INTRODUCTION
Bariatric surgery is the most effective therapy available for significant and sustainable weight loss in morbidly obese patients.1,2 As a result of the rising prevalence of obesity, improvements in perioperative safety, and expanded insurance coverage, bariatric surgery utilization has increased in the last decade.3,4 Changes in procedure use over time reflect emerging evidence regarding the comparative safety and effectiveness of available procedures.1,2,5 An understanding of current trends in bariatric procedure utilization is essential to primary care physicians counseling morbidly obese patients considering surgical intervention.
Though recent reports have documented increased use of sleeve gastrectomy (SG) in certain populations,4,6 the extent to which this procedure has supplanted other procedures, such as Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB), is poorly understood. Moreover, it is unclear if relative utilization differs within clinical subgroups that might be predicted to have better outcomes with a specific procedure. To better understand current trends in bariatric surgery utilization, we examined procedure rates in patients undergoing bariatric surgery in Michigan between 2006 and 2013.
METHODS
We studied adults undergoing primary inpatient and outpatient bariatric surgery within the 39-hospital Michigan Bariatric Surgery Collaborative (MBSC) between June 2006 and December 2013. Details of prospective data collection have been previously described.5 In brief, trained data abstractors review the medical record and collect information on patient demographics, comorbidities, intraoperative and perioperative processes, and 30-day outcomes of all patients undergoing bariatric surgery in participating hospitals. Hospitals are audited annually to ensure data accuracy. There is no missing data.
We calculated relative utilization stratified by procedure type and year of procedure, and we examined procedure rates within clinically important subgroups. Cuzick's test for trend was used to assess differences in procedure use across years, and Chi squared was used to evaluate differences in procedure use between subgroups. All p-values are two-tailed, with alpha set at 0.05. Analyses were performed using STATA version 12.1(StataCorp). This study was considered exempt by the Institutional Review Board at the University of Michigan.
RESULTS
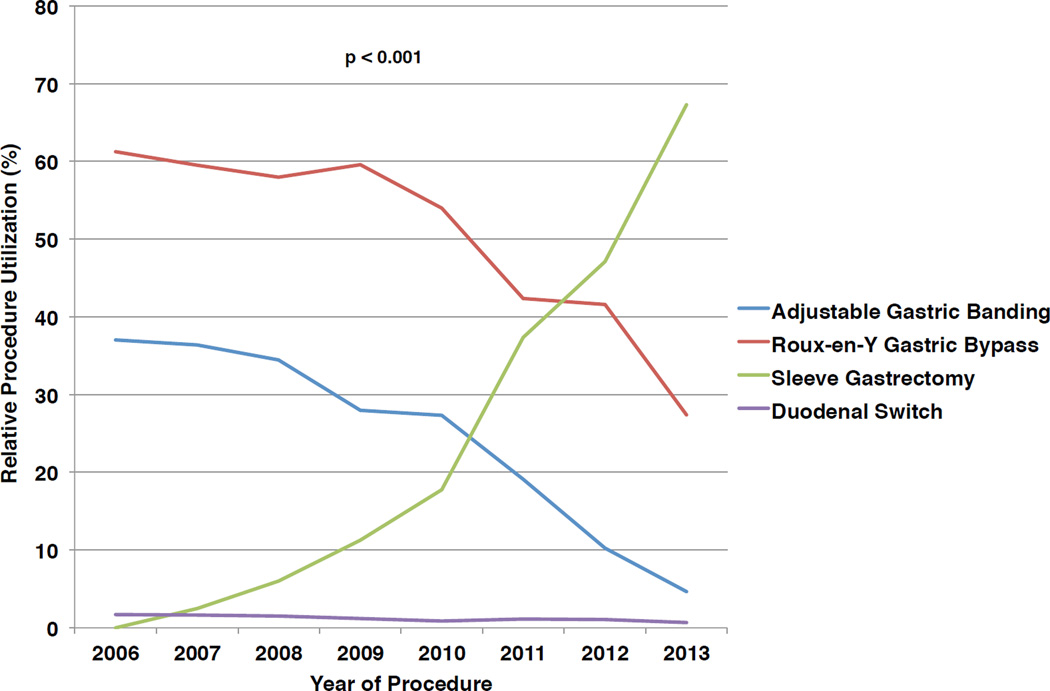
The final cohort included 43,732 patients undergoing bariatric surgery. As shown in Figure 1, relative utilization of SG increased 61%, from 6.0%(95%CI:5.4–6.6%) of all procedures in 2008, to 67.3%(95%CI:66.0–68.6%) of all procedures in 2013. During the same period, use of RYGB decreased from 58.0%(95%CI:56.8–59.1%) to 27.4%(95%CI:26.2–28.6), and use of LAGB decreased from 34.5%(95%CI:33.3–35.6%) to 4.6%(95%CI:4.1–5.2).
Figure 1.
Relative utilization of common bariatric procedures in Michigan during the period June 2006 to December 2013.
Changes in utilization over time within clinically important subgroups (Table 1) were similar to the overall trend: use of SG increased, while rates of RYGB and LAGB decreased. While SG was the most common procedure across all subgroups in 2012 and 2013, SG rates were relatively lower in patients 65 years and older [43.0%, 95%CI: 39.4–46.6%vs.57.9%, 95%CI:56.9–58.9% in patients <65 years, P< 0.001], patients with gastroesophageal reflux disease (52.9%, 95%CI:51.9–54.5%vs.60.8%,95%CI:59.5–62.1% without reflux, P<0.001) and patients with type II diabetes (49.1%,95%CI:48.3–51.6% vs.60.4%,95%CI:59.3–61.5% without diabetes, P< 0.001).
Table 1.
Trends in relative procedure utilization of the three most commonly used bariatric procedures during the period June 2006 to December 2013, stratified by clinically important patient subgroups [GERD: Gastroesophageal Reflux Disease; CI: Confidence Interval; values shown are number (percentage) unless otherwise noted; p-values represent Cuzick's test for trend
| 2006 – 2007 | 95% CI | 2008 – 2009 | 95% CI | 2010 – 2011 | 95% CI | 2012 – 2013 | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| Total | 5610 (100.0) | 14,384 (100.0) | 12,843 (100.0) | 10,895 (100.0) | |||||
| Adjustable Gastric Banding | 2046 (36.5) | 35.2 – 37.7 | 4467 (31.1) | 30.3 – 31.8 | 3006 (23.4) | 22.7 – 24.1 | 820 (7.5) | 7.0 – 8.0 | |
| Roux-en-Y Gastric Bypass | 3356 (59.8) | 58.5 – 61.1 | 8459 (58.8) | 58.0 – 59.6 | 6222 (48.4) | 47.5 – 49.3 | 3780 (34.7) | 33.8 – 35.6 | < 0.001 |
| Sleeve Gastrectomy | 115 (2.0) | 1.7 – 2.4 | 1265 (8.8) | 8.3 – 9.2 | 3486 (27.1) | 26.4 – 27.9 | 6201 (56.9) | 56.0 – 57.8 | |
| Age < 65 years | 5446 (97.1) | 13,714 (95.3) | 12,148 (94.6) | 10,174 (93.4) | |||||
| Adjustable Gastric Banding | 1961 (36.0) | 34.7 – 37.3 | 4135 (30.2) | 29.4 – 30.9 | 2766 (22.8) | 22.0 – 23.5 | 723 (7.1) | 6.6 – 7.6 | |
| Roux-en-Y Gastric Bypass | 3279 (60.2) | 58.9 – 61.5 | 8173 (58.6) | 58.8 – 60.4 | 5821 (47.9) | 47.0 – 48.8 | 3477 (34.2) | 33.2 – 35.1 | < 0.001 |
| Sleeve Gastrectomy | 114 (2.1) | 1.7 – 2.5 | 1213 (8.8) | 8.4 – 9.3 | 3445 (28.4) | 27.6 – 29.2 | 5891 (57.9) | 56.9 – 58.9 | |
| Age ≥ 65 years | 164 (2.9) | 670 (4.7) | 695 (5.4) | 721 (6.6) | |||||
| Adjustable Gastric Banding | 85 (51.8) | 44.2 – 59.5 | 332 (49.6) | 45.8 – 53.3 | 240 (34.5) | 31.0 – 38.1 | 97 (13.4) | 11.0 – 15.9 | |
| Roux-en-Y Gastric Bypass | 77 (47.0) | 39.2 – 54.6 | 286 (42.7) | 38.9 – 46.4 | 401 (57.7) | 54.0 – 61.4 | 303 (42.0) | 38.4 – 45.6 | < 0.001 |
| Sleeve Gastrectomy | 1 (0.6) | 0 – 1.8 | 52 (7.8) | 5.7 – 9.8 | 41 (5.9) | 4.1 – 7.6 | 310 (43.0) | 39.4 – 46.6 | |
| BMI < 60 kg/m^2 | 5088 (90.7) | 13134 (91.3) | 11772 (91.7) | 9965 (91.5) | |||||
| Adjustable Gastric Banding | 1969 (38.7) | 37.4 – 40.0 | 4320 (32.9) | 32.1 – 33.7 | 2909 (24.7) | 23.9 – 25.5 | 786 (7.9) | 7.3 – 8.4 | |
| Roux-en-Y Gastric Bypass | 2944 (57.9) | 56.5 – 59.2 | 7623 (58.0) | 57.2 – 58.9 | 5607 (47.6) | 46.7 – 48.5 | 3395 (34.1) | 33.1 – 35.0 | < 0.001 |
| Sleeve Gastrectomy | 96 (1.9) | 1.5 – 2.3 | 1027 (7.8) | 7.4 – 8.3 | 3144 (26.7) | 25.9 – 27.5 | 5706 (57.3) | 56.3 – 58.2 | |
| BMI ≥ 60 kg/m^2 | 522 (9.3) | 1250 (8.7) | 1071 (8.3) | 930 (8.5) | |||||
| Adjustable Gastric Banding | 77 (14.8) | 11.7 – 17.8 | 147 (11.8) | 10.0 – 13.5 | 97 (9.1) | 7.3 – 10.8 | 34 (3.7) | 2.4 – 4.9 | |
| Roux-en-Y Gastric Bypass | 412 (78.9) | 75.4 – 82.4 | 836 (66.9) | 64.3 – 69.5 | 615 (57.4) | 54.4 – 60.4 | 385 (41.4) | 38.2 – 44.6 | < 0.001 |
| Sleeve Gastrectomy | 19 (3.6) | 2.0 – 5.2 | 238 (19.0) | 16.9 – 21.2 | 342 (31.9) | 29.1 – 34.7 | 495 (53.2) | 50.0 – 56.4 | |
| GERD | 2754 (49.1) | 6874 (47.8) | 6422 (50.0) | 5552 (51.0) | |||||
| Adjustable Gastric Banding | 975 (35.4) | 33.6 – 37.2 | 2023 (29.4) | 28.4 – 30.5 | 1556 (24.2) | 23.2 – 25.3 | 461 (8.3) | 7.6 – 9.0 | |
| Roux-en-Y Gastric Bypass | 1662 (60.4) | 58.5 – 62.2 | 4171 (60.7) | 59.5 – 61.8 | 3249 (50.6) | 49.4 – 51.8 | 2096 (37.8) | 49.3 – 51.8 | < 0.001 |
| Sleeve Gastrectomy | 45 (1.63) | 1.2 – 2.1 | 553 (8.0) | 7.4 – 8.7 | 1558 (24.3) | 23.2 – 25.3 | 2953 (53.2) | 51.9 – 54.5 | |
| No GERD | 2856 (50.9) | 7510 (52.2) | 6421 (50.0) | 5343 (49.0) | |||||
| Adjustable Gastric Banding | 1071 (37.5) | 35.7 – 39.3 | 2444 (32.5) | 31.5 – 33.6 | 1450 (22.6) | 21.6 – 23.6 | 359 (6.7) | 6.0 – 7.4 | |
| Roux-en-Y Gastric Bypass | 1694 (59.3) | 57.5 – 61.1 | 4288 (57.1) | 56.0 – 58.2 | 2973 (46.3) | 45.1 – 47.5 | 1684 (31.5) | 30.3 – 32.8 | < 0.001 |
| Sleeve Gastrectomy | 70 (2.4) | 1.9 – 3.0 | 712 (9.5) | 8.8 – 10.1 | 1928 (30.0) | 28.9 – 31.1 | 3248 (60.8) | 59.4 – 62.1 | |
| Type II Diabetes | 1720 (30.6) | 4721 (32.8) | 4202 (32.7) | 3625 (33.3) | |||||
| Adjustable Gastric Banding | 552 (32.1) | 29.9 – 34.3 | 1276 (27.0) | 25.8 – 28.3 | 854 (20.3) | 19.1 – 21.5 | 222 (6.1) | 5.3 – 6.9 | |
| Roux-en-Y Gastric Bypass | 1110 (64.5) | 62.3 – 66.8 | 2955 (62.6) | 61.2 – 64.0 | 2304 (54.8) | 53.3 – 56.3 | 1563 (43.1) | 41.5 – 44.7 | < 0.001 |
| Sleeve Gastrectomy | 32 (1.9) | 1.2 – 2.5 | 428 (9.1) | 8.2 – 9.9 | 996 (23.7) | 22.4 – 25.0 | 1810 (49.9) | 48.3 – 51.6 | |
| No Type II Diabetes | 3890 (69.4) | 9663 (67.2) | 8641 (67.3) | 7270 (66.7) | |||||
| Adjustable Gastric Banding | 1494 (38.4) | 36.9 – 39.9 | 3191 (33.0) | 32.1 – 34.0 | 2152 (24.9) | 24.0 – 25.8 | 598 (8.2) | 7.6 – 8.8 | |
| Roux-en-Y Gastric Bypass | 2246 (57.7) | 56.2 – 59.3 | 5504 (57.0) | 56.0 – 57.9 | 3918 (45.3) | 44.3 – 46.4 | 2217 (30.5) | 29.4 – 31.6 | < 0.001 |
| Sleeve Gastrectomy | 83 (2.1) | 1.7 – 2.6 | 837 (8.7) | 8.1 – 9.2 | 2490 (28.8) | 27.9 – 29.8 | 4391 (60.4) | 59.3 – 61.5 | |
DISCUSSION
Analysis of recent practice in Michigan revealed SG to be the most common procedure performed for patients pursuing bariatric surgery, surpassing RYGB in 2012. Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type II diabetes,1 SG has become the predominant procedure in both groups.
This analysis is limited to procedures performed in a single state. While use of this detailed bariatric-specific registry in Michigan allows a more accurate assessment of trends in procedure utilization than administrative data, it may limit the generalizability of our results. Although unmeasured confounders may influence procedure use, this bias is unlikely to alter these findings given the large magnitude of the differences observed.
Although long-term outcomes of SG are still unclear, these changes may reflect the favorable perioperative safety profile and emerging evidence of successful weight-loss at 2 to 3 years after SG.5 These findings are important to inform primary care physicians of the predominant procedure used in bariatric surgery today, regardless of preexisting comorbidity, and will assist the preoperative counseling of patients considering surgical therapy for morbid obesity.
Acknowledgments
Funding/Support: Dr. Reames is supported by a grant from the National Cancer Institute (5T32CA009672-23).
Role of the Sponsors: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: BNR had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr. Dimick reports serving as consultant and having an equity interest in ArborMetrix Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in the study. BNR, JFF, DB, and AMC have no conflicts of interest to disclose.
Disclaimer: The views expressed in this Research Letter do not necessarily represent those of the US government.
REFERENCES
- 1.Hainer V, Toplak H, Mitrakou A. Treatment Modalities of Obesity: What fits whom? Diabetes Care. 2008;31(Supplement 2):S269–S277. doi: 10.2337/dc08-s265. [DOI] [PubMed] [Google Scholar]
- 2.Padwal R, Klarenbach S, Wiebe N, et al. Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med. 2011 Oct;26(10):1183–1194. doi: 10.1007/s11606-011-1721-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg. 2011 Aug;213(2):261–266. doi: 10.1016/j.jamcollsurg.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen NT, Nguyen B, Gebhart A, Hohmann S. Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013 Feb;216(2):252–257. doi: 10.1016/j.jamcollsurg.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Carlin AM, Zeni TM, English WJ, et al. The Comparative Effectiveness of Sleeve Gastrectomy, Gastric Bypass, and Adjustable Gastric Banding Procedures for the Treatment of Morbid Obesity. Annals of Surgery. 2013;257(5):791–797. doi: 10.1097/SLA.0b013e3182879ded. [DOI] [PubMed] [Google Scholar]
- 6.Lazzati A, Guy-Lachuer R, Delaunay V, Szwarcensztein K, Azoulay D. Bariatric surgery trends in France: 2005–2011. Surg Obes Relat Dis. 2013 Aug 26; doi: 10.1016/j.soard.2013.07.015. [DOI] [PubMed] [Google Scholar]