Abstract
In this article, we present the results of a systematic review of state, county, and municipal restrictions on the use of electronic cigarettes (e-cigarettes) in public spaces within the United States, alongside an overview of the current legal landscape. The lack of federal guidance leaves lower-level jurisdictions to debate the merits of restrictions on use in public spaces without sufficient scientific research. As we show through a geographic assessment of restrictions, this has resulted in an inconsistent patchwork of e-cigarette use bans across the United States of varying degrees of coverage. Bans have emerged over time in a manner that suggests a “bottom up” diffusion of e-cigarette clean air policies. Ultimately, the lack of clinical and scientific knowledge on the risks and potential harm reduction benefits has led to precautionary policymaking, which often lacks grounding in empirical evidence and results in spatially uneven diffusion of policy.
Keywords: electronic cigarettes, policy debate, health policy, geographic distribution of policy
1. Introduction
In January 2014, NBC’s telecast of the Golden Globe Awards drew criticism when stars such as Julia Louis Dreyfus and Leonardo DiCaprio were shown puffing on electronic cigarettes, or “e-cigarettes,” during the award show (Git 2014). Among the critics were four U.S. Senators who wrote an open letter to NBC and the Hollywood Foreign Press, requesting that steps be taken to prevent showing e-cigarette usage in future broadcasts, arguing that, “Such action would help to avoid the glamorization of smoking and protect the health of young fans” (Durbin et al. 2014). These senators and other lawmakers in favor of various types of restrictions argue that the health effects and safety of e-cigarette use are unknown, that allowing public representations may re-normalize smoking and contribute to clean air enforcement problems, and that e-cigarettes are a danger to young people for whom they may serve as a gateway to conventional cigarette use. Opponents of restrictions argue that e-cigarettes offer a safer alternative to tobacco smoking, and e-cigarette usage should not be excessively discouraged in the interests of harm reduction.
Electronic cigarette usage is novel and, as a result, policy is changing quickly and has outpaced scientific knowledge on the health effects of use and exposure. A range of restrictions on e-cigarette use have been introduced in recent years; however, these responses have not been uniform at the geographic level at which policies have been passed (e.g. municipal, county, state), nor across the types of spaces that have been regulated (e.g. schools, workplaces, bars, restaurants, parks). The variation in responses to e-cigarette use leads us to consider the following questions in this article:
What are the legal foundations of the implementation of e-cigarette clean air policies in the United States?
What are the temporal and geographic patterns of the enactment of e-cigarette clean air policies across the U.S.?
What are the key points in debates surrounding enactment of these policies and the public health implications of prohibiting e-cigarette use in public spaces?
We address the first question through a review of current empirical research on e-cigarettes, followed by an outline of the legal decisions and patterns of diffusion relevant to the current policy environment in the U.S. We address the second question by assessing underutilized data on the geographic patterns of e-cigarette clean air restrictions temporally and spatially across the U.S. For the final question, we summarize key points in the debate surrounding e-cigarette clean air policies, while providing examples of discussions stemming from these debates. In considering these issues, we address the role of place in policymaking both with respect to the spaces in which restrictions are being enacted as well as the geographic distribution of these policies. While the policy data used for this paper are specific to the U.S., these policy debates are occurring globally (Gartner and McNeill 2010), and thus the shifting landscape of e-cigarette policy may have broader implications.
2. The current state of empirical research on e-cigarettes
Electronic cigarettes are battery-operated devices that simulate smoking. A practice sometimes described as “vaping,” users inhale vapor produced from the combustion of a solution, usually water and propylene glycol (Riker et al. 2012). The liquid is often flavored like tobacco, menthol, or with various sweet or fruity flavors, and may or may not include nicotine. Many e-cigarettes offer adjustable doses of nicotine through the attachment of cartridges. While vaping is largely believed to be safer than smoking because e-cigarettes contain fewer toxins and particulates than smoke from tobacco, the recent introduction of e-cigarettes means that the long-term effects of vaping or exposure to second-hand vapors is not yet conclusively established. While also advocated by some as a tool to reduce or cease smoking, studies have not yet definitively established whether e-cigarettes are an effective smoking cessation tool, nor established the health effects of vaping as an adjunct to smoking (Riker et al. 2012). Vapors emitted from e-cigarettes contain some toxins; however, the toxicity levels were 9 to 450 times lower than those in cigarette smoke (Goniewicz et al. 2014) and bystander exposure to vapors is likely much safer than exposure to second-hand smoke (McAuley et al. 2012; Schripp et al. 2012; Hajek et al. 2014). Despite these findings, public health concerns remain in that where restrictions on tobacco smoke are already in place, allowing vaping may still expose bystanders to secondhand particulates, which have potential health effects (Schober et al. 2014). The assessment of the toxicity levels ultimately remains uncertain due to weak federal regulatory practices and the resulting lack of consistent quality control (Cobb et al. 2010; Goniewicz, Hajek, and McRobbie 2014).
The practice of vaping has grown in popularity. In a 2012 survey of Australia, Canada, the U.K., and the U.S., almost half of respondents were aware of e-cigarettes, although this varied greatly from 20% in Australia to 73% in the U.S. (Adkison et al. 2013). The same survey shows the U.S. leading the other three countries by considerable margins in both lifetime (have tried at least once) and current e-cigarette use (Adkison et al. 2013). Awareness of e-cigarettes has grown rapidly in the U.S.: from four in ten adults in 2010 to three in four adults in 2012 (CDC 2013a; Adkison et al. 2013; King et al. 2013). The CDC data from June 2014 suggests that 14.1% of American adults have tried e-cigarettes at least once (Agaku et al. 2014). Of those Americans who reported themselves as current e-cigarette users, 17.9% reported everyday use (Agaku et al. 2014). Research suggests that current smokers are more likely to use e-cigarettes than the general population, and former smokers are also slightly more likely to “vape” than those who have never been smokers (CDC 2013a; King et al. 2013; Pearson et al. 2012). Individuals who reported currently using e-cigarettes were more likely to be recent quitters of smoking than long-term quitters (Zhu et al. 2013). Research using data collected in 2012 found that among never smokers, 1.0% had tried e-cigarettes, and among those smokers who quit more than one year ago, 2.4% had tried them (Zhu et al. 2013). This was in stark contrast to 26.8% of those who quit smoking during the past year who reported trying e-cigarettes at least once and 32.2% of current smokers. Of those who had tried e-cigarettes, 54.9% indicated one of the reasons they did so was because they were trying to quit smoking, and 49.9% reported trying e-cigarettes because they believed them to be safer than cigarettes (Zhu et al. 2013).
E-cigarette use is also increasing among youth (CDC 2013b). The CDC reported that the percentage of high school students who reported using e-cigarettes at least once rose from 4.7% in 2011 to 10.0% in 2012 (CDC 2013b). In 2012, 76.3% of middle and high schoolers who reported using an e-cigarette during the last 30 days also reported smoking conventional cigarettes (CDC 2013b). Among middle school students, 1 in 5 students who reported trying e-cigarettes had not yet tried tobacco cigarettes (CDC 2013b). Research specifically on adolescent boys suggests that while awareness is high, only a minority of respondents reported a willingness to try e-cigarettes (Pepper et al. 2013). Current tobacco smoking remains the strongest predictor of e-cigarette use among teens (Camenga et al. 2014).
Tobacco smoking is the leading cause of preventable death in the U.S., accounting for 1 in every 5 deaths each year (CDC 2014). Knowledge about the negative health effects of smoking, combined with increased tobacco regulation in recent decades has led to a considerable decrease in smoking across the U.S. (CDC 2014). Many smokers who seek to quit use outpatient treatments for reducing the withdrawal symptoms of nicotine. Such therapies often include alternative nicotine delivery systems such as chewing gum, patches, and lozenges (Riker et al. 2012). Similarly, e-cigarettes offer an alternative form of nicotine delivery and may be used in smoking cessation treatment. Yet, the extent to which e-cigarette usage may be an effective smoking cessation tool is uncertain. Several studies relying on surveys using convenience samples reported that respondents perceive e-cigarettes as safer than tobacco (Etter and Bullen 2011) and that they use e-cigarettes in an attempt to abstain from smoking (Etter 2010; Etter and Bullen 2011; Siegel, Tanwar, and Wood 2011). Recent longitudinal research demonstrated that e-cigarettes help prevent smoking relapse and contribute to cessation (Etter and Bullen 2014). Preliminary research suggests that e-cigarettes may not be entirely harmless, but are considerably safer than smoking tobacco and that health benefits are expected for smokers who switch to vaping (Farsalinos and Polosa 2014; Meier, Tackett, and Wagener 2013). Additionally, some research showed that smokers who use e-cigarettes may be more highly motivated to quit smoking (Pokhrel et al. 2013). Overall, these findings suggest that e-cigarettes may serve as a means of harm reduction in public health efforts to reduce tobacco smoking.
3. The legal context of e-cigarette regulation
E-cigarettes were invented in China and introduced to U.S. markets during 2006-2007 (Riker et al. 2012). The FDA responded quickly in 2008 and blocked all new shipments of e-cigarettes under its power to regulate “drug delivery devices” in accordance with the Federal Food, Drug, and Cosmetic Act of 1938 (FDCA) (Riker et al. 2012). The FDA’s classification of e-cigarettes as “drug delivery devices” was challenged in federal courts by Sottera, Inc., an importer and distributor of e-cigarettes (Hardin 2011; Riker et al. 2012). The distributors argued that e-cigarettes are actually tobacco products because they contain nicotine and are not marketed for therapeutic purposes (Hardin 2011). A federal district court, and later the D.C. Circuit Appellate Court, agreed with the distributors and ruled that e-cigarettes, which are marketed for pleasure rather than cessation, should be classified as “tobacco products” and therefore could not be blocked by the FDA (Hardin 2011; Sottera, Inc. v. FDA 2010). The FDA proposed a new rule that would allow for the wider regulation of tobacco products to include items such as hookahs and e-cigarettes under the 2009 Family Smoking Prevention and Tobacco Control Act (TCA), and which also allows the FDA to issue regulations of these products in the interest of public health (OIRA 2013). Currently, there are no federal laws regulating the production, sale, or use of e-cigarettes.
Similar to the lack of federal e-cigarette regulation, there was very little federal regulation of tobacco products prior to the TCA, and there are still no federal policies stipulating clean air requirements in public spaces. For example, the Smoke-Free Federal Workplace Act failed to gain sufficient support in the U.S. Congress as recently as 2009. So despite the minimal federal regulation of tobacco, what forces led to such wide adoption of tobacco clean air regulations that may lend insight into the current emergence of analogous restrictions on e-cigarettes?
Political scientists have contended that in federal systems, policies may diffuse vertically downward from the national level to states, horizontally from state to state, or vertically upward from local to state (Shipan and Volden 2006). In the latter case of “bottom-up federalism,” local level changes may serve as “policy experiments” that state-level legislators look to as guides for crafting effective or popular state policy (Shipan and Volden 2006). Bottom-up diffusion often depends on the level of “professionalism” of the state legislature, as well as the strength of interest groups (Shipan and Volden 2006). Clean air tobacco bans in the U.S. spread bottom-up from localities to the state level in states containing professional legislatures and strong health lobbyists (Shipan and Volden 2006), with similar directional patterns in other federal systems such as Australia (Chapman and Wakefield 2001), Canada (Nykiforuk, Eyles, and Campbell 2008), Germany (Anger, Kvasnicka, and Siedler 2011), and India (Shimkhada and Peabody 2003) (cf. Brazil: Correa, Barreto, and Passos 2009). Other U.S. states, many of which lacked local level regulation, adopted smoking bans in response to the strong influence of regulations passed by neighboring states where local level policy had diffused upward to the state, as well as to top-down pressures from national organizations and government (Shipan and Volden 2006).
This process may lend insight into understanding the current state of e-cigarette regulation in the U.S. as, following the Sottera decision, many state and local legislatures have opted to regulate e-cigarettes rather than wait for federal regulation to guide policymaking. The emergent political discourse at the state and local level regarding e-cigarette restrictions surrounds two issues that the lack of federal policy leaves open, which are also facilitating discussions of both smoke-free and vapor-free clean air policies. First, while there is consensus on the harmful effects of secondhand smoke emanating from the federal level in the Surgeon General’s report (U.S. OSH 2006), the research on e-cigarette vapor exposure is just emerging. The lack of federal controls on the contents of e-cigarettes implies considerable inconsistency in the contents of first and secondhand vapor in public spaces (Goniewicz, Hajek, and McRobbie 2014), resulting in debate on whether or how exactly vapors affect clean air. Second, as described later, some state and local governments initially moved to enact e-cigarette policies to restrict access to minors, but clean air policies are often incorporated into these discussions. In this regard, discussions of other policies on e-cigarettes have stimulated debates of restricting vaping under clean air regulations. Other locales have attempted to apply their current tobacco clean air regulations to e-cigarettes, but even this has been met with difficulty.
The ability of state and local governments to bring electronic cigarettes under pre-existing smoking bans often turns on how existing statutes defined “smoking” (Hardin 2011). These definitions of “smoking” were almost always set prior to the existence of e-cigarettes and other tobacco products that have been introduced to the U.S. fairly recently, and their wording affects the extent to which state and local governments have been able to prohibit public vaping without major legislative revisions (Hardin 2011). Broader legislation used to ban “smoking” as an act of inhaling and exhaling a substance more generally has been successfully construed in some states, without revision, to include “vaping” because it consists of the same act (Hardin 2011). Those states whose statutes define “smoking” more narrowly as specifically the combustion or burning of tobacco have had difficulty extending existing bans to e-cigarettes, and require adding new language to their statutes in order to extend bans (Hardin 2011). New York City, for example, regulated e-cigarette use by adding language explicitly prohibiting the use of e-cigarettes in public places to their existing smoke-free air acts (NYC Council 2013). Similarly, Chicago amended the definition of tobacco products from “any substance containing tobacco leaf” to “any product…in any form, containing nicotine derived from tobacco,” and also added a specific prohibition of electronic cigarette devices (City of Chicago OCC 2014). Some states have determined that because “vaping” does not consist of inhaling smoke, which occurs as the result of burning, it is not in fact “smoking” (Hardin 2011). Many states, counties, and cities have faced obstacles in attempts to pass bans or have not attempted to pass or extend bans at all. The inconsistency in passage of vapor-free clean air and e-cigarette policies has led to a patchwork pattern of regulations. Next, we examine the temporal and geographic patterns of clean air regulation of e-cigarette use in the U.S.
4. Current policies regulating e-cigarette use
4.1. Data
The control of smoking within public spaces has been extended to e-cigarette use in recent years. In assessing the geographic distribution of e-cigarette clean air regulations, we use the regulation database from the nonprofit American Nonsmokers’ Rights Foundation, which maintains the most comprehensive collection of nationwide tobacco policies at all jurisdictional levels, including for e-cigarettes (ANRF 2014). We use this database to illustrate the emergence of such restrictions both temporally and spatially at the three levels of state, county, and municipality. The data are current as of March 2014. Given that many existing clean-air regulations were passed prior to the invention of e-cigarettes, clarifications of these policies have been a necessary step by governmental bodies. As the ANRF database tracks the date at the point of legislative clarification of these existing clean-air policies such that they subsequently apply to e-cigarettes, such clarifications to existing policies are accounted for in this analysis.
4.2. Geographic and temporal patterns of e-cigarette clean air restrictions
Jurisdictions within the U.S. are increasingly passing restrictions on e-cigarette usage in public, although of varying form and geographic coverage. Some bans restrict use of e-cigarettes in schools or municipal and/or county buildings. Others restrict use in parks and other public places. Existing smoke-free and clean air acts usually mandate that workplaces, bars, or restaurants, or some combination of the three, are smoke-free. Many e-cigarette usage bans have followed a similar structure. Those policies which ban use in all three settings are usually referred to as comprehensive bans.
Table 1 depicts the temporal emergence of e-cigarette policies as of the end of the first quarter of each year, shown both as any restriction and the subset of jurisdictions with comprehensive bans. Suffolk County, New York passed the first e-cigarette clean air ordinance (a comprehensive ban) in September 2009. By the first quarter of 2010, just one state (New Jersey), three counties, and six municipalities had passed e-cigarette clean air restrictions, covering 3.9% of the U.S. population by any ban and 3.4% with comprehensive bans. After the Sottera decision on December 7, 2010, we see an increase in the number of bans passed and percentage of Americans covered by restrictions. The number of new restrictions consistently increased from 2011 to 2013. With the addition of several large cities in the most recent time period, 2014 saw the largest year-to-year increase in the percentage of the population covered by any (from 12.2% in 2013 to 16.9% in 2014) or comprehensive (from 6.2% to 9.2%) e-cigarette clean air restrictions. This major increase in the proportion of the population covered was the result of several major cities, including New York and Los Angeles, introducing policies. Thus, an increasing proportion of the population lives in a location that restricts e-cigarette use in public in some way. At present, approximately one out of six Americans resides in locales with such policies. We next turn to the geographic distribution of current regulations.
Table 1.
Electronic Cigarette Clean Air Regulations in the U.S. by Year, Jurisdiction, and Coverage
| 2010 1st
quarter |
2011 1st
quarter |
2012 1st
quarter |
2013 1st
quarter |
2014 1st
quarter |
|
|---|---|---|---|---|---|
|
|
|||||
| New (Total) | New (Total) | New (Total) | New (Total) | New (Total) | |
|
|
|||||
| Any restriction | |||||
| Municipalities | 6 (6) | 20 (26) | 37 (63) | 57 (120) | 45 (165) |
| Counties | 3 (3) | 4 (7) | 7 (14) | 19 (33) | 7 (40) |
| States | 1 (1) | 1 (2) | 2 (4) | 3 (7) | 2 (9) |
| % Americans | 3.9% | 5.3% | 9.2% | 12.2% | 16.9% |
| covered | |||||
|
|
|||||
| Comprehensive ban | |||||
| Municipalities | 5 (5) | 15 (20) | 20 (40) | 33 (73) | 32 (105) |
| Counties | 1 (1) | 2 (3) | 2 (5) | 12 (17) | 3 (20) |
| States | 1 (1) | 0 (1) | 1 (2) | 1 (3) | 0 (3) |
| % Americans | 3.5% | 4.3% | 5.5% | 6.2% | 9.2% |
| covered | |||||
Note: For county restrictions that cover only unincorporated areas, the unincorporated population is used.
Note: States whose only statewide restrictions apply to correctional facilities are not included in the state totals.
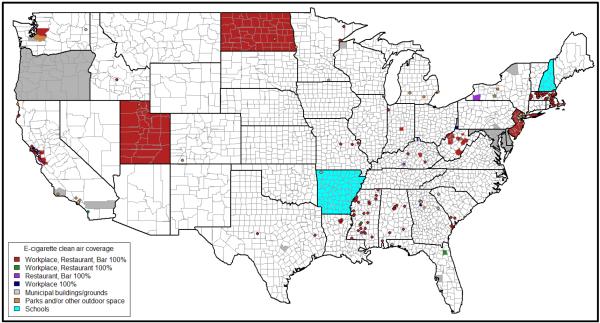
Figure 1 shows a map highlighting the current geographic coverage of restrictions on the use of e-cigarettes. In addition to workplace, bar, and/or restaurant bans, we also show jurisdictions that lack such restrictions but have banned use in municipal buildings/grounds, schools, or parks and other outdoor spaces. The results shown in Figure 1 demonstrate that e-cigarette policy is a patchwork of state and county level regulations, as well as local municipal ordinances. Huge swaths of the U.S. have no regulations. For example, the Great Plains region has many states with few policies at any level. Even within regions, some states have statewide bans, while county or local policies are the norm in other states. Thus, there is a great deal of irregularity with the geographic distribution of e-cigarette policies.
Figure 1. Geographic Coverage of Electronic Cigarette Clean Air Regulations in the U.S.
Source: American Nonsmokers’ Rights Foundation U.S. Tobacco Control Laws Restricted Use Database (current as of March 2014).
Note 1: Irregular shapes represent counties. Black-outlined circles represent a local municipality that passed a restriction at that location.
Note 2: Alaska and Hawaii are not shown. The only restriction in Alaska is a comprehensive ban in the town of Palmer. The only restriction in Hawaii is a statewide ban on e-cigarette use specifically on grounds of the State Department of Health.
Note 3: States whose only statewide restrictions apply to correctional facilities are not colored. These states are Colorado, Kansas, Oklahoma, and South Dakota.
Note 4: Restrictions superseded by higher level geographic unit restrictions are not shown. Note that some county-level restrictions only apply to unincorporated areas; therefore, local ordinances of the same category are retained in the figure for such municipalities.
As of March 2014, only New Jersey (January 2010), Utah (March 2012), and North Dakota (November 2012) have comprehensive statewide bans on e-cigarette use. These three states have restricted e-cigarette usage under their broader smoke-free air statutes which prohibit smoking in workplaces, bars, and restaurants. Both New Hampshire and Arkansas have passed statewide bans of e-cigarette use specifically in schools, while Delaware, Maryland, and Oregon have passed statewide bans on usage in municipal buildings and Hawaii restricts use specifically on the grounds of the Department of Health.
Forty counties across the U.S. enacted e-cigarette usage bans, although these vary in their coverage such that some only apply to unincorporated areas (i.e., areas with no local governmental body) or specifically target county buildings and grounds. Eleven of those counties are located in West Virginia, with all but one passing comprehensive bans. Notably, West Virginia’s county-level restrictions apply to both incorporated and unincorporated areas, such that the county law applies even to those areas with local governments. There is also a cluster of comprehensive county-level bans applying to unincorporated areas around San Francisco, while three counties in the Seattle region have also passed bans of varying coverage. Other county-level bans do not cluster, but rather appear sporadically across the country.
Municipal-level bans, indicated by circles on the map, are much more common. Within a few months of each other in late 2013 and early 2014, New York City, Chicago, and Los Angeles all passed comprehensive bans via revisions to their existing smoke-free air acts. Prior to that, the only highly populated city with a comprehensive ban was Boston (December 2011). Still, many municipalities have passed some level of regulation, totaling 165 by March 2014. This trend is quite common in Massachusetts and Mississippi, which lack state-level and (with one exception) county-level policies but feature relatively many, mostly comprehensive, municipal-level bans. While New Jersey passed the earliest statewide comprehensive ban for workplaces, restaurants, and bars, these restrictions did not apply specifically to outdoor spaces, such that some municipalities have taken this comprehensive ban one step further. Municipal bans are also common in the areas surrounding San Francisco and Los Angeles. Given that county-level restrictions in California thus far only apply to unincorporated areas, many municipalities around San Francisco have extended county-level restrictions within their incorporated borders. Other clusters of local ordinances appear around Atlanta and Birmingham, Alabama. Even with these geographic patterns, many locales remain that seemingly passed restrictions in geographic isolation.
While a new development, these patterns are reminiscent of the spread of clean air regulations for tobacco smoke. Following the pattern of “bottom-up federalism” described above, the diffusion of tobacco clean air regulations began at the local level and spread vertically to the county and state levels, rather than other more typical processes of policy enactment (Shipan and Volden 2006). In line with the diffusion of smoking bans, we might expect that e-cigarette bans will continue to primarily develop at the local level as a result of learning from other municipalities (Shipan and Volden 2008). E-cigarette bans might also be expected to continue to develop as smaller municipalities imitate larger and more influential cities that have passed bans, such as New York City, Chicago, San Francisco, and Los Angeles (Shipan and Volden 2008). Should the influence of local level bans affect the passage of state level bans, horizontal diffusion suggests an increased likelihood that neighboring governments also pass bans (Shipan and Volden 2006). This type of bottom-up federalism also appears to have some support in Germany, where cities and states are leading the way in e-cigarette use bans (Stafford 2012). Should the federal government reverse course to take a more active role and begin to pressure states, however, we might also expect top-down diffusion (Shipan and Volden 2006). As a point of comparison among federal systems, Canada has taken such a step via a de facto ban on nicotine-containing e-cigarettes; such devices must receive approval prior their sale or importation, but no company has been granted the necessary approvals for such sales or importation to date (Miller 2014). Brazil similarly has enacted a federal-level restriction (Cahn 2013). Without federal guidance in the U.S., local level politics are likely to play a lead role in determining the course of e-cigarette regulation. City councils and county-level legislative bodies continue to debate the pros and cons of e-cigarette bans. While the tobacco clean air regulations were supported by considerable scientific research, the lack of such research due to the novelty of e-cigarettes has led to controversy regarding restrictions.
5. Controversy and debate
The debate about e-cigarette usage restrictions centers on the harm reduction argument versus those who argue that vaping undermines clean air prohibitions on smoking, that it is unsafe, and that it serves as a gateway to smoking. The major problem underlying the debate is that policy is outpacing science. Research has not yet established clear effects of vaping, bystander exposure, or the long-term consequences, if any. This dearth of knowledge allows people on both sides of the argument to rely on conjecture or comparisons to tobacco smoking as fodder. The lack of data in policy debates has led, for example, to a New York City hearing that the New York Times referred to as “one of the most scientifically vague and emotionally charged health committee hearings in recent memory” (Hartocollis 2013). These arguments, as well as the lack of scientific knowledge, even manifest during considerations of whether to restrict e-cigarettes usage on a much smaller scale than the New York City hearings. As an illustrative example, we consider the city council debate in the small San Francisco area city of Benicia (Benicia City Council 2013). In deciding whether to incorporate e-cigarettes into existing city tobacco restrictions in September 2013, one council member expressed, “concern regarding proceeding with an ordinance when Council doesn’t have all the facts.” Another council member explicitly expressed concerns about minors gaining access to e-cigarettes. Then, despite her “concern regarding confusing information” on e-cigarettes, the mayor, “asked Council to err on the side of protecting the public.” The ordinance passed by a vote of 3 to 2. Thus, with recognition that scientific knowledge is not keeping pace with the perceived need for policy and without guidance at the federal or state level, jurisdictions are left to their own determinations as to whether e-cigarette restrictions are in the best interest of the public. Such lack of consistent scientific evidence has likely contributed to the geographically uneven distribution of policies, as the lack of information creates confusion among policymakers.
Those in favor of e-cigarette usage bans draw on several arguments to support their position. A heavily relied upon argument in favor of banning e-cigarette use in public is that public vaping undermines clean air laws that prohibit smoking in public and government-run places. The federal Clean Air Act was passed in 1970 and amended in 1977 and 1990 with the goal of protecting the public health from air pollutants (42 U.S.C. §7401 et seq. 1970). While this law did not include smoking bans, it raised awareness about the health risks associated with breathing in air contaminants and provided a framework by which states could regulate the air. Concerns about clean air eventually drew increased attention to the detrimental health effects of second-hand smoke exposure, fueling research during the 1970s, 1980s, and 1990s. Based on these studies, the 2006 Surgeon General’s report concluded that there were immediate adverse health effects to second-hand smoke exposure, that there is no risk-free level of exposure, and recommended policy efforts to eliminate smoking in indoor spaces in order to protect nonsmokers from exposure to second-hand smoke (U.S. OSH 2006). Yet, policy enactment occurred prior to this federal report. Restrictions on indoor smoking gained considerable momentum at the municipal level during the 1990s. During the early 2000s, several states began passing comprehensive smoking bans in the interests of protecting the public health.
Many arguments are made in favor of extending existing smoking bans to vaping. First, failing to ban e-cigarettes may undermine clean air efforts to create smoke-free environments. For example, proponents argue that because e-cigarettes are designed to look like tobacco cigarettes, enforcement of smoking bans while allowing e-cigarette use would be complicated, confusing, and challenging (Klein, Kennedy, and Berman 2014). In addition to enforcement concerns, failing to extend public smoking bans to also prohibit vaping would expose bystanders to vapors in places where they would not otherwise be exposed to smoke, such that allowing e-cigarette usage in public places might be harmful for non-users (Schober et al. 2014).
A complementary argument is that allowing vaping in public places may “re-normalize” smoking, which would reverse the efforts of public health professionals to marshal stigma in an effort to serve the broader public health (Bayer 2008; Bayer and Stuber 2006). While smoking was once considered glamorous (Brandt 1998), the denormalization of tobacco use in Western nations has led to declines in both smoking and its public acceptability (Bayer 2008). Clean air policies, such those within bars and nightclubs, have been described as intensifying the process of denormalization of smoking, especially among young people (Kelly 2009). Smoking bans and increased attention to the negative health effects of smoking and second-hand exposure have stigmatized smoking in public places. Some have argued that denormalization entails the process of marshalling stigma for the good of public health (Bayer and Bachynski 2013). Yet, others have argued that the stigma that is often coupled with denormalization may do more harm than good among disadvantaged smokers (Bell et al. 2010). Nonetheless, e-cigarette ban proponents argue that allowing vaping in public may dissipate some of the stigma associated with public smoking, thus re-normalizing the act of smoking.
The re-normalizing argument is frequently raised by proponents in regard to youth prevention efforts. Lawmakers have relied heavily on the “protection of youth” argument as a motivator for public and political support to pass bans and regulations on e-cigarettes. Many arguments about protecting youth consider young people as impressionable and highly susceptible to modeling their behavior after the things they see around them. In this line of reasoning, re-normalizing the act of smoking by allowing vaping may make youth who would otherwise be discouraged by the stigma associated with smoking more likely to try e-cigarettes and potentially tobacco cigarettes as well. As illustrated by the 2014 Golden Globes example, lawmakers have condemned celebrities for glamorizing e-cigarette use (Durbin et al. 2014; Grana, Glantz, and Ling 2011). These concerns have fueled the passage of age restrictions on the purchase of e-cigarettes, and also have been raised in the debate on public use bans.
On the other hand, many e-cigarette users argue that comprehensive bans go too far, and some public health experts have cautioned against hasty bans that fail to consider the harm reduction role of e-cigarettes (Fairchild and Colgrove 2013). Harm reduction proponents argue that vaping may be a safer alternative to smoking, and that exposure to second-hand vapors may be safer than exposure to second-hand smoke (Hajek et al. 2014). Additionally, e-cigarette usage may serve as a successful therapy for smoking cessation or at the very least reduce the number of cigarettes smoked by users (Etter 2010; Etter and Bullen 2011; Siegel, Tanwar, and Wood 2011; Hajek et al. 2014). Because of current restrictions on tobacco cigarette use, increasing costs of cigarettes due to taxation, growing stigmatization, and growing public acceptance of the negative health effects, many smokers may consider e-cigarettes as a safer, cheaper, and perhaps more accessible and usable alternative (Hajek et al. 2014).
Research suggests that many e-cigarette users do report using e-cigarettes in an attempt to quit smoking, as well as because they are “easy to use when I can’t smoke” (Zhu et al. 2013). While some report using e-cigarettes in places where tobacco smoking is banned (Dawkins et al. 2013; Foulds et al. 2011; Pepper and Brewer 2014), the extent to which avoiding smoking bans is a motivation for vaping is not firmly established (Pepper and Brewer 2014). According to a review article by Pepper and Brewer (2014), the percentage of users who describe avoiding smoking bans as a motivator for vaping varies from very small percentages (Dawkins et al. 2013; Etter 2010; Goniewicz et al. 2013; Vickerman et al. 2013) to more than 40% of respondents (Adkison et al. 2013; Dockrell et al. 2013; Foulds et al. 2011). The most recent survey data from August 2014 suggests that among e-cigarette users, “55.3% indicated using them to either cut down or quit smoking, and 38.1% reported using them in places where they could not smoke,” while 69% of users also reported using e-cigarettes at least “somewhat” to avoid smoking bans (Richardson et al. 2014:1439). In light of these findings, it may be the case that banning the public use of e-cigarettes could discourage smokers who might otherwise switch to the use of e-cigarettes in order to take advantage of fewer restrictions (Hajek et al. 2014). As a result, more people may continue smoking tobacco, which will cause serious negative health effects to themselves and people around them.
6. Public health implications
There are several public health implications of the current uncertainty regarding e-cigarette use. While a global debate is occurring as a result of treaties such as the WHO Framework Convention in Tobacco Control, implementation is not widespread and, while providing the opportunity, there has been no global consensus on e-cigarette regulation (Gartner and McNeill 2010). With little guidance from the FDA or CDC at the national level regarding e-cigarettes in the U.S., states, counties, and municipalities have been left to their own devices to decide whether and how to regulate vaping. While some entities have already acted on their own, others are likely waiting to see whether or how the FDA will regulate e-cigarettes. In the meantime, e-cigarettes go unregulated in many states, largely resulting in an inconsistent yet clustered distribution of policies across the nation. From a public health perspective, if the lack of e-cigarette clean air acts renormalizes the act of smoking, young or uninformed users may be at risk of developing nicotine addiction through the use of e-cigarettes and may potentially transition to tobacco use. Further, those who currently reside in areas with tobacco-specific clean air restrictions will experience secondhand exposure to e-cigarettes, adding toxins to the air that would otherwise not be there (Schober et al. 2014). Additionally, there is very little regulation of electronic cigarette devices and their contents, which raises questions concerning the effect of secondhand vapors that clean air acts seek to eliminate, along with product safety more generally (Cobb et al. 2010).
The health effects of vaping are largely unknown. This leaves open the possibility that users could suffer long-term negative health effects from e-cigarettes. However, preliminary research suggests that e-cigarettes may be a much safer alternative to smoking and could possibly serve as an effective smoking cessation therapy (Farsalino and Polosa 2014; Meier, Tackett, and Wagener 2013). In the absence of knowledge about the health effects of vaping, bans of use in public may be counter-productive to harm reduction efforts. As was highlighted by Fairchild and Colgrove (2013), “If e-cigarettes can reduce, even slightly, the blight of six million tobacco-related deaths a year, trying to force them out of sight is counterproductive.” And do we risk undermining an opportunity to save lives for the sake of dogmatic adherence to a tobacco “endgame” (Fairchild, Bayer, and Colgrove 2014)? There are many questions left open regarding vaping and e-cigarettes. What is certain is that it is imperative to implement research programs on the health effects, parameters of addiction, and patterns of use of e-cigarettes. Currently, policy decisions regarding e-cigarettes are often made relying on arguments about discouraging the smoking of tobacco products. This has resulted in an inconsistent approach to policies restricting use in various spaces across the U.S. With the novelty of e-cigarette clean air restrictions, studies have not yet considered whether the presence of policies affect youth and adult use, or whether restrictions inhibit use of e-cigarettes as a tool in smoking cessation. Future research must continue to consider the role that e-cigarettes may or may not play in reducing smoking and protecting the health of the public. In particular, by restricting e-cigarette use, do municipalities discourage smoking cessation as a result of inhibiting the use of a potential harm reduction tool in public spaces? Additionally, there is a need for more detailed analyses of how the social and political characteristics of places affect the adoption of e-cigarette regulations at various governmental levels.
Acknowledgments
The authors would like to thank the staff at the American Nonsmokers’ Rights Foundation, particularly Maggie Hopkins and Laura Walpert. The findings and conclusions herein are those of the authors and do not necessarily represent the official position of the American Nonsmokers’ Rights Foundation. We also thank Jake Brosius and Emily Ekl for research assistance.
Funding source: This work was supported by the National Institute on Drug Abuse (grant R03 DA034933). The sponsor had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The findings and conclusions herein are those of the authors and do not necessarily represent the official position of the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors have no conflict of interest to report.
Cases Cited
42 U.S.C. §7401 et seq. (1970).
Sottera, Inc. v. Food and Drug Administration, 627 F.3d 891 (D.C. Cir. 2010).
References
- Adkison SE, O’Connor RJ, Bansal-Travers M, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44(3):207–215. doi: 10.1016/j.amepre.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anger S, Kvascika M, Siedler T. One last puff? Public smoking bans and smoking behavior. J Health Econ. 2011;30(3):591–601. doi: 10.1016/j.jhealeco.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults - United States, 2012-2013. MMWR Morb Mortal Wkly Rep. 2014 Jun 27;63(25):542–547. [PMC free article] [PubMed] [Google Scholar]
- American Nonsmokers’ Rights Foundation . U.S. tobacco control laws database (restricted use version) American Nonsmokers’ Rights Foundation; Berkeley, CA: 2014. [Google Scholar]
- Bayer R. Stigma and the ethics of public health: Not can we but should we. Soc Sci Med. 2008;67(3):463–472. doi: 10.1016/j.socscimed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Bayer R, Bachynski KE. Banning smoking in parks and on beaches: Science, policy, and the politics of denormalization. Health Affairs. 2013;32(7):1291–1298. doi: 10.1377/hlthaff.2012.1022. [DOI] [PubMed] [Google Scholar]
- Bayer R, Stuber J. Tobacco control, stigma, and public health: Rethinking the relations. Am J Public Health. 2006;96(1):47–50. doi: 10.2105/AJPH.2005.071886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell K, Salmon A, Bowers M, Bell J, McCullough L. Smoking, stigma, and tobacco ‘denormalization’. Soc Sci Med. 2010;70(6):795–799. doi: 10.1016/j.socscimed.2009.09.060. [DOI] [PubMed] [Google Scholar]
- Benicia City Council City council minutes. The City of Benicia, CA. http://www.ci.benicia.ca.us/vertical/sites/%7B3436CBED-6A58-4FEF-BFDF-5F9331215932%7D/uploads/MINI091713.pdf. Published September 17, 2013. Accessed April 8, 2014.
- Brandt AM. Blow some my way: Passive smoking, risk, and American Culture. In: Lock S, Reynolds L, Tansey EM, editors. Ashes to Ashes: The History of Smoking and Health. Amsterdam, Rodopi: 1998. pp. 164–187. [PubMed] [Google Scholar]
- Cahn Z. France acts on electronic cigarettes. J Public Health Pol. 2013;34(4):560–564. doi: 10.1057/jphp.2013.32. [DOI] [PubMed] [Google Scholar]
- Camenga DR, Delmerico J, Kong G, et al. Trends in use of electronic nicotine delivery systems by adolescents. Addict Behav. 2014;39(1):338–340. doi: 10.1016/j.addbeh.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (a) About one in five U.S. adult cigarette smokers have tried an electronic cigarette. CDC Newsroom. http://www.cdc.gov/media/releases/2013/p0228_electronic_cigarettes.html. Published February 28, 2013. Accessed March 12, 2014.
- Centers for Disease Control and Prevention (b) E-cigarette use more than doubles among U.S. middle and high school students from 2011-2012. CDC Newsroom. http://www.cdc.gov/media/releases/2013/p0905-ecigarette-use.html. Published September 5, 2013. Accessed March 12, 2014.
- Centers for Disease Control and Prevention Adult cigarette smoking in the United States: current estimate. CDC Fact Sheets: Smoking and Tobacco Use. http://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/. Published February 14, 2014. Accessed March 31, 2014.
- Champan S, Wakefield M. Tobacco control advocacy in Australia: reflections on 30 years of progress. Health Educ Behav. 2001;28(3):274–289. doi: 10.1177/109019810102800303. [DOI] [PubMed] [Google Scholar]
- City of Chicago Office of the City Clerk Clean Indoor Air Ordinance. File No. SO2013-61610, Version 1. https://chicago.legistar.com/LegislationDetail.aspx?ID=1531471andGUID=8FBB15D9-D5CF-4211-8396-78EF37BA8F87andOptions=AdvancedandSearch. Published 2014. Accessed September 2, 2014.
- Cobb NK, Byron MJ, Abrams DB, Shields PG. Novel nicotine delivery systems and public health: The rise of the “e-cigarette”. Am J Public Health. 2010;100(12):2340–2342. doi: 10.2105/AJPH.2010.199281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correa PCRP, Barreto SM, Passos VMA. Smoking-attributable mortality and years of potential life lost in 16 Brazilian capitals, 2003: a prevalence-based study. BMC Public Health. 2009;9:206. doi: 10.1186/1471-2458-9-206. doi:10.1186/1471-2458-9-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawkins L, Turner J, Roberts A, et al. ‘Vaping’ profiles and preferences: an online survey of electronic cigarette users. Addiction. 2013;108:1115–1125. doi: 10.1111/add.12150. [DOI] [PubMed] [Google Scholar]
- Dockrell M, Morison R, Bauld L, et al. E-cigarettes: prevalence and attitudes in Great Britain. Nicotine Tob Res. 2013;15:1737–1744. doi: 10.1093/ntr/ntt057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin D, Blumenthal R, Brown S, Markey E. Senators: Golden Globes should celebrate achievements in film and television, not smoking and e-cigarettes. Dick Durbin US Senator for Illinois Assistant Majority Leader. http://www.durbin.senate.gov/public/index.cfm/pressreleases?ID=84d385e1-79c9-4c99-8fb0-6e1d163f283b. Published January 14, 2014. Accessed March 31, 2014.
- Etter J. Electronic cigarettes: a survey of users. BMC Public Health. 2010;10:231. doi: 10.1186/1471-2458-10-231. doi:10.1186/1471-2458-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter J, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106(11):2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- Etter J. Bullen C. A longitudinal study of electronic cigarette users. Addict Behav. 2014;39(2):491–494. doi: 10.1016/j.addbeh.2013.10.028. [DOI] [PubMed] [Google Scholar]
- Fairchild AL, Colgrove J. The case for tolerating e-cigarettes. The New York Times. 2013 Dec 8; http://www.nytimes.com/2013/12/09/opinion/the-case-for-tolerating-e-cigarettes.html. Accessed March 31, 2014.
- Fairchild AM, Bayer R, Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco “endgame.”. N Engl J Med. 2014;370:293–29. doi: 10.1056/NEJMp1313940. [DOI] [PubMed] [Google Scholar]
- Farsalinos K, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Ther Adv Drug Saf. 2014;5(2):67–86. doi: 10.1177/2042098614524430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foulds J, Veldheer S, Berg A. Electronic cigarettes (e-cigs): view of aficionados and clinical/public health perspectives. Int J Clin Pract. 2011;65:1037–1042. doi: 10.1111/j.1742-1241.2011.02751.x. [DOI] [PubMed] [Google Scholar]
- Gartner C, McNeill A. Options for global tobacco control beyond the Framework Convention in Tobacco Control. Addiction. 2010;105(1):1–3. doi: 10.1111/j.1360-0443.2009.02720.x. [DOI] [PubMed] [Google Scholar]
- Git A. Golden Globes’ sexy portray of e-cigarettes makes lawmakers smolder. CBSNews.com. http://www.cbsnews.com/news/golden-globes-sexy-portrayal-of-e-cigarettes-makes-lawmakers-smolder/. Published January 16, 2014. Accessed March 11, 2014.
- Goniewicz ML, Lingas EO, Hajek P. Patterns of electronic cigarette use and user beliefs about their safety and benefits: in Internet survey. Drug Alcohol Rev. 2013;32:133–140. doi: 10.1111/j.1465-3362.2012.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz ML, Hajek P, McRobbie H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addiction. 2014;109(3):500–507. doi: 10.1111/add.12410. [DOI] [PubMed] [Google Scholar]
- Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23:133–139. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana RA, Glantz SA, Ling PM. Electronic nicotine delivery systems in the hands of Hollywood. Tob Control. 2011;20(6):425–426. doi: 10.1136/tc.2011.043778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek P, Etter J, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014 doi: 10.1111/add.12659. Early view. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardin DF. Blowing electronic smoke: electronic cigarettes, regulation, and protecting the public health. U Ill JL Tech and Pol’y. 2011:433–462. Fall. [Google Scholar]
- Hartocollis A. Vapors and emotions rise at hearing on E-cigarettes. The New York Times. 2013 Dec 4; http://www.nytimes.com/2013/12/05/nyregion/vapors-and-emotions-rise-at-hearing-on-e-cigarettes.html?ref=todayspaperand_r=0. Accessed March 31, 2014.
- Kelly BC. Smoke-Free Air Policy: Subcultural Shifts and Secondary Health Effects among NYC Club-Going Youth. Sociol Health Illn. 2009;31(4):569–582. doi: 10.1111/j.1467-9566.2008.01150.x. [DOI] [PubMed] [Google Scholar]
- King B, Alam S, Promoff G, Arrazola R, Dube S. Awareness and ever-use of electronic cigarettes among U.S. adults, 2010-2011. Nicotine Tob Res. 2013;15(9):1623–1627. doi: 10.1093/ntr/ntt013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein EG, Kennedy RD, Berman M. Tobacco control policies in outdoor areas of high volume American transit systems. J Commun Health. 2014;39:660–667. doi: 10.1007/s10900-014-9873-3. [DOI] [PubMed] [Google Scholar]
- McAuley TR, Hopke PK, Zhao J, Babaian S. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxical. 2012;24(12):850–857. doi: 10.3109/08958378.2012.724728. [DOI] [PubMed] [Google Scholar]
- Meier E, Tackett AP, Wagener TL. Effectiveness of electronic aids for smoking cessation. Curr Cardiovasc Risk Rep. 2013;7(6):464–472. doi: 10.1007/s12170-013-0343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A. E-cigarette debate divides regulators and consumers. CMAJ. 2014;186:E169–E170. doi: 10.1503/cmaj.109-4705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PAP. Notes on Continuous Stochastic Phenomena. Biometrika. 1950;37:17–23. [PubMed] [Google Scholar]
- New York City Council Int. 1210-2013,A. Legislative Research Center. http://legistar.council.nyc.gov/LegislationDetail.aspx?ID=1526765andGUID=15D04C6D-C760-40EA-88A4-2E40C0374E43andOptions=andSearch=. Published December 30, 2013. Accessed March 31, 2014.
- Nykiforuk CIJ, Eyles J, Campbell HS. Smoke-free spaces over time: a policy diffusion study of bylaw development in Alberta and Ontario, Canada. Health Soc Care Comm. 2008;16(1):64–74. doi: 10.1111/j.1365-2524.2007.00727.x. [DOI] [PubMed] [Google Scholar]
- Office of Information and Regulatory Affairs View rule 0910-AG38. Reginfo.gov. http://www.reginfo.gov/public/do/eAgendaViewRule?pubId=201310andRIN=0910-AG38. Published Fall 2013. Accessed March 12, 2014.
- Pearson J, Richardson A, Niaura R, Vallone D, Abrams D. E-cigarette awareness, use, and harm perceptions in U.S. adults. Am J Public Health. 2012;102(9):1758–1766. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper JK, Brewer NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review. Tob Control. 2014;23(5):375–384. doi: 10.1136/tobaccocontrol-2013-051122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper JK, Reiter PL, McRee A, Cameron LD, Gilkey MB, Brewer NT. Adolescent males’ awareness of and willingness to try electronic cigarettes. J Adolesc Health. 2013;52(2):144–150. doi: 10.1016/j.jadohealth.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Little M, Kawamoto CT, Herzog TA. Smokers who try e-cigarettes to quit smoking: Findings from a multiethnic study in Hawaii. Am J Public Health. 2013;103(9):e57–e62. doi: 10.2105/AJPH.2013.301453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson A, Pearson J, Xiao H, Stalgaitis C, Vallone D. Prevalence, harm perceptions, and reasons for using noncombustible tobacco products among current and former smokers. Am J Public Health. 2014;104(8):1437–1444. doi: 10.2105/AJPH.2013.301804. doi: 10.2105/AJPH.2013.301804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riker C, Lee K, Darville A, Hahn E. E-cigarettes: promise or peril? Nurs Clin North Am. 2012;47:159–171. doi: 10.1016/j.cnur.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Schober W, Szendrei K, Matzen W, Osiander-Fuchs H, Heitmann D, Schettgen T, Jorres RA, Fromme H. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(1):628–37. doi: 10.1016/j.ijheh.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Schripp T, Markewitz D, Uhde E, Salthammer T. Does e-cigarette consumption cause passive vaping? Indoor Air. 2012;23(1):25–31. doi: 10.1111/j.1600-0668.2012.00792.x. [DOI] [PubMed] [Google Scholar]
- Shimkhada R, Peabody JW. Tobacco control in India. B World Health Organ. 2003;81:48–52. [PMC free article] [PubMed] [Google Scholar]
- Shipan CR, Volden C. Bottom-up federalism: the diffusion of antismoking policies from U.S. cities to states. Am J Polit Sci. 2006;50:825–843. [Google Scholar]
- Shipan CR, Volden C. The mechanisms of policy diffusion. Am J Polit Sci. 2008;52(4):840–857. [Google Scholar]
- Siegel MB, Tanwar KL, Wood KS. Electronic cigarettes as a smoking cessation tool: results from an online survey. Am J Prev Med. 2011;40(4):472–475. doi: 10.1016/j.amepre.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Stafford N. Hanover bans e-cigarette use in civic offices amid calls for better safety data. BMJ. 2012;344:e3. doi: 10.1136/bmj.e3. 2012. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau . 2010 Census Gazetteer Files. U.S. Census Bureau; Washington, DC: https://www.census.gov/geo/maps-data/data/gazetteer2010.html. Published 2010. Accessed September 2, 2014. [Google Scholar]
- United States Office on Smoking and Health The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Centers for Disease Control and Prevention. http://www.ncbi.nlm.nih.gov/books/NBK44328/. Published 2006. Accessed March 31, 2014. [PubMed]
- Vickerman KA, Carpenter KM, Altman T, et al. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15:1787–1791. doi: 10.1093/ntr/ntt061. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The use and perception of electronic cigarettes and snus among the U.S. population. PLoS One. 2013;8(10):e79332. doi: 10.1371/journal.pone.0079332. doi: 10.1371/journal.pone.0079332. [DOI] [PMC free article] [PubMed] [Google Scholar]