Abstract
Web educational resources integrating interactive simulation tools provide students with an in-depth understanding of the medical imaging process. The aim of this work was the development of a purely Web-based, open access, interactive application, as an ancillary learning tool in graduate and postgraduate medical imaging education, including a systematic evaluation of learning effectiveness. The pedagogic content of the educational Web portal was designed to cover the basic concepts of medical imaging reconstruction and processing, through the use of active learning and motivation, including learning simulations that closely resemble actual tomographic imaging systems. The user can implement image reconstruction and processing algorithms under a single user interface and manipulate various factors to understand the impact on image appearance. A questionnaire for pre- and post-training self-assessment was developed and integrated in the online application. The developed Web-based educational application introduces the trainee in the basic concepts of imaging through textual and graphical information and proceeds with a learning-by-doing approach. Trainees are encouraged to participate in a pre- and post-training questionnaire to assess their knowledge gain. An initial feedback from a group of graduate medical students showed that the developed course was considered as effective and well structured. An e-learning application on medical imaging integrating interactive simulation tools was developed and assessed in our institution.
Keywords: Web-based education, Simulation, Reconstruction, FBP, Iterative algorithm, Medical imaging, Image processing, Filter, CT, SPECT
Background
Medical imaging has evolved into a key component of both clinical and research laboratories. Clinical applications include diagnosis, treatment planning, and surgical guidance. Continued imaging innovation has augmented the versatility of medical image reconstruction, processing and storage alternatives that need to be swiftly assimilated by medical practitioners and medical auxiliaries. Raising the level of future professionals training to keep up with the rapid developments in the field thus becomes more and more important, as does the need for a comprehensive medical imaging education program.
The majority of studies on learning outcomes suggest that Web-based educational interventions are effective in enhancing knowledge, attitudinal, and, to a lesser extent, skill domains [1, 2]. Web content adds graphics, sound, and video, so as to give teachers and trainees multiple paths for teaching and understanding. Information can be presented interactively, and trainees can choose the time, place, and pace of learning [3–5]. Hyper-textbooks are a source of online education that provides additional multimedia elements, as opposed to traditional textbooks [4, 5]. However, hyper-textbooks do not offer interactive computational modules that provide users with the imaging algorithms used in the various medical imaging modalities. The literature offers an increased number of articles for Web-based medical education, but only a few of them are medical-imaging-oriented, while less provide the combination of text explanations, animations, and simulations [1–3, 6–16, 20]. These references are of little help to most persons who lack the mathematical perception of physicists and engineers.
In an effort to address these aspects, we developed an open access purely Web-based, interactive educational application with simulation and self-assessment features, for training medical students, physicists, and engineers studying medical physics and radiology residents, on the basic concepts of medical image reconstruction and processing. Effort was also made to include in the developed educational application hands-on experimentation to the trainees in order to enhance their understanding of how medical images are formed and processed. A multiple choice questionnaire regarding the content material of the course has been incorporated in the Web-based platform, so that the user can self-evaluate his or her knowledge on the referred topics.
Materials and Methods
Design Considerations
The educational content of the online course focuses on the reconstruction and processing of medical images rather than on case-based medical instruction [3, 17, 18]. The educational platform has been designed to include the following features: (1) the basic concepts of the Digital Imaging and Communications in Medicine (DICOM) protocol [19] for storing and transferring medical images, (2) the principles of acquiring projections forming the sinogram of an imaged object, (3) the principles of reconstructing tomographic images from their projections using either the filtered back projection (FBP) or iterative reconstruction (IR) methods [20, 21], and (4) image processing using (a) the information from the corresponding intensity histogram and (b) a number of filters applied in the spatial or frequency domains [11]. A number of options were provided for assisting users in the understanding of the parameters that affect medical image quality, quantified using the modulation transfer function (MTF) [23].
The structure of the course has been designed to present the basic topics of medical imaging in a short and intuitive way before proceeding to interactive image reconstruction and image processing. The design of the application is characterized by the degree of flexibility necessary to present the user with the option to navigate through the above-mentioned three pedagogic sessions as well as in between them, thus allowing learners to skip information they already know and move on to subjects they are less familiar with.
The referenced methods for acquiring medical images are tomographic systems of Radiology and Nuclear Medicine. While a number of phantom images (test objects) are included in the simulation tool to facilitate understanding of the studied topics, the users are also able to upload their images in DICOM format.
Password-protected access was chosen mainly to permit the creation of user profiles for the tracking of self-improvement. Emphasis has been given to the simplicity, time efficiency, and privacy protection of the account creation procedure.
Developing the Web-Based Educational Platform
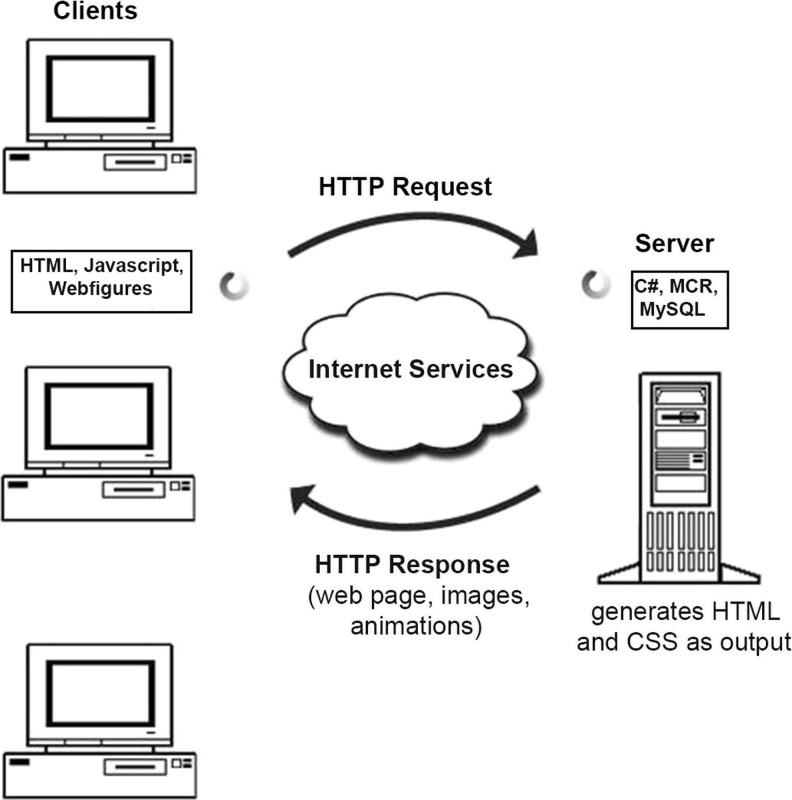
Effective online learning requires the developer to carefully construct a program that integrates principles of active learning, motivation, and evaluation with creative Web design [24]. The interactive Web portal has been developed to host the educational application, based on the system architecture of a server and a client layer (Fig. 1) and consists of 52 Web pages. The server receives requests through the client Web browser over the internet using the Internet Information Services (IIS). The Web server is responsible for handling all the requests that are coming from clients. When a request comes from client to server, IIS takes that request, processes it, and sends a response back to the client.
Fig. 1.
The architecture of a MCR server and a client layer over the internet used for developing the online educational application
If the request includes graphics processing, the IIS calls one of the 83 customized computational modules developed in house using MATLAB® [25] to handle it. Similar work has been also performed by Wu et al. [15] and Dikshit et al. [16], who developed an intuitive interactive curriculum for Miami University, USA, using MATLAB Web Server software. As of MATLAB Release 2006b, MATLAB Web Server was discontinued and Mathworks no longer supports the Web server. Our interactive platform is based on server-side .NET components created by MATLAB Deployment Tool and incorporated in the developed .NET Web application. The framework .NET stands for the software package that provides language and service interoperability. Two different programming languages were used to manage the webpage interactivity. C# code handles server-side functions, while JavaScript code performs client-side functions. Client data, like the user profile, is stored in a linked server database using structured query language (SQL) [26]. All educational graphics and animations were designed or formatted by MATLAB Image Processing Toolbox and along with several interactive tools of image processing and reconstruction are accessible to everyone. These technologies were appropriately combined to achieve real-time interactivity and simulation.
Self-Evaluation
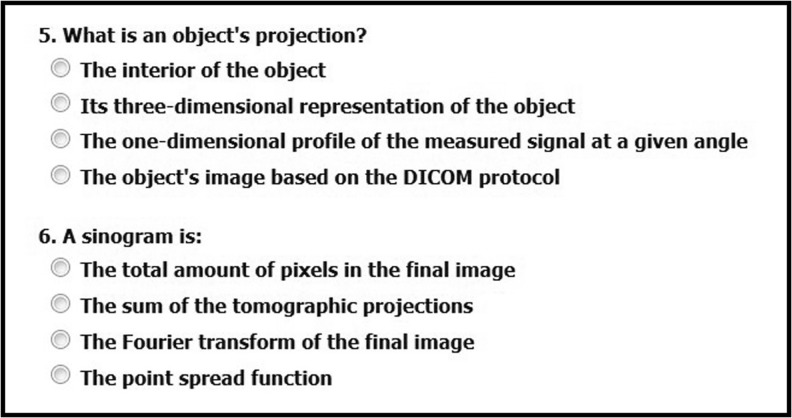
Based on the educational content of the online course, a 22-question multiple choice quiz has been integrated in the Web platform of the application. The questions of the multiple choice quiz have been strategically chosen to evaluate in-depth understanding of the course content (Fig. 2). The learners are advised to take the same multiple choice questionnaire pre- and post-training (maximum allowed time is 22 min or 1 min per question on average). The number of times that the learner can answer the questionnaire is not constrained by the educational tool. The score of the learner each time he or she takes the questionnaire is stored in the database and can be used for self-assessment of the gained knowledge.
Fig. 2.
A sample of the online self-assessment questionnaire
Results
Interacting with the Online Application
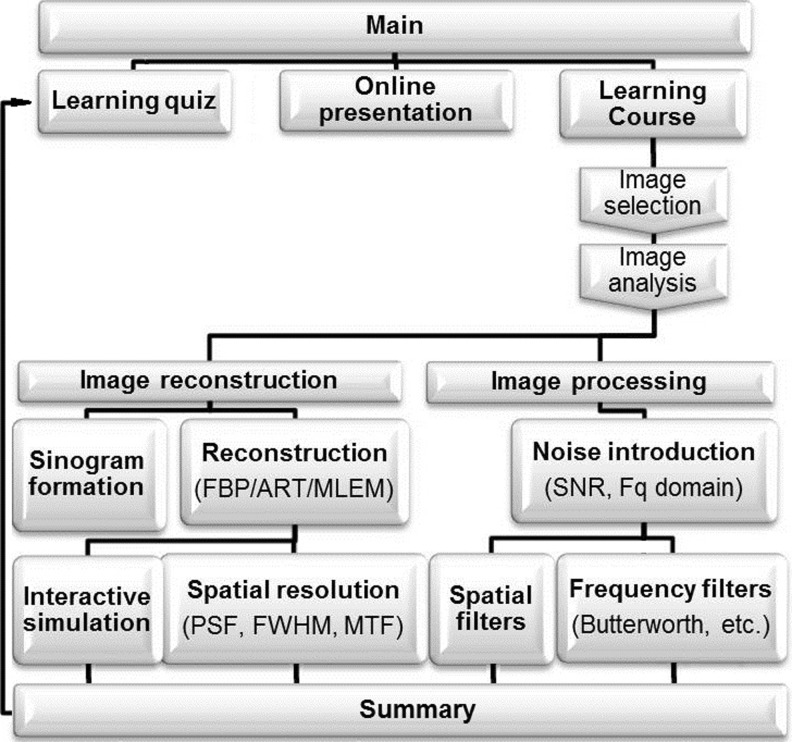
The medical imaging Web portal can be accessed at http://medicalimaging.med.uoa.gr. At the starting page, the user is prompted to a simple initialization process of about 3 min to create a new account. After log-in, the user can either choose to preview the online presentation of an introduction to medical imaging of about 10 min or to navigate through the website and interact with the simulation tools. The educational path of the online application is presented in Fig. 3. Initially, the learner is given the ability to choose a patient image obtained using a tomographic system of Radiology or Nuclear Medicine, anonymized, and stored in DICOM format in the server, an image from a set of test objects created in house, or upload one from his or her personal computer. The basic tags (e.g., characteristics of imaging system, pixel size, etc.) [19], included in the header of the image file, are presented. For a better understanding of these concepts, the Web portal provides a simultaneous viewing of the selected image, the numerical values of the image pixels in a matrix, and a graph of the image histogram as well as information from the image metadata. The application analyzes all the pixels to provide image characteristics such as the highest, lowest, and mean values of the image brightness, followed by the image contrast (Michelson-based contrast measure [26]).
Fig. 3.
A graphical representation of the website flowchart. After log-in, the users can choose between three learning modalities: the learning quiz, the online presentation, and the interactive application
The educational environment has been designed to cover the main topics in medical imaging and explain not only post-acquisition image processing fundamentals but also the actual process of generating medical images.
Reconstruction Methods
The registered signal varies in each imaging modality ranging from X-ray attenuation in X-ray transmission computed tomography (CT) to radionuclide distribution in nuclear medicine positron emission tomography (PET) or single photon emission tomography (SPECT) and frequency and phase-encoded radio-frequency (RF) information in magnetic resonance imaging (MRI) [27]. On the contrary, the reconstruction of the sampled information to form trans-axial images is performed using techniques based on the same principles in all these imaging modalities.
The objective of this educational section is to provide an overview of the most common reconstruction methods, not only using text but also employing animations and simulations for a better understanding. The educational application presents and applies filtered back projection (FBP) and the most commonly used iterative reconstruction algorithms (IR): maximum likelihood expectation maximization (MLEM) and algebraic reconstruction technique (ART) [1, 20]. Iterative reconstruction methods allow the incorporation of imaging models more accurately than the Radon model assumed in the FBP algorithm [27].
The developed application provides a sinogram (Radon transform data) under the assumption that the selected image represents a cross-section of the theoretically scanned physical object. The simulation creates a parallel-beam transformation of the initial image and then calls the selected reconstruction algorithm to recreate the initial image from the transformation. This technique is commonly used to test reconstruction algorithms [28].
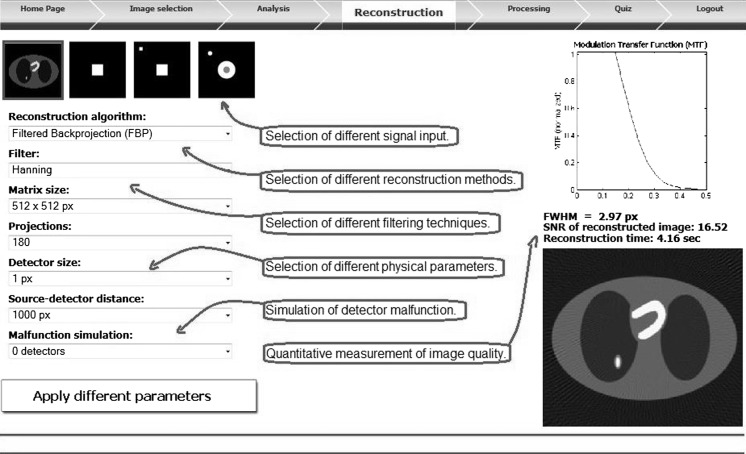
Facilitating insight to the similarities and differences of the image reconstruction methods, the user can reconstruct the same object with all the reconstruction methods with control over a number of parameters including detector size, matrix size, iteration number, and filter type (Fig. 4). The effect of missing data (i.e., projections) in the measured sinogram, caused by a possible detector malfunction during image acquisition, on the reconstructed image has been also included in the website. During reconstruction, the developed application performs common methods of image and system quality control of the simulated tomographic system, so that the user can compare the result of different geometries and reconstruction parameters both visually and quantitatively [27, 29].
Fig. 4.
A snapshot of the interactive simulation of reconstruction methods. The arrangement of the objects in the screenshot has been slightly changed relative to the site to facilitate presentation
Image Processing
The developed application uses a learning-by-doing method to provide understanding of the histogram manipulation and image filtering in the spatial and frequency domain manipulation techniques, commonly used in medical imaging [22].
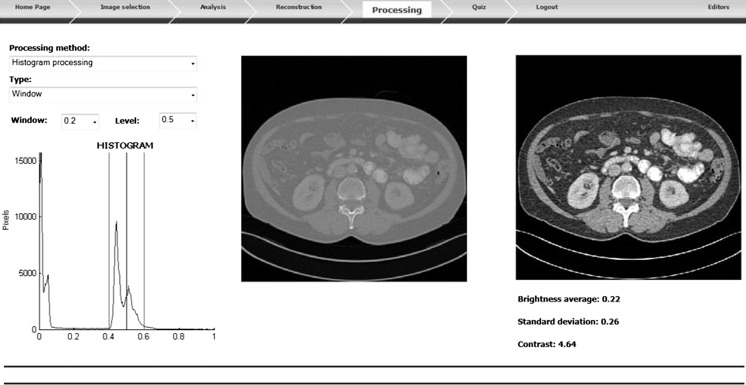
Histogram processing consists of a collection of techniques, such as windowing, normalization, and equalization. Besides explanatory text with figures for each method, the user can interactively delineate the differences of the various techniques by applying each one to the selected image. When windowing is selected, a desired range of intensity values in the output image can be specified, so that the data values are remapped to fill the entire intensity range (Fig. 5). The process of adjusting intensity values can be done automatically by the normalization and equalization method. Besides the visual result, the histogram of the original and the processed image appears after each method application.
Fig. 5.
A snapshot of a histogram windowing example. The arrangement of the objects in the screenshot has been slightly changed relative to the site to facilitate presentation
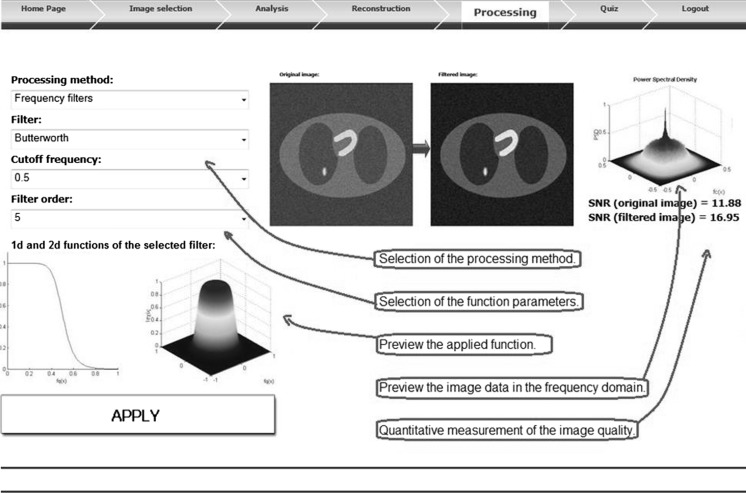
The developed educational Web portal provides the tools to introduce the learner to image filters in both the spatial and frequency domains and presents some filters with equivalents in both domains [22, 27]. The frequency filters are applied in the frequency domain of an image and can manipulate the spatial frequency components independently. The educational website presents an ideal filter and provides the testing of the most common frequency filters found in medical imaging systems of Radiology and Nuclear Medicine departments [22, 27]: Gaussian, Butterworth, Hanning, Hamming, Shepp-Logan, Cosine, Blackman, and Parzen filters.
Random noise can be added to the initial image by selecting the desired signal-to-noise ratio (SNR) of the resulting image, so that the effect of the filters can be better discerned. When the user chooses a filter and selects the desired parameters, a graphical representation of the filter’s function is shown. After applying the filter to the image, the user is able to observe the final image, the suppressed information, and their graphical representations in the frequency domain (Fig. 6).
Fig. 6.
A snapshot of a frequency filtering example. The arrangement of the objects in the screenshot has been slightly changed relative to the site to facilitate presentation
The same pattern is also used in the case of the spatial (average, median, Gaussian) and edge enhancement (Sobel, Perwitt, Laplacian, LoG) filters of the educational application [22]. Trainees responded favorably to the interactive processing methods and noted that these methods stimulate learning by reinforcing current knowledge and by highlighting differences between the processing techniques.
Image-Quality Assessment
In general, the most important factors associated with medical image quality are noise, spatial resolution, and contrast [29]. A common way to quantify the level of noise in an image is to estimate the SNR. The developed educational application has the inherent advantage of knowing the original signal, since it uses an initial image to apply the reconstruction and processing methods. In the section on reconstruction, the original signal is the selected image, while in the image processing section, the original signal is the image before the addition of noise. The subtraction of the original and the resulting image matrix is considered as noise, and the SNR is obtained easily.
Conversely, spatial resolution describes the size of the smallest objects that can be discerned as separate by an imaging system. Instead of attempting to define spatial resolution with minimum object size parameter, it is better to describe the way the contrast of an imaged object is lost in the imaging system as spatial frequency increases [27]. This is commonly performed using the modulation transfer function (MTF) [23]. During the reconstruction of a selected object, the developed educational tool simultaneously reconstructs an empty (black) image with a white pixel in the middle, according to the parameters specified, to obtain the response of the virtual imaging system to a point source (point spread function, PSF). The PSF is the spatial domain version of the modulation transfer function, so MTF is obtained by Fourier transformation of the PSF and normalizing the Fourier spectrum to a maximum value of 1. The width of the PSF graph at half maximum returns another indicative parameter of spatial resolution, the full width at half maximum (FWHM) value (Fig. 4). Using these quantitative methods, the differences between the implemented techniques and the relation of image quality to the chosen parameters in each technique are highlighted.
Discussion
Learning experience in the form of a computer-supported course is fast growing and can promote lifelong continuing medical education (CME) [1–3, 17, 19]. The majority of studies on learning outcomes suggest that Web-based lifelong CME interventions are effective in enhancing knowledge [1]. In view of the above, an open access purely Web-based, interactive educational application on medical imaging combining text, pictures, animations, and dynamic simulations, resembling real-world workstation functionality was developed. The Web portal includes a virtual imaging system in order to augment student understanding of how medical images are acquired and processed, while providing the opportunity to manipulate various factors, the user may understand the impact on image appearance. The learner can interact with the developed program using any personal computer connected to the internet, with no commercial software needed, at a pace appropriate to his or her learning ability. The target audience of the application could be medical school students, physicists, and engineers studying medical physics and radiology residents.
A preliminary evaluation of the application course was performed using a five-point Likert scale (1 = poor, 5 = excellent) by 46 medical students of our institution that took the lesson on medical imaging. The questionnaire of the evaluation along with mean results are presented in Table 1 and showed that the content of the course was considered effective, well structured, and relevant for their learning. On the other hand, the mean rating for the sufficiency of the online course without a pre-course lecture was only 2.74 on a five point scale, suggesting that the developed application is a useful teaching tool as a supplement to, and not a substitute for, the lecture-based learning at our institute.
Table 1.
Overall assessment of the Web-based course on a five-point Likert-scale (1 = poor, 5 = excellent). Presented results are mean values obtained by analyzing the response of 46 graduate medical students
| Evaluation form questions | Mean |
|---|---|
| How relevant is the course for your learning? | 4.09 |
| How well structured is the online course? | 3.91 |
| How clear are the contents of the online course? | 4.02 |
| How satisfying is the interaction with the application? | 4.13 |
| How satisfying is the overall usage of the application? | 4.26 |
| How sufficient is the Web-based course without a pre-course lecture? | 2.74 |
Conclusion
Medical imaging education in most universities and colleges is restricted to a limited number of class hours for their curricula. Efficient training within limited hours thus becomes crucially important. Web-based medical education could provide practicing health professionals with convenient and cost-effective tools for continuing education [30]. Medical courses can be envisaged in a blended instructional environment, both synchronous and asynchronous, with a tutor who guides the learners through an educational application, responds to emerging queries, initiates discussion on the illustrative topics, and supervises student self-evaluation [19]. This educational approach complies with the general opinion of our department and the evaluating group of our project. We believe that we have created a useful learning tool on medical imaging, recommended as a hands-on supplement to textbooks and didactics. Future plans include further development, content enrichment of the Web portal, and assessing the learning efficiency and the retention of knowledge among graduate and postgraduate students.
Acknowledgments
The authors would like to thank all the graduate students who participated in the assessment of this work for providing useful feedback. The authors would also like to thank Michalis Gatzonis for his contribution to this project.
Funding
None.
Conflicts of Interest
None.
Ethical Approval
Not applicable.
Contributor Information
Dimitrios Papamichail, Phone: +30-21-7462454, FAX: +30-21-7462369, Email: dimitris.papamihail@gmail.com.
Evaggelos Pantelis, Email: vpantelis@phys.uoa.gr.
Panagiotis Papagiannis, Email: ppapagi@phys.uoa.gr.
Pantelis Karaiskos, Email: pkaraisk@med.uoa.gr.
Evangelos Georgiou, Email: egeorgiou@med.uoa.gr.
References
- 1.Curran VR, Fleet L. A review of evaluation outcomes of web-based continuing medical education. Med Educ. 2005;39:561–567. doi: 10.1111/j.1365-2929.2005.02173.x. [DOI] [PubMed] [Google Scholar]
- 2.Childs S, Blenkinsopp E, Hall A, Walton G: Effective e-learning for health professionals and students--barriers and their solutions. A systematic review of the literature--findings from the HeXL project. Health information and libraries journal 22 Suppl 2:20–32, 2005 [DOI] [PubMed]
- 3.Grunewald M, Heckemann RA, Gebhard H, Lell M, Bautz WA. COMPARE radiology: creating an interactive Web-based training program for radiology with multimedia authoring software. Acad Radiol. 2005;10:543–553. doi: 10.1016/S1076-6332(03)80065-X. [DOI] [PubMed] [Google Scholar]
- 4.The basics of MRI. Available at: http://www.cis.rit.edu/htbooks/mri. Accessed 19 February 2013. (Archived at http://www.webcitation.org/6EY1jPolc)
- 5.MRI in heart and circulation. Available at: http://www.sunnybrook.utoronto.ca:8080/%7Egawright/menu_mr_ng.html. Accessed 19 February 2013. (Archived at http://www.webcitation.org/6EY25xw4t)
- 6.Canadè A, Palladino F, Pitzalis G, Campioni P, Marano P. Web-based radiology: a future to be created. Rays. 2003;28:109–117. [PubMed] [Google Scholar]
- 7.Choules AP. The use of elearning in medical education: a review of the current situation. Postgrad Med J. 2007;83:212–216. doi: 10.1136/pgmj.2006.054189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chumley-Jones HS, Dobbie A, Alford CL. Web-based learning: sound educational method or hype? A review of the evaluation literature. Acad Med: J Assoc Am Med Coll. 2002;77:S86–93. doi: 10.1097/00001888-200210001-00028. [DOI] [PubMed] [Google Scholar]
- 9.Hoa D, Micheau A, Gahide G. Creating an interactive Web-based e-learning course: a practical introduction for radiologists. Radiographics. 2006;26:e25. doi: 10.1148/rg.e25. [DOI] [PubMed] [Google Scholar]
- 10.Mahmoudi SE, Akhondi-Asl A, Rahmani R, Faghih-Roohi S, Taimouri V, Sabouri A, Soltanian-Zadeh H. Web-based interactive 2D/3D medical image processing and visualization software. Comput Methods Prog Biomed. 2010;98:172–182. doi: 10.1016/j.cmpb.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Masters K, Ellaway R. e-Learning in medical education Guide 32 Part 2: Technology, management and design. Med Teach. 2008;30:474–489. doi: 10.1080/01421590802108349. [DOI] [PubMed] [Google Scholar]
- 12.O’Connell T, Chang D. Informatics in Radiology: Web-based Preliminary Reporting System for Radiology Residents with PACS Integration. Radiographics. 2012;32:2127–34. doi: 10.1148/rg.327105701. [DOI] [PubMed] [Google Scholar]
- 13.Scatarige JC, Garland MR, Corl FM, O’Keefe CF, Fishman EK. Visitors and content preferences on an educational web site dedicated to clinical body computed tomography: results of a 2001 audit and online survey. Investig Radiol. 2002;37:53–9. doi: 10.1097/00004424-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Smothers V, Ellaway R, Greene P. The E-learning evolution-leveraging new technology approaches to advance healthcare education. Med Teach. 2008;30:117–118. doi: 10.1080/01421590701881681. [DOI] [PubMed] [Google Scholar]
- 15.Wu D, Dikshit A, Zhao W. Medical imaging curriculum development: an interactive simulation system for different modalities. Conf Proc: Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Conference. 2004;7:5172–75. doi: 10.1109/IEMBS.2004.1404440. [DOI] [PubMed] [Google Scholar]
- 16.Dikshit A, Wu D, Wu C, Zhao W. An online interactive simulation system for medical imaging education. Comput Med Imaging Graph: Off J Comput Med Imaging Soc. 2005;29:395–404. doi: 10.1016/j.compmedimag.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Miles KA. Diagnostic imaging in undergraduate medical education: an expanding role. Clin Radiol. 2005;60:742–745. doi: 10.1016/j.crad.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 18.Wangel M, Niemitukia L, Katila T, Soimakallio S. WWW–an effective way of teaching radiology. Comput Methods Prog Biomed. 2001;66:91–98. doi: 10.1016/S0169-2607(01)00141-9. [DOI] [PubMed] [Google Scholar]
- 19.Brown NJ, Britton KE, Plummer DL. Standardisation in medical image management. Int J Med Inform. 1998;48:227–238. doi: 10.1016/S1386-5056(97)00129-9. [DOI] [PubMed] [Google Scholar]
- 20.Zeng GL. Image reconstruction–a tutorial. Comput Med Imaging Graph: Off J Comput Med Imaging Soc. 2001;25:97–103. doi: 10.1016/S0895-6111(00)00059-8. [DOI] [PubMed] [Google Scholar]
- 21.Beister M, Kolditz D, Kalender WA. Iterative reconstruction methods in X-ray CT. Phys Med. 2012;28:94–108. doi: 10.1016/j.ejmp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Dougherty G. Digital Image Processing for Medical Applications. NY: Cambridge University Press; 2009. [Google Scholar]
- 23.Kudomi S, Ueda K, Ueda Y, Kawakubo M, Sanada T. Evaluation of the spatial resolution of multiplanar reconstruction images. Radiol Phys Technol. 2008;1:229–233. doi: 10.1007/s12194-008-0033-2. [DOI] [PubMed] [Google Scholar]
- 24.Cook D, Dupras D. A practical guide to developing effective web-based learning. J Gen Intern Med. 2004;19:698–707. doi: 10.1111/j.1525-1497.2004.30029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sobie EA: An introduction to MATLAB. Science signaling 4:tr7, 2011 [DOI] [PMC free article] [PubMed]
- 26.Kukkonen H, Rovamo J, Tiippana K, Näsänen R. Michelson contrast, RMS contrast and energy of various spatial stimuli at threshold. Vis Res. 1993;33:1431–36. doi: 10.1016/0042-6989(93)90049-3. [DOI] [PubMed] [Google Scholar]
- 27.Bourne R. Fundamentals of Digital Imaging in Medicine. London: Springer; 2010. [Google Scholar]
- 28.Herman G. Fundamentals of Computerized Tomography. London: Springer; 2009. [Google Scholar]
- 29.Hendee W, Ritenour E. Medical Imaging Physics. 4. NY: Wiley-Liss; 2002. [Google Scholar]
- 30.Richardson ML, Norris TE. Online delivery of continuing medical education over the worldwide web: an online needs assessment. Am J Roentgenol. 1997;168:1161–64. doi: 10.2214/ajr.168.5.9129405. [DOI] [PubMed] [Google Scholar]