Abstract
Purpose
Access to critical care is a crucial component of healthcare systems. In low-income countries, the burden of critical illness is substantial, but the capacity to provide care for critically ill patients in intensive care units (ICUs) is unknown. Our aim was to systematically review the published literature to estimate the current ICU capacity in low-income countries.
Methods
We searched 11 databases and included studies of any design, published 2004-August 2014, with data on ICU capacity for pediatric and adult patients in 36 low-income countries (as defined by World Bank criteria; population 850 million). Neonatal, temporary, and military ICUs were excluded. We extracted data on ICU bed numbers, capacity for mechanical ventilation, and information about the hospital, including referral population size, public accessibility, and the source of funding. Analyses were descriptive.
Results
Of 1,759 citations, 43 studies from 15 low-income countries met inclusion criteria. They described 36 individual ICUs in 31 cities, of which 16 had population greater than 500,000, and 14 were capital cities. The median annual ICU admission rate was 401 (IQR 234-711; 24 ICUs with data) and median ICU size was 8 beds (IQR 5-10; 32 ICUs with data). The mean ratio of adult and pediatric ICU beds to hospital beds was 1.5% (SD 0.9%; 15 hospitals with data). Nepal and Uganda, the only countries with national ICU bed data, had 16.7 and 1.0 ICU beds per million population, respectively. National data from other countries were not available.
Conclusions
Low-income countries lack ICU beds, and more than 50% of these countries lack any published data on ICU capacity. Most ICUs in low-income countries are located in large referral hospitals in cities. A central database of ICU resources is required to evaluate health system performance, both within and between countries, and may help to develop related health policy.
Introduction
Providing acute care to critically ill patients is a global enterprise, regardless of health system capacity [1,2]. However, the high cost of trained healthcare workers, infrastructure, and supplies has limited the development of intensive care units (ICUs) in low-income countries [3]. Additionally, the effectiveness of traditionally resource-intensive critical care in such settings is unknown, and ICU expansion in areas of severe resource constraint is therefore controversial [4].
The burden of critical illness in low-income countries is large and likely to increase with growing urbanization, emerging epidemics and access to hospitals [5–7]. Therefore, data on critical care capacity, considering access to both physical resources and health care professionals, are essential for health system planning but generally lacking or difficult to find [8]. Our objectives were to systematically review the published literature on critical care capacity in low-income countries and to compare population-based estimates of ICU bed capacity to high-and middle-income countries where available.
Methods
Search strategy
We used broad search terms to capture all relevant studies reporting on the existence and characteristics of ICUs, as defined by study authors, in target countries (see S1 File). Target countries were defined by the World Bank as low-income, corresponding to a 2012 gross national income per capita of less than USD1,035 [9].
With the assistance of a librarian, we searched 11 databases, including Medline, EMBASE, LILACS, African Index Medicus, African Journals Online, African Healthline, Opengrey, MedCarib, IMEMR, IMSEAR, and WPRIM. We developed a comprehensive search strategy based on commonly used critical care terms, using keyword and controlled vocabulary terminologies. We searched studies from January 1, 2004—August 6, 2014 with no language restrictions (see S1 File for search strategies). We restricted the search to the past 10 years, reasoning that older studies may underestimate current capacity and would therefore be less useful for health system planning.
We included studies of any design that included information about pediatric and adult ICU capacity (number of beds) in our pre-specified list of countries. Reviews and editorials were included only if they provided new data. We excluded studies reporting only neonatal ICU data and those that focused on temporary or military hospitals.
Searching and data abstraction
Two reviewers (SM, AL) independently screened titles, citations, and abstracts for potentially relevant studies. Full-text versions of all potentially eligible studies were retrieved and reviewed by the same reviewers for inclusion in the review. Agreement between the two reviewers for inclusion of studies among full-text articles was measured using κ [10]. Disagreements were resolved by consensus and adjudication by a third reviewer (NA). Two data abstractors (SM, AL) independently extracted data from selected studies, including demographic data of treated patients, hospital and ICU bed numbers, mechanical ventilation capacity, referral population size, public accessibility, and the hospital funding. If more than one study discussed the same ICU, we abstracted data from the more recent study. Where required, we obtained translations of non-English studies. For studies reporting on national ICU capacity, we extracted total national hospital bed data from World Bank databases [9].
Statistical analysis
We summarized continuous data as mean (standard deviation, SD) if normally distributed or median (interquartile range, IQR) if not normally distributed, and categorical data as count (percentage). We constructed plots and created regression lines of ICU beds per population vs. hospital beds per population using data from included studies and reviews of ICU capacity in high-income countries [11] and plots of ICU beds per population vs. national healthcare expenditure per population using World Bank data [9]. All statistical analyses and plots were performed using R version 3.1.1(R Project for Statistical Computing, Vienna Austria).
Results
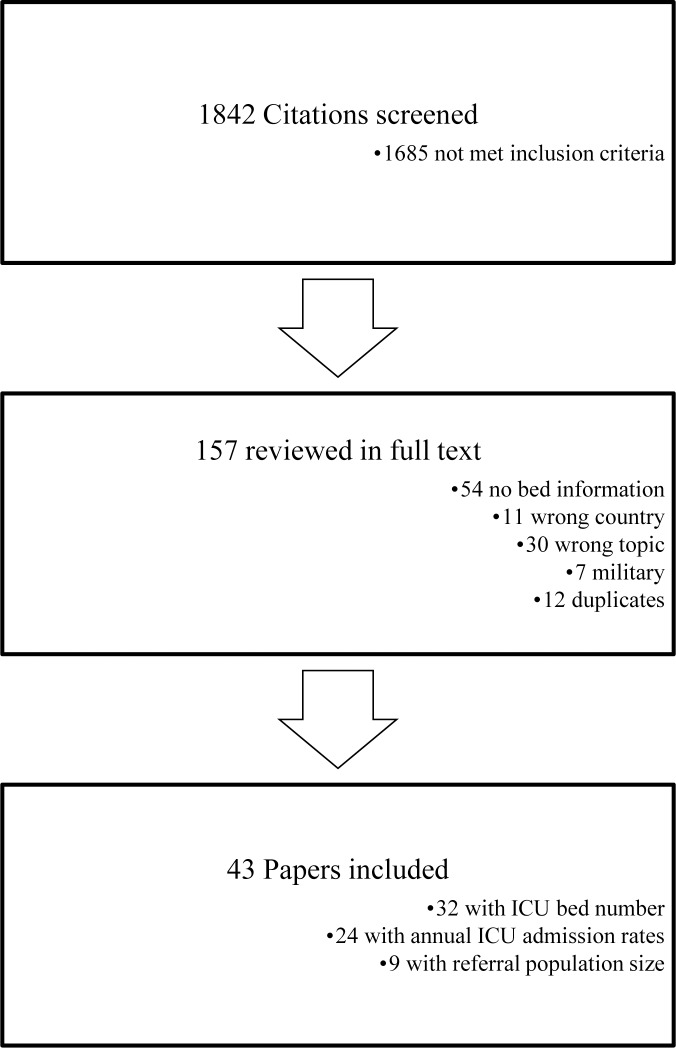
Our search identified 1759 articles, 1603 of which did not meet inclusion criteria after title and abstract review (Fig. 1). Of the 153 articles selected for full-text review, 110 were excluded (see S1 File), with 43 articles meeting selection criteria for final analysis (κ = 0.72, 95% confidence interval, 0.60–0.83). These studies described 36 individual ICUs (Table 1). Four included studies were published in abstract form only and 13 were identified only through searching journals not available on MEDLINE or EMBASE.
Figure 1. Flow diagram of study selection.
References for the citations excluded after full-text review are provided in S1 File.
Table 1. Details of ICU capacity in low-income countries from published studies.
| Country | City | Hospital | ICU type | Hospital bed numbera | ICU bed numbera | Annual ICU admissionsa | Referral Population | Reference |
|---|---|---|---|---|---|---|---|---|
| Cambodia | Phnom-Penh | Cardiological Center of Phnom-Penh | Cardiac, Adult | 32 | 8 | No data | No data | [28] |
| Cambodia | Siem Reap | Angkor Hospital for Children | Pediatric | 50 | 4 | 725 | No data | [29] |
| Comoros Islands | El Maarouf | Centre Hospitalier Regional | Adult | No data | 10 | 760 | No data | [30] |
| Democratic Republic of Congo | Lubumbashi | Provincial Hospital Jason Sendwe | No data | No data | No data | 257 | No data | [31] |
| Democratic Republic of Congo | Goma | DOCS Hospital | Adult | No data | 3 | 141 | No data | [32] |
| Eritrea | Asmara | Orotta national Referral Hospital | Adult | 300 | 9 | 390 | No data | [33] |
| Ethiopia | Addis Ababa | Yekatit 12 Hospital | Burn unit Adult & Pediatric | No data | 18 | No data | No data | [34] |
| Ethiopia | Addis Ababa | Black Lion Hospital | No data | No data | No data | 276 | No data | [35] |
| Ethiopia | Addis Ababa | Tikur Anbassa Hospital | Adult, Medical | 500 | 6 | 591 | No data | [36] |
| Ethiopia | Jimma | Jimma University Specialized Hospital | Adult | 450 | 6 | 370 | 15 million | [37,38] |
| Kenya | Kilifi | Kilifi District Hospital | Pediatric | 60 | No data | No data | 200 000 | [39] |
| Kenya | Nairobi | Kenyatta National Hospital | Adult, Pediatric | 1800 | 20 | 1200 | 32 million | [40] |
| Kenya | Nairobi | Mater Hospital | Adult | 140 | 5 | No data | No data | [41] |
| Kenya | Nakuru | Nakuru Provincial Hospital | No data | 750 | 5 | No data | No data | [42] |
| Malawi | Blantyre | Queen Elizabeth Central Hospital | Adult | No Data | 4–5 | No data | No data | [43] |
| Malawi | Lilongwe | Kamuzu Central Hospital | Adult | 600 | 4 | 234 | 9 million | [15] |
| Mali | Bamako | CHU Gabriel Toure | No data | No Data | No data | 555 | No data | [44] |
| Nepal | Dharan | Koirala Institute of Health Science | Pediatric | No data | 6 (Adult) | 425 (Adult) | No data | [45,46] |
| Nepal | Dhulikhel | Dhulikhel Hospital | Adult | 340 | 5 | No data | No data | [47] |
| Nepal | Kathmandu | Tribhuban University Teaching Hospital | Adult, Pediatric | No data | 6 | 234 | No data | [48,49] |
| Nepal | Mix | Mix | Adult, Pediatric (48 total) | 7040 (whole country) | 450, 60 | No data | 29 million | [18] |
| Nepal | Patan | Patan Hospital | Pediatric | No data | 16, 6 | 126 (pediatric) | No data | [50–52] |
| Nepal | Pokhara | Manipal Teaching Hospital | Adult, Pediatric | 750 | 11 | 992* | 3 million | [53,54] |
| Nepal | Thapathali | Norvic International Hospital and Medical Center | Adult | No data | No data | 700 | No data | [55] |
| Niger | Mirriah town | Mirriah District Hospital | Pediatric | No data | 10 | No data | No data | [56] |
| Tanzania | Dar es Salaam | Muhimbili National Hospital | Adult | 1000 | 10 | 412 | No data | [57,58] |
| Tanzania | Ifakara | St. Francis Hospital | No Data | No data | 10 | 715 | No data | [32] |
| Tanzania | Mwanza | Sekou Toure Regional Referral Hospital | Adult | 375 | 8 | No data | 3.2 million | [59] |
| Tanzania | Mwanza | Budago Medical Center | Adult, Pediatric | 1000 | 12, 10 | No data | 13 million | [16] |
| Togo | Lome | Tokoin University Hospital Center | No data | No data | No data | 1689 | No data | [60] |
| Uganda | Gulu | St. Mary's Hospital Lacor | Adult, Pediatric | 476 | 8 | 218 | No data | [61,62] |
| Uganda | Kampala | Mulago Hospital | Adult, Pediatric, Cardiac | 1500 | 12, 6, 4 | 222 (Adult) | No data | [14,63] |
| Uganda | Masaka | Masaka Regional Referral Hospital | Adult | No data | 1 | No data | No data | [63] |
| Uganda | Mbarara | Mbarara Hospital | Adult, Pediatric | No data | 2 (increasing to 8) | No data | 3 million | [23,64] |
| Zambia | Lusaka | University Teaching Hospital | No data | 1300 | 5 | No data | No data | [42] |
| Zimbabwe | Harare | Parirenyatwa Hospital | Pediatric | No data | 5 | 102 | No data | [65] |
aWhere more than one reference was available for the same hospital, we used the most recent reference for hospital, ICU bed numbers, and ICU admissions per year.
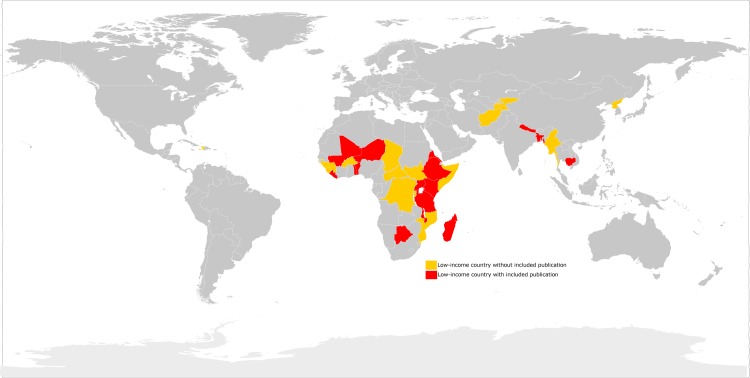
The articles included described ICU capacity in a pre-specified hospital (n = 40) or national (n = 3) region. Based on listed affiliations, 40% (17/43) of articles had corresponding authors based in the low-income country. Of 36 low-income countries defined by the World Bank, only 15 (42%) countries had studies meeting our inclusion criteria (Fig. 2). Therefore, most low-income countries had no literature on ICU capacity, or described ICUs that did not meet our inclusion criteria, such as relief or military hospitals [12,13].
Figure 2. Thirty-six low-income countries included in the search strategy with (n = 15, red) and without (n = 21, yellow) published data on ICU resource availability.
The definitions of critical care varied across the few studies that provided explicit definitions. One described ICU beds as requiring a 'pulse oximeter, mechanical ventilator, suction machine and an anesthesia provider'[14]. Others described the ICU as a 'specialized unit with more skilled nursing care,'[15] or a 'concentrated area where the level of care and supervision is considerably more sophisticated than in the ordinary ward'[16].
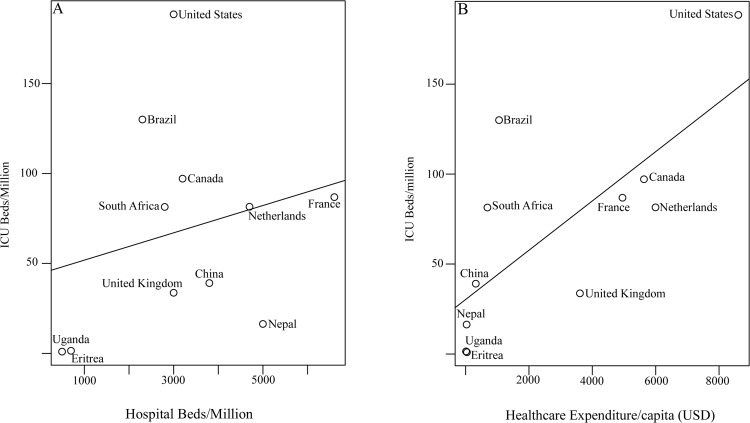
The 43 studies collectively described 36 individual ICUs. Only 3 studies explicitly quantified ICU capacity across a geographic region [17] or country [14,18]; the remaining 40 studies provided single-center descriptions (Table 1). Nine of these 40 studies provided details on referral population size without stating whether additional ICU capacity existed in other hospitals serving the same catchment area. The 36 individual ICUs were distributed among 31 cities, of which 16 had a population greater than 500,000 and 14 were national capitals. Most ICUs (94.1%, 32/34 with data on hospital type) were located in large referral hospitals in major cities. Nepal and Uganda, the only countries with national ICU bed data, had 16.7 and 1.0 ICU beds per million population, respectively [14,18]. When comparing national critical care capacity among low-income countries with data from this review and other countries from other sources [refs], the number of ICU beds per population (Fig. 3) is poorly associated with the number of hospital beds per population (R2 = 0.11, p = 0.37; R2 = 0.24, p = 0.12 if USA is excluded) and strongly associated with annual national healthcare expenditure per capita (R2 = 0.75, p = 0.002).
Figure 3. Comparison of the relationship between ICU beds and hospital beds (panel a), and between ICU beds and national healthcare expenditure per capita (panel b) in low versus selected high-income countries.
There is a non-significant trend between ICU beds and hospital beds (R2 = 0.11, p = 0.37; R2 = 0.24, p = 0.12 if USA is excluded) and a significant trend between ICU beds and national healthcare expenditure per capita (R2 = 0.76, p = 0.002). Supplementary data are from [26,27].
The median annual number of ICU admissions was 401 (IQR 234–711; 24 ICUs with data) the median ICU size was 8 beds (IQR 5–10; 32 ICUs with data), and the median annual admission rate per ICU bed was 58.5 (IQR 41–71, 13 ICUs with data). The mean number of adult and pediatric ICU beds, as a percentage of hospital beds, was 1.5% (SD 0.9%; 15 hospitals with data). Thirteen (36.1%) ICUs explicitly mentioned accepting pediatric patients.
Twenty-two (61%) ICUs provided data on mechanical ventilation capacity, of which 17 (77%) had mechanical ventilators. No study reported whether ICU access was privately or publicly funded. There were few data on physician staffing (1 of 36 ICUs), nurse:patient ratios (2 of 36 ICUs), or the presence of an educational mandate (10 of 36 ICUs).
Discussion
Based on currently available literature, access to critical care resources in World Bank-defined low-income countries is poorly described on the level of individual ICUs and even more sparingly described on a population level. By reported measures, however, ICU resources in low-income countries appear to be sparse. Not surprisingly, the number of ICU beds nationally was related to overall hospital bed capacity and even more significantly to the national expenditure on healthcare.
The inconsistency of definition of an ICU bed implies a significant challenge when comparing resources among countries; even within high-income countries, the definition of an ICU may depend on a higher nurse:patient ratio, the availability of mechanical ventilation, or the ability to support multiple organ systems simultaneously[11,19]. Future research must acknowledge these differences when performing international comparisons [20]. A consensus definition of an ICU, stratified by overall healthcare system capacity, would help with standardizing data collection and may help with planning evaluations of interventions to improve the care and outcomes of seriously ill hospitalized patients.
It is important to note that the mere presence of an ICU does not imply the ability to effectively care for critically ill patients. Similarly, counting the number of critically ill patients from the number of ICU beds in countries with insufficient capacity will lead to a gross underestimate [8]. As reported in a survey of African providers, the ability to comply with sepsis guidelines is minimal in most of Sub-Saharan Africa, despite the presence of an ICU [21]. Additionally, data on many of the features unique to critical care, such as mechanical ventilation and increased nurse:patient ratios, were absent in many of the ICUs described, belying their ability to provide care to critically ill patients. Therefore, there is an urgent need for cross-institutional collaboration for the collection of standardized resource and outcome data through registries and for sharing of appropriate management strategies in resource-constrained low-income countries [2].
There is negligible published research emerging from critical care communities in low-income countries [22]. Reasons for this may include the lack of critical care providers and researchers, funding, academic mentorship, infrastructure to perform research, or barriers to developing available data into publishable research. Given the high burden of critical illness in low-income regions with a collective population of 850 million, the high mortality for patients admitted to ICUs in these countries, and the availability of strategies for their management, there is a rationale for ICUs in all regions of the world [2,23,24]. This must be balanced, however, against the opportunity costs in healthcare systems facing broad challenges of insufficient finding, too few healthcare workers, and poor infrastructure [25]. These challenges notwithstanding, knowledge of pre-existing ICU capacity is vital to plan any future development. For example, in a recent observational study that aimed to assess the worldwide burden of critical illness through convenience sampling of ICU admissions, only 2 of the 84 countries were low-income and 2 of the 730 participating centers were from low-income countries [2].
This systematic review has a number of limitations. While our search strategies were exhaustive, we were unable to capture data on all ICUs in a region due to the lack of relevant publications. Searching of published research literature is an insensitive tool for resource determination, and centralized databases are required to estimate actual acute healthcare capacity [8]. Furthermore, there was substantial variability in availability of relevant data among the included studies and we often relied on single-sentence statements of critical care capacity. Additionally, no independent validation of results was performed. Many health systems have changed drastically since the publication of the studies included in this systematic review, and given the ten-year time frame of our data collection, some features of critical care described may be outdated.
Conclusions
Reliable published data on the availability of critical care resources in low-income regions is sparse. Existing critical care resources are modest and positively associated with national hospital bed capacity and healthcare spending. A global database of ICU capacity, facilitated by networks of critical care providers in low-income countries, would help to evaluate access to and outcomes from critical care, both within and between countries.
Supporting Information
(DOCX)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD (2010) Critical care and the global burden of critical illness in adults. Lancet 376: 1339–1346. 10.1016/S0140-6736(10)60446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, et al. (2014) Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med 2: 380–386. 10.1016/S2213-2600(14)70061-X [DOI] [PubMed] [Google Scholar]
- 3. Dunser MW, Baelani I, Ganbold L (2006) A review and analysis of intensive care medicine in the least developed countries. Crit Care Med 34: 1234–1242. [DOI] [PubMed] [Google Scholar]
- 4.Riviello ED, Letchford S, Achieng L, Newton MW (2011) Critical care in resource-poor settings: Lessons learned and future directions*. Crit Care Med. [DOI] [PubMed]
- 5. Murray CJL, Lopez AD (2013) Measuring the Global Burden of Disease. New England Journal of Medicine 369: 448–457. 10.1056/NEJMra1201534 [DOI] [PubMed] [Google Scholar]
- 6. Annez PC, Linn JF (2010) An agenda for research on urbanization in developing countries: a summary of findings from a scoping exercise. Geneva: The World Bank; [Google Scholar]
- 7. World Health Organization Ebola Response Team (2014) Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med 371: 1481–1495. 10.1056/NEJMoa1411100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Austin S, Murthy S, Wunsch H, Adhikari NK, Karir V, et al. (2014) Access to urban acute care services in high- vs. middle-income countries: an analysis of seven cities. Intensive Care Med 40: 342–352. 10.1007/s00134-013-3174-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Bank Low-Income Countries, available from data.worldbank.org, accessed December 3, 2014.
- 10. Fleiss JL, Cohen J (1973) The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educational and Psychological Measurement 33: 613–619. [Google Scholar]
- 11. Wunsch H, Angus DC, Harrison DA, Collange O, Fowler R, et al. (2008) Variation in critical care services across North America and Western Europe. Crit Care Med 36: 2787–2793, e2781–2789 10.1097/CCM.0b013e318186aec8 [DOI] [PubMed] [Google Scholar]
- 12. von Saint Andre-von Arnim A, Brogan TV, Hertzig J, Kim K, Wurm G, et al. (2011) Intensive care for infants and children in Haiti in April 2010. Pediatr Crit Care Med 12: 393–397. 10.1097/PCC.0b013e318219268d [DOI] [PubMed] [Google Scholar]
- 13. Arul GS, Reynolds J, DiRusso S, Scott A, Bree S, et al. (2012) Paediatric admissions to the British military hospital at Camp Bastion, Afghanistan. Ann R Coll Surg Engl 94: 52–57. 10.1308/003588412X13171221499027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kwizera A, Dunser M, Nakibuuka J (2012) National intensive care unit bed capacity and ICU patient characteristics in a low income country. BMC Res Notes 5: 475 10.1186/1756-0500-5-475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tomlinson J, Haac B, Kadyaudzu C, Samuel JC, Campbell EL, et al. (2013) The burden of surgical diseases on critical care services at a tertiary hospital in sub-Saharan Africa. Trop Doct 43: 27–29. 10.1177/0049475513480773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chalya PL, Gilyoma JM, Dass RM, McHembe MD, Matasha M, et al. (2011) Trauma admissions to the intensive care unit at a reference hospital in Northwestern Tanzania. Scand J Trauma Resusc Emerg Med 19: 61 10.1186/1757-7241-19-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baker T, Lugazia E, Eriksen J, Mwafongo V, Irestedt L, et al. (2013) Emergency and critical care services in Tanzania: a survey of ten hospitals. BMC Health Serv Res 13: 140 10.1186/1472-6963-13-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Acharya SP (2013) Critical care medicine in Nepal: where are we? Int Health 5: 92–95. 10.1093/inthealth/iht010 [DOI] [PubMed] [Google Scholar]
- 19. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, et al. (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302: 2323–2329. 10.1001/jama.2009.1754 [DOI] [PubMed] [Google Scholar]
- 20. Murthy S, Wunsch H (2012) Clinical review: International comparisons in critical care—lessons learned. Crit Care 16: 218 10.1186/cc11140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baelani I, Jochberger S, Laimer T, Otieno D, Kabutu J, et al. (2011) Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care 15: R10 10.1186/cc9410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dhillon G, Dabbo S, Fowler R, Adhikari N (2010) Critical care in the developing world: A literature review. American Journal of Respiratory and Critical Care Medicine 181, 2010:A1641 [Google Scholar]
- 23. Firth P, Ttendo S (2012) Intensive care in low-income countries—a critical need. N Engl J Med 367: 1974–1976. 10.1056/NEJMp1204957 [DOI] [PubMed] [Google Scholar]
- 24. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380: 2095–2128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murthy S, Adhikari NK (2013) Global health care of the critically ill in low-resource settings. Ann Am Thorac Soc 10: 509–513. 10.1513/AnnalsATS.201307-246OT [DOI] [PubMed] [Google Scholar]
- 26. Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD (2010) Critical care and the global burden of critical illness in adults. Lancet 376: 1339–1346. 10.1016/S0140-6736(10)60446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wunsch H, Angus DC, Harrison DA, Collange O, Fowler R, et al. (2008) Variation in critical care services across North America and Western Europe. Crit Care Med 36: 2787–2793, e2781–2789 10.1097/CCM.0b013e318186aec8 [DOI] [PubMed] [Google Scholar]
- 28. Morestin S, Lesbre JP, Grinda JM, Deloche A (2004) [Results of 17 months' surgical experience in the Cardiological Centre of Phnom-Penh (CCPP). The challenge of sanitation in a developing country]. Arch Mal Coeur Vaiss 97: 285–290. [PubMed] [Google Scholar]
- 29. Stoesser N, Emary K, Soklin S, Peng An K, Sophal S, et al. (2013) The value of intermittent point-prevalence surveys of healthcare-associated infections for evaluating infection control interventions at Angkor Hospital for Children, Siem Reap, Cambodia. Trans R Soc Trop Med Hyg 107: 248–253. 10.1093/trstmh/trt005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Durasnel P, Gallet de Santerre P, Merzouki D, Ridhoine M, Charif M, et al. (2005) [Should mechanical ventilation be used in ICU patients in developing countries?]. Med Trop (Mars) 65: 537–542. [PubMed] [Google Scholar]
- 31. Muteya MM, Kabey AK, Lubanga TM, Tshamba HM, Nkoy AM (2013) Prognosis of tetanus patients in the intensive care unit of Provincial Hospital Jason Sendwe, Lubumbashi, DR Congo. Pan Afr Med J 14: 93 10.11604/pamj.2013.14.93.2180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dunser MW, Baelani I, Ganbold L (2006) A review and analysis of intensive care medicine in the least developed countries. Crit Care Med 34: 1234–1242. [DOI] [PubMed] [Google Scholar]
- 33. Anichini V, Zagli G, Goitom H, Cianchi G, Cecchi A, et al. (2013) Challenges of Improving Intensive Care Medicine in Eritrea: Impact of an Italian Cooperative Project of Educational and Clinical Support. Open Journal of Anesthesiology 3: 315–319. [Google Scholar]
- 34. Mulat T, Salemark LO (2006) Description of patients admitted to a burn unit of Yekatit 12 Hosptial, Addis Ababa, Ethiopia. Ethiop Med J 44: 369–375. [PubMed] [Google Scholar]
- 35. Smitson C, Giday A, Zaeh S, Weldeyes E, O'Mara J (2013) Trends in cardiovascular disease in ethiopia: A 30-year retrospective analysis of medical-ICU admissions. Annual Scientific Sessions 2013; Vancouver, Canada. [Google Scholar]
- 36. Melaku Z, Alemayehu M, Oli K, Tizazu G (2006) Pattern of admissions to the medical intensive care unit of Addis Ababa University Teaching Hospital. Ethiop Med J 44: 33–42. [PubMed] [Google Scholar]
- 37. Smith ZA, Ayele Y, McDonald P (2013) Outcomes in critical care delivery at Jimma University Specialised Hospital, Ethiopia. Anaesth Intensive Care 41: 363–368. [DOI] [PubMed] [Google Scholar]
- 38. Agalu A, Ayele Y, Bedada W, Woldie M (2012) Medication administration errors in an intensive care unit in Ethiopia. Int Arch Med 5: 15 10.1186/1755-7682-5-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Olotu A, Ndiritu M, Ismael M, Mohammed S, Mithwani S, et al. (2009) Characteristics and outcome of cardiopulmonary resuscitation in hospitalised African children. Resuscitation 80: 69–72. 10.1016/j.resuscitation.2008.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ngumi ZW (2006) Nosocomial infections at Kenyatta National Hospital Intensive-Care Unit in Nairobi, Kenya. Dermatology 212 Suppl 1: 4–7. [DOI] [PubMed] [Google Scholar]
- 41. Murunga EM, Reriani M, Otieno CF, Wanyoike NM (2005) Comparison of antibiotic use between an 'open' and a 'closed' intensive care unit. East Afr Med J 82: 414–417. [DOI] [PubMed] [Google Scholar]
- 42. MacLeod JB, Okech M, Labib M, Aphivantrakul P, Lupasha E, et al. (2011) Evaluation of trauma and critical care training courses on the knowledge and confidence of participants in Kenya and Zambia. World J Surg 35: 9–16. 10.1007/s00268-010-0810-z [DOI] [PubMed] [Google Scholar]
- 43. Pollach G, Namboya F (2013) Preventing intensive care admissions for sepsis in tropical Africa (PICASTA): an extension of the international pediatric global sepsis initiative: an African perspective. Pediatr Crit Care Med 14: 561–570. 10.1097/PCC.0b013e318291774b [DOI] [PubMed] [Google Scholar]
- 44. Diango DM, Almeimoune AM, Beye SA, Iknane AG, Keita M, et al. (2012) [Problems related to informing families of patients in intensive care unit AT CHU Gabriel Toure (Mali)]. Mali Med 27: 66–70. [PubMed] [Google Scholar]
- 45. Baranwal AK, Ravi R, Singh R (2009) Diarrhea associated hemolytic uremic syndrome: a 3-year PICU experience from Nepal. Indian J Pediatr 76: 1180–1182. 10.1007/s12098-009-0275-y [DOI] [PubMed] [Google Scholar]
- 46. Joshi S, Agrawal B, Deo GP, Bhattarai BK, Rahman TR, et al. (2006) Percutaneous dilational tracheostomy: an initial experience in community based teaching hospital. Kathmandu Univ Med J (KUMJ) 4: 275–280. [PubMed] [Google Scholar]
- 47. Ranjit S, Bhattarai B (2011) Incidence and risk factor for ventilator-associated pneumonia in Kathmandu University Hospital. Kathmandu Univ Med J (KUMJ) 9: 28–31. [DOI] [PubMed] [Google Scholar]
- 48. Shrestha GS, Gurung R, Amatya R (2011) Comparison of Acute Physiology, Age, Chronic Health Evaluation III score with initial Sequential Organ Failure Assessment score to predict ICU mortality. Nepal Med Coll J 13: 50–54. [PubMed] [Google Scholar]
- 49. Acharya SP, Pradhan B, Marhatta MN (2007) Application of "the Sequential Organ Failure Assessment (SOFA) score" in predicting outcome in ICU patients with SIRS. Kathmandu Univ Med J (KUMJ) 5: 475–483. [PubMed] [Google Scholar]
- 50. Basnet S, Adhikari N, Koirala J (2011) Challenges in setting up pediatric and neonatal intensive care units in a resource-limited country. Pediatrics 128: e986–992. 10.1542/peds.2010-3657 [DOI] [PubMed] [Google Scholar]
- 51. Basnet S, Shrestha S, Ghimire A, Timila D, Gurung J, et al. (2012) Impact after one year of establishing pediatric ICU in Nepal. In: Medicine CC, editor; Houston, United States: Critical Care Medicine; 10.3390/jpm2020050 [DOI] [Google Scholar]
- 52. Adhikari N, Avila M, Kache S, Grover T, Ansari I, et al. (2011) Establishment of Paediatric and Neonatal Intensive Care Units at Patan Hospital, Kathmandu: Critical Determinants and Future Challenges. Journal of Nepal Paediatric Society 31: 49–56. [Google Scholar]
- 53. Paudel R, Palaian S, Bishnurath G, Hom K, Sah A, et al. (2011) Clinical Profile And Drug Utilization Pattern In An Intensive Care Unit Of A Teaching Hospital In Western Nepal. Archives of Pharmacy Practice 2: 163–169. [Google Scholar]
- 54. Shankar PR, Partha P, Dubey AK, Mishra P, Deshpande VY (2005) Intensive care unit drug utilization in a teaching hospital in Nepal. Kathmandu Univ Med J (KUMJ) 3: 130–137. [PubMed] [Google Scholar]
- 55. Pnadey R, Chokhani R, N BK (2011) Use of non invasive ventilation in patients with respiratory failure in Nepal. Kathmandu Univ Med J (KUMJ) 9: 256–259. [DOI] [PubMed] [Google Scholar]
- 56. Blackwell N, Oumarou M, Illa H, Gignoux E (2011) The treatment of severe and severe complicated malaria in young children in a resource poor setting—lessons for Australasian intensive care units (ALIMA/BEFEN malaria project, Niger); Brisbane, Australia. Anaesthesia and Intensive Care. pp. 1142–1148. [Google Scholar]
- 57. Ndugulile F, Jureen R, Harthug S, Urassa W, Langeland N (2005) Extended spectrum beta-lactamases among Gram-negative bacteria of nosocomial origin from an intensive care unit of a tertiary health facility in Tanzania. BMC Infect Dis 5: 86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Muganyizi PS, Shagdara MS (2011) Predictors of extra care among magnesium sulphate treated eclamptic patients at Muhimbili National Hospital, Tanzania. BMC Pregnancy Childbirth 11: 41 10.1186/1471-2393-11-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mitchell KB, Giiti G, Gallagher JJ (2013) Survey of care and evaluation of East African burn unit feasibility: an academic burn center exchange. J Burn Care Res 34: 78–81. 10.1097/BCR.0b013e318269be63 [DOI] [PubMed] [Google Scholar]
- 60. Djibril AM, Tomta K, Balaka K, Bagny A, M'Ba K B, et al. (2010) [Hematemesis in Togo: findings of a 12-month study in an intensive care unit]. Med Trop (Mars) 70: 311–312. [PubMed] [Google Scholar]
- 61. Towey RM, Ojara S (2008) Practice of intensive care in rural Africa: an assessment of data from Northern Uganda. Afr Health Sci 8: 61–64. [PMC free article] [PubMed] [Google Scholar]
- 62. Towey RM, Ojara S (2007) Intensive care in the developing world. Anaesthesia 62 Suppl 1: 32–37. [DOI] [PubMed] [Google Scholar]
- 63. Jacob ST, Moore CC, Banura P, Pinkerton R, Meya D, et al. (2009) Severe sepsis in two Ugandan hospitals: a prospective observational study of management and outcomes in a predominantly HIV-1 infected population. PLoS One 4: e7782 10.1371/journal.pone.0007782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Webster K, Buckley H, Ttendo S (2012) Obstetric critical care in south-west Uganda: An 18-month survery of maternal critical care admissions and outcomes; Liverpook, UK. International Journal of Obstetric Anesthesia. pp. S2–S55. [Google Scholar]
- 65. Pazvakavambwa IE (2004) An experience with surgical admissions to a paediatric ICU (PICU) in Harare, Zimbabwe. Cent Afr J Med 50: 107–110. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.