Abstract
Rituximab has been used to increase the efficacy of desensitization protocols for HLA incompatible kidney transplantation, however, controlled comparisons have not been reported. Here we examined 256 post-transplant HLA antibody levels in 25 recipients desensitized with or 25 without rituximab induction, to determine the impact of B cell depletion. We found significantly less HLA antibody rebound in the rituximab-treated patients (7% of donor specific antibodies (DSAs) and 33% of non-DSAs) compared to a control cohort desensitized and transplanted without rituximab (32% DSAs and 55% non-DSAs). The magnitude of the increase was significantly larger among patients who did not receive rituximab. Interestingly, in rituximab treated patients, of the 39 HLA antibodies that increased post-transplant, 34 were specific for HLA mismatches present in previous allografts or pregnancies, implying limited efficacy in memory B cell depletion. Compared to controls, rituximab-treated patients had a significantly greater mean reduction in DSA (−2505 versus −292 mean fluorescence intensity), but a similar rate of DSA persistence (52% in rituximab treated and 40% in non-treated recipients). Thus, rituximab induction in HLA incompatible recipients reduced the incidence and magnitude of HLA antibody rebound, but did not impact DSA elimination, antibody mediated rejection, or 5 year allograft survival when compared to recipients desensitized and transplanted without rituximab.
Keywords: rituximab, B cells, HLA antibody, desensitization, kidney transplantation
Introduction
B cell depletion protocols using rituximab, a chimeric murine/human monoclonal antibody specific for CD20, were developed to treat B cell malignancies(1) but have also been utilized to treat antibody-mediated autoimmune diseases(2, 3) and to prevent or combat humoral rejection in solid organ transplantation(4–7). In transplantation, B cell depletion has been used pre-transplantation in desensitization protocols to reduce HLA sensitization allowing access to transplantation(8–11) and perioperatively to prevent the development of de novo donor-specific HLA antibodies (DSA) or to prevent an anamnestic response(6, 12–14). It has also been utilized post-transplant, during active antibody mediated rejection (AMR) to dampen the immune response(15–17).
The efficacy of desensitization protocols that include rituximab to decrease DSA has been reported in both ABO and HLA live donor incompatible renal transplantation(8, 14,18–23). Kohei et al. also reported a decreased incidence of de novo DSA and chronic AMR among ABO incompatible recipients transplanted with rituximab induction compared to an ABO compatible cohort transplanted without rituximab(24). However, the efficacy of rituximab in preventing post-transplantation DSA rebound and enhancing post-transplantation DSA elimination after desensitization protocols has not been analyzed in controlled cohorts. Reports to date have compared patients transplanted with rituximab treatment to those that had no or less intensive desensitization treatment. Moreover, a limited number of post-transplant time-points and HLA antibodies were included in previous studies(14, 18,23, 25, 26).
This study evaluates the impact of rituximab induction on HLA-specific antibody production in patients undergoing desensitization for HLA incompatible live donor kidney transplantation. Our goal was to gain insight into the efficacy of B cell depletion in preventing the activation and differentiation of HLA specific B cells, particularly in sensitized recipients who may harbor HLA-specific memory B cells.
Results
We compared the incidence of post-transplant HLA antibody rebound in 50 patients undergoing HLA incompatible transplantation using a desensitization protocol that either did or did not include a single dose of rituximab (375 mg/m2) the day before transplantation. Patient demographics are provided in Table 1 and reflect our practice of using rituximab for patients with a higher risk for antibody mediated rejection(27, 28). The 25 patients who received rituximab induction had broader sensitization (mean CPRA = 80% versus 60%, p=0.02), a higher incidence of previous transplants (76% versus 28%, p=0.002) and repeat HLA mismatches (80% versus 0%, p<0.0001). However, the two cohorts had similar DSA levels prior to desensitization and received a similar number of plasmapheresis treatments (Table 1., p= 0.20).
Table 1.
Patient demographics
| Rituximab N=25 |
No Rituximab N=25 |
p value | |
|---|---|---|---|
| Recipient Age (mean, SD) | 41 ± 15 | 48 ± 13 | 0.08 |
| Male Gender (No. patients, %) | 8 (32%) | 7 (28%) | 1.0 |
| Previous Txn (No. patients, %) | 19 (76%) | 7 (28%) | 0.002 |
| Previous Txn ≥ 3 | 5 (20%) | 0 | 0.06 |
| HLA-A;B;DR;DQ Mismatch (mean) | 4.8 | 5.0 | 0.61 |
| Repeat HLA mismatch (No. patients, %) | 20 (80%) | 0 | 0.0001 |
| CDC CPRA1 (mean, median) | 48, 50 | 26, 3 | 0.02 |
| FCXM CPRA (mean, median) | 80, 89 | 60, 60 | 0.02 |
| Crossmatch Strength: (No. patients) | |||
| CDC+ | 2 | 1 | 1.0 |
| FCXM+ | 9 | 11 | 0.77 |
| FCXM−, DSA+ | 14 | 13 | 1.0 |
| Number of DSAs2 (mean, median) | 2.0, 2.0 | 1.7, 1.0 | 0.59 |
| Donor Age (mean, SD) | 38 ± 12 | 46 ± 11 | 0.03 |
| No. Pre-Transplant Plasmapheresis (mean) | 3.7 | 2.3 | 0.08 |
| No. Post-Transplant Plasmapheresis (mean) | 4.1 | 3.9 | 0.81 |
| anti-CD25 Induction (No. patients, %) | 10 (40%) | 12 (48%) | 0.78 |
| Thymoglobulin Induction (No. patients, %) | 15 (60%) | 13 (52%) | 0.78 |
Calculated panel reactive antibody (CPRA) was determined for HLA-specific antibodies of sufficient strength to yield a positive cytotoxicity (CDC) or flow cytometric crossmatch (FCXM).
Number of donor-specific HLA antibodies (DSAs) prior to desensitization.
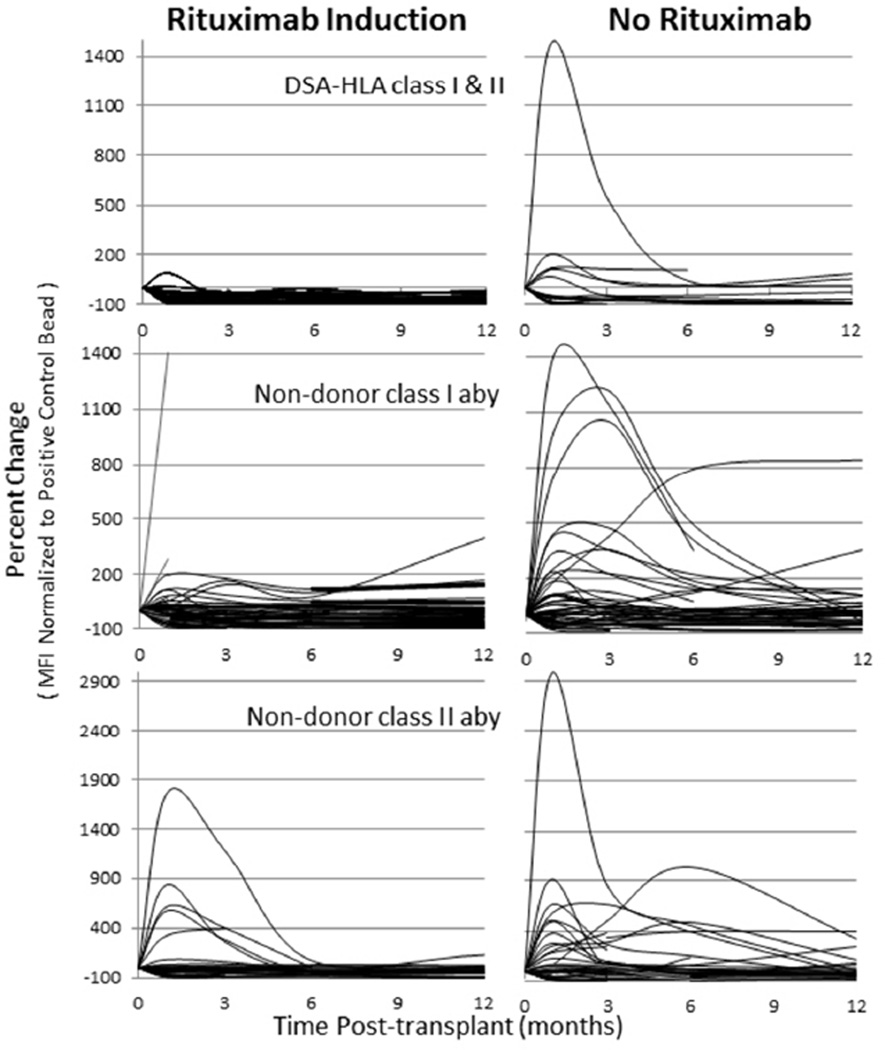
HLA antibody monitoring within the first 2 weeks post-transplant revealed an increase in DSA for 36% (9 of 25) of rituximab-treated patients and in 44% (11 of 25) of non-treated patients transplanted without rituximab (p = 0.77). Elevated DSA was treated with continued plasmapheresis and low dose IVIg; however, all patients completed desensitization treatments within 2 weeks of transplant. An extended analysis was performed on 256 HLA antibodies (DSA and non-DSA) to examine HLA antibody levels following the cessation of plasmapheresis/IVIg treatments. The percent change, comparing HLA antibody levels prior to desensitization (time zero) to four time points (1, 3, 6, 12 months) post-transplant are plotted in Figure 1. The MFI for each antibody was normalized to the positive control bead value, to account for inter-run variability, and the percent change from time zero was calculated. Among rituximab treated patients, 7% (2 of 29) of DSAs examined and 33% (37 of 111) of non-DSAs were increased at one month post-transplant. In patients transplanted without rituximab, more HLA antibodies were increased at one month post-transplant, 32% (8 of 25) of DSAs and 55% (50 of 91) of non-DSAs. The frequency of HLA antibody rebound was significantly higher in patients transplanted without rituximab induction for both DSA, p = 0.03 and non-DSA, p= 0.003. Moreover, the magnitude of the antibody increase was also larger in patients transplanted without rituximab induction. The mean percent increase at one month for all HLA antibodies examined was 294 (median=70) among the lower immunologic risk patients transplanted without rituximab, compared to 207 (median= 10) for those transplanted with rituximab induction (p=0.02).
Figure 1. HLA antibody rebound following HLA-incompatible transplantation: decreased incidence and magnitude in recipients receiving rituximab induction.
HLA antibodies (54 DSA and 202 non-DSA) were measured prior to desensitization (time 0) and at four post-transplant time points (1, 3, 6, 12 months) in patients transplanted with or without rituximab induction. MFI values were normalized to the positive control bead and percent change from time zero was plotted. The incidence of post-transplant DSA (p = 0.03) and non-DSA class I and class II HLA antibody (p= 0.0027) rebound and the magnitude of the antibody rebound (p=0.02) were lower in patients transplanted with rituximab induction compared to those without induction.
In both cohorts, HLA antibody rebounds detected at 1–3 months post-transplant were transient, with 95 of 105 antibodies (90%) subsiding without any further plasmapheresis treatments. Of the 10 DSAs detected at 1 month post-transplant, seven remained at a low level detectable only by bead immunoassays. The remaining three DSAs were of moderate levels, detected at a level sufficient to yield a weakly positive FCXM. These stronger rebounds occurred in three patients, two of which received rituximab induction. Protocol biopsy surveillance at one month identified subclinical rejection (histopathology evidence of AMR without graft dysfunction) in seven patients with DSA rebound, including the three patients with the strongest DSA levels.
Two patients showed no evidence of rejection and one patient, with normal allograft function, was not biopsied due to anticoagulation therapy.
No distinction between HLA class I versus class II specificities was observed in antibodies (DSA or non-DSA) that increased post-transplantation. For rituximab-treated patients, the incidence of non-DSA HLA class I versus class II antibody rebound was 36% and 30%, respectively, and in patients transplanted without rituximab induction, 50% and 62% (Figure 1).
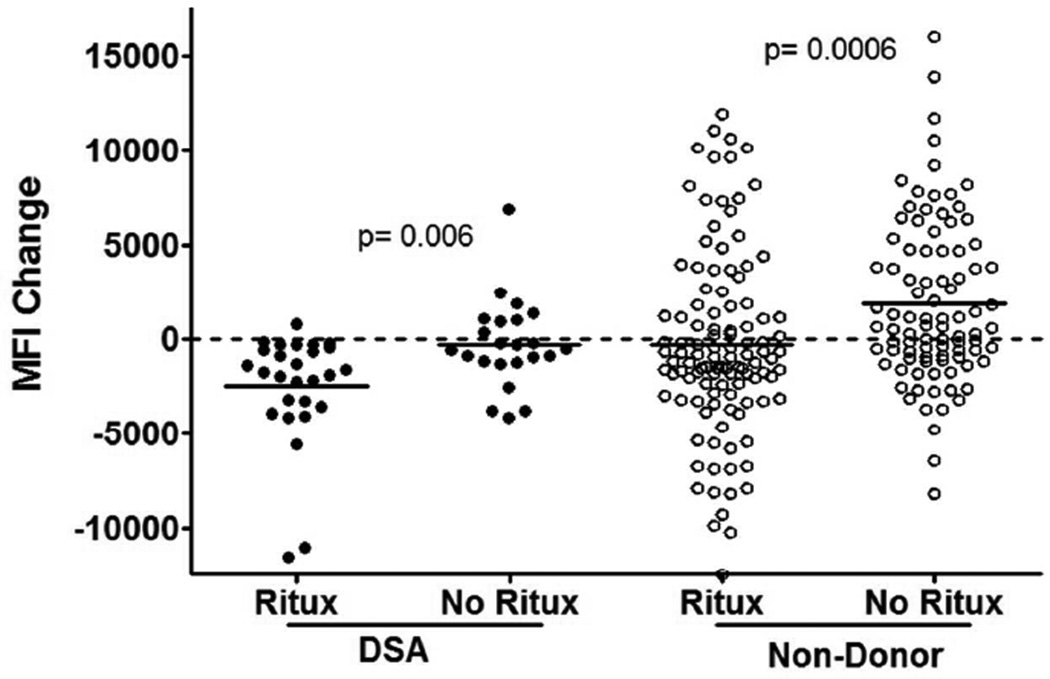
The assessment of HLA antibody levels using a percent-change calculation, which normalizes for inherent test-to-test variability, tends to emphasize changes in weaker antibodies more than strong antibodies. For that reason, we reanalyzed the data calculating the absolute difference in MFI (without normalization) of the pre-desensitization serum and the peak post-transplant serum, with zero representing no change from pre-desensitization baseline levels. Patients transplanted with rituximab induction showed a greater reduction in DSA from baseline levels compared to the control group (−2505 versus −292 MFI, p= 0.006). Rituximab treatment also impacted the mean MFI change of non-DSA HLA antibodies (−309 versus +1938 MFI, p= 0.0006) post-transplantation (Figure 2). Moreover, the impact of rituximab induction to decrease antibody levels was observed across HLA antibodies of different baseline (time zero) levelss (categorized as: weak = MFI < 4000; moderate = MFI 4000–9000; strong = MFI > 9000, data not shown).
Figure 2. Rituximab induction reduces donor-specific (DSA) and non-DSA HLA antibody strength and incidence of rebound post-transplantation.
The change in pre-treatment MFI and peak post-transplant MFI for donor-specific (DSA) and non-DSA HLA antibodies were compared between patients transplanted with or without rituximab induction. Values plotted above dotted line represent a post-transplant antibody rebound above pre-treatment levels. The mean MFI change for DSA (−2505 versus −292, p= 0.006) and for non-DSA HLA antibodies (−309 versus +1938, p= 0.0006) are denoted by solid lines and were statistically lower in patients transplanted with rituximab induction.
Thirteen (52%) of the rituximab-treated recipients and 10 (40%) non-rituximab recipients had detectable DSA at one year post-transplantation. In the majority of these patients (19 of 23), these antibodies were of weak levels and detectable only by bead immunoassays. However in four recipients, three in the rituximab-treated cohort and one in the non-rituximab group, DSA at one year post-transplantation was of moderate levels and directed toward HLA class II antigens. Two of these four patients developed transplant glomerulopathy within two years of transplant, and both had received rituximab induction.
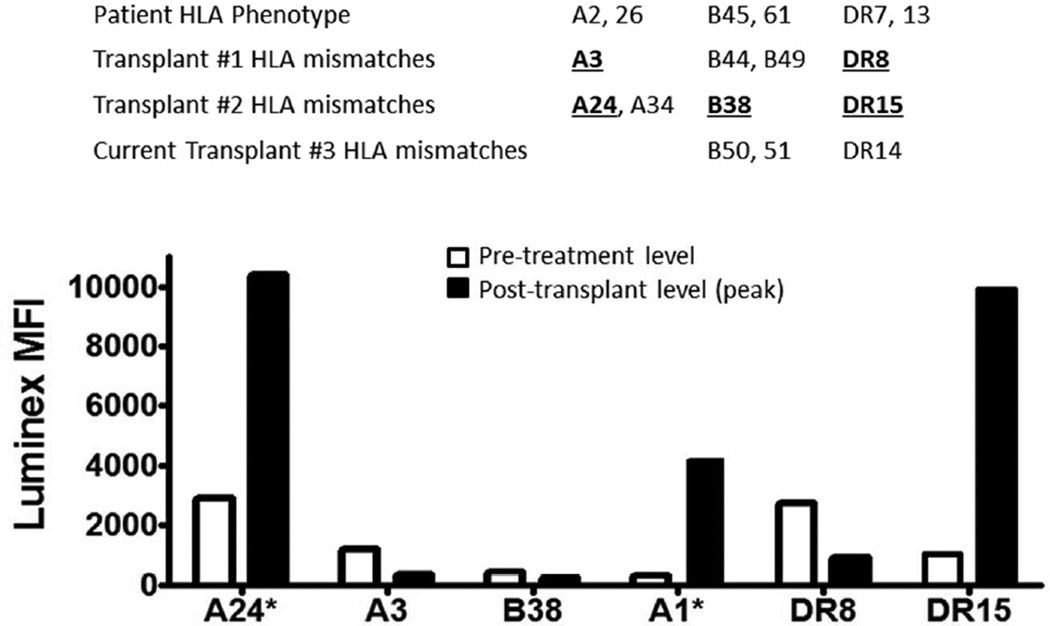
Nine rituximab-treated (36%) and seven (28%) non-rituximab treated patients showed no increase in HLA antibodies post-transplantation. For the remaining patients, post-transplant increases were seen for some but not all HLA antibody specificities. We analyzed factors that may predict which HLA specificities would increase post-transplant and found that baseline levels of the HLA antibodies prior to desensitization was not predictive of post-transplant rebound in either the rituximab treated (p=0.65) or non-rituximab treated (p=0.17) cohorts. Previous HLA mismatches did impact the likelihood of rebound. In 19 rituximab treated patients with previous transplants, 34 of 39 (87%) HLA antibodies that increased post-transplant were specific for HLA epitopes shared with previous allografts or pregnancies. Figure 3 provides a detailed example of post-transplantation HLA antibody increases in a representative rituximab-treated recipient. This patient had no increase in DSA toward his current (3rd) transplant; however, all of the non-DSA HLA antibodies that increased could be attributed to previously mismatched HLA antigens/epitopes.
Figure 3. Post-transplantation HLA antibody rebound reflects previous HLA antigen mismatches but not pre-transplantation baseline HLA antibody strength.
HLA phenotypes for the recipient and three renal allografts are provided. This patient received rituximab induction and experienced rebounds in non-DSA HLA antibodies but no increase in DSA directed toward the current (3rd) allograft. MFI values for HLA antibodies detected prior to desensitization and one month following the 3rd transplantation are shown. All HLA antibodies specific for previous HLA mismatches are shown and the asterisk highlights antibody reactivity toward a known cross-reactive epitope in a previous mismatched antigen (HLA-A1 and HLA-A24).
Post-transplant clinical outcomes and complications are shown in Table 2. The incidence of infection (bacterial, viral, and fungal) during the first year post transplant was 44% in patients treated with rituximab and 28% in non-depleted patients, but this difference was not significant (p= 0.24). The total number of infections was greater in the rituximab treated group (27 versus 10), but reflects multiple infections in a limited number of patients.
Table 2.
Clinical outcomes and complications
| Rituximab N=25 |
No Rituximab N=25 |
p value | ||
|---|---|---|---|---|
| DSA Rebound <2 weeks post-transplant | 0.77 | |||
| No. patients | 9 (36%) | 11 (44%) | ||
| Strength of Rebound: | FCXM+ | 4 (16%) | 5 (20%) | |
| FCXM−, DSA+ | 5 (20%) | 6 (24%) | ||
| DSA Persistence at 1 year: | No. patients | 13 | 10 | 0.57 |
| class I | 4 | 6 | ||
| class II | 5 | 3 | ||
| class I & II | 4 | 1 | ||
| Serum Creatinine (mean ± SD) | ||||
| 1 year | 1.10 ± 0.30 | 1.26 ± 0.39 | 0.21 | |
| 2 year | 1.07 ± 0.22 | 1.28 ± 0.53 | 0.10 | |
| Infections ≤ 1 year | No. patients | 11 | 7 | 0.38 |
| Bacterial | No. infections | 15 | 6 | |
| Viral | 10 | 4 | ||
| Fungal | 2 | 0 | ||
| Total infections | 27 | 10 | 0.08 | |
| Acute rejection1 ≤ 3 months | No. patients | 19 | 14 | 0.23 |
| CMR | No. episodes | 8 | 2 | |
| Subclinical CMR | 4 | 3 | ||
| Total | 12 | 5 | ||
| AMR | 3 | 4 | ||
| Subclinical AMR | 1 | 2 | ||
| Total | 4 | 6 | ||
| Mixed CMR & AMR | 2 | 2 | ||
| Subclinical mixed | 5 | 2 | ||
| Total | 7 | 4 | ||
| Transplant glomerulopathy | ||||
| No. Patients (< 2 years) | 4 | 2 | 0.17 | |
Despite the increased number of immunologic risk factors among rituximab-treated patients, no significant difference was observed in the incidence of acute rejection within the first 3 months of transplant between the cohorts (Rituximab: 76% and No-Rituximab: 56%, p=0.23) (Table 2). Many of these rejection episodes were cellular rejections (28 of 38 were CMR or mixed AMR/CMR) and cellular rejection was more than twice as common in the rituximab treated group (12 versus 5). There were a similar number of episodes of AMR and mixed rejections between the two study groups. Mean serum creatinine values (Table 2) at one and two years post-transplant were 1.10 and 1.07 mg/dL, respectively, in the rituximab-treated cohort and 1.26 and 1.28 mg/dL, respectively, in the non-rituximab cohort (p=0.21 and p=0.10).
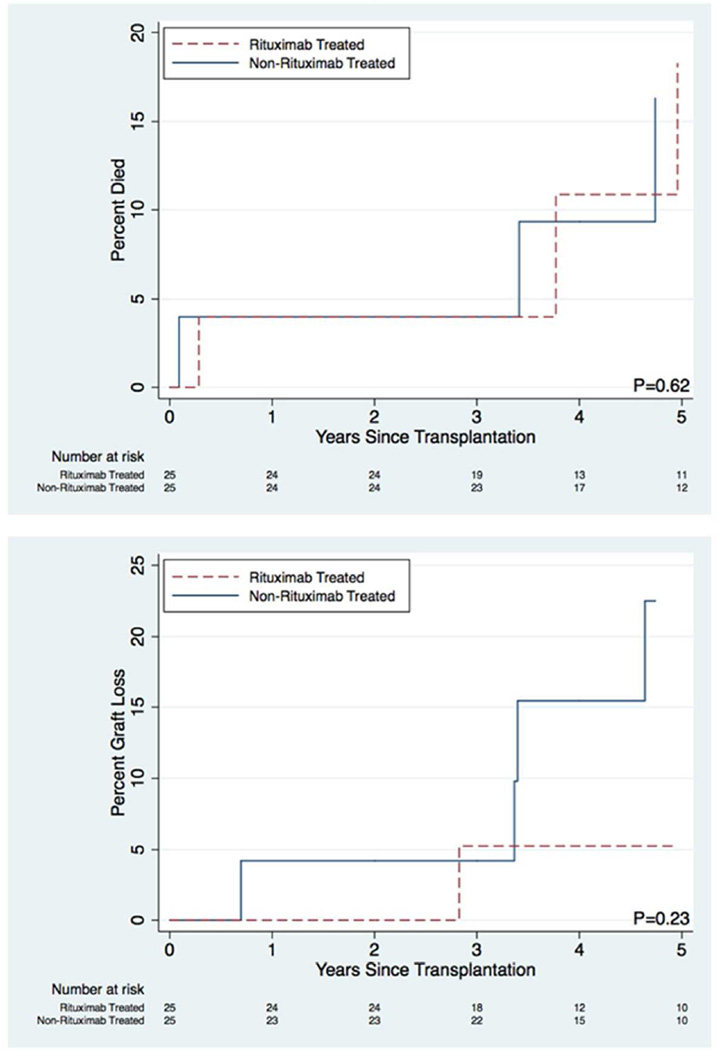
Analysis of patient and graft survival was augmented by linking patients to the Scientific Registry of Transplant Recipients (SRTR) data and Kaplan–Meier method was used to estimate patient and death-censored graft survival at 1 and 5 years post-transplantation (Figure 4). Between-group differences were evaluated using log-rank tested. One and 5-year patient survival were 96.0% and 81.7% in the rituximab treated group and 96.0% and 83.7% in the non-rituximab treated group (P=0.6) (Figure 4A). One and 5-year death-censored graft survival were 100.0% and 94.7% in the rituximab treated group and 95.8% and 77.5% in the non-rituximab treated group (P=0.23) (Figure 4B).
Figure 4. Mortality and death-censored graft loss in the rituximab treated vs. non-rituximab treated cohorts.
Kaplan–Meier estimates of (A) patient 1 and 5-year survival were 96.0% (95% CI: 74.8–99.4%) and 81.7% (95% CI: 51.9–94.0%) in the rituximab treated group and 96.0% (95% CI: 74.8–99.4%) and 83.7% (95% CI: 56.3–94.6%) in the non-rituximab treated group (P=0.6) (B) graft 1 and 5-year death-censored survival were 100.0% and 94.7% (95% CI: 68.0–99.0%) in the rituximab treated group and 95.8% (95% CI: 73.9–99.4%) and 77.5% (95% CI: 49.7–91.1%) in the non-rituximab treated group (P=0.23).
These transplants occurred during a period when we were randomizing patients to receive T cell induction therapy with either anti-interleukin 2 receptor (anti-CD25) or Thymoglobulin. Analysis of post-transplant HLA antibody rebound, infection, and acute rejection did not correlate with the type of T cell induction the patients received.
Discussion
HLA incompatible recipients selected to receive rituximab induction in this study were at higher risk for anamnestic responses due to higher CPRAs, multiple transplants, and repeated HLA mismatches, yet they experienced less HLA antibody rebound (DSA and non-DSA). This reduction in HLA humoral responses, however, did not translate into reduced rates of AMR when compared to patients transplanted without rituximab. Rituximab induction did not significantly impact the persistence of DSA at 1-year post-transplantation; which was detected in 52% of the patients treated with rituximab versus 40% in the non-rituximab treated group. This incidence of DSA persistence following rituximab induction was higher in our study compared to reports by Loupy et al. (28.5%)(14) or Takagi et al. (14%)(25) at one year post-transplantation and likely reflect the increased breadth and strength of HLA sensitization in our patients. No significant difference in renal function was observed at one and two years or graft survival at 5 years post-transplantation between these cohorts. The number of cell-mediated rejections were higher in the rituximab-treated cohort, which may be due to increased allo-sensitization or a consequence of deleting B regulatory cells that serve to restrain effector T cell responses and influence the development of T regulatory cells(29, 30).
Our study is the first to determine the impact of rituximab induction on DSA rebound in patient cohorts receiving the same desensitization regimen without additional B cell depleting therapy.(14, 18,23, 25). Gloor et al. reported decreased but persistent DSA in 10 of 12 HLA incompatible renal recipients at 4 months post-transplant. These recipients were desensitized using a protocol that included plasmapheresis, IVIg, and a single dose of rituximab (375 mg/m2) as induction; however, all recipients also underwent splenectomy prior to transplant. Studies by Hirai et al., Takagi et al., and Loupy et al. compared post-transplant DSA levels in HLA incompatible recipients transplanted following desensitization that included plasmapheresis and rituximab induction to retrospective cohorts transplanted across DSA with no desensitization or in deceased donor transplants using a protocol involving high dose IVIg alone.
HLA antibody rebounds observed at 1–3 months post-transplantation (Figure 1.) were transient and declined without intervention, suggesting that they were generated by newly formed short-lived plasma cells(31, 32). Analysis of both DSA and non-DSA levels post-transplantation confirm that the trauma of surgery and antigenic stimulation of the immune system can elicit both antigen-specific and nonspecific antibody responses(33) and that the current B cell depletion strategies can reduce or blunt but not prevent new HLA antibody production post-transplant. Reducing B cell numbers in sensitized patients prior to the transplant likely decreased the number of HLA specific B cells that could be activated and transformed into antibody-producing plasma cells. Therefore, in the rituximab treated recipients, the new plasma cells likely arose from memory B cells residing in secondary lymphoid niches and protected from depletion(34–38). Examination of the HLA antibody specificities that increased post-transplantation in our rituximab treated patients showed that 34 of 39 were to immunogenic epitopes the patient had been previously exposed to in previous allografts or pregnancies and support the existence of these immune memory reservoirs. These findings suggest a benefit in avoiding repeated HLA antigen mismatches in patients with previous transplants or HLA antigens shared with spouses when transplanting multiparous women, to guard against reactivation of occult sensitization. In such cases, kidney paired donation may offer a mechanism to increase HLA matching between recipient-donor pairs and avoid repeated HLA mismatches.
The increase in some but not all HLA antibody specificities may reflect differences in the amount of B cell memory that exists toward a particular HLA antigen. We have previously shown that the frequency of peripheral blood, HLA-specific B cells, measured using HLA tetramers, reflects prior sensitization to an HLA antigen and predicts a post-transplantation anamnestic response to that antigen in patients with no detectable antibody to that HLA antigen(39). In a subsequent study, we showed that rituximab induction abrogated this anamnestic response(40). In this current study, we show that previous sensitization and not the pre-treatment antibody levels is a better correlate of antibody rebound. This latter finding is also supported by data from Burns et al.(41).
Our findings differ from what has been reported in desensitization protocols performed that utilize B cell depletion to reduce CPRA prior transplantation(8–11). In those studies, rituximab in combination with high dose IVIg produced only transient reductions in some HLA antibodies, primarily those of weaker levels. This current study showcases the impact of desensitization coupled to transplantation in reducing HLA antibodies (DSA and non-DSA) of all levels and, in this setting, the added benefit of B cell depletion. The increased efficacy of rituximab administered at time of transplantation may hinge on increased accessibility to HLA-specific B cells and plasma cells during times of inflammation(42, 43). Increased mobilization of cells from protective niches of the bone marrow occurs in response to inflammation due to reduced CXCL12 retention signals(44). Once in the bloodstream, plasma cells lose necessary signals for long-term survival while cells expressing CD20 become more vulnerable to rituximab depletion and both events likely contribute to the subsequent decline in HLA antibody levels post-transplantation(42, 45).
Similarly, the efficacy of rituximab in the treatment of AMR may also hinge on timing and accessibility to HLA-specific B cells. If rituximab is given early in the immune response, it can reduce the number of mobilized B cells specific for donor HLA antigens, thus minimizing the magnitude of the immune response. However, if rituximab is given after AMR is established, donor-specific B cells may have already transited from the periphery into protected niches within the spleen; where they become resistant to depletion and contribute to the generation of new plasma cells. This latter scenario may explain why splenectomy or bortezimib, and not rituximab, can be more effective in quelling an active alloimmune response after a significant rise in DSA(46, 47).
Our study compared patients desensitized under the same treatment protocol and confirmed the efficacy of rituximab induction in reducing DSA rebound and overall DSA levels post-transplantation. While it seems intuitive that this would translate into lower rates of AMR and better outcomes, this was not observed in this study. The limitations of the study include a nonrandomized methodology, limited clinical follow-up, and an intervention group that contained more re-transplantations and higher baseline CPRA, which could offset the benefits of B cell depletion. In HLA sensitized cohorts, the impact of rituximab induction on transplantation outcomes may depend on individual factors such as the number of donor-specific memory B cells that are sequestered and resistant to depletion and the reserves of donor-specific plasma cells that are not effectively targeted. Therefore, further knowledge regarding the immunogenicity of HLA mismatches and the breadth of immune memory generated following HLA sensitizing events is still needed to assist in risk assessment and aid in donor selection prior to desensitization and transplantation.
Materials and Methods
Patients and Immunosuppression
This is a retrospective analysis of patients transplanted at the Johns Hopkins Hospital within the Incompatible Kidney Transplant Program. The Johns Hopkins Institutional Review Board approved the treatment protocol and use of the prospective clinical database as a research tool. Sequential HLA incompatible live donor renal transplant recipients transplanted between 2006 – 2010 were evaluated. Inclusion criteria required that all plasmapheresis treatments occurred within the first 2 weeks post-transplantation and that the patient received no additional rituximab treatments, splenectomy, or bortezomib. The desensitization protocol included alternate day, single volume plasmapheresis and 100mg/kg intravenous immunoglobulin (IVIg) (Cytogam, MedImmune, Gaithersberg, MD). The number of treatments was determined by the DSA strength prior to transplantation(6). Mycophenolate mofetil (2g/day) and tacrolimus (serum level of 8–10 ng/mL) were initiated with the start of plasmapheresis treatments. Intraoperative induction therapy included anti-IL2 receptor antibody (anti-CD25, daclizumab 2 mg/kg or Thymoglobulin, 1.5mg/kg per day for 5 days). Twenty-five patients with multiple previous transplants, and/or repeat HLA mismatches received a single dose of anti-CD20 antibodies (Rituxan®, 375 mg/m2) on the day prior to transplant. Six of 26 recipients with previous transplants had allograft nephrectomies prior to the current transplant (4 of 19 in the rituximab-treated and 2 of 7 in non-treated recipients).
HLA Antibody Assays
Post-transplant monitoring protocol included alternate day testing for the first two weeks, monthly for three months, and quarterly thereafter. The specificity and level of HLA-specific antibodies were evaluated using HLA phenotype and single antigen bead assays (Lifecodes class I and II ID panels, Immucor Gen-Probe, San Diego, CA and Single Antigen Beads, One Lambda, Canoga Park, CA) performed on a Luminex® platform. High titered sera were tested with and without dilution (1:8) and sera exhibiting high negative controls or a low positive control were treated with hypotonic dialysis prior to testing(48). All HLA antibody specificities that could be clearly delineated on the phenotype panel were selected for year-long analysis. HLA antibody levels were assessed using phenotype bead panels and changes in levels were further verified using single antigen beads. To control for test-to-test variation and the impact of interfering serum factors that can be removed by plasmapheresis, mean fluorescence intensity (MFI) values were normalized to the positive control bead and the fold change from the pre-desensitization time point was calculated:
Percent change = [(Abyn/PCn – Aby0/PC0)/Aby0/PC0] *100
Aby: test bead MFI, PC: positive control bead MFI, n: represents an individual time point (1, 3, 6, or 12 months post-transplant) and 0 represents time-zero prior to desensitization.
Crossmatch tests with donor T and B cells were performed using cytotoxicity and/or flow cytometry as previously described(49, 50). Our positive FCXM threshold correlates with DSA of moderate strength on a HLA phenotype panel (4000–9000 MFI) and a positive CDC-XM correlates with stronger DSA (MFIs > 9000)(51). Calculated panel reactive antibody (CPRA) was determined for antibodies strong enough to yield a positive complement dependent cytotoxicity crossmatch (CDC-XM) and/or flow cytometric crossmatch FCXM was calculated using the online UNOS CPRA calculator(52).
Histopathology and Rejection
Renal allograft biopsies were performed at 1, 3, 6, or 12 months post-transplantation according to protocol and additionally as indicated by dysfunction. C4d deposition was evaluated using indirect immunofluorescence. Presence of cell mediated rejection (CMR), AMR, mixed or subclinical rejection was determined using updated Banff ’97 criteria(53–56).
Statistical Methods
Kaplan–Meier method and the log-rank test were used to estimate survival in treatment groups and compare differences between groups, respectively. Patients were linked to the SRTR to allow death ascertainment from the Centers for Medicare and Medicaid Services. SRTR includes information on all donors, wait-listed transplant candidates, and transplant recipients in the U.S. provided by members of the Organ Procurement and Transplantation Network. The Health Resources and Services Administration, U.S. Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. Death-censored graft survival was defined as the time between transplant date and either graft failure date (marked by retransplantation, relisting, or a return to dialysis) or last follow-up date with a functioning graft, censoring for death and administrative end of study. Survival analyses were performed using Stata 12.0. Summary statistics including mean, median, and standard deviation were calculated using Microsoft Excel. Statistical significance was determined using Chi squared and Student’s t test (two tailed), with a p-value <0.05 considered statistically significant.
Acknowledgements
The data reported here have been supplied by the Minneapolis Medical Research Foundation (MMRF) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government. We also thank J. Houp for assistance with CPRA calculations.
Funding: Supported by a grant (R01 DK098431 and RC1 DK086731) from the National Institute of Diabetes and Digestive and Kidney Diseases and by the Charles T. Bauer Foundation (R.M.).
Footnotes
Disclosures
All the authors declared no competing interests.
References
- 1.Maloney DG, Liles TM, Czerwinski DK, et al. Phase I clinical trial using escalating single-dose infusion of chimeric anti-CD20 monoclonal antibody (IDEC-C2B8) in patients with recurrent B-cell lymphoma. Blood. 1994;84:2457–2466. [PubMed] [Google Scholar]
- 2.Edwards JC, Szczepanski L, Szechinski J, et al. Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350:2572–2581. doi: 10.1056/NEJMoa032534. [DOI] [PubMed] [Google Scholar]
- 3.Looney RJ, Anolik JH, Campbell D, et al. B cell depletion as a novel treatment for systemic lupus erythematosus: a phase I/II dose-escalation trial of rituximab. Arthritis Rheum. 2004;50:2580–2589. doi: 10.1002/art.20430. [DOI] [PubMed] [Google Scholar]
- 4.Aranda JM, Jr, Scornik JC, Normann SJ, et al. Anti-CD20 monoclonal antibody (rituximab) therapy for acute cardiac humoral rejection: a case report. Transplantation. 2002;73:907–910. doi: 10.1097/00007890-200203270-00013. [DOI] [PubMed] [Google Scholar]
- 5.Sawada T, Fuchinoue S, Teraoka S. Successful A1-to-O ABO-incompatible kidney transplantation after a preconditioning regimen consisting of anti-CD20 monoclonal antibody infusions, splenectomy, and double-filtration plasmapheresis. Transplantation. 2002;74:1207–1210. doi: 10.1097/00007890-200211150-00001. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery RA, Zachary AA. Transplanting patients with a positive donor-specific crossmatch: a single center's perspective. Pediatr Transplant. 2004;8:535–542. doi: 10.1111/j.1399-3046.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 7.Becker YT, Becker BN, Pirsch JD, Sollinger HW. Rituximab as treatment for refractory kidney transplant rejection. Am J Transplant. 2004;4:996–1001. doi: 10.1111/j.1600-6143.2004.00454.x. [DOI] [PubMed] [Google Scholar]
- 8.Vo AA, Peng A, Toyoda M, et al. Use of intravenous immune globulin and rituximab for desensitization of highly HLA-sensitized patients awaiting kidney transplantation. Transplantation. 2010;89:1095–1102. doi: 10.1097/TP.0b013e3181d21e7f. [DOI] [PubMed] [Google Scholar]
- 9.Kozlowski T, Andreoni K. Limitations of rituximab/IVIg desensitization protocol in kidney transplantation; is this better than a tincture of time? Ann Transplant. 2011;16:19–25. doi: 10.12659/aot.881860. [DOI] [PubMed] [Google Scholar]
- 10.Marfo K, Ling M, Bao Y, et al. Lack of effect in desensitization with intravenous immunoglobulin and rituximab in highly sensitized patients. Transplantation. 2012;94:345–351. doi: 10.1097/TP.0b013e3182590d2e. [DOI] [PubMed] [Google Scholar]
- 11.Lobashevsky AL, Higgins NG, Rosner KM, et al. Analysis of anti-HLA antibodies in sensitized kidney transplant candidates subjected to desensitization with intravenous immunoglobulin and rituximab. Transplantation. 2013;96:182–190. doi: 10.1097/TP.0b013e3182962c84. [DOI] [PubMed] [Google Scholar]
- 12.Gloor JM, DeGoey SR, Pineda AA, et al. Overcoming a positive crossmatch in living-donor kidney transplantation. Am J Transplant. 2003;3:1017–1023. doi: 10.1034/j.1600-6143.2003.00180.x. [DOI] [PubMed] [Google Scholar]
- 13.Tyden G, Genberg H, Tollemar J, et al. A randomized, doubleblind, placebo-controlled, study of single-dose rituximab as induction in renal transplantation. Transplantation. 2009;87:1325–1329. doi: 10.1097/TP.0b013e3181a235fd. [DOI] [PubMed] [Google Scholar]
- 14.Loupy A, Suberbielle-Boissel C, Zuber J, et al. Combined posttransplant prophylactic IVIg/anti-CD 20/plasmapheresis in kidney recipients with preformed donor-specific antibodies: a pilot study. Transplantation. 2010;89:1403–1410. doi: 10.1097/TP.0b013e3181da1cc3. [DOI] [PubMed] [Google Scholar]
- 15.Zarkhin V, Li L, Kambham N, et al. A randomized, prospective trial of rituximab for acute rejection in pediatric renal transplantation. Am J Transplant. 2008;8:2607–2617. doi: 10.1111/j.1600-6143.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaposztas Z, Podder H, Mauiyyedi S, et al. Impact of rituximab therapy for treatment of acute humoral rejection. Clin Transplant. 2009;23:63–73. doi: 10.1111/j.1399-0012.2008.00902.x. [DOI] [PubMed] [Google Scholar]
- 17.Lefaucheur C, Nochy D, Andrade J, et al. Comparison of combination Plasmapheresis/IVIg/anti-CD20 versus high-dose IVIg in the treatment of antibody-mediated rejection. Am J Transplant. 2009;9:1099–1107. doi: 10.1111/j.1600-6143.2009.02591.x. [DOI] [PubMed] [Google Scholar]
- 18.Gloor JM, DeGoey S, Ploeger N, et al. Persistence of low levels of alloantibody after desensitization in crossmatch-positive living-donor kidney transplantation. Transplantation. 2004;78:221–227. doi: 10.1097/01.tp.0000128516.82593.47. [DOI] [PubMed] [Google Scholar]
- 19.Vo AA, Lukovsky M, Toyoda M, et al. Rituximab and intravenous immune globulin for desensitization during renal transplantation. N Engl J Med. 2008;359:242–251. doi: 10.1056/NEJMoa0707894. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery RA, Locke JE, King KE, et al. ABO Incompatible Renal Transplantation: A Paradigm Ready for Broad Implementation. Transplantation. 2009;87:1246–1255. doi: 10.1097/TP.0b013e31819f2024. [DOI] [PubMed] [Google Scholar]
- 21.Montgomery RA, Lonze BE, King KE, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365:318–326. doi: 10.1056/NEJMoa1012376. [DOI] [PubMed] [Google Scholar]
- 22.Morath C, Beimler J, Opelz G, et al. Living donor kidney transplantation in crossmatch-positive patients enabled by peritransplant immunoadsorption and anti-CD20 therapy. Transpl Int. 2012;25:506–517. doi: 10.1111/j.1432-2277.2012.01447.x. [DOI] [PubMed] [Google Scholar]
- 23.Hirai T, Kohei N, Omoto K, et al. Significance of low-level DSA detected by solid-phase assay in association with acute and chronic antibody-mediated rejection. Transpl Int. 2012;25:925–934. doi: 10.1111/j.1432-2277.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- 24.Kohei N, Hirai T, Omoto K, et al. Chronic antibody-mediated rejection is reduced by targeting B-cell immunity during an introductory period. Am J Transplant. 2012;12:469–476. doi: 10.1111/j.1600-6143.2011.03830.x. [DOI] [PubMed] [Google Scholar]
- 25.Takagi T, Ishida H, Shirakawa H, et al. Changes in anti-HLA antibody titers more than 1 year after desensitization therapy with rituximab in living-donor kidney transplantation. Transpl Immunol. 2010;23:220–223. doi: 10.1016/j.trim.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Roberts DM, Jiang SH, Chadban SJ. The treatment of acute antibody-mediated rejection in kidney transplant recipients-a systematic review. Transplantation. 2012;94:775–783. doi: 10.1097/TP.0b013e31825d1587. [DOI] [PubMed] [Google Scholar]
- 27.Susal C, Dohler B, Opelz G. Presensitized kidney graft recipients with HLA class I and II antibodies are at increased risk for graft failure: a Collaborative Transplant Study report. Hum Immunol. 2009;70:569–573. doi: 10.1016/j.humimm.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 28.Morath C, Opelz G, Zeier M, Susal C. Kidney transplantation for high-risk sensitized patients - the "Heidelberg algorithm". Transplant Proc. 2011;43:801–804. doi: 10.1016/j.transproceed.2011.02.074. [DOI] [PubMed] [Google Scholar]
- 29.Mauri C, Bosma A. Immune regulatory function of B cells. Annu Rev Immunol. 2012;30:221–241. doi: 10.1146/annurev-immunol-020711-074934. [DOI] [PubMed] [Google Scholar]
- 30.Lemoine S, Morva A, Youinou P, Jamin C. Human T cells induce their own regulation through activation of B cells. J Autoimmun. 2011;36:228–238. doi: 10.1016/j.jaut.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Stegall MD, Moore N, Taner T, et al. Down-Regulating Humoral Immune Responses: Implications for Organ Transplantation. Transplantation. 2013 doi: 10.1097/TP.0b013e3182a72115. [DOI] [PubMed] [Google Scholar]
- 32.Tangye SG. Staying alive: regulation of plasma cell survival. Trends Immunol. 2011;32:595–602. doi: 10.1016/j.it.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 33.Locke JE, Zachary AA, Warren DS, et al. Proinflammatory events are associated with significant increases in breadth and strength of HLA-specific antibody. Am J Transplant. 2009;9:2136–2139. doi: 10.1111/j.1600-6143.2009.02764.x. [DOI] [PubMed] [Google Scholar]
- 34.Ellyard JI, Avery DT, Phan TG, et al. Antigen-selected, immunoglobulin-secreting cells persist in human spleen and bone marrow. Blood. 2004;103:3805–3812. doi: 10.1182/blood-2003-09-3109. [DOI] [PubMed] [Google Scholar]
- 35.Genberg H, Hansson A, Wernerson A, et al. Pharmacodynamics of rituximab in kidney transplantation. Transplantation. 2007;84:S33–S36. doi: 10.1097/01.tp.0000296122.19026.0f. [DOI] [PubMed] [Google Scholar]
- 36.Ramos EJ, Pollinger HS, Stegall MD, et al. The effect of desensitization protocols on human splenic B-cell populations in vivo. Am J Transplant. 2007;7:402–407. doi: 10.1111/j.1600-6143.2006.01632.x. [DOI] [PubMed] [Google Scholar]
- 37.DiLillo DJ, Hamaguchi Y, Ueda Y, et al. Maintenance of long-lived plasma cells and serological memory despite mature and memory B cell depletion during CD20 immunotherapy in mice. J Immunol. 2008;180:361–371. doi: 10.4049/jimmunol.180.1.361. [DOI] [PubMed] [Google Scholar]
- 38.Stegall MD, Dean PG, Gloor J. Mechanisms of alloantibody production in sensitized renal allograft recipients. Am J Transplant. 2009;9:998–1005. doi: 10.1111/j.1600-6143.2009.02612.x. [DOI] [PubMed] [Google Scholar]
- 39.Zachary AA, Kopchaliiska D, Montgomery RA, et al. HLA-specific B cells: II. Application to transplantation. Transplantation. 2007;83:989–994. doi: 10.1097/01.tp.0000259019.68244.d7. [DOI] [PubMed] [Google Scholar]
- 40.Zachary AA, Lucas DP, Montgomery RA, Leffell MS. Rituximab Prevents an Anamnestic Response in Patients With Cryptic Sensitization to HLA. Transplantation. 2013;95:701–704. doi: 10.1097/TP.0b013e31827be3c1. [DOI] [PubMed] [Google Scholar]
- 41.Burns JM, Cornell LD, Perry DK, et al. Alloantibody levels and acute humoral rejection early after positive crossmatch kidney transplantation. Am J Transplant. 2008;8:2684–2694. doi: 10.1111/j.1600-6143.2008.02441.x. [DOI] [PubMed] [Google Scholar]
- 42.Odendahl M, Mei H, Hoyer BF, et al. Generation of migratory antigen-specific plasma blasts and mobilization of resident plasma cells in a secondary immune response. Blood. 2005;105:1614–1621. doi: 10.1182/blood-2004-07-2507. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez-Garcia I, Ocana E, Jimenez-Gomez G, et al. Immunization-induced perturbation of human blood plasma cell pool: progressive maturation, IL-6 responsiveness, and high PRDI-BF1/BLIMP1 expression are critical distinctions between antigen-specific and nonspecific plasma cells. J Immunol. 2006;176:4042–4050. doi: 10.4049/jimmunol.176.7.4042. [DOI] [PubMed] [Google Scholar]
- 44.Ueda Y, Yang K, Foster SJ, et al. Inflammation controls B lymphopoiesis by regulating chemokine CXCL12 expression. J Exp Med. 2004;199:47–58. doi: 10.1084/jem.20031104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yoshida T, Mei H, Dorner T, et al. Memory B and memory plasma cells. Immunol Rev. 2010;237:117–139. doi: 10.1111/j.1600-065X.2010.00938.x. [DOI] [PubMed] [Google Scholar]
- 46.Tzvetanov I, Spaggiari M, Oberholzer J, et al. Cell population in spleens during antibody-mediated rejection: pathologic and clinical findings. Transplantation. 2012;94:255–262. doi: 10.1097/TP.0b013e3182562881. [DOI] [PubMed] [Google Scholar]
- 47.Waiser J, Budde K, Schutz M, et al. Comparison between bortezomib and rituximab in the treatment of antibody-mediated renal allograft rejection. Nephrol Dial Transplant. 2012;27:1246–1251. doi: 10.1093/ndt/gfr465. [DOI] [PubMed] [Google Scholar]
- 48.Zachary AA, Lucas DP, Detrick B, Leffell MS. Naturally occurring interference in Luminex assays for HLA-specific antibodies: characteristics and resolution. Hum Immunol. 2009;70:496–501. doi: 10.1016/j.humimm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Hetrick SJ, Schillinger KP, Zachary AA, Jackson AM. Impact of pronase on flow cytometric crossmatch outcome. Hum Immunol. 2011;72:330–336. doi: 10.1016/j.humimm.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Hopkins KA. The basic lymphocyte microcytotoxicity tests: standard and AHG enhancement. In: Hahn AB, Land GA, Strothman RM, editors. The ASHI Laboratory Manual. Mt. Laurel, NJ: 2000. p. 1.C.1.1. [Google Scholar]
- 51.Zachary AA, Sholander JT, Houp JA, Leffell MS. Using real data for a virtual crossmatch. Hum Immunol. 2009;70:574–579. doi: 10.1016/j.humimm.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 52.CPRA Calculator: Organ Procurement and Transplantation Network. 2014 Feb [Google Scholar]
- 53.Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8:753–760. doi: 10.1111/j.1600-6143.2008.02159.x. [DOI] [PubMed] [Google Scholar]
- 54.Racusen LC, Colvin RB, Solez K, et al. Antibody-mediated rejection criteria - an addition to the Banff 97 classification of renal allograft rejection. Am J Transplant. 2003;3:708–714. doi: 10.1034/j.1600-6143.2003.00072.x. [DOI] [PubMed] [Google Scholar]
- 55.Mengel M, Sis B, Haas M, et al. Banff 2011 Meeting report: new concepts in antibody-mediated rejection. Am J Transplant. 2012;12:563–570. doi: 10.1111/j.1600-6143.2011.03926.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kraus ES, Parekh RS, Oberai P, et al. Subclinical Rejection in Stable Positive Crossmatch Kidney Transplant Patients: Incidence and Correlations. American Journal of Transplantation. 2009;9:1826–1834. doi: 10.1111/j.1600-6143.2009.02701.x. [DOI] [PubMed] [Google Scholar]