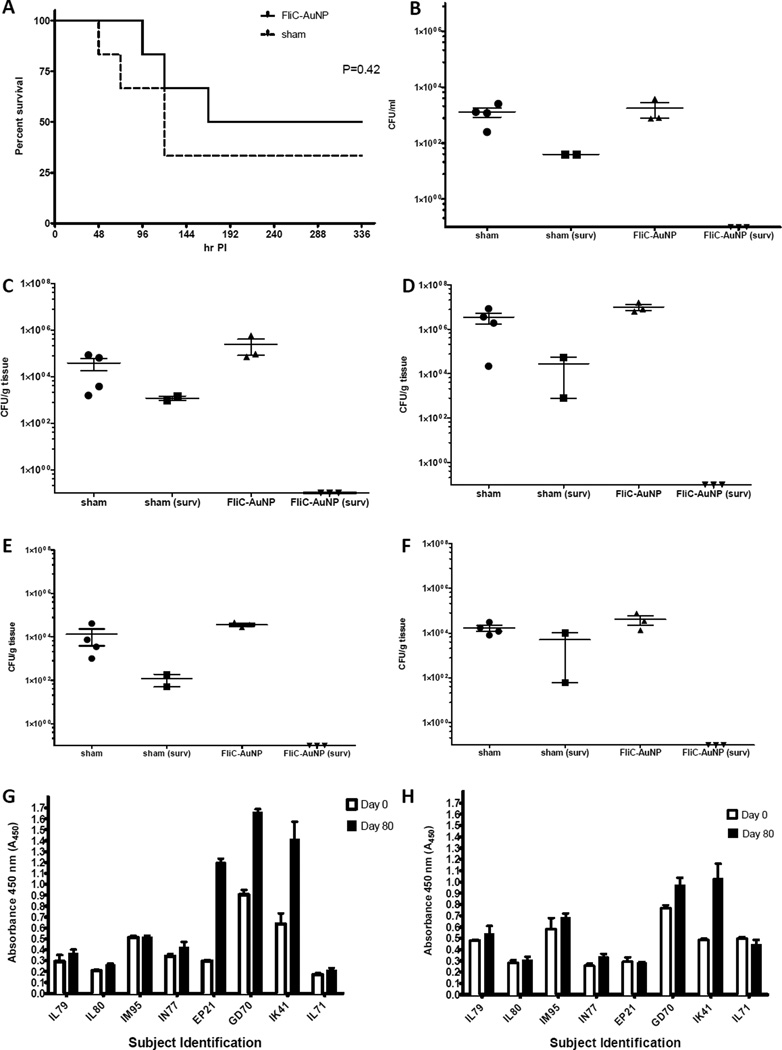
Two groups of rhesus macaques were prime and boosted vaccinated with either the AuNP glycoconjugate vaccine (n=6) or sham-vaccinated with an equivalent volume of filter-sterilized PBS (n=2). All animals were challenged with aerosolized B. mallei 30 days after final vaccine boost. Aerosolized animals received mean inhaled dose of 6.4×104 ± 4.3×104 CFU/animal. Because NHPs are exposed singly to the aerosolized bacteria and due to the individual variability of their respiratory function, experimental challenge doses tend to vary slightly from animal to animal. In this study, all doses were within acceptable range of our target dose (1.0×104 CFU/animal), with only one animal (IL79) receiving a lower dose than the target (Supplemental Fig. 2). Better protection (survival) was observed in the vaccinated group (3 survivors of a total of 6) as compared to the sham control (2/6), both sham-vaccinated controls (IL79 and IL80), succumbed on days 5 after exposure. However, the difference in overall survival was not significant by the log rank test (p=0.42) (Fig. 2A). Control group animals experienced higher temperature spikes initially and succumbed to infection between days 2–5. In contrast, the survivors of the vaccinated group showed milder fever initially with an additional later phase fever response while maintaining some diurnal pattern in recovery (data not shown). Vaccinee non-survivors exhibited similar initial fever patterns but ultimately succumbed to infection between days 4–6 post-challenge.
Figure 2. Protective properties of the nanoparticle glycoconjugate glanders vaccine.
(A) Survival of NHPs immunized with AuNP glycoconjugate vaccine or PBS and challenged with B. mallei ATCC 23344. Bacterial burden in the bronchoalveolar lavage (B), bronchial lymph nodes (C), lung (D), spleen (E) and liver (F) of vaccinated and sham NHPs. Anti-LPS (G) and anti-FliC (H) specific serum IgG at days 0 and 80 post-immunization. Groups of 6 NHPs received AuNP glycoconjugate vaccine or PBS, along with alhydrogel as adjuvant. The results are expressed as means ± the standard deviations (SD) of triplicate values.
Bacterial determination from BALs revealed a striking difference between the surviving sham and vaccinated animals. On day 80 post-challenge, approximately 1×102 CFU/mL of B. mallei were recovered from the surviving animals in the control group and approximately 1×103 CFU/mL were recovered from the 3 vaccinated animals that died, but no bacteria were detected in 3 vaccinated animals that survived (Fig. 2B). A post-mortem necropsy was performed on animals that succumbed to challenge during the 14-day post-challenge period. Microbiological examination revealed high numbers of B. mallei were isolated from the bronchial lymph nodes, lungs, spleens, and livers, of the seven animals (four sham and three vaccinated) that succumbed to infection (Fig. 2C-F), indicating that the death of animals was likely caused by systemic B. mallei infection. The survivors were humanely euthanized at the study endpoint (30 days post-challenge) and B. mallei was not detected in the organs of any of the vaccinated animals (EP21, GD70 and IK41), suggesting that the AuNP glycoconjugate vaccine protected surviving animals from disseminated infection (Fig. 2 C-F).
On day 80 post-challenge, serum LPS-specific IgG titers were significantly increased in the surviving glyconjugate vaccinated animals (EP21, GD70 and IK41) compared to the non- surviving glyconjugate vaccinated animals (IM95, IN77 and IL71) and the controls (IL79 and IL80) (Fig. 2G). The titers of FliC-specific serum IgG were increased in the majority of NHPs regardless of treatment, but they showed a trend for significance in vaccinated surviving NHPs GD70 and IK41 (Fig. 2H). In contrast, we did not observe any significant increase in the LPS-specific or FliC-specific BALs IgGs regardless of the treatment (data not shown). This is the first study to show a nanoparticle glycoconjugate vaccine to be immunogenic when delivered to NHPs prior to inhalational challenge with B. mallei and was effective to clear bacteria in surviving vaccinated NHPs These results provide important model development and proof-of-concept data for further evaluation of vaccines or other therapeutics against Burkholderia infections.
Supplementary Material
Supplemental Figure 1. Infection study time line. (A) LD50 analysis time line of B. mallei ATCC 23344 in Rhesus macaques (EN76, IK56, IK72 and EN77) infected via aerosol delivery over a 30 day period with bronchoalveolar lavage (BAL) measurements taken at days 1, 4 and 14 post-challenge. (B) Protection study time line including nanoparticle-linked glycoconjugate vaccines (IM95, IK41, IN77, EP21, GD70 and IL71) and control Rhesus macaques (IL79 and IL80). Serum and BAL collected at day 0 and 80 post immunisation. BAL also measured 14 days post challenge.
Supplemental Figure 2. Challenge doses (CFU/animal) comparisons of B. mallei after aerosol challenge during model development and vaccination experiment. Each solid circle and square represents the experimental CFU of each independent NHP. The triangles represent all animals combined and the range of dosing.
Supplemental Figure 3. Body temperature (°C) following exposure to B. mallei ATCC 23344 in survivors and non-survivors displayed as hour means for non-vaccinated [(A) EN76, (B) IK56, (C) IK72, and (D) EN77] and vaccinated [(E) IM95, (F) IK41, and (G) IN77)] animals. Control data (black) was plotted as mean ± SD in series for 24 h intervals and post challenge data (red) was overlaid to observe deviations from normal. Data points considered to be significant as defined by the detection thresholds (>1.5 times the maximum standard deviation of control data) were indicated as such with a green diamond in the plot. Data not available for animal IL71 due to implant hardware failure.
Acknowledgments
We thank Mardelle Susman for editorial support and Omar Qazi and Katherine Brown for providing the purified LPS. The study performed in the laboratories of AGT, RWT and CJR was supported by NIH/NIAID grant U54 AI057156. CJR was also supported in part through the NIH/OD grant OD-011104-51 (Tulane National Primate Research Center Base grant). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAID or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
None.
References
- 1.Whitlock GC, Estes DM, Torres AG. Glanders: off to the races with Burkholderia mallei. FEMS Microbiol Lett. 2007;277:115–122. doi: 10.1111/j.1574-6968.2007.00949.x. [DOI] [PubMed] [Google Scholar]
- 2.Galyov EE, Brett PJ, Deshazer D. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu Rev Microbiol. 2010;64:495–517. doi: 10.1146/annurev.micro.112408.134030. [DOI] [PubMed] [Google Scholar]
- 3.Wheelis M. First shots fired in biological warfare. Nature. 1998;395:213. doi: 10.1038/26089. [DOI] [PubMed] [Google Scholar]
- 4.Van Zandt KE, Greer MT, Gelhaus HC. Glanders: an overview of infection in humans. Orphanet J Rare Dis. 2013;8:131. doi: 10.1186/1750-1172-8-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipsitz R, et al. Workshop on Treatment of and Postexposure Prophylaxis for Burkholderia pseudomallei and B. mallei Infection, 2010. Em Infect Dis. 2012;18:e2. doi: 10.3201/eid1812.120638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva EB, Dow SW. Development of Burkholderia mallei and pseudomallei vaccines. Front Cell Infect Microbiol. 2013;3:10. doi: 10.3389/fcimb.2013.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burtnick MN, et al. Development of capsular polysaccharide-based glycoconjugates for immunization against melioidosis and glanders. Front Cell Infect Microbiol. 2012;2:108. doi: 10.3389/fcimb.2012.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qazi O, et al. Sero-characterization of lipopolysaccharide from Burkholderia thailandensis. Trans R Soc Trop Med Hyg. 2008;102:S58–S60. doi: 10.1016/S0035-9203(08)70016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson M, et al. Evaluation of lipopolysaccharide and capsular polysaccharide as subunit vaccines against experimental melioidosis. J Med Microbiol. 2004;53:1177–1182. doi: 10.1099/jmm.0.45766-0. [DOI] [PubMed] [Google Scholar]
- 10.Brett PJ, Woods DE. Structural and immunological characterization of Burkholderia pseudomallei O-polysaccharide-flagellin protein conjugates. Infect Immun. 1996;64:2824–2828. doi: 10.1128/iai.64.7.2824-2828.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnamachari Y, et al. Nanoparticle delivery systems in cancer vaccines. Pharm Res. 2011;28:215–236. doi: 10.1007/s11095-010-0241-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chithrani BD, Ghazani AA, Chan WCW. Determining the size and shape dependence of gold nanoparticle uptake into mammalian cells. Nano Lett. 2006;6:662–668. doi: 10.1021/nl052396o. [DOI] [PubMed] [Google Scholar]
- 13.Shah M, Badwaik VD, Dakshinamurthy R. Biological applications of gold nanoparticles. J Nanosci Nanotechnol. 2014;14:344–362. doi: 10.1166/jnn.2014.8900. [DOI] [PubMed] [Google Scholar]
- 14.Fuller DH, Loudon P, Schmaljohn C. Preclinical and clinical progress of particle mediated DNA vaccines for infectious diseases. Methods. 2006;40:86–97. doi: 10.1016/j.ymeth.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Gregory AE, et al. A gold nanoparticle-linked glycoconjugate vaccine against Burkholderia mallei. Nanomedicine. 2014 doi: 10.1016/j.nano.2014.08.005. Available online 3 September 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartings JM, Roy CJ. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol Methods. 2004;49:39–55. doi: 10.1016/j.vascn.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 17.West TE, et al. Activation of Toll-like receptors by Burkholderia pseudomallei. BMC Immunol. 2008;9:46. doi: 10.1186/1471-2172-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith KD, et al. Toll-like receptor 5 recognizes a conserved site on flagellin required for protofilament formation and bacterial motility. Nat Immunol. 2003;4:1247–1253. doi: 10.1038/ni1011. [DOI] [PubMed] [Google Scholar]
- 19.Sprague LD, et al. A possible pitfall in the identification of Burkholderia mallei using molecular identification systems based on the sequence of the flagellin fliC gene. FEMS Immunol Med Microbiol. 2002;34:231–236. doi: 10.1111/j.1574-695X.2002.tb00629.x. [DOI] [PubMed] [Google Scholar]
- 20.Bergman MA, et al. CD4+-T-cell responses generated during murine Salmonella enterica serovar Typhimurium infection are directed towards multiple epitopes within the natural antigen FliC. Infect Immun. 2005;73:7226–7235. doi: 10.1128/IAI.73.11.7226-7235.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Infection study time line. (A) LD50 analysis time line of B. mallei ATCC 23344 in Rhesus macaques (EN76, IK56, IK72 and EN77) infected via aerosol delivery over a 30 day period with bronchoalveolar lavage (BAL) measurements taken at days 1, 4 and 14 post-challenge. (B) Protection study time line including nanoparticle-linked glycoconjugate vaccines (IM95, IK41, IN77, EP21, GD70 and IL71) and control Rhesus macaques (IL79 and IL80). Serum and BAL collected at day 0 and 80 post immunisation. BAL also measured 14 days post challenge.
Supplemental Figure 2. Challenge doses (CFU/animal) comparisons of B. mallei after aerosol challenge during model development and vaccination experiment. Each solid circle and square represents the experimental CFU of each independent NHP. The triangles represent all animals combined and the range of dosing.
Supplemental Figure 3. Body temperature (°C) following exposure to B. mallei ATCC 23344 in survivors and non-survivors displayed as hour means for non-vaccinated [(A) EN76, (B) IK56, (C) IK72, and (D) EN77] and vaccinated [(E) IM95, (F) IK41, and (G) IN77)] animals. Control data (black) was plotted as mean ± SD in series for 24 h intervals and post challenge data (red) was overlaid to observe deviations from normal. Data points considered to be significant as defined by the detection thresholds (>1.5 times the maximum standard deviation of control data) were indicated as such with a green diamond in the plot. Data not available for animal IL71 due to implant hardware failure.