Abstract
Introduction:
Inflammatory bowel diseases (IBD; Crohn’s disease (CD), ulcerative colitis (UC)) often affect women in their reproductive years. Few studies have analyzed the impact of mode of child-birth on long-term IBD outcomes.
Methods:
We used a multi-institutional IBD cohort to identify all women in the reproductive age group with a diagnosis of IBD prior to pregnancy. We identified the occurrence of a new diagnosis code for perianal complications, IBD-related hospitalization and surgery, and initiation of medical therapy after either a vaginal delivery or caesarean section (CS). Cox proportional hazards models adjusting for potential confounders was used to estimate independent effect of mode of child-birth on IBD outcomes.
Results:
Our cohort included 360 women with IBD (161 CS). Women in the CS group were likely to be older and more likely to have complicated disease behavior prior to pregnancy. During follow-up, there was no difference in the likelihood of IBD-related surgery (multivariate hazard ratio 1.75, 95% confidence interval (CI) 0.40 – 7.75), IBD-related hospitalization (HR 1.39), initiation of immunomodulator therapy (HR 1.45) or anti-TNF therapy (HR 1.11). Among the 133 CD pregnancies with no prior perianal disease, we found no excess risk of subsequent new diagnosis perianal fistulae with vaginal delivery compared to CS (HR 0.19, 95% CI 0.04 – 1.05).
Conclusions:
Mode of delivery did not influence natural history of IBD. In our cohort, vaginal delivery was not associated with increased risk of subsequent perianal disease in women with CD.
Keywords: Crohn’s disease, ulcerative colitis, pregnancy, delivery, caesarean section
INTRODUCTION
Inflammatory bowel diseases (IBD) are chronic immunologically mediated diseases with a peak incidence for both Crohn’s disease (CD) and ulcerative colitis (UC) occurring during the 2nd-4th decades of life1, 2. Owing to its protracted lifelong course characterized by periods of remission and relapse, many women with IBD go through their reproductive years with concerns about the impact of disease on pregnancy outcomes, and conversely about the impact of pregnancy and childbirth on their disease. Despite the growing wealth of literature on this topic, significant gaps in knowledge and perception remain3-5. Most prior studies in this area have focused on fertility and fecundity, effect of the pregnancy itself on course of IBD during pregnancy and the immediate post-partum period, and the effect of IBD on pregnancy outcomes including gestational age and birth weight6-15. Reassuringly, apart from a weak increase in incidence of preterm births and low birth weight babies, neither CD nor UC are associated with other adverse pregnancy or health outcomes6-15. Furthermore, most of the current medications for treatment of IBD may be safely continued during pregnancy and in the post-partum period10, 16-18.
The recent decades have witnessed a significant increase in the proportion of women delivering via caesarean section (CS)19-21. Those with IBD seem to be at 1.5-2 fold increase in likelihood of childbirth via CS9, 13, 22, 23. This increase does not appear to be solely due to obstetric indications and is likely influenced in part by patient and provider preferences. One plausible reason for this preference towards operative delivery is the concern regarding perineal trauma during vaginal childbirth in those with established IBD, particularly those with CD who may be prone towards development of perianal disease with their CD. The data in this area, both incidence of new diagnosis of perianal involvement as well as outcomes of perianal fistula in those with established perianal CD, is limited both in the number of patients studied as well as the methods employed with biases stemming from self-report, small cohorts, or short duration of follow-up24-27. Thus, larger cohorts examining the effect of mode of delivery on long-term outcomes of women with CD or UC are important to provide objective and accurate estimates on relative safety of the two modalities of childbirth.
Using a large multi-institutional IBD cohort, we identified all women who had childbirth at one of two tertiary referral IBD centers. We examined the impact of mode of delivery on IBD outcomes over a median follow-up of 4 years.
METHODS
Study Cohort
Our study cohort included data from women seeking care at two major tertiary centers in Boston (Massachusetts General Hospital (MGH) and Brigham and Women’s Hospital (BWH)) and affiliated medical centers comprising the Partners Healthcare network. The two hospitals together serve over 3 million patients in the greater Boston metropolitan area and serve as referral centers. The development of our IBD cohort has been described in detail in previous publications28-33. In brief, we first identified all patients with at least one International Classification of Diseases, 9th edition, clinical modification (ICD-9-CM) codes for CD (555.x) or UC (556.x). Using a combination of codified data for diagnoses and procedures, free text concepts identified using natural language processing from office visit notes, discharge summaries, pathology, laboratory, and radiology reports, endoscopy findings, and operative reports, and medication use determined using electronic prescription data from the medical record, we developed and validated an algorithm that defined CD or UC with a positive predictive value of 97%S. This yielded a final IBD cohort of 5,522 UC and 5,506 CD patients30.
For the purpose of this study, we identified all women with IBD who had at least one pregnancy and delivery at our institutions (n=497). Women with codes for vaginal delivery (ICD-9-CM 650, 660-669) comprised the vaginal delivery group while those who underwent delivery via caesarean section comprised the CS group (ICD-9-CM 669.7, 74.0-74.9). If patients had codes for both on the same day, they were assigned to the CS group. Only deliveries occurring after the first diagnosis code for CD or UC were included in this analysis resulting in a final cohort of 360 women. Only the first pregnancy after diagnosis of IBD was included in the analysis. Spontaneous abortions were not included in the analysis.
Variable definition
Information was recorded about age at pregnancy and age at first diagnosis code for CD or UC, disease duration (interval since first diagnostic code for CD or UC) at pregnancy, race, and type of IBD. Among those with CD, complicated disease phenotype was defined by the presence of codes for stricturing or penetrating complications (Supplementary Table). As well the presence of codes for perianal fistula, anorectal strictures, or perianal surgery was noted separately. The use of immunomodulators (azathioprine, 6-mercaptopurine (6-MP), methotrexate) and monoclonal antibodies to tumor necrosis factor α (anti-TNF) (infliximab, adalimumab, and certolizumab pegol) were defined both prior to and following pregnancy using the electronic prescription function of our medical record.
Outcomes
Our primary study outcomes included the following: - (i) new prescriptions for immunomodulator or anti-TNF therapy after pregnancy (in prior non-users); (ii) IBD-related hospitalizations defined as those hospitalizations where IBD was determined to be primary diagnosis on discharge, and (iii) an IBD-related bowel resection surgery. Furthermore, among those with CD, we specifically examined the occurrence of a new diagnosis code for perianal fistulizing disease or perianal surgical procedures in those with no such codes prior to pregnancy.
Statistical Analysis
All statistical analysis was performed using Stata 12.0 (StataCorp, College Station, TX). Continuous variables were summarized using medians and inter-quartile ranges (IQR) while categorical variables were expressed as proportions and compared using the chi-square test. All patients contributed person-time from the date of delivery (vaginal or CS) until the subsequent pregnancy, occurrence of one of our study outcomes, end of follow-up in our health system, or death. Kaplan-Meier survival curves were constructed to compare time to occurrence of events, stratifying by mode of childbirth and differences compared using the log-rank test. Cox proportional hazards models defined the independent effect of the mode of childbirth (vaginal delivery vs. CS), adjusting for other relevant covariates in the model. All survival models satisfied the proportional hazards assumption.
As choice of mode of delivery is a non-random occurrence and is likely influenced by severity of prior disease and phenotype, we additionally performed a propensity score adjusted analysis. We first calculated a propensity score that predicted likelihood of delivery via CS based on age, duration of disease, IBD type, prior medical therapy, IBD-related surgery, perianal disease, or disease phenotype (penetrating or stricturing complications). The propensity score performed well in differentiating those likely to delivery vaginally from those who delivered via CS (p < 0.0001). In addition to the unadjusted hazard ratio (HR), we calculated the HR and 95% confidence intervals (CI) for models additionally adjusting for the propensity score, and a multivariate model adopting traditional methods incorporating variables that met statistical significance on the univariate analysis (p < 0.05) or were deemed to be clinically relevant based on existing literature. The study was approved by the Institutional Review Board of Partners Healthcare.
RESULTS
Our IBD cohort included 2,702 women between the ages of 18-45 years (1,320 UC, 1,382 CD) among whom 497 women had at least one successful term pregnancy at our institution. A total of 137 women had a pregnancy before the first diagnosis code for CD or UC and were excluded, leaving 360 women available for analysis. Among these, 161 delivered through CS and 198 had a vaginal delivery. Table 1 compares the characteristics for women across the two modes of delivery. Women in the CS group were slightly older (mean age 33.5 years vs. 32.1 years) but were similar to the vaginal delivery group in race and distribution of IBD. The patients had a mean follow up of 2 years (interquartile range (IQR) 1-5 years) at our center prior to their pregnancy, and had a post-pregnancy follow-up of 4 years (IQR 2–8 years). Among women with CD, those with prior perianal disease (20% vs. 8%) or complicated disease behavior (21% vs. 5%) were more likely to delivery via CS than vaginally (p < 0.05 for both comparisons). There was no difference in medical therapy prior to pregnancy across both groups though the CS group was more likely to have a prior IBD-related surgery (9% vs. 4%, p=0.02).
Table 1.
Characteristics of women with IBD, stratified by modality of childbirth
| Characteristic | C-Section (n = 161) % |
Vaginal delivery (n = 198) % |
p-value |
|---|---|---|---|
| Mean age (in years) (SD) | 33.5 (4.9) | 32.1 (5.2) | 0.01 |
| Mean disease duration at pregnancy (in years) (SD) |
3.3 (3.4) | 2.9 (2.9) | 0.20 |
| Mean age at first IBD code (in years) (SD) |
30.1 (5.6) | 29.5 (6.5) | 0.30 |
| Race | 0.43 | ||
| White | 85 | 88 | |
| Non-white | 15 | 12 | |
| IBD type | 0.13 | ||
| Crohn’s disease | 47 | 39 | |
| Ulcerative colitis | 53 | 61 | |
| Perianal disease+ | 20 | 8 | 0.03 |
| Complicated disease behavior+ | 21 | 5 | 0.003 |
| Disease history prior to pregnancy |
|||
| Immunosuppression use | 19 | 15 | 0.30 |
| IBD-related hospitalization | 22 | 17 | 0.21 |
| IBD-related surgery | 9 | 4 | 0.02 |
| Duration of follow-up after delivery (in years) |
4.9 (3.8) | 5.2 (3.9) | 0.50 |
C-section – Caesarean section; SD – standard deviation; IBD – inflammatory bowel disease
Immunomodulators including azathioprine, 6-mercaptopurine, or methotrexate Anti-TNF agents including infliximab, adalimumab, or certolizumab pegol
- among those with Crohn’s disease
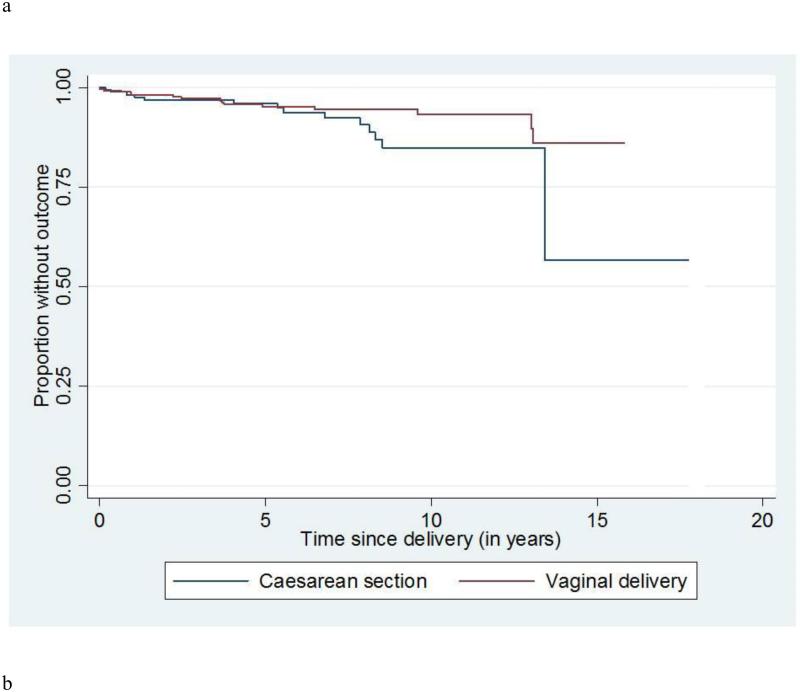
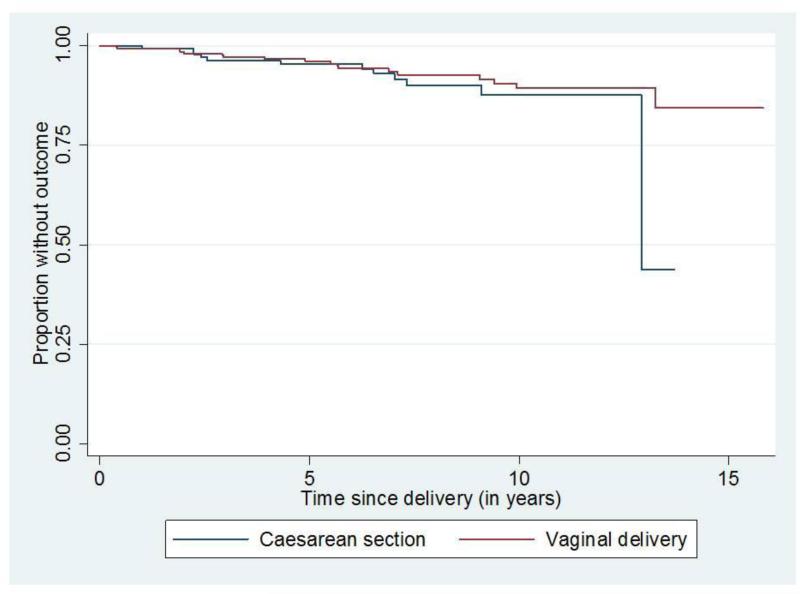
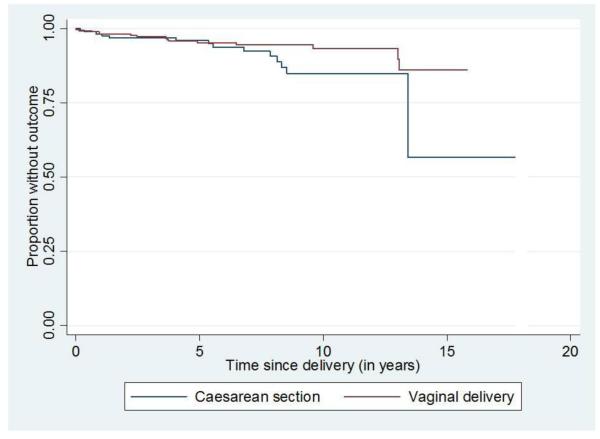
Table 2 presents the results of unadjusted and adjusted models comparing the various outcomes between the vaginal delivery and the CS groups. Ninety-nine (99/199, 50%) patients had a subsequent IBD-related hospitalization after pregnancy among the vaginal delivery group compared to 65/161 (40%) in the CS group (HR for vaginal delivery compared to CS 1.20, 95% CI 0.87 – 1.64). The difference between the two groups remained non-significant in both the propensity score adjusted model (HR 1.20, 95% CI 0.87 – 1.65) and multivariate-adjusted HR (1.39, 95% CI 0.98 – 1.96). There was also no difference in the time to initiation of immunomodulator therapy (HR 1.45, 95% CI 0.82 – 2.57) or anti-TNF therapy (HR 1.11, 95% CI 0.44 – 2.77) among women who were non-users at the time of the index pregnancy (Figure 1). In subgroup analysis, mode of delivery did not affect subsequent health outcomes in either CD or UC (p-interaction > 0.05). Similarly, 3% of the vaginal delivery group and 7% of the CS group subsequently required an IBD-related surgery with no statistically significant difference on the propensity score adjusted (HR 0.59, 95% CI 0.19 – 1.84) or multivariate adjusted models (HR 1.75, 95% CI 0.40 – 7.75) (Figure 2).
Table 2.
Multivariate analysis of perianal fistula, IBD-related surgery and hospitalization by delivery type
| Outcome | Unadjusted HR (95% CI) |
Propensity score adjusted HR (95% CI) |
Multivariate adjusted HR† (95% CI) |
|---|---|---|---|
| Perianal fistula‡ | 0.21 (0.04 – 0.99) | 0.25 (0.05 – 1.22) | 0.19 (0.04 – 1.05) |
| Perianal fistula surgery‡ | 0.33 (0.03 – 3.17) | 0.43 (0.04 – 4.20) | 0.92 (0.02 – 4.79) |
| IBD-related hospitalization | 1.20 (0.87 – 1.64) | 1.20 (0.87 – 1.65) | 1.39 (0.98 – 1.96) |
| IBD-related surgery | 0.34 (0.12 – 0.99) | 0.59 (0.19 – 1.84) | 1.75 (0.40 – 7.75) |
| Immunomodulator use | 1.40 (0.81 – 2.40) | 1.31 (0.76 – 2.27) | 1.45 (0.82 – 2.57) |
| Anti-TNF use | 0.85 (0.37 – 1.98) | 0.93 (0.40 – 2.21) | 1.11 (0.44 – 2.77) |
Hazard ratios are for comparison between vaginal delivery and C-section (reference category)
HR – Hazard ratio, CI – confidence interval; IBD – inflammatory bowel disease; TNF – tumor necrosis factor α
Immunomodulators including azathioprine, 6-mercaptopurine, or methotrexate Anti-TNF agents including infliximab, adalimumab, or certolizumab pegol
Among those with Crohn’s disease
Adjusted for age, disease phenotype, need for surgery, immunosuppression or hospitalization prior to pregnancy, and disease duration
Figure 1.
New prescriptions for immunomodulator or anti-TNF biologic therapy, by mode of childbirth
Figure 2.
Risk of IBD-related surgery, by mode of childbirth
Among 133 CD pregnancies with no prior perianal disease, 2/72 (3%) were noted to have a subsequent diagnosis code for perianal disease compared to 8/61 (13%) in the CS group (unadjusted HR for vaginal delivery compared to CS 0.21, 95% CI 0.04 – 0.99). However, this difference appeared to be due to difference in the selection of mode of delivery based on patient characteristics. Neither the propensity score adjusted model (HR 0.25, 95% CI 0.05 – 1.22) nor multivariate adjusted model (HR 0.19, 95% CI 0.04 – 1.05) demonstrated a difference in subsequent perianal fistula by mode of delivery. Similarly there was no difference in the likelihood of needing subsequent perianal procedures by mode of delivery (Table 2).
DISCUSSION
Examination of pregnancy outcomes in patients with CD and UC is an important area of research. Most studies in the field have focused on fertility in such patients, pregnancy and birth outcomes including gestational age and birth weight, and effect of medication exposure during pregnancy, particularly immunosuppressive and anti-TNF medications, on such outcomes6-17, 24. Few have specifically examined the effect of mode of delivery on long-term outcomes in patients with CD and none focusing on UC13, 24-27. Indeed, professional society guidelines and expert opinions only briefly discuss the choice regarding the mode of delivery in IBD patients10. However, the trend towards growing utilization of CS in both the IBD and general population and tendency towards recommendation of this as preferred strategy due to concern about the impact of perineal and pelvic trauma on disease frequently involving the rectum and lower colon, it is important to provide accurate and objective data regarding the long-term impact of mode of delivery on disease outcomes in those with IBD. Using data from a large multi-institutional validated electronic medical record cohort of women with either CD or UC, we provide reassuring data that mode of delivery did not impact subsequent disease outcomes in terms of escalation of medical therapy, IBD-related surgery or hospitalization. Importantly, in women with CD who had no prior perianal involvement, there was no increase in risk of a new perianal fistula diagnosis or surgical procedure following vaginal delivery.
There is growing utilization of CS in patients with IBD. More pregnancies occurring after IBD result in a CS than those prior to an IBD diagnosis22. In a meta-analysis by Cornish et al., women with IBD were 1.5 times more likely to delivery via C-section when compared to controls23. A recent study using an administrative database including data from 2,882 women with CD, identified that between 42.8 – 83.1% of women with CD delivered via C-section24. The reason for this increasing trend is unclear. While perianal disease appears to favor delivery via CS24-27, only a small proportion of women with CD have established perianal disease prior to pregnancy. Thus, it is likely that the secular increase in CS may be influenced by patient or provider preferences or obstetric indications. With the wealth of data suggesting that perinatal outcomes are similar in IBD compared to non-IBD patients, it is unlikely that differential distribution of obstetric indications are sole determinants for the high CS rate in those with IBD. Reassuringly, our findings suggest that vaginal delivery is not associated with worse long-term outcomes over a median follow-up of over 4 years in both CD and UC. The potential for complications associated with CS including the higher rate of requiring CS in subsequent pregnancies34, and potential for both short- and long-term post-operative complications suggest that prudence be used in making decisions regarding mode of delivery in patients with IBD. This is particularly relevant as a substantial portion of IBD patients may require abdominal surgery subsequently for management of their disease.
Much of the focus on the effect of perineal trauma has been on the risk of development of perianal complications in those with CD. In patients with established perianal CD, a small study by Ilnyckyji et al. suggested that women with active disease all reported worsening of perianal symptoms post-partum, while those with inactive disease remained quiescent25. In a study based on survey of gastroenterologists, among those with no history of perianal CD, the rate of perianal complications was greater (17.9%) in those with vaginal delivery leading the authors to speculate that perineal trauma during vaginal delivery may have resulted in subsequent perianal disease27. However, the estimates based on surveys have numerous limitations including lack of objective confirmation of perianal disease and potential for bias in self-report resulting in the high rate of perianal disease reported post-partum. In contrast, Smink et al. from the Netherlands identified no increase in risk of progression to perianal involvement in CD patients without perianal disease prior to pregnancy for vaginal compared with CS delivery (5% vs. 14%, p=NS)26. We have recently described that vaginal delivery may be safe in women with perianal disease and not associated with short-term increase in risk of complications, albeit acknowledging a selection bias in women trialing a vaginal birth35. We extend the findings of that study to this larger cohort without perianal disease prior to delivery and provide reassuring data that in a wider population of CD, vaginal delivery does not appear associated with an increase in incidence of perianal or other complications. However, we could not study whether the patients with active CD were more likely to have perianal complications after vaginal delivery in this EMR dataset. Some of the CS that were performed may have been in women with active CD whose physicians were concerned about the risk for perianal complications.
We readily acknowledge several limitations to our study. First, albeit one of the largest cohort to examine the impact of mode of delivery on subsequent disease outcomes in patients with IBD, our cohort consisted of patients who were seeking care and delivered at one of two major tertiary referral centers in Boston and thus may not be representative of IBD in the community. However as this is indeed the cohort most enriched for severe disease and adverse outcomes, demonstrating the safety of vaginal delivery in this cohort provides reassurance to most women with IBD. Second, this cohort was not adequately powered to examine specifically the effect of mode of delivery on women with established perianal CD. However a complementary study recently published by our group supports the safety of vaginal delivery in that cohort as well, albeit acknowledging a selection bias in the choice of mode of delivery35. Third, we did not have information on the indication for CS (obstetric, provider, or patient preference) or occurrence of complications such as need for episiotomy or perianal tear during vaginal delivery and post-operative complications in the CS group. Fourth, it is possible that we may have inadequate follow-up on patients after delivery to determine IBD outcomes. However, we would not expect this to be differential by mode of childbirth.
In conclusion, we demonstrate that there is no difference in long-term outcomes between women with either CD or UC delivering via vaginal birth compared to caesarean section. Reassuringly, we did not identify an effect of mode of delivery on risk of new perianal disease in women with CD. Further prospective studies examining impact of mode of delivery on functional outcomes such as incontinence would provide complementary data. At this time, patients and providers may be reassured about a trial of vaginal birth for most IBD patients without an obstetric indication for CS delivery.
Supplementary Material
Sources of Funding
The study was supported by NIH U54-LM008748. A.N.A is supported by funding from the American Gastroenterological Association and from the US National Institutes of Health (K23 DK097142). K.P.L. is supported by NIH K08 AR060257 and the Harold and Duval Bowen Fund. E.W.K is supported by grants from the NIH (K24 AR052403, P60 AR047782, R01 AR049880).
Footnotes
Financial conflicts of interest: None
Specific author contributions:
An author may list more than one contribution, and more than one author may have contributed to the same element of the work
Study concept and design – Ananthakrishnan,
Data Collection – Ananthakrishnan, Cheng, Gainer, Cagan, Cai, Churchill, Kohane, Shaw, Liao, Murphy
Analysis – Ananthakrishnan
Preliminary draft of the manuscript – Ananthakrishnan
Approval of final version of the manuscript – Ananthakrishnan, Cheng, Gainer, Cagan, Cai, Churchill, Kohane, Shaw, Liao, Murphy
Guarantor of the article: Ananthakrishnan
REFERENCES
- 1.Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785–94. doi: 10.1053/j.gastro.2011.01.055. [DOI] [PubMed] [Google Scholar]
- 2.Loftus EV, Jr., Sandborn WJ. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:1–20. doi: 10.1016/s0889-8553(01)00002-4. [DOI] [PubMed] [Google Scholar]
- 3.Mountifield RE, Prosser R, Bampton P, et al. Pregnancy and IBD treatment: this challenging interplay from a patients' perspective. J Crohns Colitis. 2010;4:176–82. doi: 10.1016/j.crohns.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Selinger CP, Eaden J, Selby W, et al. Patients' knowledge of pregnancy-related issues in inflammatory bowel disease and validation of a novel assessment tool ('CCPKnow') Aliment Pharmacol Ther. 2012;36:57–63. doi: 10.1111/j.1365-2036.2012.05130.x. [DOI] [PubMed] [Google Scholar]
- 5.Selinger CP, Eaden J, Selby W, et al. Inflammatory bowel disease and pregnancy: lack of knowledge is associated with negative views. J Crohns Colitis. 2013;7:e206–13. doi: 10.1016/j.crohns.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Agret F, Cosnes J, Hassani Z, et al. Impact of pregnancy on the clinical activity of Crohn's disease. Aliment Pharmacol Ther. 2005;21:509–13. doi: 10.1111/j.1365-2036.2005.02384.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferrero S, Ragni N. Inflammatory bowel disease: management issues during pregnancy. Arch Gynecol Obstet. 2004;270:79–85. doi: 10.1007/s00404-003-0489-6. [DOI] [PubMed] [Google Scholar]
- 8.Friedman S, Regueiro MD. Pregnancy and nursing in inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:265–73. doi: 10.1016/s0889-8553(01)00015-2. xii. [DOI] [PubMed] [Google Scholar]
- 9.Kornfeld D, Cnattingius S, Ekbom A. Pregnancy outcomes in women with inflammatory bowel disease--a population-based cohort study. Am J Obstet Gynecol. 1997;177:942–6. doi: 10.1016/s0002-9378(97)70298-9. [DOI] [PubMed] [Google Scholar]
- 10.Mahadevan U, Cucchiara S, Hyams JS, et al. The London Position Statement of the World Congress of Gastroenterology on Biological Therapy for IBD with the European Crohn's and Colitis Organisation: pregnancy and pediatrics. Am J Gastroenterol. 2011;106:214–23. doi: 10.1038/ajg.2010.464. quiz 224. [DOI] [PubMed] [Google Scholar]
- 11.Ng SW, Mahadevan U. Management of inflammatory bowel disease in pregnancy. Expert Rev Clin Immunol. 2013;9:161–73. doi: 10.1586/eci.12.103. quiz 174. [DOI] [PubMed] [Google Scholar]
- 12.Rogers RG, Katz VL. Course of Crohn's disease during pregnancy and its effect on pregnancy outcome: a retrospective review. Am J Perinatol. 1995;12:262–4. doi: 10.1055/s-2007-994469. [DOI] [PubMed] [Google Scholar]
- 13.Huang VW, Habal FM. From conception to delivery: Managing the pregnant inflammatory bowel disease patient. World J Gastroenterol. 2014;20:3495–3506. doi: 10.3748/wjg.v20.i13.3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahadevan U, Sandborn WJ, Li DK, et al. Pregnancy outcomes in women with inflammatory bowel disease: a large community-based study from Northern California. Gastroenterology. 2007;133:1106–12. doi: 10.1053/j.gastro.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 15.Selinger CP, Leong RW, Lal S. Pregnancy related issues in inflammatory bowel disease: evidence base and patients' perspective. World J Gastroenterol. 2012;18:2600–8. doi: 10.3748/wjg.v18.i21.2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gisbert JP, Chaparro M. Safety of anti-TNF agents during pregnancy and breastfeeding in women with inflammatory bowel disease. Am J Gastroenterol. 2013;108:1426–38. doi: 10.1038/ajg.2013.171. [DOI] [PubMed] [Google Scholar]
- 17.Hutson JR, Matlow JN, Moretti ME, et al. The fetal safety of thiopurines for the treatment of inflammatory bowel disease in pregnancy. J Obstet Gynaecol. 2013;33:1–8. doi: 10.3109/01443615.2012.716106. [DOI] [PubMed] [Google Scholar]
- 18.Saha S, Wald A. Safety and efficacy of immunomodulators and biologics during pregnancy and lactation for the treatment of inflammatory bowel disease. Expert Opin Drug Saf. 2012;11:947–57. doi: 10.1517/14740338.2012.720970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen VM, Baskett TF, O'Connell CM. Contribution of select maternal groups to temporal trends in rates of caesarean section. J Obstet Gynaecol Can. 2010;32:633–41. doi: 10.1016/s1701-2163(16)34566-2. [DOI] [PubMed] [Google Scholar]
- 20.Fairley L, Dundas R, Leyland AH. The influence of both individual and area based socioeconomic status on temporal trends in Caesarean sections in Scotland 1980-2000. BMC Public Health. 2011;11:330. doi: 10.1186/1471-2458-11-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts CL, Algert CS, Carnegie M, et al. Operative delivery during labour: trends and predictive factors. Paediatr Perinat Epidemiol. 2002;16:115–23. doi: 10.1046/j.1365-3016.2002.00409.x. [DOI] [PubMed] [Google Scholar]
- 22.Manosa M, Navarro-Llavat M, Marin L, et al. Fecundity, pregnancy outcomes, and breastfeeding in patients with inflammatory bowel disease: a large cohort survey. Scand J Gastroenterol. 2013;48:427–32. doi: 10.3109/00365521.2013.772229. [DOI] [PubMed] [Google Scholar]
- 23.Cornish J, Tan E, Teare J, et al. A meta-analysis on the influence of inflammatory bowel disease on pregnancy. Gut. 2007;56:830–7. doi: 10.1136/gut.2006.108324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hatch Q, Champagne BJ, Maykel JA, et al. Crohn's disease and pregnancy: the impact of perianal disease on delivery methods and complications. Dis Colon Rectum. 2014;57:174–8. doi: 10.1097/DCR.0b013e3182a41381. [DOI] [PubMed] [Google Scholar]
- 25.Ilnyckyji A, Blanchard JF, Rawsthorne P, et al. Perianal Crohn's disease and pregnancy: role of the mode of delivery. Am J Gastroenterol. 1999;94:3274–8. doi: 10.1111/j.1572-0241.1999.01537.x. [DOI] [PubMed] [Google Scholar]
- 26.Smink M, Lotgering FK, Albers L, et al. Effect of childbirth on the course of Crohn's disease; results from a retrospective cohort study in the Netherlands. BMC Gastroenterol. 2011;11:6. doi: 10.1186/1471-230X-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brandt LJ, Estabrook SG, Reinus JF. Results of a survey to evaluate whether vaginal delivery and episiotomy lead to perineal involvement in women with Crohn's disease. Am J Gastroenterol. 1995;90:1918–22. [PubMed] [Google Scholar]
- 28.Ananthakrishnan AN, Cagan A, Gainer VS, et al. Normalization of plasma 25-hydroxy vitamin D is associated with reduced risk of surgery in Crohn's disease. Inflamm Bowel Dis. 2013;19:1921–7. doi: 10.1097/MIB.0b013e3182902ad9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ananthakrishnan AN, Cagan A, Gainer VS, et al. Mortality and extraintestinal cancers in patients with primary sclerosing cholangitis and inflammatory bowel disease. J Crohns Colitis. 2014 doi: 10.1016/j.crohns.2014.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ananthakrishnan AN, Cai T, Savova G, et al. Improving case definition of Crohn's disease and ulcerative colitis in electronic medical records using natural language processing: a novel informatics approach. Inflamm Bowel Dis. 2013;19:1411–20. doi: 10.1097/MIB.0b013e31828133fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ananthakrishnan AN, Cheng SC, Cai T, et al. Serum Inflammatory Markers and Risk of Colorectal Cancer in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2014 doi: 10.1016/j.cgh.2013.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ananthakrishnan AN, Cheng SC, Cai T, et al. Association Between Reduced Plasma 25-Hydroxy Vitamin D and Increased Risk of Cancer in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2013 doi: 10.1016/j.cgh.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ananthakrishnan AN, Gainer VS, Perez RG, et al. Psychiatric co-morbidity is associated with increased risk of surgery in Crohn's disease. Aliment Pharmacol Ther. 2013;37:445–54. doi: 10.1111/apt.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351:2581–9. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 35.Cheng AG, Oxford EC, Sauk J, et al. The impact of mode of delivery on outcomes in patients with perianal. Crohn’s disease Inflamm Bowel Dis. 2014 doi: 10.1097/MIB.0000000000000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.