Abstract
It is hypothesized that persons who use drugs (PWUD) in Vietnam who are also HIV-positive may face additional challenges in psychosocial outcomes, and these challenges may extend to their family members. In this study, we examined depressive symptoms, stigma, social support, and caregiver burden of HIV-positive PWUD and their family members, compared to the outcomes of HIV-negative PWUD and their family members. Baseline, 3-month, and 6-month assessment data were gathered from 83 PWUD and 83 family members recruited from four communes in Phú Tho Province, Vietnam. For PWUD, although we observed a general decline in overall stigma over time for both groups, HIV-positive PWUD consistently reported significantly higher overall stigma for all three periods. Depressive symptoms among family members in both groups declined over time; however, family members of HIV-positive PWUD reported higher depressive symptoms across all three periods. In addition, family members of HIV-positive PWUD reported lower levels of tangible support across all three periods. Caregiver burden among family members of HIV-positive PWUD increased significantly over time, whereas the reported burden among family members of HIV-negative PWUD remained relatively unchanged. The findings highlight the need for future interventions for PWUD and family members, with targeted and culturally specific strategies to focus on the importance of addressing additional stigma experienced by PWUD who are HIV-positive. Such challenges may have direct negative impact on their family members’ depressive symptoms, tangible support and caregiver burden.
Keywords: Persons who use drugs, family members, HIV-positive drug users, Vietnam
INTRODUCTION
The HIV epidemic in Vietnam has been concentrated primarily in persons who use drugs (PWUD) who account for 65% of reported HIV infections, at least 90% of whom are men (Hammett et al., 2012; FHI, 2010; VAAC, 2009). The experience of PWUD in Vietnam reflects the battery of factors of stereotyping and discrimination that may lead to stigmatization (Link & Phelan, 2001). With “pre-existing” stigma, PWUD are likely to experience a higher degree of HIV stigma (Mahajan et al., 2009). Given these convergence of negative factors, it is hypothesized that HIV-positive PWUD may face additional challenges with stigma and discrimination (Kermode el al., 2008; Ogden & Nyblade, 2005).
In Vietnam, as in many Asian cultures, the family is considered a critical extension of one’s self (Salter et al., 2010). Given that the family plays an important role supporting PWUD around treatment adherence (Li et al, 2013), the impact of HIV on PWUD may extend to their family members. Although past studies have focused on stigma and discrimination (Li et al., 2013; Gaudine et al., 2009; Hong et al., 2004; Nyblade et al., 2008; Pharris et al., 2011), few data are available on the mental and social impact of HIV on PWUD and their family members in Vietnam. This study aimed to compare the outcomes of HIV-positive PWUD with those of HIV-negative PWUD and their family members.
METHODS
Study Design and Participants
This study uses data from an intervention pilot conducted in Vietnam, described in detail by Li and colleagues (Li et al., 2013), conducted between August 2011 and February 2012 in Phú Thọ Province in northern Vietnam. The four selected communes in Phú Tho were matched into two pairs based on geographic area and number of PWUD. After the baseline assessment, the two communes in each pair were randomized to either an intervention or a standard care condition. The study was approved by the Institutional Review Boards (IRB) of the University of California, Los Angeles, and the Vietnam National Institute of Hygiene and Epidemiology.
In Vietnam, service providers in the commune health center (CHC) provide curative and preventive health services to PWUD in the community (World Health Organization 2010). The CHC providers introduced the project through verbal explanation and a printed flyer to PWUD, who were then referred to a study recruiter, who screened PWUD individually for eligibility. The inclusion criteria were: 1) age 18 or above, 2) a history of drug use, 3) residence in the participating commune, and 4) willingness to invite a family member to participate in the study. Upon enrolling PWUD and with their consent, family members were recruited. The inclusion criteria for family member participants were: 1) age 18 or over, 2) immediate or extended family member and living with the PWUD, and 3) previous knowledge of the drug use status of the PWUD. Written informed consent was obtained for PWUD and family members. All participants were assessed at baseline, 3- and 6-months.
Measures
Depressive symptoms were measured by using a short version of the Zung Self-Rating Depression Scale (Zung 1965). This 9-item instrument was adapted from the original 20-item questionnaire and was successfully used in China (Li et al. 2011). A higher overall score indicated a higher depressive symptoms (Cronbach’s α=0.84 for PWUD and 0.75 for family members).
Tangible support was assessed based on the four-item subscale in the Medical Outcomes Study Social Support Scale (Sherbourne and Stewart 1991), a higher score indicating higher tangible social support (Cronbach’s α=.94 for PWUD and 0.94 for family members).
Overall stigma perceived by PWUD was assessed using a seventeen-item subscale adapted from Herek and Capitanio (1993). The subscale has been validated in an Asian population in previous studies (Li, Lee, Thammawijaya, Jiraphongsa, & Rotheram-Borus, 2009), a higher score implying a higher degree of overall stigma (Cronbach’s α = 0.80).
Drug use by PWUD was determined using the Addiction Severity Index (ASI), a widely used instrument to quantify addictive behavior (McLellan et al., 1992). PWUD reported their frequency and severity of using illicit substances in the previous 30 days. A drug composite score was constructed, with a higher score indicating more severe drug using problems (McGahan, Griffith, Parente, & McLellan, 1986).
Caregiver burden perceived by family members was assessed using the Perceived Caregiver Burden Scale (Stommel, Given, & Given, 1990), which has been used in our previous studies (Lee, Li, Jiraphongsa, & Rotheram-Borus, 2010). This 17-item scale assessed family members’ perception of having a drug-using relative and its impact on health, finances, and feelings of entrapment. A higher score reflected a higher level of burden (Cronbach’s α = 0.82).
We also collected background information, including gender, age, and education, duration of drug use and HIV status.
Data Analysis
Baseline differences by HIV status of PWUD were analyzed using t tests. Plots of means over time were generated to graphically examine the outcomes over time. We estimated mixed-effect models to fit outcomes with the HIV status of PWUD as the main effect, visit (baseline, 3-, or 6-month follow-up), and HIV status-by-visit interaction. The models also included commune-level random effects to account for dependence within communes and a first-order autoregressive covariance structure to account for repeated observations within each participant. We present estimated difference in outcome measures at baseline, 3-month, and 6-month follow-up between HIV-negative and HIV-positive PWUD through model contrasts. The results from F-tests for the main effects (group and visit effects) and the interaction term were reported. Statistical analyses were conducted using SAS for Windows (Version 9.2).
RESULTS
Table 1 describes participants’ baseline characteristics. Of 83 PWUD in the study, 16 (19.3%) were HIV-positive. Age of PWUD ranged from 18 to 49 years (mean age=33.7; Standard deviation [SD] = 6.8S). Family members’ age ranged from 19 to 76 (mean=43.6; SD=16.0). All PWUD in our study were men. The majority of the family members in the study was female caregivers (n=75; 84%). For PWUD, there were no significant differences by HIV status for the mean scores of overall stigma, depressive symptoms, tangible support, and drug use at baseline. Similarly, we found no significant differences for family members’ depressive symptoms and caregiver burden.
Table 1.
Baseline sample characteristics of injection drug users (PWUD) and family members by HIV status of PWUD (n=83).
| HIV status of PWUD | |||
|---|---|---|---|
|
| |||
| Parameter | Positive (n=16) | Negative (n=67) | p-valuea |
| Age (Mean ± SD) | |||
| PWUD | 32.5 ± 4.35 | 33.9 ± 7.30 | 0.4519 |
| FM | 52.63 ± 16.06 | 41.38 ± 15.31 | 0.0107 |
| Male (%) | |||
| PWUD | 16 (100) | 66 (100) | – |
| FM | 0 (0) | 8 (11.9) | 0.3436b |
| Years of education (Mean ± SD) | |||
| PWUD | 11.25 ± 2.79 | 10.63 ± 2.28 | 0.3505 |
| FM | 8.94 ± 4.07 | 10.28 ± 4.12 | 0.2427 |
| PWUD’ overall stigma (Mean ± SD) | 63.00 ± 3.88 | 59.34 ± 7.16 | 0.0525 |
| Depressive symptoms (Mean ± SD) | |||
| PWUD | 17.13 ± 4.06 | 17.54 ± 5.61 | 0.7827 |
| FM | 19.75 ± 5.76 | 18.09 ± 4.71 | 0.2287 |
| Tangible support (Mean ± SD) | |||
| PWUD | 15.56 ± 2.37 | 14.87 ± 3.81 | 0.4866 |
| FM | 13.63 ± 2.90 | 15.70 ± 3.73 | 0.0408 |
| Drug use (Mean ± SD) | 0.11 ± 0.07 | 0.15 ± 0.07 | 0.1067 |
| Family member caregiver burden (Mean ± SD) | 50.88 ± 10.84 | 53.88 ± 7.95 | 0.2105 |
Independent sample t-test;
Fisher’s Exact test
Table 2 outlines the results from mixed-effects regression models on overall stigma, depressive symptoms, tangible support, and caregiver burden, with Figure 1 showing the plots of least squares means. For PWUD, we observed a general decline in overall stigma over time for both groups; however, HIV-positive PWUD consistently reported higher stigma for all three periods (p=0.0008). Differences were statistically significant at baseline (Parameter estimate = 4.27; p=0.012), 3-month follow-up (Parameter estimate = 4.37; p=0.010), and at 6-month follow-up (Parameter estimate = 4.51; p=0.008). For family members, depressive symptoms declined significantly over time for both groups (p<0.0001); however, family members of HIV-positive PWUD reported higher depressive symptoms across all three time periods, the difference being statistically significant at 3-month follow-up (Parameter estimate =2.35; p=0.040). We observed a general increase in tangible support for both groups (p<0.0001); however, family members of HIV-positive PWUD consistently reported lower levels of tangible social support, differences being statistically significant at baseline (Parameter estimate = −1.91; p=0.006) and at 3-month follow-up (Parameter estimate= −1.67; p=0.016). Family members of HIV-negative PWUD reported relatively constant levels of caregiver burden. On the contrary, family members of HIV-positive PWUD reported an increase in burden over time, and this increase in caregiver burden was significant at 6-month follow-up, indicated by significant HIV status-by-visit interaction (p=0.0387).
Table 2.
Results from mixed-effects regression models for PWUD and family members (n=83)a
| Overall stigma (PWUD) | Depressive symptoms (Family members) | Tangible support (Family member) | Caregiver burden (Family members) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Parameter | Est. | P | Est. | P | Est. | P | Est. | P |
| Main effectb | ||||||||
| PWUD’ HIV-status | 0.0008 | 0.0549 | 0.0086 | 0.9311 | ||||
| Visit | 0.1203 | <0.0001 | <0.0001 | 0.1065 | ||||
| Interactionb | ||||||||
| Visit × PWUD’ | ||||||||
| HIV-status | 0.9925 | 0.6730 | 0.1643 | 0.0387 | ||||
| Comparisonsc | ||||||||
| Baseline | 4.2744 | 0.0120 | 1.3913 | 0.2211 | −1.9089 | 0.0062 | −3.0056 | 0.1984 |
| 3-months | 4.3677 | 0.0103 | 2.3512 | 0.0395 | −1.6709 | 0.0163 | 0.0401 | 0.9863 |
| 6-months | 4.5066 | 0.0082 | 1.6945 | 0.16366 | −0.4759 | 0.4901 | 2.5345 | 0.2777 |
Outcomes adjusted for participants’ age, gender, and educational status
P value from F-test. The significances of the main effects were not of interest.
Estimated difference in outcome measures at baseline, 3-month and 6-month follow-up between HIV-positive and HIV-negative PWUD (for PWUD and family members of PWUD) through model contrasts.
Figure 1.
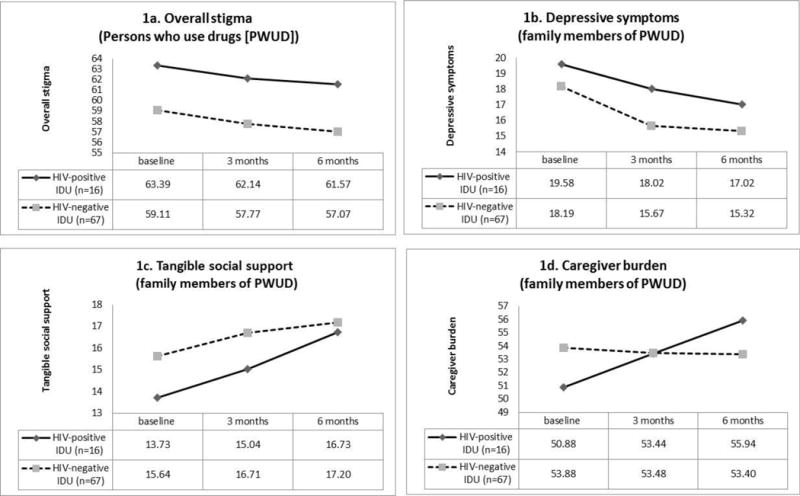
Overall stigma, depressive symptoms, tangible social support, and caregiver burden by HIV status of PWUD
DISCUSSION
Stigma, lack of tangible support, depressive symptoms, and caregiver burden are some of the challenges facing PWUD and family members. Such challenges may be amplified if PWUD are also HIV-positive. A study by Li and colleagues demonstrated that PWUD and family members face multiple challenges (Li et al., 2013). This study makes additional contribution by examining potential differences among HIV-positive and HIV-negative PWUD and their family members. Our study findings confirm our hypothesis that the level of overall stigma experienced by HIV-positive PWUD is more substantial, which in turn may impact their family members’ mental and social outcomes. Our findings confirm our hypothesis that HIV-positive PWUD may face layered stigma, where HIV stigma is “layered on top of pre-existing stigma associated with drug use” (Nyblade, 2006), and the additional challenges of layered stigma may extend to family members.
As in many studies, some limitations should be noted, including a relative small sample size, generalizability to other geographic areas, self-reported data, and other “layers” of stigma not captured in the study. Despite these limitations, our findings underscore the importance of addressing additional challenges for HIV-positive PWUD. Understanding the potential connection between the experience of layered stigma by PWUD and its impact on their family members is critical for guiding future HIV prevention programs and policies that effectively address stigma. Our findings underscore the need for future interventions to consider the impact of HIV to design targeted, culturally specific, and tailored strategies to focus on the differences in challenges for PWUD and family members.
Acknowledgments
This study was funded by National Institute on Drug Abuse (NIDA/NIH) grant number R34DA029493. Dr. Lee’s time for this manuscript was supported by the National Institute of Mental Health (NIMH 5K01MH085503). The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH. We would like to thank the project team members in Hanoi and Phú Thọ, Vietnam, for their contributions to this study.
Footnotes
Clinical Trial Registration: NCT01540188
References
- Family Health International, National Institute for Hygiene and Epidemiology (FHI) Results from the HIV/STI Integrated Biological and Behavioral Surveillance (IBBS) in Vietnam, 2009. Hanoi: Family Health International; 2010. [Google Scholar]
- Hammett TM, Kling R, Van NTH, Son DH, Binh KT, Oanh KTH. HIV prevention interventions for female sexual partners of injection drug users in Hanoi, Vietnam: 24-month evaluation results. AIDS Behav. 2012;16(5):1164–1172. doi: 10.1007/s10461-011-0062-4. [DOI] [PubMed] [Google Scholar]
- Gaudine A, Gien L, Thuan TT, Dung DV. Perspectives of HIV-related stigma in a community in Vietnam: a qualitative study. Int J Nurs Stud. 2010;47(1):38–48. doi: 10.1016/j.ijnurstu.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Herek GM, Capitanio JP. Public reactions to AIDS in the United States: A second date of stigma. American Journal of Public Health. 1993;83:574–577. doi: 10.2105/ajph.83.4.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong KT, Anh NTV, Ogden J. Understanding HIV/AIDS related stigma and discrimination in Vietnam. Washington DC: International Center for Research on Women; 2004. [Google Scholar]
- Kermode M, Devine A, Chandra P, Dzuvichu B, Gilbert T, Herrman H. Some peace of mind: Assessing a pilot intervention to promote mental health among widows of injecting drug users in north-east India. BMC Public Health. 2008;22(8):294. doi: 10.1186/1471-2458-8-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Li L, Jiraphongsa C, Rotheram-Borus MJ. Caregiver burden of family members of persons living with HIV in Thailand. International Journal of Nursing Practice. 2010;16:57–63. doi: 10.1111/j.1440-172X.2009.01812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Lee SJ, Thammawijaya P, Rotheram-Borus MJ. Stigma, Social Support, and Depression among People Living with HIV in Thailand. AIDS Care. 2009;21(8):1007–1013. doi: 10.1080/09540120802614358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Liang LJ, Ding YY, Ji GP. Facing HIV as a family: predicting depressive symptoms with correlated responses. Journal of Family Psychology. 2011;25:202–209. doi: 10.1037/a0022755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Nguyen AT, Liang LJ, Lin C, Farmer S, Flore M. Mental Health and Family Relations among People Who Inject Drugs and Their Family Members in Vietnam. International Journal of Drug Policy. 2013;24(6):545–549. doi: 10.1016/j.drugpo.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Ortiz DJ, Szekeres G, Coates JJ. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGahan PL, Griffith JA, Parente R, McLellan AT. Addiction Severity Index Composite Scores Manual. Philadelphia, PA: Department of Veterans Affairs Medical Center; 1986. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Ogden J, Nyblade L. Common at its core: HIV-related stigma across contexts. Washington, DC: International Center on Research for Women; 2005. [Google Scholar]
- Nyblade LC. Measuring HIV stigma: Existing knowledge and gaps. Psychology Health and Medicine. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Nyblade L, Hong KT, Anh NV, Ogden J, Jai A, Stangl A, et al. Communities Confront HIV Stigma in Vietnam: Participatory Intervention Reduce HIV-Related Stigma in Two Provinces. Washington DC: Hanoi, Vietnam, Interventional Center for Research on Women (ICRW); Institute for Social Development Studies (ISDS); 2008. [Google Scholar]
- Pharris A, Hoa NP, Tishelman C, Marrone G, Chuc NT, Brugha R, et al. Community patterns of stigma towards persons living with HIV: A population-based latent class analysis from rural Vietnam. BMC Public Health. 2011;11:705. doi: 10.1186/1471-2458-11-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salter ML, Go VF, Minh NL, Gregowski A, Ha TV, Rudolph A, et al. Influence of perceived secondary stigma and family on the response to HIV infection among injection drug users in Vietnam. AIDS Education and Prevention. 2010;22:558–570. doi: 10.1521/aeap.2010.22.6.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Stommel M, Given CW, Given B. Depression as an overriding variable explaining caregiver burdens. Journal of Aging and Health. 1990;2(1):81–102. [Google Scholar]
- Vietnam Administration for HIV/AIDS Control (Ministry of Health) (VAAC), Family Health International. 2007 HIV/AIDS estimates and projections. Hanoi: VAAC; 2009. 2009. [Google Scholar]
- World Health Organization. Good practice in Asia: Targeted HIV prevention for injecting drug users and sex workers. 2010 Retrieved March 1, 2014, from www.who.int/hiv/pub/idu/good_practice_aisa_idu.pdf.
- Zung WW. A Self-rating Depression Scale. Archives of General Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]


