Abstract
Pediatric brain tumor (BT) survivors are at risk for psychosocial late effects across many domains of functioning, including neurocognitive and social. The literature on the social competence of pediatric BT survivors is still developing and future research is needed that integrates developmental and cognitive neuroscience research methodologies to identify predictors of survivor social adjustment and interventions to ameliorate problems. This review discusses the current literature on survivor social functioning through a model of social competence in childhood brain disorder and suggests future directions based on this model. Interventions pursuing change in survivor social adjustment should consider targeting social ecological factors.
Keywords: brain tumor, survivorship, late effects, social competence
From a psychosocial perspective, survivors of pediatric brain tumors (BT) are an understudied and vulnerable group. Medical advances have increased five-year survival rates for pediatric BTs from 54.8% in 1976 [1] to 72.1% in 2006 [2], but more effective therapies have increased risk for a multitude of neurodevelopmental late effects that significantly impact psychosocial adjustment. In addition to potential neurologic deficits [3] and disruptions to the endocrine system [4], pediatric BT survivors often experience neurocognitive late effects [5] and social difficulties with peers [6]. Notably, pediatric BT survivors have the poorest health-related quality of life (HRQOL) [7] compared to other childhood cancer survivors and attain developmental milestones of adulthood (e.g., marriage, living independently) at lower rates compared to controls [8, 9]. The foundation for these poor outcomes may lie in part in the difficulties with social competence that survivors experience in childhood [6]. Understanding the social competence of pediatric BT survivors can guide clinical and research efforts to reduce psychosocial late effects for this population.
Social competence generally refers to an individual’s ability to achieve personal goals through social interaction while simultaneously maintaining positive interpersonal relationships over time and across various contexts [10, 11]. Social competence is a developmental and transactional construct influenced by intra-individual factors and the social environment [12]. Theorists have proposed that social competence is comprised of three distinct factors: individual characteristics, social interactions and social adjustment [13, 14]. Individual characteristics include the child’s abilities that influence their behavior in social situations (e.g., social skills). Social interactions relates to characterizations of actual behavior with others while social adjustment refers to others’ and self-perceptions of the quality of a child’s social relationships and how well they attain socially desirable and developmentally appropriate goals [13, 14].
Research examining the social competence of pediatric BT survivors generally relies on self, parent or teacher ratings of one of the three components of social competence [15]. Parents and teachers rate survivor social skills using such measures as the Social Skills Rating System (SSRS) [16]. Social adjustment is typically measured through self, parent or teacher ratings using the Social Competence and Social Problems subscales of the widely-used Achenbach system of measures, including the Child Behavior Checklist (CBCL) [17]. Procedures for obtaining information on the social interactions and social adjustment of survivors directly from peers also have been employed [18]. Such methods involve soliciting nominations of children who fit different behavioral roles during social interactions (e.g., leader), examining reciprocated friendships or obtaining ratings of how much each child in a classroom is liked.
Survivor neuropsychological functioning is likely relevant to their social competence. Studies have documented neurocognitive late effects across multiple domains of functioning in pediatric BT survivors [5] and highlighted salient risk factors. A recent meta-analysis revealed medium-to-large effects sizes for deficits in overall intellectual functioning (IQ) [5], as well as large effect sizes for deficits in attention, verbal memory, and language [5]. Factors such as age at diagnosis [19, 20], tumor location [21–23] and the modality and toxicity of treatments [24] influence the type and severity of late effects. Cranial radiation [24, 25], particularly before the age of 8 [26–28], dramatically increases the risk for neurocognitive deficits due to disruptions in white matter volume development [19, 29]. While the occurrence of neurocognitive late effects is well established, less is known about how these difficulties affect functioning in other areas. For example, neurocognitive deficits may act as a mediator of poor survivor social adjustment.
The literature describing the social competence of pediatric BT survivors is still developing. In general, pediatric BT survivors experience increased social adjustment difficulties [6], including greater social isolation [18]. Most investigations are cross-sectional and reveal deficits in social adjustment when contrasted with other childhood cancer survivors [30–32], other chronic illness groups [33] and healthy controls [34]. Understanding the extent of social adjustment difficulties in pediatric BT survivors and the mechanisms for their social deficits is important given the long-term consequences of poor social adjustment in childhood [35, 36]. Children who are less accepted socially are at risk for both concurrent and later behavioral and emotional problems including substance abuse, academic difficulties, and poor psychological functioning [36, 37]. Given the importance of social adjustment to overall development [36] and the risk for poor psychosocial outcomes in adult survivors of pediatric BTs [8, 9], additional research is needed that examines predictors of problematic survivor social adjustment and potential interventions.
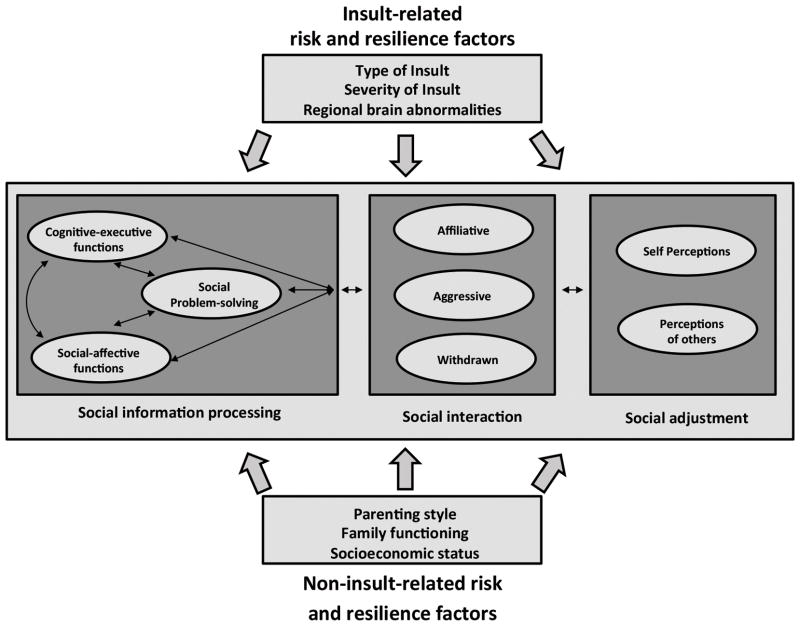
Research on survivor social competence could benefit from employing a framework that integrates insights gained from the developmental literature with social neuroscience to guide the focus of future studies. One model of social competence in children with brain disorder developed by Yeates and colleagues (Figure 1) [38] has direct applicability to pediatric BT survivors and offers a framework through which to conduct research on survivor social functioning. Research informed by this model could highlight key factors that influence survivor social adjustment and identify malleable intervention targets. The purpose of this review is to describe the key components of this model; critically review the existing literature on pediatric BT survivor social competence through the framework of the model; and offer directions for future research.
Figure 1.
A model of social competence in children with brain disorder [38].
Model of Social Competence in Childhood Brain Disorder
Yeates and colleagues’ [38] model of social competence is grounded in social neuroscience and developmental psychology and integrates risk and resilience factors associated with central nervous system (CNS) insults, the family environment, and characteristics of the individual child. Given that medical and family-systems factors have particular relevance to social, functional, and HRQOL outcomes in pediatric BT survivors [39], the model may be ideal for examining social outcomes within this survivor population. Associations in the model have been examined within pediatric traumatic brain injury (TBI), a group evidencing disturbances in social functioning [40].
The model specifies three components of social competence: social information processing (SIP), social interaction, and social adjustment [14, 41]. SIP consists of individual characteristics that impact social behavior and includes three sublevel components: social problem-solving, social-affective functions, and cognitive-executive functions. Social problem-solving reflects reasoning in social situations and includes interpreting cues, identifying goals and generating, selecting, and implementing responses to the situation [38]. Social-affective functioning includes things such as emotion regulation, pragmatic language, and appreciation of self and others’ mental states [42]. Studies within pediatric TBI highlight the impact of difficulties with social problem-solving [43] and social-affective functioning [44], including deficits in pragmatic language [45] and interpreting facial expressions [46].
The model presumes that optimal social-affective functions and successful implementation of social problem-solving skills are contingent upon intact neurocognitive abilities, namely aspects of executive function. Executive function refers to self-regulatory processes necessary for successful goal-directed problem-solving and includes planning, organization, attention regulation and working memory [47]. Previous research has demonstrated associations between executive function and social adjustment in both typically developing children [48] and a multitude of clinical populations [48–52]. Furthermore, evidence from social cognitive neuroscience suggests a significant overlap between the brain regions controlling cognitive-executive and SIP functions [38].
The quality of SIP abilities influences the nature of interactions with others. Children’s behaviors during social interactions generally are characterized as either affiliative, aggressive, or withdrawn [13]. Successful social interaction depends on a child’s recognition of the situational context and their interpersonal relationship with those involved [35]. Social adjustment refers to the appraisals of the effectiveness of a child’s social interactions and peer acceptance, which may vary depending upon whether they are rated by the self or others. This distinction is important, particularly when evaluating populations who may lack insight into the extent of their deficits [53].
The model [38] identifies different insult-related and non-insult-related risk and resiliency factors as moderating influences on social competence. These include endogenous (i.e., patient and disease-related) and exogenous (i.e., family systems, socioeconomic status) factors that affect children’s neurobehavioral functioning and social competence [40]. Consistent with social ecological theory [54], the model implicates distal (e.g., family socio-economic status) and proximal environmental factors (e.g., family functioning, parenting style) as having direct and moderating influences on social competence. Parental acceptance, family emotional expressiveness and general family functioning may influence children’s social competence [55–58]. Within the context of childhood brain disorder, family factors may either exacerbate the effects of insult or act as a buffer to the cognitive and social declines [42, 59].
Furthermore, these insult-related and non-insult related factors may interact with one another over time to influence social functioning outcomes [38]. For example, parents of children who experience TBI or cancer demonstrate increased distress [60–62], which may in-turn negatively influence the quality of the family environment and the child’s social adjustment [63]. Additionally, early brain insult may leave children more prone to environmental and family influences during the recovery process [59].
Although not depicted specifically in Figure 1, the authors of the model emphasize developmental considerations in describing the model’s components [38]. Normal developmental changes are associated with improvements in SIP abilities, increased complexity in social interactions and changes in parenting style [38]. Additionally, the timing of CNS insults in terms of a child’s developmental level is an important factor. Neurological dysfunction and acquired brain injury can disrupt normal brain development during critical periods, thereby impacting the development of SIP abilities [40]. The extent of the impact may depend on interacting elements including etiology; location and extent of tissue damage; and the age of disease onset or insult [64].
Application to Pediatric Brain Tumor
Yeates and colleagues’ [38] model offers an informative framework for understanding the social competence of childhood BT survivors [6]. The model is appropriate given the combined effects of the tumor and tumor-directed treatments on brain development [65]. Although, little research has examined predictors of survivor social adjustment, there are studies that can be viewed within this framework of social competence. For the purposes of this review, literature searches were conducted using PubMed and PsycINFO to identify relevant studies. The keywords “pediatric brain tumor,” “childhood brain tumor” and “CNS malignancies” were searched in combination with the following terms: social competence, social skills, social adjustment, social functioning, social problems, psychosocial adjustment, emotion, and neuropsychological functioning. Reference lists were checked for additional articles. Articles that were included for the current review met the following criteria: 1) published in English, 2) included pediatric BT participants, 3) presented novel data on social functioning (i.e., not a review paper). Articles presenting data from social skills interventions were not included. A total of 30 articles were identified and 24 of those met the inclusion criteria. Those studies are summarized in Table I.
Table I.
Summary of Studies on the Social Competence of Pediatric Brain Tumor Survivors.
| Study | Purpose | Study design | Sample | Measures | Results |
|---|---|---|---|---|---|
| Aarsen et al [79] | Document functional outcomes of survivors of low-grade astrocytomas | Cross-sectional study; assessed survivors 3–11 years post diagnosis | 38 survivors of low-grade astrocytomas | Child Behavior Checklist, Teacher Report Form, Youth Self Report | Infratentorial tumors related to more teacher-reported social problems; tumor recurrences related to more self-reported social problems |
| Armstrong et al [82] | Describe associations between region-specific radiation dose and self-reported neuropsychological and social outcomes | Retrospective cohort study -Childhood Cancer Survivorship Study (CCSS) | 818 CCSS participants with CNS malignancies | Short-Form 36 Social Functioning subscale (2 items that assess extent physical or emotional health problems interfere with social activities) | Radiation to temporal region associated with significantly more health-related disruptions in social activities per self-report |
| Barrera et al [75] | Compare social outcomes of childhood cancer survivors with controls | Retrospective, cohort study | 800 survivors of childhood cancer (122 CNS tumors) age 6–16 and 923 controls | Child Behavior Checklist, Ontario Child Health Survey | BT survivors more likely than controls to have no close friends; cranial radiation increased risk for having no friends |
| Bonner et al [33] | Assess social functioning and facial expression recognition skills of BT survivors compared to children with juvenile rheumatoid arthritis (JRA) | Cross-sectional | 51 survivors of BT and 31 children with JRA ages 6–17 | Child Behavior Checklist, Diagnostic Analysis of Nonverbal Accuracy – Revised, Social Skills Rating System; Wechsler Intelligence Scale for Children – 3rd edition | BT group worse social functioning and made more errors reading adult facial expressions after controlling for IQ; poorer facial recognition and younger age at diagnosis associated with worse parent-rated social adjustment |
| Brinkman et al [80] | Examine longitudinal parent-reported social outcomes among children treated for embryonal BTs | Longitudinal; parents completed measures at diagnosis and yearly for 5 years | 220 youth diagnosed with embryonal BT (ages 5–21 at diagnosis); categorized into high-risk and average-risk groups | Child Behavior Checklist, Woodcock Johnson Test of Cognitive Abilities | Parent-reported social problems increased at greater rate over time for high-risk group compared to average risk group; posterior fossa syndrome increased risk for social problems over time; better IQ associated with better social functioning over time |
| Carey et al [84] | Examine whether BT survivors evidence nonverbal learning disability and examine associations between neuropsychological and social functioning | Cross-sectional | 15 childhood BT survivors, ages 8–12 | Beery Developmental Test of Visual-Motor Integration – 4th edition, Child Behavior Checklist, Grooved Pegboard Test, NEPSY subtests, Social Skills Rating System, Teacher Report Form, Wechsler Intelligence Scale for Children – 3rd edition, Youth Self-Report | Survivors had significantly higher parent-reported social problems compared to norms; nonsignificant trend for poorer nonverbal neuropsychological abilities being related to more parent-reported social problems |
| Carlson-Green et al [83] | Examine contextual factors associated with behavioral and neurocognitive outcomes over time | Longitudinal; family data obtained at diagnosis and child data from approximately 24 months later | 63 children treated for BT, ages 2–6 at diagnosis | Child Behavior Checklist, Coping Health Inventory for Parents, Family Environment Scale, Family Inventory of Life Events, Stanford-Binet Intelligence Scale – Fourth Edition, Vineland Adaptive Behavior Scale | Higher family socio-economic status at diagnosis associated with better parent-rated survivor adaptive functioning |
| Carpentieri et al [31] | Compare social adjustment of BT survivors with non-CNS cancer survivors; examine changes in social adjustment over time | Cross-sectional comparison of two survivor group; longitudinal examination of BT group data | 40 BT survivors and 40 non-CNS cancer survivors, ages 4–16 | Child Behavior Checklist, Rating of cosmetic and functional impairment, Wechsler Intelligence Scale for Children – Revised | BT group had worse parent-rated social adjustment compared to non-CNS cancer group; BT group demonstrated increases in parent-rated social problems over time; children with abnormal brain volume and non-third ventricle tumor have more social problems |
| Carpentieri et al [91] | Describe psychosocial functioning of adolescent survivors of childhood BT | Cross-sectional | 32 BT survivors, ages 12–18 | Behavior Assessment System for Children – 2nd edition – self, parent and teacher report | No difficulties related to social skills or interpersonal relationships reported across raters |
| Foley et al [78] | Compare adjustment in children with hypothalamic BTs to other BT group; examine associations between family functioning and survivor adjustment | Cross-sectional | 29 children treated for hypothalamic BT and 29 children treated for other types of BT; both groups off treatment at least 6 months | Child Behavior Checklist, McMaster Family Assessment Device | Combined sample had more parent-rated social problems compared to normative sample; in combined sample, younger age at diagnosis related to more parent-rated social problems |
| Hardy et al [76] | Examine and compare social outcomes of children with BTs both on and off therapy | Cross-sectional | 15 children with BT on treatment and 15 children with BT ≥ 6 months post-treatment, ages 7–16 | Child Behavior Checklist, Harter’s Self-Perception Profile for Children, Wechsler Scale of Intelligence – 3rd edition | No difference between groups on parent-ratings of survivor social adjustment; off-therapy participants self-reported lower social acceptance; lower self-reported social acceptance related to more parent-rated problems with aggression, depression and somatization |
| Holmquist et al [71] | Investigate emotional and behavioral outcomes of pediatric BT survivors | Cross-sectional | 54 survivors of childhood BT, mean age of 10, approximately 3 years off treatment | California Verbal Learning Test – Children’s edition, Child Behavior Checklist, Conners’ Rating Scales – Revised, Wechsler Intelligence Scale for Children – 3rd edition | Lower IQ related to increased parent-rated social problems; poor verbal learning related to parent-rated social withdrawal |
| Kullgren et al [70] | Examine long-term social outcomes in pediatric BT survivors | Longitudinal – first time point 1–2 years after diagnosis and second time point 3–4 years after diagnosis | 40 survivors of childhood BT, age 4–16 at Time 1 | Child Behavior Checklist, Family Life Inventory of Life Events, Stanford-Binet Intelligence Scale – 4th edition, Vineland Adaptive Behavior Scales | Survivors demonstrate poor parent-rated social adjustment over time; lower IQ predictive of more parent-rated social problems over time; higher number of treatment modalities and low family socio-economic status predictive of more parent-rated social problems over time |
| Long et al [92] | Examine pediatric BT survivor perceptions of interactions with peers at school | Cross-sectional | 22 BT survivors and 22 healthy comparisons, ages 8–18 | School Experiences Questionnaire (developed for study) | No differences in self-reported perceptions of peer interactions between groups |
| Moyer et al [66] | Examine impact of survivor attentional abilities on social functioning in ALL and BT survivors | Cross-sectional | 211 BT survivors and 258 ALL survivors, ages 6–19 | Conners’ Rating Scales – revised short version, Social Skills Rating System, Wechsler Intelligence Scale for Children – 3rd edition or Wechsler Adult Intelligence Scale – 3rd edition | More parent-and teacher-reported attention problems associated with more parent-reported social problems; female gender, lower IQ and parent-rated attention problems predicted more parent-reported social problems |
| Mulhern et al [68] | Compare adjustment of children with BT with non-CNS cancers and examine predictors of adjustment | Cross-sectional | 81 children with recently diagnosed BT and 31 children with recently diagnosed non-CNS cancers, ages 4–16 | Child Behavior Checklist, rating of cosmetic and functional impairment, Wechsler Intelligence Scale for Children – Revised | Lower IQ related to less participation in social activities; single-parent status and severe functional impairment related to more parent-rated social problems |
| Patel et al [72] | Examine attention dysfunction in pediatric BT survivors | Cross-sectional | 70 pediatric BT survivors, ages 6–16 | California Verbal Learning Test for Children, Child Behavior Checklist, Trails Making Test A and B, Wechsler Intelligence Scale for Children – 3rd edition | Survivors characterized as having attention dysfunction had more parent-reported social problems than non-attention dysfunction survivors |
| Poggi et al [67] | Evaluate presence of cognitive and psychological disorders in pediatric BT survivors | Cross-sectional | 76 pediatric BT survivors, ages 0–18 | Child Behavior Checklist, Vineland Adaptive Behavior Scales, age appropriate Wechsler Intelligence Scales | Greater time since diagnosis related to worse parent-rated social skills; lower IQ related to more parent-reported social problems |
| Schulte et al [69] | Examine associations between body mass index, cognitive functioning and social competence in childhood BT survivors | Cross-sectional | 54 survivors of childhood BTs, ages 8–18 | Child Behavior Checklist, Social Skills Rating System, Self-Perception Profile, Wechsler Abbreviated Scale of Intelligence, Youth Self-Report | Higher BMI and higher IQ related to better parent-reported social competence; IQ moderated effect of BMI in predicting self-perceptions of close friendships – survivors with lower BMI and lower IQ had lower self-perceptions of close friendships |
| Vannatta et al [18] | Examine behavioral reputation and peer acceptance of childhood BT survivors | Cross-sectional; data collected from survivors, teachers and peers | 28 childhood BT survivors and 28 nonchronically ill, same classroom, same gender comparison peers, ages 8–18 | Likert Rating Scale (of all children in class), Revised Class Play, Three Best Friends | BT survivors described by peer, teacher and self-reports as more socially isolated than comparisons; BT survivors selected as best friend less often than comparisons; no differences on reciprocated friendships or like ratings between groups; peers perceived BT survivors as being more sick, more fatigued and often absent |
| Willard et al [77] | Examine emotional, behavioral and neurocognitive functioning in ependymoma survivors over time | Longitudinal; data presented from pre-radiation baseline evaluation and 5 years later | 113 youth treated for pediatric ependymoma using conformal radiation therapy, age 1–16 at baseline | Child Behavior Checklist, age appropriate Wechsler Intelligence Scales | Parent-rated survivor social competence significantly differed from norms at Year 5 but not at baseline; no significant change in parent ratings of survivor social competence over time |
| Willard et al [73] | Examine relation between gender, history of cranial radiation therapy and facial expression recognition in pediatric BT survivors | Cross-sectional | 53 pediatric BT survivors (27 females), ages 6–17; 34 survivors received cranial radiation therapy | Diagnostic Analysis of Nonverbal Accuracy – Revised, Social Skills Rating System, Wechsler Intelligence Scale for Children – 3rd edition | Interaction between gender and history of cranial radiation therapy on facial expression recognition – females with history of cranial radiation therapy performed more poorly than females without history of cranial radiation therapy |
| Wolfe et al [49] | Examine associations between executive function and social skills in pediatric BT survivors | Cross-sectional | 24 pediatric BT survivors, ages 8–18 | Behavior Rating Inventory of Executive Function, Social Skills Information System, Tasks of Executive Control, Wechsler Abbreviated Scale of Intelligence or Wechsler Intelligence Scale for Children – 4th edition | Poorer parent-rated survivor executive function was related to poorer parent-rated survivor social skills but not survivor self-reported social skills; lower levels of response inconsistency on executive function task related to poorer parent-and survivor-reported social skills; greater variability in response style on task predicted both parent-and survivor-reported social skills while controlling for IQ |
| Wolfe-Christensen et al [81] | Assess if posterior fossa syndrome is associated with increased risk for social problems in pediatric BT survivors | Cross-sectional | 21 pediatric BT survivors, ages 6–17; 6 of 21 had posterior fossa syndrome | Child Behavior Checklist, Conners Rating Scale-93 | Posterior fossa syndrome associated with increased risk in parent-reported survivor social problems |
Social Information Processing
Studies examining the components of SIP in childhood BT survivors have largely focused on their neurocognitive functioning rather than social problem-solving or social-affective functioning. Across a range of studies, lower IQ has been shown to predict poorer parent-rated social skills [66, 67], engagement in fewer activities [68], a self-perception of fewer close friends [69] and increased parent-rated social adjustment problems [67, 70, 71].
The associations between specific domains of neurocognitive functioning and survivor social functioning also have been investigated. Difficulties with verbal learning have been associated with increased parent-rated social withdrawal [71]. Two studies have demonstrated associations between survivor attentional dysfunction and poorer parent-rated social functioning [66, 72]. Another study examined the associations between self- and parent-rated survivor social skills and survivor executive function in 24 survivors [49]. After controlling for IQ, survivor performance on executive function tasks predicted both self- and parent-ratings of survivor social skills. Additionally, parent ratings of survivor executive function significantly predicted parent ratings of survivor social skills independent of survivor IQ [49]. Notably, the role of processing speed has not been examined in survivors’ social functioning. Survivors who take more time to process information and respond in social situations may be at risk for poorer social interactions and decreased peer acceptance.
The social problem-solving and social-affective functioning of childhood BT survivors have received little empirical examination. Compared to children with juvenile rheumatoid arthritis, survivors of pediatric BT demonstrate more difficulties recognizing out-of-context adult facial expressions after controlling for IQ [33, 73]. Furthermore, poorer facial recognition abilities have been associated with increased parent-reported social adjustment problems [33]. The social problem-solving abilities of survivors have been examined within the context of a social skills intervention [74] but have not been compared to controls or examined in terms of their associations with other processes or outcomes.
Social Interaction and Social Adjustment
Studies examining the social interactions and social adjustment of pediatric BT survivors generally show problems when compared to controls. A large, cross-sectional study of childhood cancer survivors revealed that parents of pediatric BT survivors reported that survivors were significantly more likely than comparisons without a chronic illness to not have any close friends and less likely to use friends as confidants [75]. Furthermore, compared to comparisons without a chronic illness, pediatric BT survivors are less accepted socially by their peers and teacher-, peer- and self-reports indicate greater social isolation[18]. Additionally, children with BTs who are rated by their parents as having behavioral or emotional difficulties, self-report worse social acceptance [76].
Longitudinal studies on survivor social adjustment offer mixed findings. One study found relatively stable, normal social functioning over a 5-year period [77] while another showed stable, poor survivor social adjustment over a three-to-four year period [70]. However, another study reported increased social problems two-to-three years after diagnosis [31]. A potential reason for the equivocal findings is the reliance on parent ratings of survivor social adjustment.
Insult-Related Risk and Resilience Factors
A limited number of insult-related risk factors have been examined in terms of their associations with survivor social competence. In general, younger age at diagnosis has been related to poorer parent-rated social competence [33, 78] and greater functional and neurocognitive deficits, which, in turn, limit engagement in social activities [78]. Additionally, children with abnormal brain volume, infratentorial tumors, and tumors outside the third ventricle demonstrate poorer social adjustment [31, 68, 79].
Several other disease and treatment-related elements have been associated with survivor social competence. Treatment-related cosmetic disfigurements, neurological impairments that impact activities of daily living (e.g., posterior fossa syndrome), lower survivor body mass index, and missed school for medical care all increase the risk of parent-rated survivor social adjustment problems [31, 68, 69, 80, 81]. Furthermore, tumor recurrence [79], greater time since diagnosis, [67] and treatment with cranial or cranio-spinal radiation [33, 73] are associated with poorer parent-rated social adjustment. Among long-term survivors with CNS malignancies from the Childhood Cancer Survivorship Study (CCSS), those who received radiation to the temporal region of the brain reported more disruptions in social activities due to health or emotional problems [82]. Two prospective studies showed that increased tumor risk status [80] and higher number of treatment modalities [70] are associated with poorer parent-rated survivor social functioning over time.
Non-Insult-Related Risk and Resilience Factors
Little research has examined non-insult-related risk and resilience factors contributing to social competence in pediatric BT survivors. Family environment factors, such as single-parent status[68] and low socio-economic status [68, 70, 83], have been related to poorer parent-rated survivor social adjustment. This suggests that family variables may act as moderators to survivor social outcomes but additional research is needed.
Conclusions & Future Directions
The model of social competence in children with brain disorder [38] holds significant promise as a framework for understanding the social functioning deficits observed in pediatric BT survivors. This model has demonstrated utility within childhood TBI and is relevant to childhood BT survivorship. Given the improved survival rates for childhood BTs and the increased emphasis on HRQOL, additional research is warranted that focuses on the social functioning of childhood BT survivors. Studies that seek to identify predictors of social adjustment are needed and the presented model of social competence offers specific domains to explore. Notably, research that examines the social-affective functioning and social problem-solving of survivors, as well as the role of families in influencing the components of social competence are essential next steps. In addition to providing a greater knowledge base on the social competence of pediatric BT survivors, studies that examine the associations between model components will help to evaluate the utility of this model in this population and determine whether or not the model should be modified to better reflect pediatric BT survivorship.
This review has underscored the current status of investigation into survivor social competence and highlighted directions for future research. Existing studies on the associations between survivor neurocognitive functioning and social functioning generally suggest that impairments in IQ, attention regulation, and executive function are associated with aspects of parent-rated social functioning [49, 66–70, 72]. While these studies implicate neurocognitive functioning in survivor social functioning, they generally focus on global intelligence and do not adequately examine how specific domains of neurocognitive functioning influence other aspects of SIP, social interactions, or social adjustment. Only five studies explored how aspects of neurocognitive functioning relate to social functioning [49, 66, 71, 72, 84] and one of those studies include survivors of acute lymphoblastic leukemia along with BT survivors [66]. Of the studies examining attention regulation and social functioning, only one incorporated objective, performance-based measures of attention regulation [72]. Furthermore, although the study on survivor executive functioning and social skills presents innovative data, it is limited by its small sample size [49]. Additional studies are needed with larger samples that incorporate more rigorous, varied approaches to measuring different neurocognitive domains in order to establish associations between these abilities and the other components of social competence, including peer ratings of survivor social adjustment.
Given the paucity of research on the social-affective functioning and social problem-solving abilities of childhood BT survivors, few conclusions can be made about their contributions to survivor outcomes. Clearly additional research is needed in this area. The lack of a standard way to measure social-affective functioning and social problem-solving is an important limitation that could impact future research. Current approaches to assessing social problem-solving involve asking children how they would respond to hypothetical social dilemmas and have arisen out of research on children with behavioral disorders [85]. Although some attempts have been made to modify these approaches to adequately reflect the difficulties experienced by pediatric BT survivors [74], additional work is needed to develop sound measures of social problem-solving and other SIP components.
While there are some studies linking insult-related and non-insult-related risk and resilience factors to social competence, the evidence on these associations could be greatly enhanced by adding measures of social functioning and family variables to ongoing clinical trials. Many of these clinical trials compare different treatment modalities and evaluate the neuropsychological functioning of those enrolled. Incorporating measures of social functioning and family functioning into these protocols could advance the field’s understanding of the associations between tumor-directed treatments, neuropsychological functioning, family functioning, and survivor social outcomes. In particular, variables such as family functioning, family management of survivor late effects, and parenting style need additional study in order to identify potential malleable intervention targets and enhance outcomes.
Future research also should address two other significant weaknesses of the current literature on survivor social competence. First, only one published study has obtained peer reports on survivor social functioning [18] with the rest relying on parent- and teacher-reports. This is problematic in that peer nomination data are reliable and predict future functioning and generally have low correlations with parent- and teacher-reports of children’s social adjustment [86]. Obtaining peer report data in future research also could further our understanding of the scope of survivor social adjustment difficulties and serve as a robust indicator of the impact of interventions.
Second, the studies on survivor social competence mostly have been cross-sectional with few studies offering longitudinal data [31, 70, 77, 80, 83]. Prior longitudinal studies generally only report parent ratings of survivor social adjustment. Little is known about how the components of survivor SIP change over time and how changes in the different aspects of SIP influence changes in social adjustment. Such longitudinal research could clarify the role of moderating and mediating variables in contributing to survivor social outcomes. Additionally, prospective studies of survivor social competence could identify critical developmental periods (e.g., transition to adolescence) where the importance of certain factors (e.g., improved attentional functioning) may be more essential to successful social interactions and adjustment.
The research needed to enhance our understanding of survivor social functioning and the mechanisms that influence social adjustment has the potential to improve survivor social outcomes. Research conducted within this framework of social competence could be instrumental in intervention development. For example, studies that demonstrate that positive changes in survivor social problem-solving or family functioning over time lead to improvements in survivor social adjustment could guide the development of interventions that target those variables to improve survivor social functioning. Research examining the impact of social skills interventions for pediatric BT survivors has demonstrated a modest impact on survivor social performance [74] and social adjustment [87, 88]. Further work is needed to determine whether adapting existing intervention approaches could improve survivor social outcomes. Specifically, family-based interventions that address family management of neurobehavioral sequelae in pediatric TBI [89] or school-based interventions that seek to change peer perceptions of children with autism spectrum disorders [90] could be adapted for pediatric BT survivors to improve social functioning outcomes.
Acknowledgments
The preparation of this article was supported in part by Grants 1K07CA178100-01 and 1R03CA162970-01A1 to Matthew C. Hocking.
References
- 1.Ries LAG, et al. SEER Cancer Statistics Review, 1973–1999. 2002 [cited 2010 December 21]; Available from: http://seer.cancer.gov/csr/1973_1999/
- 2.CBTRUS. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004–2006. 2010 doi: 10.1093/neuonc/not151. [cited 2010 December 20]; Available from: www.cbtrus.org. [DOI] [PMC free article] [PubMed]
- 3.Packer RJ, et al. Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2003;21:3255–3261. doi: 10.1200/JCO.2003.01.202. [DOI] [PubMed] [Google Scholar]
- 4.Gurney JG, et al. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer. 2003;97:663–673. doi: 10.1002/cncr.11095. [DOI] [PubMed] [Google Scholar]
- 5.Robinson KE, et al. A quantitative meta-analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatric Blood and Cancer. 2010;55:525–531. doi: 10.1002/pbc.22568. [DOI] [PubMed] [Google Scholar]
- 6.Schulte F, Barrera M. Social competence in childhood brain tumor survivors: a comprehensive review. Supportive Care in Cancer. 2009;18:1499–1513. doi: 10.1007/s00520-010-0963-1. [DOI] [PubMed] [Google Scholar]
- 7.Zeltzer L, et al. Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2009;27:2396–2404. doi: 10.1200/JCO.2008.21.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ness KK, et al. Physical performance limitations among adult survivors of childhood brain tumors. Cancer. 2010;116:3034–3044. doi: 10.1002/cncr.25051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zebrack B, et al. Psychological outcomes in long-term survivors of childhood brain cancer: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2004;22:999–1006. doi: 10.1200/JCO.2004.06.148. [DOI] [PubMed] [Google Scholar]
- 10.Rubin KH, Rose-Krasnor L. Interpersonal problem-solving. In: Van Hassett VB, Hersen M, editors. Handbook of Social Development. Plenum; New York: 1992. pp. 283–323. [Google Scholar]
- 11.Bukowski WM, Rubin KH, Parker J. Social competence. In: Smelser NJ, Baltes PB, editors. International encyclopedia of social and behavioral sciences. Elsevier; Oxford, England: 2001. pp. 14258–14264. [Google Scholar]
- 12.Rubin KH, Krasnor LR. Social-cognitive and social behavioral perspectives on problem solving. In: Perlmutter M, editor. Cognitive perspectives on children’s social and behavioral development: The Minnesota Symposia on child psychology. Erlbaum; Hillsdale, NJ: 1986. pp. 1–68. [Google Scholar]
- 13.Rubin KH, Bukowski WM, Parker J. Peer interactions, relationships, and groups. In: Eisenberg N, editor. Handbook of Child Psychology: Social, Emotional, and Personality Development (6th Edition) Wiley; New York: 2006. pp. 571–645. [Google Scholar]
- 14.Nassau JH, Drotar D. Social competence among children with central nervous system-related chronic health conditions: A review. Journal of Pediatric Psychology. 1997;22:771–793. doi: 10.1093/jpepsy/22.6.771. [DOI] [PubMed] [Google Scholar]
- 15.Schulte F, Barrera M. Social competence in pediatric brain tumor survivors: evaluating the psychometric properties of assessment tools. Supportive Care in Cancer. 2014;22:561–569. doi: 10.1007/s00520-013-2035-9. [DOI] [PubMed] [Google Scholar]
- 16.Gresham FM, Elliott SN. Social Skills Rating System. Circle Pines: American Guidance Service; 1990. [Google Scholar]
- 17.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 18.Vannatta K, et al. A controlled study of peer relationships of children surviving brain tumors: Teacher, peer, and self ratings. Journal of Pediatric Psychology. 1998;23:279–287. doi: 10.1093/jpepsy/23.5.279. [DOI] [PubMed] [Google Scholar]
- 19.Mulhern RK, et al. Risks of young age for selected neurocognitive deficits in medulloblastoma are associated with white matter loss. Journal of Clinical Oncology. 2001;19:472–479. doi: 10.1200/JCO.2001.19.2.472. [DOI] [PubMed] [Google Scholar]
- 20.Sands SA, et al. Long-term quality of life and neuropsychologic functioning for patients with CNS germ-cell tumors: From the First International Germ-Cell Tumor Study. Neuro-Oncology. 2001;3:175–183. doi: 10.1093/neuonc/3.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.King TZ, et al. Verbal memory abilities of children with brain tumors. Child Neuropsychology. 2004;10:76–88. doi: 10.1080/09297040490911096. [DOI] [PubMed] [Google Scholar]
- 22.Mulhern RK, et al. Neuropsychological status of children treated for brain tumors: A critical review and integrative analysis. Medical and Pediatric Oncology. 1992;20:181–191. doi: 10.1002/mpo.2950200302. [DOI] [PubMed] [Google Scholar]
- 23.Papazoglou A, et al. Cognitive predictors of adaptive functioning vary according to pediatric brain tumor location. Developmental Neuropsychology. 2008;33:505–520. doi: 10.1080/87565640802101490. [DOI] [PubMed] [Google Scholar]
- 24.Turner CD, et al. Late effects of therapy for pediatric brain tumor survivors. Journal of Child Neurology. 2009;24:1455–1463. doi: 10.1177/0883073809341709. [DOI] [PubMed] [Google Scholar]
- 25.de Ruiter MA, et al. Neurocognitive consequences of a paediatric brain tumour and its treatment: a meta-analysis. Developmental Medicine & Child Neurology. 2013;55:408–417. doi: 10.1111/dmcn.12020. [DOI] [PubMed] [Google Scholar]
- 26.Radcliffe J, et al. Cognitive deficits in long-term survivors of childhood medulloblastoma and other noncortical tumors: Age-dependent effects of whole brain radiation. International Journal of Developmental Neuroscience. 1994;12:327–334. doi: 10.1016/0736-5748(94)90081-7. [DOI] [PubMed] [Google Scholar]
- 27.Ris MD, et al. Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: A Children’s Cancer Group study. Journal of Clinical Oncology. 2001;19:3470–3476. doi: 10.1200/JCO.2001.19.15.3470. [DOI] [PubMed] [Google Scholar]
- 28.Robinson KE, et al. Neurocognitive late effects of pediatric brain tumors of the posterior fossa: A quantitative review. Journal of the International Neuropsychological Society. 2013;19:1–10. doi: 10.1017/S1355617712000987. [DOI] [PubMed] [Google Scholar]
- 29.Mulhern RK, et al. Neurocognitive deficits in medulloblastoma survivors and white matter loss. Annals of Neurology. 1999;46:834–841. doi: 10.1002/1531-8249(199912)46:6<834::aid-ana5>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 30.Armstrong FD, et al. The Miami Pediatric Quality of Life Questionnaire: Parent scale. International Journal of Cancer. 1999;(Suppl 12):11–17. doi: 10.1002/(sici)1097-0215(1999)83:12+<11::aid-ijc4>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 31.Carpentieri SC, et al. Behavioral resiliency among children surviving brain tumors: a longitudinal study. Journal of Clinical Child Psychology. 1993;22:236–246. [Google Scholar]
- 32.Fossen A, Abrahamsen TG, Storm-Mathisen I. Psychological outcome in children treated for brain tumor. Pediatric Hematology and Oncology. 1998;15:479–488. doi: 10.3109/08880019809018309. [DOI] [PubMed] [Google Scholar]
- 33.Bonner MJ, et al. Social functioning and facial expression recognition in survivors of pediatric brain tumors. Journal of Pediatric Psychology. 2008;33:1142–1152. doi: 10.1093/jpepsy/jsn035. [DOI] [PubMed] [Google Scholar]
- 34.Palmer SN, et al. The PedsQL Brain Tumor Module: initial reliability and validity. Pediatric Blood and Cancer. 2007;49:287–293. doi: 10.1002/pbc.21026. [DOI] [PubMed] [Google Scholar]
- 35.Parker J, et al. Peer relationships and developmental psychopathology. In: Cicchetti D, Cohen D, editors. Developmental Psychopathology: Risk, Disorder, and Adaptation (Vol. 2, 2nd edition) Wiley; New York: 2006. pp. 419–493. [Google Scholar]
- 36.Parker JG, Asher SR. Peer relations and later personal adjustment: Are low-accepted children at risk? Psychological Bulletin. 1987;102:357–389. doi: 10.1037//0033-2909.102.3.357. [DOI] [PubMed] [Google Scholar]
- 37.Coie JD. Toward a theory of peer rejection. In: Asher SR, Coie JD, editors. Peer Rejection in Childhood. Cambridge University Press; Cambridge, England: 1990. pp. 365–401. [Google Scholar]
- 38.Yeates KO, et al. Social outcomes in childhood brain disorder: a heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hocking MC, et al. Neurocognitive and family functioning and quality of life among young adult survivors of childhood brain tumors. The Clinical Neuropsychologist. 2011;25:942–962. doi: 10.1080/13854046.2011.580284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anderson V, et al. Impact of early brain insult on the development of social competence. In: Anderson V, Beauchamp MH, editors. Developmental Social Neuroscience and Childhood Brain Insult: Theory and Practice. Guilford; New York: 2012. pp. 231–253. [Google Scholar]
- 41.Cavell T. Social adjustment, social performance, and social skills: a tri-component model of social competence. Journal of Clinical Child Psychology. 1990;19:111–122. [Google Scholar]
- 42.Yeates KO, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 43.Janusz JA, et al. Social problem-solving skills in children with traumatic brain injury: Long-term outcomes and prediction of social competence. Child Neuropsychology. 2002;8:179–194. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- 44.Dennis M, et al. How children with head injury represent real and deceptive emotion in short narratives. Brain and Language. 1998;61:450–483. doi: 10.1006/brln.1997.1886. [DOI] [PubMed] [Google Scholar]
- 45.Dennis M, et al. Emotional expression and socially modulated emotive communication in children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:34–43. doi: 10.1017/S1355617712000884. [DOI] [PubMed] [Google Scholar]
- 46.Dennis M, et al. Irony and empathy in children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:338–348. doi: 10.1017/S1355617712001440. [DOI] [PubMed] [Google Scholar]
- 47.Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Developmental Neuropsychology. 2004;25:135–158. doi: 10.1080/87565641.2004.9651925. [DOI] [PubMed] [Google Scholar]
- 48.Jacobson LA, Williford AP, Pianta RC. The role of executive function in children’s competent adjustment to middle school. Child Neuropsychology. 2011;17:255–280. doi: 10.1080/09297049.2010.535654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolfe KR, et al. Executive functions and social skills in survivors of pediatric brain tumor. Child Neuropsychology. 2012 doi: 10.1080/09297049.2012.669470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alduncin N, et al. Executive function is associated with social competence in preschool-aged children born preterm or full term. Early Human Development. 2014 doi: 10.1016/j.earlhumdev.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ganesalingam K, et al. Executive functions and social competence in young children 6 months following traumatic brain injury. Neuropsychology. 2011;25:466–476. doi: 10.1037/a0022768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schonfield AM, et al. Executive functions predict social skills following prenatal alcohol exposure. Child Neuropsychology. 2006;12:439–452. doi: 10.1080/09297040600611338. [DOI] [PubMed] [Google Scholar]
- 53.Prigatano GP. Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: A 20-year perspective. Journal of Head Trauma Rehabilitation. 2005;20:19–29. doi: 10.1097/00001199-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Bronfrenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 55.Cassidy J, et al. Family-peer connections: The roles of emotional expressiveness within the family and children’s understanding of emotions. Child Development. 1992;63:603–618. doi: 10.1111/j.1467-8624.1992.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 56.McDowell DJ, Parke RD. Parental correlates of children’s peer relations: An empirical test of a tripartite model. Developmental Psychology. 2009;45:224–235. doi: 10.1037/a0014305. [DOI] [PubMed] [Google Scholar]
- 57.Masten AS, Coatsworth JD. The development of competence in favorable and unfavorable environments: Lessons from research on successful children. American Psychologist. 1998;53:205–220. doi: 10.1037//0003-066x.53.2.205. [DOI] [PubMed] [Google Scholar]
- 58.Ross H, Howe N. Family influences on children’s peer relationships. In: Rubin KH, Bukowski WM, Laursen B, editors. Handbook of peer interactions, relationships, and groups. Social, emotional and personality development in context. Guilford Press; New York, NY: 2009. pp. 508–527. [Google Scholar]
- 59.Taylor HG, et al. Influences on first year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- 60.Wade SL, et al. Long-term parental and family adaptation following pediatric brain injury. Journal of Pediatric Psychology. 2006;31:1072–1083. doi: 10.1093/jpepsy/jsj077. [DOI] [PubMed] [Google Scholar]
- 61.Patino-Fernandez AM, et al. Acute stress in parents of children newly diagnosed with cancer. Pediatric Blood and Cancer. 2008;50:289–292. doi: 10.1002/pbc.21262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alderfer MA, et al. Patterns of posttraumatic stress symptoms in parents of childhood cancer survivors. Journal of Family Psychology. 2005;19:430–440. doi: 10.1037/0893-3200.19.3.430. [DOI] [PubMed] [Google Scholar]
- 63.Anderson V, et al. Understanding predictors of functional recovery and outcome thirty months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- 64.Dennis M, et al. Age, plasticity, and homeostasis in childhood brain disorders. Neuroscience and Behavioral Reviews. 2013;37:2760–2773. doi: 10.1016/j.neubiorev.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moore BD., III Neurocognitive outcomes in survivors of childhood cancer. Journal of Pediatric Psychology. 2005;30:51–63. doi: 10.1093/jpepsy/jsi016. [DOI] [PubMed] [Google Scholar]
- 66.Moyer KH, et al. The impact of attention on social functioning in survivors of pediatric acute lymphoblastic leukemia and brain tumors. Pediatric Blood and Cancer. 2012;59:1290–1295. doi: 10.1002/pbc.24256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Poggi G, et al. Brain tumors in children and adolescents: Cognitive and psychological disorders at different ages. Psycho-Oncology. 2005;14:386–395. doi: 10.1002/pon.855. [DOI] [PubMed] [Google Scholar]
- 68.Mulhern RK, et al. Factors associated with social and behavioral problems among children recently diagnosed with brain tumor. Journal of Pediatric Psychology. 1993;18:339–350. doi: 10.1093/jpepsy/18.3.339. [DOI] [PubMed] [Google Scholar]
- 69.Schulte F, et al. Body weight, social competence, and cognitive functioning in survivors of childhood brain tumors. Pediatric Blood and Cancer. 2010;55:532–539. doi: 10.1002/pbc.22543. [DOI] [PubMed] [Google Scholar]
- 70.Kullgren KA, et al. Risk factors associated with long-term social and behavioral problems among children with brain tumors. Journal of Psychosocial Oncology. 2003;21:73–87. [Google Scholar]
- 71.Holmquist LA, Scott J. Treatment, age, and time-related predictors of behavioral outcome in pediatric brain tumor survivors. Journal of Clinical Psychology in Medical Settings. 2002;9:315–321. [Google Scholar]
- 72.Patel SK, et al. Attention dysfunction and parent reporting in children with brain tumors. Pediatric Blood and Cancer. 2007;49:970–974. doi: 10.1002/pbc.21151. [DOI] [PubMed] [Google Scholar]
- 73.Willard VW, Hardy KK, Bonner M. Gender differences in facial expression recognition in survivors of pediatric brain tumors. Psycho-Oncology. 2009;18:893–897. doi: 10.1002/pon.1502. [DOI] [PubMed] [Google Scholar]
- 74.Schulte F, Vannatta K, Barrera M. Social problem solving and social performance after a group social skills intervention for childhood brain tumor survivors. Psychooncology. 2014;23:183–189. doi: 10.1002/pon.3387. [DOI] [PubMed] [Google Scholar]
- 75.Barrera M, et al. Educational and social late effects of childhood cancer and related clinical, personal, and familial characteristics. Cancer. 2005;104:1751–1760. doi: 10.1002/cncr.21390. [DOI] [PubMed] [Google Scholar]
- 76.Hardy KK, et al. Perceived social competency in children with brain tumors: Comparison between children on and off therapy. Journal of Pediatric Oncology Nursing. 2010;27:156–163. doi: 10.1177/1043454209357918. [DOI] [PubMed] [Google Scholar]
- 77.Willard VW, et al. Emotional and behavioral functioning after conformal radiation therapy for pediatric ependymoma. International Journal of Radiation Oncology Biology and Physics. 2014;88:814–821. doi: 10.1016/j.ijrobp.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Foley B, et al. The impact of childhood hypothalamic/chiasmatic brain tumors on child adjustment and family functioning. Children’s Health Care. 2000;29:209–223. [Google Scholar]
- 79.Aarsen FK, et al. Functional outcome after low-grade astrocytoma treatment in childhood. Cancer. 2006;106:396–402. doi: 10.1002/cncr.21612. [DOI] [PubMed] [Google Scholar]
- 80.Brinkman TM, et al. Parent-reported social outcomes after treatment for pediatric embryonal tumors: A prospective longitudinal study. Journal of Clinical Oncology. 2012;30:4134–4140. doi: 10.1200/JCO.2011.40.6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wolfe-Christensen C, et al. Persistent psychosocial problems in children who develop posterior fossa syndrome after medulloblastoma resection. Pediatric Blood and Cancer. 2007;49:723–726. doi: 10.1002/pbc.21084. [DOI] [PubMed] [Google Scholar]
- 82.Armstrong GT, et al. Region-specific radiotherapy and neuropsychological outcomes in adult survivors of childhood CNS malignancies. Neuro-Oncology. 2010;12:1173–1186. doi: 10.1093/neuonc/noq104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carlson-Green B, Morris RD, Krawiecki NS. Family and illness predictors of outcome in pediatric brain tumors. Journal of Pediatric Psychology. 1995;20:769–784. doi: 10.1093/jpepsy/20.6.769. [DOI] [PubMed] [Google Scholar]
- 84.Carey ME, et al. Neuropsychological functioning and social functioning of survivors of pediatric brain tumors: Evidence of nonverbal learning disability. Child Neuropsychology. 2001;7:265–272. doi: 10.1076/chin.7.4.265.8730. [DOI] [PubMed] [Google Scholar]
- 85.Dodge KA, et al. Multidimensional latent-construct analysis of children’s social information processing patterns: Correlations with aggressive behavior problems. Psychological Assesment. 2002;14:60–73. doi: 10.1037//1040-3590.14.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Noll RB, Bukowski WM. Commentary: Social competence in children with chronic illness: The devil is in the details. Journal of Pediatric Psychology. 2012;37:959–966. doi: 10.1093/jpepsy/jss058. [DOI] [PubMed] [Google Scholar]
- 87.Barakat LP, et al. Evaluation of a social-skills training group intervention with children treated for brain tumors: A pilot study. Journal of Pediatric Psychology. 2003;28:299–307. doi: 10.1093/jpepsy/jsg019. [DOI] [PubMed] [Google Scholar]
- 88.Barrera M, Schulte F. A group social skills intervention program for survivors of childhood brain tumors. Journal of Pediatric Psychology. 2009;34:1108–1118. doi: 10.1093/jpepsy/jsp018. [DOI] [PubMed] [Google Scholar]
- 89.Wade SL, Carey J, Wolfe CR. The efficacy of an online cognitive-behavioral family intervention in improving child behavior and social competence following pediatric brain injury. Rehabilitation Psychology. 2006;51:179–189. [Google Scholar]
- 90.Kasari C, et al. Making the connection: randomized controlled trial of social skills at school for children with autism spectrum disorders. The Journal of Child Psychology and Psychiatry. 2012;53:431–439. doi: 10.1111/j.1469-7610.2011.02493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]