Abstract
Aims
A discussion on the reasons educational interventions about eczema, by nurses, are successful, with the subsequent development of a theoretical framework to guide nurses to become effective patient educators.
Background
Effective child and parent education is the key to successful self-management of eczema. When diagnosed, children and parents should learn to understand the condition through clear explanations, seeing treatment demonstrations and have ongoing support to learn practical skills to control eczema. Dermatology nurses provide these services, but no one has proposed a framework of the concepts underpinning their successful eczema educational interventions.
Design
A discussion paper.
Data Sources
A literature search of online databases was undertaken utilizing terms ‘eczema OR atopic dermatitis’, ‘education’, ‘parent’, ‘nurs*’, ‘framework’, ‘knowledge’, motivation’, in Scopus, CINAHL, Web of Science, Medline and Pubmed. Limits were English language and 2003–2013.
Implications for Nursing
The framework can inform discussion on child and parent education, provide a scaffold for future research and guide non-specialist nurses, internationally, in providing consistent patient education about eczema.
Conclusion
Founded on an understanding of knowledge, the framework utilizes essential elements of cognitive psychology and social cognitive theory leading to successful self-management of eczema. This framework may prove useful as a basis for future research in child and parent education, globally, in the healthcare community. A framework has been created to help nurses understand the essential elements of the learning processes at the foundation of effective child and parent education. The framework serves to explain the improved outcomes reported in previous nurse-led eczema educational interventions.
Keywords: atopic dermatitis, behaviour, declarative knowledge, eczema, education, framework, procedural knowledge
Why is this research or review needed?
The theoretical foundations explaining why eczema nurse educational interventions are effective have not been explored.
Likewise, the importance of the different ways declarative and procedural knowledge are learnt and assimilated by the learner has not been recognized and applied to eczema education.
What are the key findings?
This framework unites concepts from health, education and cognitive psychology and guides nurses in the processes needed to facilitate the learning and the behavioural changes necessary to manage eczema.
The framework incorporates three important elements: understanding the nature of knowledge, the process of instruction and motivation.
How should the findings be used to influence policy/practice/research/education?
The framework should help nurses understand the key issues in child and parent education in eczema and has the potential, once tested, to improve educational interventions by nurses for eczema.
The framework should provide a scaffold for research into educational interventions to improve treatment adherence for eczema and other chronic conditions.
Introduction
The need for effective, consistent child and parent education (CPE) to help their mastery of the self-management of any chronic health condition cannot be overstated. This is especially true for children with eczema (also termed atopic dermatitis or AD) a chronic, fluctuating, multi-factorial condition, commonly seen in children across the world (Barbarot et al. 2013). Both genetic and environmental factors play key roles in its manifestation of dry, itchy skin from an impaired skin barrier and production of less moisturising factors (Cork & Danby 2009). Management involves regular, ongoing use of emollients to rehydrate the skin and restore barrier function (British Dermatological Nursing Group (BDNG) 2012a). Eczematous skin prone to periods of inflammation and infection requires additional medicated treatments (Schneider et al. 2013). Eczema has greater psychosocial burden than is commonly recognized (Odhiambo et al. 2009). Eczema education must be structured to help children and their families learn to control the condition and reduce the burden of care as, in Australia, skin conditions are the third highest chronic complaint causing children to visit their General Practitioner (Australian Bureau of Statistics 2010).
Globally, dermatology nurses, mostly in secondary care settings, have been shown to provide effective eczema education to children with eczema and their parents, optimizing care, support and satisfaction, minimizing relapses, reducing the psychosocial impact of the condition and providing care equivalent to that of the dermatologist (Cork et al. 2003, Grillo et al. 2006, Moore et al. 2009, Schuttelaar et al. 2010, Ersser et al. 2013, Jackson et al. 2013). However, no educational interventions have developed any theory or framework to explain why the interventions were successful, although Schuttelaar et al. (2010), Ersser et al. (2013) and Jackson et al. (2013) utilized Social Cognitive Theory (sometimes termed Social Learning Theory) where learning and motivation achieved significantly improved self-management skills (Bandura 1986, 1997).
Background
Eczema: management and burden of care
A genetic mutation that impairs the skin barrier means that skin is easily penetrated by irritants, allergens and bacteria, and constant vigilance is required to offset exacerbations (Cork & Danby 2009). Immunological and inflammatory processes and reduced moisturising factors confound the issue (Schneider et al. 2013). Topical preparations need to be altered according to the fluctuating skin condition, making eczema care seems complex (National Institute for Health and Clinical Excellence (NICE) 2007, Barbarot et al. 2013). Children and parents suffer distress with the manifestations causing interrupted sleep and reduced quality of life (QOL) (Camfferman et al. 2010, Santer et al. 2013). About 9% of severe cases experiencing recurring infection require hospitalization (Zuberbier et al. 2006, Kelsay et al. 2010). QOL is further diminished by the costs of treatments and the time taken to undertake them (Fraught et al. 2007, Santer et al. 2013). For some parents, concurrent food allergy and the fear that their child's eczema will progress to asthma and/or hay fever create an additional burden (Campbell 2012, Newland et al. 2012). This progression is termed the ‘allergic march’, where the clinical manifestation of allergic disease changes as one grows older (Spergel 2010). Primarily a condition of children, eczema is more often continuing through adolescence to adulthood making timely, effective eczema education by nurses, more important than ever (Spergel 2010).
The foundations of management and control are the regular application of leave-on emollients needed to rehydrate the skin and restore the barrier function. Children need to have approximately 250 g of emollient per week applied topically and adults 500 g of emollient per week (NICE 2007). Skin cleansers often complement management (Cheong 2009). The cornerstones of treatment are topical corticosteroid preparations (TCS) to reduce inflammation and itch. These are used aggressively when eczema exacerbates, but most people fear using TCS, meaning that they are often underutilized (Storm et al. 2008, Smith et al. 2010, Royal College of Paediatrics & Child Health (RCPCH) 2011, Mancini et al. 2012). This treatment approach allows long periods of remission. However, if the treatment approach is not undertaken, the resulting poorly controlled eczema requires additional treatment strategies, such as wet wrapping to reduce the itch and protect the skin, but application is time consuming and children may not be willing participants in this therapy (Krakowski et al. 2008, Devillers & Oranje 2012). Medicated baths, oral or systemic antibiotics or antiviral medications are required if infection occurs (Schneider et al. 2013).
The complexities of the fluctuating condition mean that children with eczema and their parents need direction and support to understand clearly why they need to carry out the recommended ongoing treatments that can seem onerous, especially when the skin condition looks normal (Santer et al. 2013). Children and parents must gain the practical skills needed to manage the condition, including the correct application of the various topical preparations and they need to learn how to discern the subtle changes in skin condition indicating the need for adjustments to the treatment (Barbarot et al. 2013). As well as requiring the knowledge and practical skills, children and parents need to develop the resilience required to manage the condition in the long term, ensuring that they adhere to the treatment requirements (Nicol & Ersser 2010). Algorithms help healthcare providers diagnose and treat eczema, but these give little help on how to provide eczema education following the diagnosis (NICE 2007, RCPCH 2011, Newland et al. 2012). Time-centred medical consultations mean that most doctors cannot provide the necessary instruction, help and support children and their parents need to learn how to manage the condition. Less than 35% of specialists provide an eczema care-plan that targets individualized treatments and assists child and parent recall, leaving many wondering what they are required to do, for how long and why (Chisolm et al. 2008, Rork et al. 2012).
Challenges of nurses providing eczema education
The success of nurse-led educational interventions for eczema management suggests that nurses are ideally placed to provide effective CPE (Cork et al. 2003, Grillo et al. 2006, Moore et al. 2009, Schuttelaar et al. 2010, Ersser et al. 2013 Jackson et al. 2013). Despite CPE being included in the standards of nursing competencies globally, none describes a theoretical framework that underpins effective patient education to meet those standards (World Health Organisation 1998, Gilmore et al. 2005, Nursing and Midwifery Board of Australia 2006, NICE 2007, Scottish Intercollegiate Guidelines Network (SIGN) 2011, British Dermatological Nursing Group 2012b, Royal Children's Hospital's 2013). A framework explaining the reasons why CPE by dermatology nurses is effective would assist other nurses, such as those in primary care settings, to identify and understand the important elements of patient education and guide and contextualize what they should do to become competent patient educators (Courtenay & Carey 2007).
Data sources
A search of the literature from 2003–2013, limited to English language, was undertaken using terms ‘eczema OR atopic dermatitis’, ‘education*’, ‘knowledge’, ‘framework OR model’, ‘nurs*’, ‘parent’ in Scopus, Web of Science, Medline, PubMed and CINAHL databases to identify if any frameworks or models had been made explicit in nurse-led eczema education. Six papers were identified where reference was made to a representative framework or model (Ersser et al. 2007, Chisolm et al. 2010, Schuttelaar et al. 2010, Royal College of Nursing (RCN) 2012, Ersser et al. 2013, Jackson et al. 2013). Both Ersser et al. (2013) and Jackson et al. (2013) described the same ‘Eczema Education Programme’.
A further eight papers reported success with nurse-led eczema educational interventions, focussing on various aspects, all of which seem to be important (Cork et al. 2003, Grillo et al. 2006, Moore et al. 2009, Nicol & Ersser 2010, de Bes et al. 2011, Friedman et al. 2011, Barbarot et al. 2013, Stalder et al. 2013). This highlights the need for a framework, which synthesizes these elements and which is based on sound educational theory.
Staab et al.'s (2006) eczema education ‘school’, conducted by a large multi-disciplinary team, did not report the nurse as a major educator in the programme nor describe any theoretical underpinning. This paper was therefore excluded.
Discussion
The ‘framework’ from the Royal College of Nursing, RCN (2012) summarized how and what nurses need to do to improve child and parent understanding, knowledge and management of dermatological conditions, but did not explain why nurses need to achieve these goals (RCN 2012). However, components in the RCN framework – knowledge, information and learning – were identified as common aspects of nurses’ successful eczema educational interventions of Cork et al. (2003), Grillo et al. (2006), Moore et al. (2009), Schuttelaar et al. (2010), Ersser et al. (2013) and Jackson et al. (2013). The systematic review of educational and psychological interventions for eczema, by Ersser et al. (2007) determined that few of the seven interventions examined could be compared because the methodologies used varied greatly and most studies were not robust. No theoretical framework or foundation to the studies were identified.
Chisolm et al. (2010) created a framework guided by their review of research into Health Belief, Health Behaviour and Social Cognitive Theory models, but they stated (p. 230) that ‘although AD treatment education programs can improve adherence, we do not yet know why….’. They recognized that written care-plans, follow-up appointments, discussion between the practitioner and the patient when care-plans are created were important factors in improving adherence to treatments. Fundamental to Social Cognitive Theory (SCT) is the idea that learning occurs best when the learner observes a task or skill, practises it and refines it, with the mastery providing motivation for potential behaviour changes. This has important consequences in health care where treatment and management of ongoing conditions need self-efficacy to develop (Bandura 1986, 1997). At no point were health behaviours, an important aspect of SCT, linked to patients’ or parents’ existing and newly gained knowledge about eczema. These are needed to master eczema care (Nicol & Ersser 2010). None of what is currently known about learning and knowledge was examined, with authors, concluding that future research was needed.
Schuttelaar et al. (2010) utilized SCT theory to motivate 55 patients aged 16 years and younger, to learn to control and manage eczema successfully. The nurse practitioner explained the aetiology of eczema, details about topical treatments, triggers and demonstrated application of those treatments. The role of the nurse as a motivator was recognized as an important aspect of helping participants to understand what they needed to undertake. This led to improved adherence. Follow-up appointments at 4, 8 and 12 monthly intervals helped the participants to practise what they needed to do, revisit things that were unclear and feel supported. Participants in the intervention group felt increased satisfaction with the service, compared with those who saw the dermatologist. The authors recognized limitations of a non-blinded intervention carried out in specialized, secondary care. No attempt was made to assess any knowledge gain of the participants. Behaviour changes were attributed to SCT, but no explanation was given as to why this improved the outcomes. The eczema education workshops by Grillo et al. (2006) and Moore et al. (2009) where explanation, demonstration and support featured had similar findings.
The Eczema Education Program (EEP) utilized social learning theory as the construct underpinning nurse-led eczema group education (Ersser et al. 2013, Jackson et al. 2013). Self-management, knowledge and understanding of eczema triggers, treatments and management showed statistically significant improvement. Importantly, this programme was conducted in primary care and resulted in less return visits to the general practitioner. Researchers noted limitations of the programme not having a control group, but a future randomized control trial is planned. There was also difficulty in retaining those primary care nurses who were trained especially for the EEP meaning that the expert eczema nurses assumed responsibility for the educational intervention (Ersser et al. 2013). Primary care eczema education studies prior to the EEP have not been robustly explored (Chinn et al. 2002).
What are the essential elements of successful nurse-led eczema education to be incorporated into a framework? A systematic review, by Friedman et al. (2011) on effective teaching strategies and patient education determined that those involving structured, culturally appropriate and patient-centred features improved knowledge, decreased anxiety and increased consumer satisfaction.
Nicol and Ersser (2010), de Bes et al. (2011) and Stalder et al. (2013) explored the role of the eczema nurse educator detailing the success of various educational interventions that improved patient knowledge. Successful modes of delivery included one-on-one face-to-face sessions, group workshops, eczema ‘schools’, DVDs, written information and access to support groups. However, no authors described any theoretical framework under-pinning improvement in knowledge or practical skill development.
Barbarot et al. (2013) highlighted the importance of health professionals recognizing that the giving of information alone will not help patients with long-term illness develop the knowledge and skills necessary to manage their condition. Barbarot et al. (2013) supported Cork et al. (2003), adding that mastering the treatment skills is essential for long-term management. However, no studies explained why the interventions were successful. We contend that to have a fuller understanding of effective CPE, it is necessary to identify the basic elements of the nature of knowledge, cognitive psychology and social cognitive theory and how these interplay in the learning process.
Towards a framework for CPE
We argue that effective CPE should be based on some key principles. These begin with an understanding of the nature of knowledge and how it is gained by the learner through experience and instruction. Effective CPE should also facilitate the behaviour and life-style changes that are necessary for long-term adherence. A framework of effective CPE should therefore build in each of these key principles.
The nature of knowledge
Keeves (1997) explained the concept of knowledge and human enquiry identifying three ‘world views’, using the work of Popper and Eccles (1977). World 1 holds objects and structures created by people, such as the health systems, hospitals, universities and communities. World 2 is the world of the individual mind, the subjective and for eczema education, it is the patient and/or parent learner. World 3 contains the output of people's minds, various forms of stored knowledge, such as published health and nursing research, evidence-based nursing standards and patient-centred health information material. Learning occurs in the mind of the learner (World 2) when the learner experiences something from World 1, the real world, or gains information from World 3, either from some form of stored knowledge or through instruction from someone (Figure1).
Figure 1.
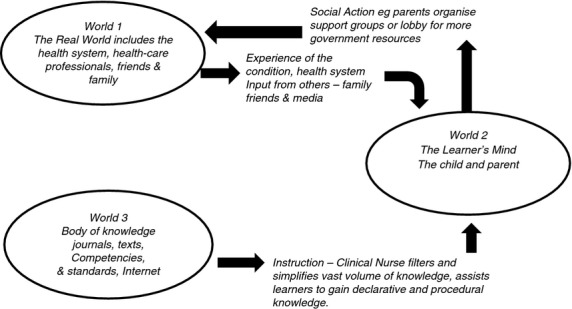
A model of the knowledge exchanges experienced by children and parents based on Keeves (1997, p. 2) after Popper and Eccles (1977).
It is important to understand that World 3 contains much information. The mind of the learner is bombarded with information, particularly since the advent of the internet. The nurse in the CPE role has the difficult task of acting as a conduit, feeding and filtering information from World 3. Keeves (1997) emphasizes a threefold purpose in education – the transfer of knowledge, filtering and assimilating that knowledge and then developing the skills of enquiry to test the new ideas against what is known already, critically evaluating new information. This is particularly important for eczema, where there is copious misinformation available.
Kahneman (2011) has identified that World 2, where patient education occurs in the child's or parent's mind, works as two separate systems. System 1 operates automatically and quickly, whereas System 2 is more deliberate and slow, requiring more effort and mental activity. Effective learning takes place when System 2 is engaged and explains why patients cannot take information in during the often short medical consultation (Ridd & Purdy 2009). Kahneman's (2011) concept suggests that the success of any health-related education rests on recognizing that it takes time and careful explanation to help children and parents link the new information given to them about eczema with their prior knowledge. Only then can sense be made of the new knowledge related to their condition and development of the skills and confidence required to self-manage the condition occur. We contend that nurses are well placed to provide this education, having more time to undertake the task. This was recently demonstrated by (Ersser et al. 2013, Jackson et al. 2013).
Anderson (2005) and Marzano et al. (1997) identified two different kinds of knowledge, declarative and procedural, both of which require different strategies to be acquired and assimilated. Declarative knowledge is defined as the knowledge associated with facts and concepts, like the significance of an impaired skin barrier in eczema sufferers. The acquisition and assimilation of declarative knowledge requires three phases (Marzano et al. 1997, Anderson 2005). Firstly, the learner attempts to make sense of the incoming information by constructing meaning and tries to connect to what is already known. Following this ‘constructing meaning’ phase, the child/parent seeks to organize knowledge, making more connections with what they already know and consolidating their understanding of what the nurse has explained. Finally, once the knowledge is organized, it is stored ready to be retrieved for use later. For declarative knowledge, much time is spent constructing meaning.
As an example of declarative knowledge, children and parents should gain an understanding of skin function and in particular, what is happening to the skin of an eczema sufferer. The abstraction of the skin, likening eczematous skin to a brick wall with missing mortar joints, helps children and parents easily understand how skin function is compromised, how easily irritants and allergens penetrate damaged skin and why using soap compounds the problem (Cork 1997, BDNG 2012a). They readily understand why a primary goal of eczema treatment is to replace the missing and crumbling ‘mortar’ in the skin, using thick enough emollients to re-establish skin function. For CPE, it recognizes what children and parents already know about eczema and links it to what they can readily understand. It also provides an easy way of learning how emollient therapy works. Thus, the ‘brick wall’ model allows learners to construct meaning, organize their knowledge and store it in an easily retrievable manner. They can ask questions, discuss concerns and have the opportunity to work through the three phases of gaining and assimilating declarative knowledge, creating less chance to be led astray by the myriad of misinformation from media and friends. This helps explain the success of EEP by Ersser et al. (2013) and Jackson et al. (2013).
Procedural knowledge is identified as the knowledge necessary to complete practical tasks, such as applying topical treatments (Marzano et al. 1997). The first step constructs a model of the process to be learnt. Eczema nurse educators break the process down into small steps, illustrating with diagrams, creating a care-plan and then demonstrating the procedure. An effective eczema educator must also allow children and parents to feel the varying textures of the different thicknesses of emollients as cosmetic acceptability is an important factor in adherence for persons with eczema (Carr 2006, Ellis et al. 2011, Coyner & Purath 2012). The second step in acquiring procedural knowledge involves shaping the skill, recognizing how to vary the procedure according to specific needs and learning how to avoid common errors. For eczema, this involves learning to apply the emollient in a downward direction, in the direction the hairs erupt from the skin, not up and down or in circles, as is common practice (NICE 2007). It also involves the child and parent learning how to apply topical corticosteroid preparations to the reddened areas, using the validated ‘finger-tip’ method to quantify the amount to use (Long et al. 1998). Alternatively, the nurse demonstrates applying the required amount until a ‘shine’ appears on the skin (NICE 2007). Nurses, as effective patient educators, help learners become skilled in monitoring their symptoms using their senses, particularly sight and touch. Parents need to be shown how to observe and feel skin and need practice in recognizing the subtle changes that influence the ongoing treatment cycle. The third aspect of developing procedural knowledge involves internalizing the skill, practising until the skill becomes automatic (Figure2). Children and parents need to practise until they can recognize whether the dryness of the skin needs a thick cream emollient or a greasier preparation. This is an important factor in the increased satisfaction experienced in the nurse-led educational interventions and EEP (Cork et al. 2003, Grillo et al. 2006, Moore et al. 2009, Schuttelaar et al. 2010, Ersser et al. 2013, Jackson et al. 2013).
Figure 2.
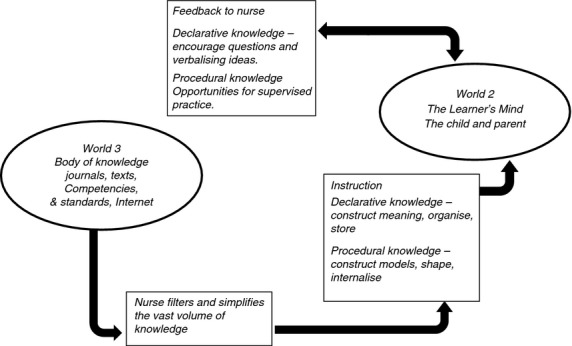
A model of the instruction and feedback process in which the child and parents acquire and refine knowledge and skills, adapted from Keeves (1997, p. 2).
The importance of instruction in both declarative and procedural knowledge
With limited instruction, children and parents have difficulty recognizing what they need to do for the long-term, especially adjusting medications and treatments. The nurse is an essential component in simplifying the myriad of complex concepts and helping children and parents develop the necessary skills.
One of the nurse's primary tasks in managing eczema (NICE 2007, RCN 2012) is patient education and the nurse provides a vital link between the healthcare provider diagnosing the condition and the children and parents, enabling improved adherence to recommendations (Cork et al. 2003, Schuttelaar et al. 2010, Ersser et al. 2013, Jackson et al. 2013). The nurse identifies the gaps in knowledge and understanding, helps children and parents assimilate their ideas and verbalize their understanding, thus creating a feedback mechanism. The nurse can review any treatment techniques children and parents have not mastered and help them develop fluency with their ideas. Fears about side effects of the topical corticosteroid preparations, which pose a challenge to nurses caring for those with eczema may also be reduced (Smith et al. 2010, Nicol 2011, Santer et al. 2013). Support by health professionals, especially expert eczema nurses, is a common theme highlighted in educational interventions and focus groups (Cork et al. 2003, Grillo et al. 2006, Moore et al. 2009, Schuttelaar et al. 2010, Smith et al. 2010, Ersser et al. 2013, Jackson et al. 2013).
Behavioural changes – Social cognitive theory (SCT)
Health behaviours in CPE result from cognitive, behavioural and environmental factors with cognition an important mediator (Figure3). Bandura (1986) has suggested that SCT provides a model that explores the factors that determine the longevity of behavioural changes resulting in successful outcomes. SCT explains how children and parents through gaining knowledge, confidence in self-management and self-monitoring techniques and developing strategies undergo behavioural changes that allow them to persist with treatments despite the intermittent difficulties characteristic of eczema (Bandura 1986, 1997). They develop realistic outcome expectations that assist the resilience, perseverance and long-term commitment, essential factors when lengthy treatments may only produce some reduction in symptoms (Bartholomew et al. 2000). If learners believe that the task is achievable, the more likely it is that they will be motivated to try and subsequently succeed. Therefore, they are more likely to engage in emollient therapy if they have the confidence that they can do it and believe their efforts will lead to an improvement in eczema symptoms and self-efficacy as shown by Ersser et al. (2013) and Jackson et al. (2013).
Figure 3.
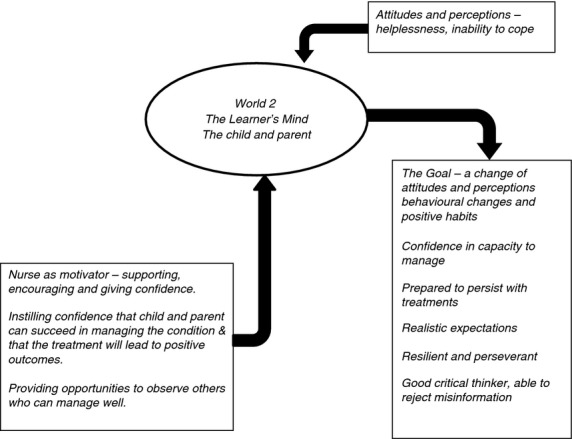
Social Cognitive Theory – the role of the nurse as a motivator, adapted from Keeves (1997, p. 2).
Bandura (1986) identified four important sources of information relevant to behaviour change. The first is existing personal experience. The second is vicarious experience, such as when learners can observe others successfully managing. A third influencing source is verbal persuasion from others and the final one is physiological feedback. Children and their parents can be greatly reassured when they see a nurse demonstrating emollient therapy and wet wraps and are then encouraged to try it for themselves. Reassurance and encouraging feedback from a nurse as the parent builds confidence are more likely to lead to lasting behavioural changes. Lastly, witnessing the benefits of eczema reduction and the improved QOL are going to motivate the patient or parents to maintain the positive behavioural changes. The improved outcome and satisfaction of EEP can be explained using these ideas (Ersser et al. 2013, Jackson et al. 2013).
In clinical practice, nurses usually meet parents and patients at the point of their previous and existing experience, acting as role models and demonstrating the various techniques. Nurses can instil confidence that the child and parent have the capacity to succeed with the necessary treatments providing encouragement through guided practice and reassurance that the treatment will have a positive effect (Nicol & Ersser 2010). Subsequent visits provide opportunities to point out and celebrate progress made (Figure3). By motivating and reinforcing the procedures when making time for supervised practice, parents and children gradually develop the skills to undertake these complex treatment tasks confidently. Nurses also motivate and support children and parents during setbacks when triggers or infection may exacerbate eczema (Ersser et al. 2007, 2013, Schuttelaar et al. 2010, de Bes et al. 2011, Jackson et al. 2013). This assists children and parents to more easily accept the responsibility of making the necessary life-style changes for successful long-term management (Bandura 1986).
The goals of CPE in eczema
To summarize, for the framework, the goals of eczema CPE are to help children with eczema and their parents to:
gain the knowledge necessary to understand the condition.
quantify and clarify terms commonly used in eczema management.
simplify, filter, organize and target the information that is most important to the individual's needs, consistent with the healthcare provider's recommendations.
understand the eczema care-plan created for them.
explain, demonstrate and assist in learning how to undertake these processes.
learn how to monitor symptoms, adjusting treatments in a feedback cycle, as the severity of the condition varies.
develop the sensitivity needed to discern the symptom variation and the subtle changes in the skin.
develop, practise and fine-tune the skills needed to administer treatments.
change their behaviours in ways necessary for long-term management.
We argue that a framework based on an understanding of how knowledge is built on the individual's experience of the world, an understanding of the importance of instruction in both declarative and procedural knowledge and an understanding of what motivates children and parents to make the necessary life-style changes is the next essential step towards improving CPE in eczema management. Such a framework will help those seeking to develop their skills in CPE and, at the same time, complement the various standards of CPE in the eczema guidelines and provide a structure to facilitate research (NICE 2007, RCPCH 2011, RCN 2012).
The proposed framework
We have argued that any successful CPE programme should be founded on an understanding of how the learner in World 2 interacts with Worlds 1 and 3 to gain knowledge. Also, we argue that CPE involves helping the learners understand their experiences from World 1, the real world and dealing with the vast body of knowledge from World 3. Nurses act as a conduit of information from World 3 providing the learners with the skills needed to assess new information. It is further suggested that real learning can only take place when the learner has time to engage in the depth of mental activity necessary. This has been an important argument for nurses to take on the responsibility for CPE, as doctors have too little time for effective CPE. An important distinction between declarative and procedural knowledge has been outlined. It follows that for children and parents to develop the necessary practical skills, demonstration and practice are vital.
The nurse's role in motivating both children and parents to adhere to the treatments provides educational support, enabling children and parents to undertake the treatments with confidence, knowing that doing so will lead to improved outcomes (Jackson et al. 2013). This also enables the long-term behavioural changes. This suggests a multi-layered approach, where the nurse, in clinical practice, attends to all of these elements (Figure4). It shows how effective CPE should be based on an understanding of how learning takes place, the role of the expert instructor in interpreting and filtering and in helping learners to gain both declarative and procedural knowledge. At the same time, CPE demonstrates modelling practices that will lead to the necessary behavioural and lifestyle changes. Like any model, this framework needs to be tested and revised.
Figure 4.
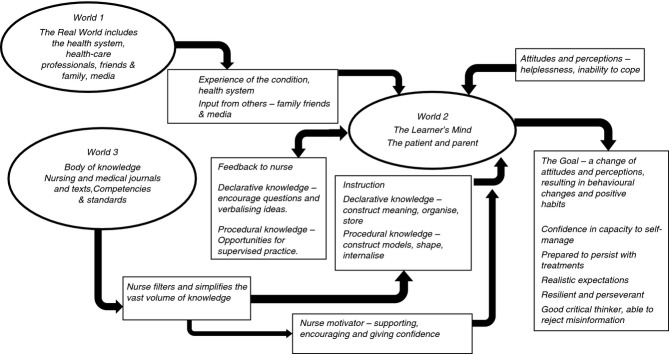
A Framework for Nurse-led intervention for the education children with eczema and their parents, adapted from Keeves (1997, p. 2).
Implications for nursing
This framework is founded on an understanding of the nature of knowledge as it applies to the health profession and that effective management of eczema hinges on children and parents being given the necessary knowledge and developing the skills and confidence to manage the condition successfully. Nurses in clinical practice need guidance in both how and why this approach is needed to improve outcomes. The framework can guide nurses providing eczema education with improved theoretical understanding potentially leading to a consistent approach needed in both primary and secondary care (Courtenay & Carey 2007, Jackson et al. 2013).
Conclusion
Effective patient education by eczema nurses is a complex process that has not previously been explained in the light of what is currently known about effective learning. Success of educational interventions in clinical practice depends on understanding the nature of knowledge, recognizing that knowledge and skills are learnt in different ways and that building confidence is essential. Previously, there has not been any framework to explain the success of educational interventions involving eczema nurses. The proposed framework has, as its philosophical basis, an understanding of knowledge and how individuals gain this knowledge through instruction. The importance of instruction, particularly in gaining declarative and procedural knowledge, and the role of the nurse have been linked to SCT to provide an understanding of how this instruction can be enhanced, emphasizing the nurse's role as a motivator, towards behavioural change and self-efficacy. These components working in concert have been shown to lead to successful self-management of eczema. This paper provides a schematic way of understanding patient education and a means of helping nurses to become more effective patient educators through understanding the underlying principles. The framework provides a means of supporting nurses new to CPE for eczema.
This framework offers a representation of educational intervention by nurses. It should now be tested, discussed and refined as the importance of the role of the nurse working in CPE and as an agent of life-style change is more fully understood. If nurses and health professionals understand the theoretical framework underpinning their effective patient education strategies, it may assist with educational intervention programmes having a more consistent and perhaps, standardized approach globally. This may provide an effective framework for future research into educational interventions by nurses and provide a means by which this research may be made more coherent, less diverse and more systematic.
Acknowledgments
The authors thank Professor John Keeves for his willingness to share his insights into knowledge and education.
Funding
No grants or funding was obtained.
Conflict of interest
There are no conflicts of interest by the authors.
Author contributions
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/ethical_1author.html)]:
substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
drafting the article or revising it critically for important intellectual content.
References
- Anderson J. Cognitive Psychology and its Implications. 6th edn. New York: Worth Publishers; 2005. [Google Scholar]
- Australian Bureau of Statistics. Health of Children in Australia: A snapshot, 2004–05. Australian Bureau of Statistics Canberra; 2010. , cat number 4829.0.55.001, last updated 7th March, 2007. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/mf/4829.0.55.001/ on 04 December 2013. [Google Scholar]
- Nursing and Midwifery Board of Australia. 2006. National Competency Standards for the Registered Nurse. Retrieved from http://www.nursingmidwiferyboard.gov.au/ on 02 January 2014.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- Barbarot S, Bernier C, Deleuran M, De RL, Eichenfield L, Hachem M, Marcoux M, Morren M-A, Torrelo A. Stalder J. Therapeutic patient education in children with atopic eczema. A position paper on objectives and recommendations. Pediatric Dermatology. 2013;30(2):199–206. doi: 10.1111/pde.12045. doi: 10.1111/pde.12045. [DOI] [PubMed] [Google Scholar]
- Bartholomew L, Shegog R. Parcel G. Watch, discover, think and act: a model for patient education program development. Patient Education and Counseling. 2000;39(2–3):269–280. doi: 10.1016/s0738-3991(99)00045-2. [DOI] [PubMed] [Google Scholar]
- de Bes J, Legierse C, Prinsen C. De Korte J. Patient education in chronic skin diseases: a systematic review. Acta Dermatology Venerology. 2011;91(1):12–17. doi: 10.2340/00015555-1022. doi: 10.2340/00015555-1022. [DOI] [PubMed] [Google Scholar]
- British Dermatological Nursing Group. Best practice in emollient therapy: a statement for healthcare professionals. Dermatology Nursing. 2012a;11(4):S1–S19. [Google Scholar]
- British Dermatological Nursing Group. 2012b. Dermatology Nursing Competencies: Developing Dermatology Nurses from Novice to Expert. Retrieved from http://www.bdng.org.uk/documents/EmollientBPG.pdf on 05 January 2014.
- Camfferman D, Kennedy J, Gold M, Martin J, Winwood P. Lushington K. Eczema Sleep and behaviour in Children. Journal of Clinical Sleep Medicine. 2010;6(6):581–588. [PMC free article] [PubMed] [Google Scholar]
- Campbell D. Role of food allergy in childhood atopic dermatitis. Journal of Paediatrics and Child Health. 2012;48(12):1058–1064. doi: 10.1111/j.1440-1754.2011.02125.x. . doi: 10.1111/j.1440-1754.2011.02125.x. [DOI] [PubMed] [Google Scholar]
- Carr J. Emollient treatment for childhood eczema: involving children and parents. Journal of Family Health Care. 2006;16(4):105–107. [PubMed] [Google Scholar]
- Cheong W. Gentle cleansing and moisturizing for patients with atopic dermatitis and sensitive skin. American Journal of Clinical Dermatology. 2009;10(Suppl. 1):13–17. doi: 10.2165/0128071-200910001-00003. [DOI] [PubMed] [Google Scholar]
- Chinn D, Poyner T. Sibley G. Randomized controlled trial of a single dermatology nurse consultation in primary care on the quality of life in children with atopic eczema. British Journal of Dermatology. 2002;146(3):432–439. doi: 10.1046/j.1365-2133.2002.04603.x. doi: 10.1046/j.1365-2133.2002.04603.x. [DOI] [PubMed] [Google Scholar]
- Chisolm S, Taylor S, Balkrishnan R. Feldman S. Written Action plans: potential to improve outcomes for children with atopic dermatitis. Journal of the American Academy of Dermatology. 2008;59(4):677–683. doi: 10.1016/j.jaad.2008.04.025. [DOI] [PubMed] [Google Scholar]
- Chisolm S, Taylor S, Gryswacz J, O'Neil J, Balkrishnan R. Feldman S. Health behaviour models: a framework for studying adherence in children with atopic dermatitis. Clinical and Experimental Dermatology. 2010;35(3):228–232. doi: 10.1111/j.1365-2230.2009.03741.x. doi: 10.1111/j.1365-2230.2009.03741.x. [DOI] [PubMed] [Google Scholar]
- Cork M. The importance of skin barrier function. Journal of Dermatological Treatment. 1997;8(S1):S7–S13. . doi: 10.3109/09546639709160948. [Google Scholar]
- Cork M. Danby S. Skin barrier breakdown: a renaissance in emollient therapy. British Journal of Nursing. 2009;18(14):872–877. doi: 10.12968/bjon.2009.18.14.43356. [DOI] [PubMed] [Google Scholar]
- Cork MJ, Britten J, Butler I, Young S, Murphy R. Keohane S. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. British Journal Dermatology. 2003;149:582–589. doi: 10.1046/j.1365-2133.2003.05595.x. doi: org/10.1046/j.1365-2133.2003.05595.x. [DOI] [PubMed] [Google Scholar]
- Courtenay M. Carey N. A review of the impact and effectiveness of nurse-led care in dermatology. Journal of Clinical Nursing. 2007;16(1):122–128. doi: 10.1111/j.1365-2702.2006.01702.x. doi 10.1111/j.1365-2133.2005.06979.x. [DOI] [PubMed] [Google Scholar]
- Coyner T. Purath J. Improving treatment adherence in patients with atopic dermatitis. The Journal of the Dermatology Association of America. 2012;4(6):374–377. doi: 10.1097/JDN.0b013e318274b4a9. [Google Scholar]
- Devillers A. Oranje A. Wet-wrap treatment in children with atopic dermatitis: a practical guideline. Pediatric Dermatology. 2012;29(1):24–27. doi: 10.1111/j.1525-1470.2011.01691.x. [DOI] [PubMed] [Google Scholar]
- Ellis R, Koch L. Williams J. Potential barriers to adherence in pediatric dermatology. Pediatric Dermatology. 2011;28(3):242–244. doi: 10.1111/j.1525-1470.2011.01493.x. [DOI] [PubMed] [Google Scholar]
- Ersser SJ, Latter S, Sibley A, Satherley PA. Wellbourne S. Psychological and educational interventions for atopic eczema in children. Cochrane Database Systematic Review. 2007;(3):CD004054. doi: 10.1002/14651858.CD004054.pub2. doi: 10.1002/14651858.CD004054.pub2. [DOI] [PubMed] [Google Scholar]
- Ersser S, Farasat H, Jackson K, Dennis H, Sheppard Z. More A. A service evaluation of the Eczema Education Programme: an analysis of child, parent and service outcomes. British Journal of Dermatology. 2013;169(3):629–636. doi: 10.1111/bjd.12414. doi:10.1111/bjd.12414. [DOI] [PubMed] [Google Scholar]
- Fraught J, Bierl C, Barton B. Kemp A. Stress in young mothers of young children with eczema. Archives of Diseases in Childhood. 2007;92:683–686. doi: 10.1136/adc.2006.112268. doi:10.1136/adc.2006.112268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman A, Cosby R, Boyko S, Hatton-Bauer J. Turnbull G. Effective teaching strategies and methods of delivery for patient education: a systematic review and practice guideline recommendations. Journal of Cancer Education. 2011;26(1):12–21. doi: 10.1007/s13187-010-0183-x. doi:10.1007/s13187-010-0183-x. [DOI] [PubMed] [Google Scholar]
- Gilmore G, Olsen L, Taub A. Connell D. Overview of the national health educator competencies update project, 1998–2004. Health Education Behaviour. 2005;32:725. doi: 10.1177/1090198105280757. doi:10.1177/1090198105280757. [DOI] [PubMed] [Google Scholar]
- Grillo M, Gassner L, Marshman G, Dunn S. Hudson P. Pediatric atopic eczema: the impact of an educational intervention. Pediatric Dermatology. 2006;23(5):428–436. doi: 10.1111/j.1525-1470.2006.00277.x. doi:10.1111/j.1525-1470.2006.00277.x. [DOI] [PubMed] [Google Scholar]
- Jackson K, Ersser S, Dennis H, Farasat H. More A. The Eczema Education Programme: intervention development and model feasibility. Journal of the European Academy of Dermatology and Venerology. 2013 doi: 10.1111/jdv.12221. doi: 10.1111/jdv.12221 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Kahneman D. Thinking, Fast and Slow. New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- Keeves JP. Introduction: towards a unified view of educational research. In: Keeves JP, editor. Educational Research, Methodology and Measurement: An International Handbook. 2nd edn. New York: Pergamon; 1997. pp. 1–7. [Google Scholar]
- Kelsay K, Klinnert M. Bender B. Addressing the psychosocial aspects of atopic dermatitis. Immunology Clinics of North America. 2010;30(3):385–396. doi: 10.1016/j.iac.2010.05.003. doi:10.1016/j.iac.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Krakowski A, Eichenfield L. Dohil M. Management of atopic dermatitis in the pediatric population. Pediatrics. 2008;122(4):812–824. doi: 10.1542/peds.2007-2232. doi:10.1542/peds.2007-2232. [DOI] [PubMed] [Google Scholar]
- Long C, Mills C. Finlay A. A practical guide to topical therapy in children. British Journal of Dermatology. 1998;138(2):293–296. doi: 10.1046/j.1365-2133.1998.02077.x. [DOI] [PubMed] [Google Scholar]
- Mancini A, Paller A, Simpson E, Ellis C. Eichenfield L. Improving the patient-clinician and parent-clinician partnership in atopic dermatitis management. Seminars in Cutaneous Medicine and Surgery. 2012;31(3 suppl):S23–S28. doi: 10.1016/j.sder.2012.07.003. doi:10.1016/j.sder.2012.07.003. [DOI] [PubMed] [Google Scholar]
- Marzano R, Pickering DJ, Arrendondo DE, Blackburn GJ, Brandt RS, Moffett CA, Paynter DE, Pollock JE. Whisler JS. Dimensions of learning teacher's manual. 2nd edn. Alexandria, VA: ASCD; 1997. [Google Scholar]
- Moore E, Williams A, Manias E. Varigos G. Eczema workshops reduce the severity of childhood eczema. Australasian Journal of Dermatology. 2009;50(2):100–106. doi: 10.1111/j.1440-0960.2009.00515.x. doi:10.1111/j.1440-0960.2009.00515.x. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. Atopic Eczema in Children: Management of Atopic Eczema in Children from Birth up to the Age of 12 years. London: NICE; 2007. . Retrieved from http://www.nice.org.uk/CG057 on 07 January 2014. [Google Scholar]
- Newland K, Warren L. Gold M. Food allergy and infantile eczema: a clinical approach and algorithm. Australasian Journal of Dermatology. 2012;54(2):79–84. doi: 10.1111/j.1440-0960.2012.00911.x. doi:10.1111/j.1440-0960.2012.00911.x. [DOI] [PubMed] [Google Scholar]
- Nicol N. Efficacy and safety considerations in topical treatments for atopic dermatitis. Pediatric Nursing. 2011;37(6):295–301. [PubMed] [Google Scholar]
- Nicol N. Ersser S. The role of the nurse-educator in managing atopic dermatitis. Immunology Allergy Clinics North America. 2010;30(3):369–383. doi: 10.1016/j.iac.2010.06.007. doi:10.1016/j.iac.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Odhiambo J, Williams C, Tadd C, Robertson C, Asher A ISAAC Three Study Group. Global variations in prevalence of eczema symptoms in children from ISAAC phase three. Journal of Allergy and Clinical Immunology. 2009;124(6):1251–1258. doi: 10.1016/j.jaci.2009.10.009. e23, doi: 10.1016/j.jaci.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Popper K. Eccles J. The Self and Its Brain. Berlin: Springer-Verlag; 1977. [Google Scholar]
- Ridd M. Purdy S. Exacerbations of atopic eczema in children: 10 minute consultation. British Medical Journal. 2009;339:b2997. doi: 10.1136/bmj.b2997. doi:10.1136/bmj.b2997. [DOI] [PubMed] [Google Scholar]
- Rork J, Sheehan W, Gaffin J, Timmons K, Sidbury R, Schneider L. Phipatanakul W. Parental response to written eczema action plans in children with eczema. Archives of Dermatology. 2012;148(3):391–392. doi: 10.1001/archdermatol.2011.2267. doi:10.1001/archdermatol.2011.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal Children's Hospital. 2013. Clinical guidelines (hospital) eczema management. Retrieved from http://www.rch.org.au/rchcpg/index.cfm?doc_id=9971 on 12 December 2013.
- Royal College of Nursing. 2012. RCN competences: an education and training framework for Paediatric dermatological nursing. Retrieved from https://www.rcn.org.uk/__data/assets/pdf_file/0004/259033/003317.pdf on 06 January 2014.
- Royal College of Paediatrics and Child Health. 2011. Allergy care pathways for children: eczema. Retrieved from http://www.rcpch.ac.uk/allergy on 01 January 2014.
- Santer M, Burgess H, Yardley L, Ersser S, Lewis-Jones S, Muller I, Hugh P. Little P. Managing childhood eczema: qualitative study exploring carers’ experiences of barriers and facilitators to treatment adherence. Journal of Advanced Nursing. 2013;69(11):2493–2501. doi: 10.1111/jan.12133. doi:10.1111/jan.12133. [DOI] [PubMed] [Google Scholar]
- Schneider L, Tilles S, Lio P, Boguniewicz M, Beck L, LeBovidge J. Novak N. Atopic dermatitis: a practice parameter update 2012. Journal of Allergy and Clinical Immunology. 2013;131(2):295. doi: 10.1016/j.jaci.2012.12.672. doi:10.1016/j.jaci.2012.12.672. [DOI] [PubMed] [Google Scholar]
- Schuttelaar M, Vermeulen K, Drukker N. Coenraads P. A randomised controlled trial in children with eczema: nurse practitioner vs. dermatologist. British Journal of Dermatology. 2010;162(1):162–170. doi: 10.1111/j.1365-2133.2009.09502.x. doi:10.1111/j.1365-2133.2009.09502.x. [DOI] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guidelines Network (SIGN) 2011. SIGN Management of atopic eczema in primary care, Edinburgh. (SIGN publication no. 125). Retrieved from http://www.sign.ac.uk on 21 December 2013.
- Smith S, Hong E, Fearns S, Blaszczynski A. Fisher G. Corticosteroid phobia and other confounders in the treatment of childhood atopic dermatitis explored using parent focus groups. Australasian Journal of Dermatology. 2010;51(3):168–174. doi: 10.1111/j.1440-0960.2010.00636.x. doi:10.1111/j.1440-0960.2010.00636.x. [DOI] [PubMed] [Google Scholar]
- Spergel J. Epidemiology of atopic disease and the atopic march in children. Immunology Allergy Clinics North America. 2010;30(3):269–280. doi: 10.1016/j.iac.2010.06.003. . doi:10.1016/j.iac.2010.06.003. [DOI] [PubMed] [Google Scholar]
- Staab D, Diepgen T, Fartasch M, Kupfer J, Lob-Corzilius T, Ring J, Schwee S, Scheidt R, Schmitt-Ott G, Schnopp C, Szczepanski R, Werfel T, Wittenmeier M, Wahn U. Gieler U. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomized controlled trial. British Medical Journal. 2006;332(7547):933–938. doi: 10.1136/bmj.332.7547.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalder J-F, Bernier C, Ball A, De Raeve L, Gieler U, Deleuran M, Marcoux D, Eichenfield L, Lio P, Lewis-Jones S, Gelmetti C, Takaoka R, Chiaverini C, Misery L, Barbarot S for the Oriented Patient-Education Network in Dermatology (OPENED) Therapeutic patient education in atopic dermatitis: worldwide experiences. Pediatric Dermatology. 2013;30(3):329–334. doi: 10.1111/pde.12024. doi:10.1111/pde.12024. [DOI] [PubMed] [Google Scholar]
- Storm A, Benfeldt E, Andersen S. Sterup J. A prospective study of patient adherence to topical treatments: 95% of patients underdose. Journal American Academy of Dermatology. 2008;59(6):975–980. doi: 10.1016/j.jaad.2008.07.039. doi:10.1016/j.jaad.2008.07.039. [DOI] [PubMed] [Google Scholar]
- World Health Organisation. 1998. Therapeutic patient education, continuing education programmes for health care providers in the field of prevention of chronic diseases: a report of the WHO working group. Retrieved from http://www.euro.who.int/__data/assets/pdf_file/0007/145294/E63674.pdf on 20 August 2013.
- Zuberbier T, Orlow T, Paller S, Taieb A, Allen R, Hernanz-Hermosa J, Ocampo-Candiani J, Cox M, Langeraar J. Simon J. Patient perspectives on the management of atopic dermatitis (ISOLATE) Journal Allergy and Clinical Immunology. 2006;118(1):226–232. doi: 10.1016/j.jaci.2006.02.031. doi: 10.1016/j.jaci.2006.02. [DOI] [PubMed] [Google Scholar]


