Abstract
The HIV epidemic in Peru is concentrated among men who have sex with men (MSM). Given that MSM have been documented as early adopters of emerging technology, we examined communication technology access and utilization, and mobile health (mHealth) acceptance among Peruvian MSM and transgender women (TGW) in order to gauge opportunities for mHealth-enabled HIV interventions. A convenience sample of 359 HIV-infected MSM and TGW recruited from three sites in Lima, Peru completed standardized assessments of alcohol use disorders (AUDs), risky sexual behavior, and antiretroviral therapy (ART) adherence along with self-constructed measures of communication technology access and utilization, and mHealth acceptance. Most (86%) participants had daily access to any cell phone, including smartphones (30%). The most frequent communication activities were receiving and making calls, and receiving and sending text messages using cell phones. On a 5-point Likert scale, participants expressed interest in using mHealth for medication reminders (M=3.21, SD=1.32) and engaging in anonymous online interactions with health professionals to discuss HIV-related issues (M=3.56, SD=1.33). Importantly, no significant differences were found in communication technology use and mHealth acceptance among participants with AUDs, depression and suboptimal ART adherence, all of which are associated with poor HIV treatment outcomes. Findings show support for implementing mHealth-based intervention strategies using cell phones to assess and reduce HIV-risk behaviors among HIV-infected MSM and TGW.
Keywords: mHealth, communication technology, men who have sex with men (MSM), HIV, Peru
Introduction
In South America, the HIV epidemic is concentrated among men who have sex with men (MSM) (Baral, Sifakis, Cleghorn, & Beyrer, 2007; Beyrer et al., 2012). This is especially true in Peru, where HIV prevalence among MSM ranges between 10–22% (Sanchez et al., 2007) compared to only 0.2% in the general population (Carcamo et al., 2012) and 0.5–2.2% among female sex workers (Alarcon et al., 2012; Carcamo et al., 2012). The prevalence of alcohol use disorders (AUDs) is also extremely high among Peruvian MSM (Ludford et al., 2013). AUDs are associated with multiple high-risk sexual behaviors such as having unprotected sex, having multiple sexual partners and being a sex worker (Deiss et al., 2013; Ludford et al., 2013; Segura et al., 2008); and with suboptimal adherence to antiretroviral therapy (ART) (Ferro et al., 2013). Maintaining optimal ART adherence is crucial for achieving viral suppression and reducing sexual transmission of HIV. For Peruvian MSM, the combination of AUDs, risky sexual behavior and suboptimal ART adherence is thus contributing to the propagation of the HIV epidemic. As a result, over half of new HIV infections in Peru occur among MSM (Alarcon et al., 2012; UNAIDS, 2012).
Given the elevated presence of HIV, AUDs and risky sex among Peruvian MSM, HIV prevention and intervention strategies must target multiple risk factors. Additionally, based on recent international guidelines (Thompson et al., 2012), the next generation of adherence interventions should be scaled back, both in terms of cost and personnel. Mobile technologies can provide innovative, cost-effective and efficacious strategies to target alcohol abuse, improve ART adherence, and optimize HIV treatment outcomes (Boyer, Smelson, Fletcher, Ziedonis, & Picard, 2010; Lester, Gelmon, & Plummer, 2006). In healthcare management, mobile health (mHealth) - the use of mobile and wireless devices to improve health outcomes - is an innovative and cost-effective tool in managing personal healthcare and promoting preventive behaviors (Fjeldsoe, Marshall, & Miller, 2009; Katz & Nordwall, 2008; Lim, Hocking, Hellard, & Aitken, 2008). It has been suggested that mHealth’s greatest benefits can be felt in resource-limited settings (Atun & Sittampalam, 2006; Karanja et al., 2011; Leach-Lemens, 2009; Lester et al., 2006); thus making its use particularly appealing in vulnerable populations, such as HIV-infected MSM in a middle-income country like Peru.
mHealth interventions such as cell phone reminders and text messaging have already been shown to be efficacious in improving treatment adherence in patients with various chronic conditions like diabetes (Hanauer, Wentzell, Laffel, & Laffel, 2009; Yoon & Kim, 2008), tuberculosis (Hoffman et al., 2010; Person, Blain, Jiang, Rasmussen, & Stout, 2011), malaria (Asiimwe et al., 2011; Meankaew et al., 2010), asthma (Prabhakaran, Chee, Chua, Abisheganaden, & Wong, 2010; Ryan et al., 2009), and more recently among people living with HIV/AIDS (PLWHA) (Lester & Kariri, 2009; Lester et al., 2010; Pop-Eleches et al., 2011). Despite these promising trends, a systematic review of mHealth studies in HIV research (Fraser, 2013) points to a lack of evidence on the use of mHealth tools in addressing the needs of one particular group of PLWHA – MSM. Historically, MSM and lesbian, gay, bisexual, transgender (LGBT) consumers have been documented as early adopters of information and communication technologies such as the internet (Bolding, Davis, Sherr, Hart, & Elford, 2004; Reback, Ling, Shoptaw, & Rohde, 2010). To date however, there are no published data on the use and acceptance of mobile technologies and mHealth interventions among HIV-infected MSM in South American countries, including Peru.
Peru is experiencing rapid growth in mobile phone adoption and use – sales of cell phones increased from 9.8 million in 2007 (OSIPTEL, 2007) to nearly 33 million in 2012 (CIA, 2009), thereby reaching a penetration rate of 110%. The mobile market growth is being driven by postpaid customers, mobile broadband and smartphones (Extensia, 2012). Even though broadband’s growth rate has been proportionately slow due to infrastructure challenges, Peruvians are active internet users with almost a third of the population accessing the internet in public internet cafes called cabinas públicas (Extensia, 2012). The growth of communication technology in Peru shows promise in being able to integrate mHealth tools to aid health management. There is still, however, a dearth of information about the acceptance of mHealth and communication technology. A quasi-quantitative study conducted in Peru found that three-fourths of PLWHA were willing to use cell phones to receive reminders about their HIV medication and receive messages about their sexual health (Curioso & Kurth, 2007). Despite that study, there remains no published assessment of communication technology use or mHealth acceptance among HIV-infected MSM. To address this gap, we sought to examine the use of communication technology (i.e., landline phone, internet, cell phone) and acceptance of mHealth among HIV-infected Peruvian MSM and transgender women (TGW) in order to gauge the feasibility of designing and implementing a mHealth-enabled HIV-risk reduction program.
Methods
Study sample and procedure
A convenience sample of 359 HIV-infected MSM and TGW was recruited over 12 weeks from three sites at two NGOs providing healthcare in Lima, Peru. Eligibility criteria included 1) 18–65 years of age; 2) born male; and 3) diagnosed with HIV for at least one year. Patients were approached by clinical staff at each site and referred to research assistants. After informed consent, they completed a computer-assisted self-administered survey to assess socio-demographic characteristics, AUDs, depression, risky sexual behavior, ART adherence, along with measures of communication technology access and utilization, and mHealth acceptance. Participants were paid 25 Nuevos Soles (approximately US $9.50) for their time. Approval for this study was obtained from the Institutional Review Boards at Yale University, Associación Civil Impacta Salud y Educación and Via Libre.
Measures
Socio-demographic variables included self-reported measures of age, sex, sexual orientation, education, employment status, income and living situation. Depression was measured using the 10-item Center for Epidemiologic Studies Depression Scale (CES-D 10) (Radloff, 1977) with a cut-off of > 7 to define moderate-to-severe depression. Health literacy was assessed using the Short Test of Functional Health Literacy in Adults (STOHFLA) (Chew, Bradley, & Boyko, 2004). AUDs were scored using the World Health Organization’s validated 10-item Alcohol Use Disorders Identification Test (AUDIT) (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), with standard cut-offs of ≥ 8 to define any AUD and ≥ 20 to define alcohol dependence. Risky sexual behavior was measured using the Alaska criteria consisting of five binary items associated with HIV seroconversion (Sanchez et al., 2009). ART adherence was assessed by self-report using a previously validated visual analog scale (VAS) (Giordano, Guzman, Clark, Charlebois, & Bangsberg, 2004). Based on findings that suggest that viral suppression is correlated with high levels of adherence (Elul et al., 2013), adherence was categorized as optimal (≥ 90%) and perfect (100%).
Due to the lack of validated communication technology access and utilization scales and a mHealth acceptance scale, we self-constructed these measures for the purpose of this study. For communication technology access and utilization, the availability of various information and communication technologies (ICT) in South America was assessed in order to create the items. The mHealth acceptance measure was constructed after conducting a literature review of the various mHealth tools and strategies being used in health management studies. Access to various communication technologies (i.e., landline telephone, cell phone, computer etc.) was measured as a categorical variable. Participants’ utilization of various communication devices (e.g., ‘receiving text messages on a mobile device’) was assessed with nine items scored on a 5-point Likert scale (ranging from 1 = ‘never’ to 5 = ‘always’). mHealth acceptance (e.g., ‘interested in using mobile technology for medication reminders’) was assessed using eight items scored on a 5-point Likert scale (ranging from 1 = ‘not interested at all’ to 5 = ‘very interested’). Finally, participants’ preference of type of mHealth medication reminder (‘phone call’, ‘text message’, ‘email’) was assessed with three nominal variables.
Standardized measures that have been previously translated and validated in Spanish were used. Self-constructed measures, however, were first created in English, translated into Spanish and then back-translated into English to ensure face validity (Brislin, 1970). The translated questionnaire was pilot-tested among HIV-infected MSM in Lima prior to dissemination of the survey.
Data analysis
Data were analyzed using SPSS 19 (IBM, New York). Descriptive statistics and frequencies were conducted on all relevant study measures. One-way MANOVAs were conducted to determine if significant (p < 0.05) differences existed in communication technology use and mHealth acceptance between participants who might be targets for future intervention, specifically those meeting criteria for an AUD, depression and optimal ART adherence, all of which are associated with poor HIV treatment outcomes (Altice et al., 2011; Maru et al., 2008; Wood, Hogg, et al., 2004; Wood, Montaner, et al., 2004). Chi-square tests were conducted to examine if significant differences existed between access to communication technology between participants with and without optimal adherence.
Results
Participants (Table 1) were relatively young (M=34.0 years) and well-educated. Most (79.1%) participants self-identified as homosexual and 13.3% as transgender (none identified as heterosexual). Most had either full or part-time employment (71%), with only 3.5% falling under the poverty line. The mean health literacy score was high across multiple categories. Nearly 60% met screening criteria for moderate to severe depression. The prevalence of AUDs in this sample was also high – 39.8% met screening criteria for an AUD and 4.2% were dependent drinkers (see Table 1). Self-reported risky sexual behaviors were highly prevalent; in the previous 6 months, 78.3% reported unprotected sex during their last encounter, 34.8% reported having anal sex with more than five partners, and 22.6% reported having sex with HIV-infected partners. The prevalence for any risky sex, i.e., was extraordinarily high – 90.8% reported having engaged in at least one risky sexual behavior recently. Of the 359 HIV-infected, participants, 313 (87.2%) were on ART, with 85.6% reporting optimal adherence and 54.5% reporting perfect adherence
Table 1.
Characteristics of study participants (N = 359)
| Socio-demographic Characteristics | n (%) |
|---|---|
| Age in years [Mean (SD)] | 34.0 (8.11) |
| Sex | |
| Male | 279 (77.7) |
| Transgender | 48 (13.3) |
| Sexual Orientation | |
| Homosexual | 284 (79.1) |
| Bisexual | 60 (16.7) |
| Heterosexual | 15 (4.2) |
| Education | |
| Primary | 8 (2.2) |
| Secondary | 103 (28.7) |
| College | 246 (68.5) |
| Completed college (N=246) | 131 (53.3) |
| Employment Status | |
| Stable job | 163 (45.4%) |
| Part-time job | 92 (25.6%) |
| Unemployed | 33 (9.2%) |
| Below poverty level (less than 257 Nuevos Soles per month) | 11 (3.5) |
| Whom do you live with? | |
| Single | 71 (19.8) |
| Male partner (gay) | 47 (13.1) |
| Relatives (parents, other) | 199 (55.4) |
| Depressiona | |
| No depression | 142 (39.6) |
| Moderate to severe depression | 215 (59.9) |
| Health Literacy Score [Mean (SD)] | |
| How often do you have problems learning about your medical condition because of difficulty understanding written information?b | 1.80 (0.80) |
| How often do you have someone (like a family member, friend, hospital/clinic worker, or caregiver) help you read hospital materials?b | 1.90 (0.93) |
| How confident are you filling out medical forms by yourself?c | 3.15 (1.08) |
| Alcohol Use Disorders | |
| Any AUD | 143 (39.8) |
| Alcohol dependence | 15 (4.2) |
| Risky Sex | |
| Anal sex with more than 5 partners in the past 6 months | 125 (34.8) |
| Sex with HIV-positive partners in the last 6 months | 81 (22.6) |
| Sex with a person with an STI in the past 6 months | 56 (15.6) |
| Sexual activity as sex worker in the last 6 months | 23 (6.4) |
| Did not use protection (i.e. use a condom) during the last sexual encounter | 281 (78.3) |
| ART Adherence | |
| On ART currently | 313 (87.2) |
| Optimal ART ≥ 90% | 267 (85.6) |
| Perfect ART = 100% | 170 (54.5) |
Measured using the CES-D 10 scale with a cut-off of >7 to indicate moderate to severe depression
Scored on a 5-point Likert scale (1=Never, 2=Rarely, 3=Sometimes, 4=Often, 5=Always)
Scored on a 5-point Likert scale (1 being ‘Not at all confident’ to 5 being ‘Extremely confident’)
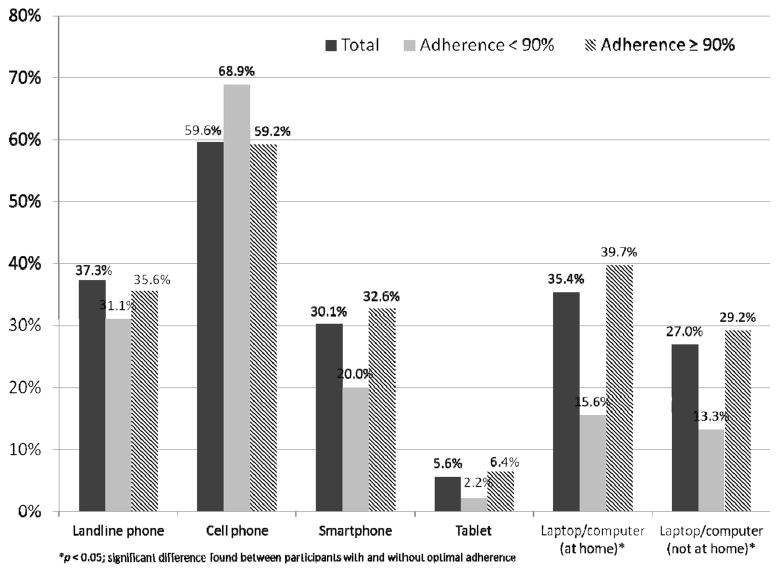
With respect to communication technology access, the majority had daily access to standard cell phones (59.6%), 30.1% had access to a smartphone, 37.3% used landlines and 35.4% regularly accessed a personal laptop/computer (Figure 1). Chi-square tests conducted to examine differences in daily access to various communication technologies between participants with and without optimal adherence found no significant differences, except that participants with optimal adherence were significantly more likely (p < 0.05) to report having daily access to a laptop/computer either at home or outside.
Figure 1.
Percentage of participants with daily access to communication technology (N = 359)
*p<0.05; significant difference found between participants with and without optimal adherence
The most frequent activity was receiving calls or text messages on a mobile device, followed by making calls and sending text messages on a mobile device (see Table 2). The least frequent activities were browsing the internet on a mobile device or computer, and making and receiving calls on a landline telephone. Table 2 also depicts participants’ interest in accepting various mHealth interventions. Overall, there was interest in mHealth for health management behaviors especially in using technology for medication reminders (M=3.21, SD=1.32) and engaging in an anonymous internet chat with a health professional to discuss HIV-related issues (M=3.56, SD=1.33). Participants were also interested in receiving electronic medication reminders on a daily, weekly or monthly basis; daily reminders however, garnered the highest interest (M=3.23, SD=1.20). The results of the MANOVA showed that no differences existed between participants having an AUD and depression and their use and acceptance of communication technology and mHealth. An overall significant effect, however, was seen for mHealth acceptance among participants with and without optimal ART adherence at Lambda (2, 309) = 6.30, p < 0.01. Follow-up univariate ANOVAs however indicated that participants with sub-optimal adherence were less likely than those with optimal adherence to show interest in only one specific mHealth activity – engagement in an anonymous internet chat with a health professional to discuss HIV-related issues (F (1,310) = 12.57, p < 0.001).
Table 2.
Communication technology use and mHealth acceptance among study participants
| Overall Mean (SD) | Factors Commonly Associated with Poor HIV Treatment Outcome
|
||||||
|---|---|---|---|---|---|---|---|
| Alcohol Use Disorder | Depression | Optimal Adherence ≥ 90% | |||||
|
| |||||||
| Yes | No | Yes | No | Yes | No | ||
| Communication Technology Utilization | |||||||
|
| |||||||
| a How often do you do the following… | |||||||
| Receive calls on landline telephone | 2.39 (1.18) | 2.38 (1.22) | 2.40 (1.17) | 2.42 (1.18) | 2.35 (1.20) | 2.43 (1.20) | 2.27 (1.27) |
| Make calls on landline telephone | 2.40 (1.05) | 2.41 (1.05) | 2.40 (1.06) | 2.48 (1.10) | 2.28 (0.97) | 2.41 (1.07) | 2.47 (1.04) |
| Receive calls on your mobile device (cell phone, smartphone, tablet) | 3.73 (1.18) | 3.78 (1.20) | 3.70 (1.17) | 3.73 (1.12) | 3.71 (1.28) | 3.80 (1.13) | 3.47 (1.22) |
| Make calls on your mobile device (cell phone, smartphone, tablet) | 3.47 (1.23) | 3.46 (1.26) | 3.48 (1.22) | 3.43 (1.24) | 3.51 (1.22) | 3.49 (1.20) | 3.24 (1.20) |
| Receive text messages on your mobile device (cell phone, smartphone, tablet) | 3.57 (1.23) | 3.59 (1.22) | 3.56 (1.24) | 3.60 (1.24) | 3.50 (1.21) | 3.59 (1.19) | 3.40 (1.27) |
| Send text messages on your mobile device (cell phone, smartphone, tablet) | 3.34 (1.32) | 3.38 (1.26) | 3.31 (1.37) | 3.41 (1.36) | 3.24 (1.27) | 3.36 (1.30) | 3.18 (1.37) |
| Browse the internet on your smartphone, tablet, computer or laptop | 2.07 (1.44) | 1.99 (1.43) | 2.13 (1.45) | 2.07 (1.45) | 2.09 (1.43) | 2.14 (1.47) | 1.76 (1.21) |
| Send and/or receive emails while at home | 2.47 (1.46) | 2.22 (1.39) | 2.63 (1.49) | 2.62 (1.50) | 2.25 (1.38) | 2.54 (1.47) | 2.16 (1.36) |
| Send and/or receive emails when not at home | 2.48 (1.30) | 2.44 (1.30) | 2.51 (1.30) | 2.50 (1.33) | 2.47 (1.25) | 2.53 (1.30) | 2.24 (1.26) |
|
| |||||||
| mHealth Acceptance | |||||||
|
| |||||||
| b How interested would you be in… | |||||||
| Interested in using technology for medication reminders | 3.21 (1.32) | 3.27 (1.34) | 3.17 (1.30) | 3.13 (1.35) | 3.32 (1.27) | 3.23 (1.35) | 2.87 (1.27) |
| Interested in engaging in an anonymous internet chat with a health professional to discuss HIV-related issues | 3.56 (1.33) | 3.59 (1.21) | 3.55 (1.40) | 3.60 (1.34) | 3.52 (1.30) | 3.67 (1.29)* | 2.93 (1.32)* |
| Interested in receiving daily electronic medication reminders | 3.23 (1.20) | 3.25 (1.23) | 3.22 (1.19) | 3.24 (1.22) | 3.22 (1.20) | 3.23 (1.21) | 3.08 (1.08) |
| Interested in receiving weekly electronic medication reminders | 3.15 (1.19) | 3.09 (1.19) | 3.19 (1.20) | 3.17 (1.19) | 3.12 (1.21) | 3.13 (1.20) | 3.00 (1.16) |
| Interested in receiving monthly electronic medication reminders | 3.11 (1.26) | 3.10 (1.29) | 3.11 (1.24) | 3.12 (1.26) | 3.09 (1.27) | 3.08 (1.28) | 2.89 (1.18) |
| Interested in sending back a response to a daily text message medication reminders | 3.14 (1.33) | 3.20 (1.31) | 3.10 (1.35) | 3.12 (1.35) | 3.15 (1.32) | 3.10 (1.34) | 3.00 (1.23) |
| Interested in sending back a response to a weekly text message medication reminders | 3.17 (1.32) | 3.21 (1.32) | 3.14 (1.33) | 3.22 (1.33) | 3.07 (1.31) | 3.13 (1.31) | 2.87 (1.26) |
| Interested in sending back a response to a monthly text message medication reminders | 3.08 (1.28) | 3.11 (1.29) | 3.05 (1.28) | 3.08 (1.27) | 3.06 (1.30) | 3.06 (1.30) | 2.82 (1.18) |
Scored on a 5-point Likert scale (from 1 being ‘Never’ to 5 being ‘Always’)
Scored on a 5-point Likert scale (from 1 being ‘Not interested at all’ to 5 being ‘Very interested’)
Univariate ANOVA test was significant at p < 0.001; this was preceded by a one-way MANOVA that yielded an overall significant effect of optimal adherence on mHealth acceptance
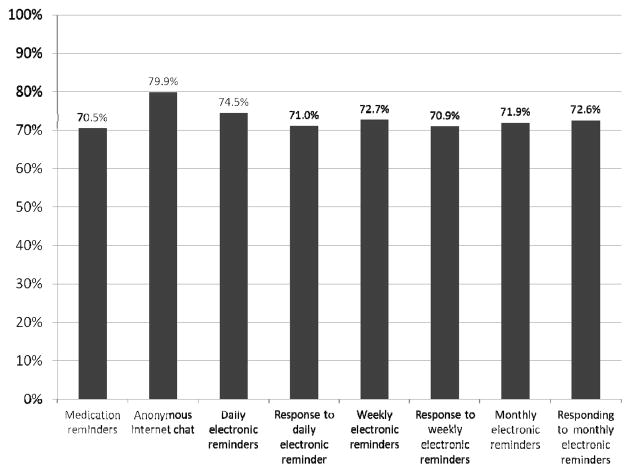
Figure 2 shows the percentage of participants who expressed moderate to high interest in accepting various mHealth interventions. Across all categories, 79.9% expressed interest in anonymous internet chats with a health professional. Table 3 depicts participants’ preference for the type of mHealth medication reminder. Approximately 40% of participants preferred text message reminders, 25% preferred phone calls and 15% preferred emails. The most preferred electronic medication reminder was a daily text message (43.3%). Only 10% of participants expressed no interest in receiving any form of electronic medication reminder.
Figure 2.
Interest in mHealth acceptance among study participants (N = 359)
Table 3.
Preference for type and frequency of mHealth medication reminder among study participants (N = 359)
| Frequency of Reminder | Type of Electronic Medication Reminder n (%)
|
|||
|---|---|---|---|---|
| Text message | Phone call | Not interested | ||
| Daily electronic medication reminder | 136 (43.3) | 64 (20.4) | 45 (14.3) | 28 (8.9) |
| Weekly electronic medication reminder | 127 (40.4) | 78 (24.8) | 44 (14.0) | 30 (9.6) |
| Monthly electronic medication reminder | 115 (36.6) | 76 (24.2) | 49 (15.6) | 43 (13.7) |
Discussion
To our knowledge, this is the first quantitative assessment of communication technology use and mHealth acceptance among HIV-infected MSM and TGW in South America. Even though mHealth projects have occasionally been implemented in Peru and other South American countries (Gazzer, 2012)), there is an inherent lack of empirical knowledge about the acceptability of such innovative tools among MSM and TGW, especially those with co-morbid substance use disorders (SUDs) and depression. This study offers tangible evidence supporting the development of mHealth-based intervention strategies in this socially-marginalized and understudied population.
The findings from our study show that Peruvian MSM and TGW have good access to communication technology tools, especially cell phones and smartphones Interestingly, smartphone adoption among Peruvian MSM is significantly higher than the general population (Andina, 2013). This is consistent with previous studies that have also found MSM and LGBT populations to be early adopters of emerging communication technologies (Bolding et al., 2004; Reback et al., 2010). More participants used cell phones to communicate (e.g., primarily through text messages) compared to landline phones and the internet. This likely reflects the fast-paced growth of mobile technology infrastructure in Peru (CIA, 2009). While considering technology for health and development purposes in low and middle-income countries, slow technology diffusion and digital divide are usually common obstacles. MSM in Peru, however, seem to be relatively sophisticated in their access to and use of communication technology, thus making them an ideal population for introducing mHealth intervention tools.
With respect to mHealth acceptance, our findings show considerable interest among Peruvian HIV-infected MSM in mHealth interventions for medication reminders and engaging in anonymous interactions with healthcare providers to discuss HIV-related issues. The latter is an especially important finding as it tallies with findings in HIV-infected minority populations in the U.S., especially where there are high levels of HIV-related stigma (Kalichman, Benotsch, Weinhardt, Austin, & Luke, 2002). The anonymity provided by online interactions can reduce negative consequences of stigma and facilitate more self-disclosure regarding one’s sexual identity and HIV status, both of which remain taboo in much of Peru. Importantly, there were no significant differences in communication technology use and mHealth acceptance among participants based on factors that have been shown to be associated with poor HIV treatment outcomes, specifically having an AUD, suffering from depression and maintaining sub-optimal ART adherence (Altice et al., 2011; Maru et al., 2008; Wood, Hogg, et al., 2004; Wood, Montaner, et al., 2004). Of note, however, participants with sub-optimal adherence were less likely to be interested in engaging in an anonymous internet chat with a health professional to discuss HIV-related issues. It may be that individuals with adherence difficulties have internal trouble engaging fully in their HIV care or alternatively, they might prefer face-to-face interactions to discuss HIV-related health issues.
Overall, participants were willing to adopt daily electronic ART medication reminders. Almost two-thirds of the participants expressed a preference for receiving medication reminders through cell phones. Cell phone reminders have been successfully used in resource-constrained settings like sub-Saharan Africa to improve ART adherence (Lester & Kariri, 2009; Lester et al., 2010). Cell phone messages can similarly be utilized in the MSM community for medication reminders and additionally to target them with HIV-prevention or risk-reduction health campaigns. Overall, this study has documented empirical support for a mHealth-based intervention among HIV-infected Peruvian MSM, including for those with underlying characteristics associated with decreased ART adherence such as AUDs. mHealth tools such as cell phones can be used in several ways to benefit the health of HIV-infected MSM community. Firstly, they can be used for medication and appointment reminders as a means to improve HIV monitoring and health outcomes, as has been shown elsewhere (da Costa et al., 2012; Lester et al., 2010). Secondly, mobile technology can be used to collect real-time data through ecological momentary assessments (EMA) of risk behaviors (such as sexual risk behaviors) among HIV-infected MSM so as to establish concurrency between inter-related risk factors and thus design effective HIV-prevention programs. Lastly, mHealth can be integrated into large-scale CBT or pharmocological interventions targeting MSM with AUDs to improve medication adherence and retention in care. There is a need for innovative HIV prevention strategies that are specifically designed for HIV-infected MSM and TGW with a focus on reducing both alcohol use and risky sexual behavior; mHealth tools are ideally placed to offer innovative, cost-effective and efficacious strategies.
Limitations
The use of self-reported data may have resulted in inaccuracies due to recall bias, but there is no reason for participants to over- or under-report findings here. Questions relating to mHealth acceptance were hypothetical in nature. Participants’ acceptance of any particular mHealth tool can be better gauged through an acceptability study. Finally, due to the specificity of the population described in this study, specifically MSM and TGW, the findings may not be generalizable to other populations. Nonetheless, the results provide support for the development and implementation of mHealth intervention programs as a means of improving HIV outcomes.
Conclusion
Peru’s rapidly expanding mobile and broadband infrastructure and our assessment of communication technology use and mHealth acceptance among HIV-infected MSM support further development and implementation of mHealth intervention programs among HIV-infected MSM that target HIV-related health behaviors and risk-reduction strategies. Important among these findings is that the group of individuals who might benefit most from such technologies (i.e., those with AUDs, depression, or suboptimal adherence) were no less likely than their counterparts to endorse use of mHealth strategies. mHealth tools especially cell phones, can offer cost-effective and efficacious methods of improving medication adherence and health outcomes. Additionally, they can also be integrated into multimodal counseling or pharmacological interventions targeting HIV-infected MSM with AUDs. mHealth interventions are emerging as innovative strategies to improve health, yet there remains insufficient evidence to inform implementation and scale-up (Tomlinson, Rotheram-Borus, Swartz, & Tsai, 2013); thus, there is a need for more efficacy and effectiveness trials.
References
- Alarcon JO, Pun M, Gutierrez C, Whittembury A, Tejada R, Suarez L, Cuchi P. Estimation and analysis of HIV incidence in the adult population in Peru: Results of application of the MoT mathematical model. Rev Peru Med Exp Salud Publica. 2012;29(4):452–460. doi: 10.1590/s1726-46342012000400006. [DOI] [PubMed] [Google Scholar]
- Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, Finkelstein R. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: Results from a multisite study. J Acquir Immune Defic Syndr. 2011;56(Suppl 1):S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andina. [Accessed February 16, 2014];Smartphone penetration in Peru reaches 17 percent. Andina 2013 [Google Scholar]
- Asiimwe C, Gelvin D, Lee EJ, Amor YB, Quinto E, Katureebe C, Berg M. Use of an innovative, affordable, and open-source short message service–based tool to monitor Malaria in remote areas of Uganda. The American Journal of Tropical Medicine and Hygiene. 2011;85(1):26–33. doi: 10.4269/ajtmh.2011.10-0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atun R, Sittampalam S. A review of the charcteristics and benefits of SMS in delivering healthcare. The Role of Mobile Phones in Increasing Accessibility and Efficiency in Healthcare Report 2006 [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test. Geneva, Switzerland: World Health Organization (W.H.O.); 2001. [Google Scholar]
- Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: A systematic review. PLoS Med. 2007;4(12):e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, Brookmeyer R. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolding G, Davis M, Sherr L, Hart G, Elford J. Use of gay Internet sites and views about online health promotion among men who have sex with men. AIDS Care. 2004;16(8):993–1001. doi: 10.1080/09540120412331292453. [DOI] [PubMed] [Google Scholar]
- Boyer E, Smelson D, Fletcher R, Ziedonis D, Picard R. Wireless technologies, ubiquitous computing and mobile health: Application to drug abuse treatment and compliance with HIV therapies. Journal of Medical Toxicology. 2010;6(2):212–216. doi: 10.1007/s13181-010-0080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brislin RW. Back-Translation for Cross-Cultural Research. Journal of Cross-Cultural Psychology. 1970;1:185–216. [Google Scholar]
- Carcamo CP, Campos PE, Garcia PJ, Hughes JP, Garnett GP, Holmes KK Peru Preven study team. Prevalences of sexually transmitted infections in young adults and female sex workers in Peru: A national population-based survey. Lancet Infect Dis. 2012;12(10):765–773. doi: 10.1016/S1473-3099(12)70144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- CIA. The World Facebbok. 2009 Retrieved Oct. 1, 2013, from https://www.cia.gov/library/publications/the-world-factbook/geos/pe.html.
- Curioso Walter H, Kurth Ann E. Access, use and perceptions regarding Internet, cell phones and PDAs as a means for health promotion for people living with HIV in Peru. BMC medical informatics and decision making. 2007;7(1):24. doi: 10.1186/1472-6947-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Costa TM, Barbosa BJ, Gomes e Costa DA, Sigulem D, de Fatima Marin H, Filho AC, Pisa IT. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform. 2012;81(4):257–269. doi: 10.1016/j.ijmedinf.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deiss RG, Clark JL, Konda KA, Leon SR, Klausner JD, Caceres CF, Coates TJ. Problem drinking is associated with increased prevalence of sexual risk behaviors among men who have sex with men (MSM) in Lima, Peru. Drug Alcohol Depend. 2013;132(1–2):134–139. doi: 10.1016/j.drugalcdep.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elul B, Basinga P, Nuwagaba-Biribonwoha H, Saito S, Horowitz D, Nash D, Asiimwe A. High levels of adherence and viral suppression in a nationally representative sample of HIV-infected adults on antiretroviral therapy for 6, 12 and 18 months in Rwanda. PLoS One. 2013;8(1):e53586. doi: 10.1371/journal.pone.0053586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Extensia. Peru - Telecoms, Mobile, Broadband and Forecasts 2012 [Google Scholar]
- Ferro EG, Weikum D, Vagenas P, Copenhaver M, Gonzales P, Peinado J, Altice FL. Alcohol use disorders negatively influence antiretroviral medication adherence among men who have sex with men and transgender women in Peru. Paper presented at the 7th IAS Conference on HIV Pathogenesis, Treatment and Prevention; Kuala Lumpur . 2013. http://pag.ias2013.org/Abstracts.aspx?AID=1733. [Google Scholar]
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine. 2009;36(2):165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- Fraser H. mHealth for HIV treatment & prevention: A systematic review of the literature. Open AIDS Journal. 2013;7 doi: 10.2174/1874613620130812003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzer E. How Peru and Latin America are using mHealth. Exchange. 2012 Oct 8;:14–15. 2013. [Google Scholar]
- Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5(2):74–79. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11(2):99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman Jeffrey A, Cunningham Janice R, Suleh Andrew J, Sundsmo Aaron, Dekker Debra, Vago Fred, Hunt-Glassman Jonathan. Mobile direct observation treatment for Tuberculosis patients: A technical feasibility pilot using mobile phones in Nairobi, Kenya. American Journal of Preventive Medicine. 2010;39(1):78–80. doi: 10.1016/j.amepre.2010.02.018. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Benotsch EG, Weinhardt LS, Austin J, Luke W. Internet use among people living with HIV/AIDS: Association of health information, health behaviors, and health status. AIDS Educ Prev. 2002;14(1):51–61. doi: 10.1521/aeap.14.1.51.24335. [DOI] [PubMed] [Google Scholar]
- Karanja S, Mbuagbaw L, Ritvo P, Law J, Kyobutungi C, Reid G, Lester R. A workshop report on HIV mHealth synergy and strategy meeting to review emerging evidence-based mHealth interventions and develop a framework for scale-up of these interventions. Pan Afr Med J. 2011;10:37. [PMC free article] [PubMed] [Google Scholar]
- Katz DL, Nordwall B. Novel interactive cell-phone technology for health enhancement. J Diabetes Sci Technol. 2008;2(1):147–153. doi: 10.1177/193229680800200122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach-Lemens C. Using mobile phones in HIV care and prevention. HIV & AIDS Treatment in Practice. 2009;137:7. [Google Scholar]
- Lester RT, Gelmon L, Plummer FA. Cell phones: Tightening the communication gap in resource-limited antiretroviral programmes? AIDS. 2006;20(17):2242–2244. doi: 10.1097/QAD.0b013e3280108508. [DOI] [PubMed] [Google Scholar]
- Lester RT, Kariri A. Mobilizing cell phones to improve antiretroviral adherence and follow-up in Kenya: A randomized controlled trial in progress. WHO Essential Medicines Monitor. 2009;2:Article 1. [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. The Lancet. 2010;376(9755):1838–1845. doi: 10.1016/s0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Lim Megan SC, Hocking Jane S, Hellard Margaret E, Aitken Campbell K. SMS STI: A review of the uses of mobile phone text messaging in sexual health. International Journal of STD & AIDS. 2008;19(5):287–290. doi: 10.1258/ijsa.2007.007264. [DOI] [PubMed] [Google Scholar]
- Ludford KT, Vagenas P, Lama JR, Peinado J, Gonzales P, Leiva R, Peruvian HIV Sentinel Surveillance Working Group. Screening for drug and alcohol use disorders and their association with HIV-related sexual risk behaviors among men who have sex with men in Peru. PLoS One. 2013;8(8):e69966. doi: 10.1371/journal.pone.0069966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maru DS, Bruce RD, Walton M, Mezger JA, Springer SA, Shield D, Altice FL. Initiation, adherence, and retention in a randomized controlled trial of directly administered antiretroviral therapy. AIDS Behav. 2008;12(2):284–293. doi: 10.1007/s10461-007-9336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meankaew P, Kaewkungwal J, Khamsiriwatchara A, Khunthong P, Singhasivanon P, Satimai W. Application of mobile-technology for disease and treatment monitoring of malaria in the “Better Border Healthcare Programme”. Malar J. 2010;9:237. doi: 10.1186/1475-2875-9-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OSIPTEL. Telecommunications in Peru (statistics) 2007 [Google Scholar]
- Person AK, Blain ML, Jiang H, Rasmussen PW, Stout JE. Text messaging for enhancement of testing and treatment for tuberculosis, human immunodeficiency virus, and syphilis: A survey of attitudes toward cellular phones and healthcare. Telemed J E Health. 2011;17(3):189–195. doi: 10.1089/tmj.2010.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. Aids. 2011;25(6):825–834. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prabhakaran L, Chee WY, Chua KC, Abisheganaden J, Wong WM. The use of text messaging to improve asthma control: A pilot study using the mobile phone short messaging service (SMS) J Telemed Telecare. 2010;16(5):286–290. doi: 10.1258/jtt.2010.090809. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore S. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Reback Cathy J, Ling Deborah, Shoptaw Steven, Rohde Jane. Developing a text messaging risk reduction intervention for methamphetamine-using MSM: Research note. The open AIDS journal. 2010;4:116. doi: 10.2174/1874613601004030116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan D, Pinnock H, Lee AJ, Tarassenko L, Pagliari C, Sheikh A, Price D. The CYMPLA trial. Mobile phone-based structured intervention to achieve asthma control in patients with uncontrolled persistent asthma: A pragmatic randomised controlled trial. Prim Care Respir J. 2009;18(4):343–345. doi: 10.4104/pcrj.2009.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez J, Lama JR, Kusunoki L, Manrique H, Goicochea P, Lucchetti A, Celum C. HIV-1, sexually transmitted infections, and sexual behavior trends among men who have sex with men in Lima, Peru. J Acquir Immune Defic Syndr. 2007;44(5):578–585. doi: 10.1097/QAI.0b013e318033ff82. [DOI] [PubMed] [Google Scholar]
- Sanchez J, Lama JR, Peinado J, Paredes A, Lucchetti A, Russell K, Sebastian JL. High HIV and ulcerative sexually transmitted infection incidence estimates among men who have sex with men in Peru: awaiting for an effective preventive intervention. J Acquir Immune Defic Syndr. 2009;51(Suppl 1):S47–51. doi: 10.1097/QAI.0b013e3181a2671d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura E, Konda K, Salvatierra J, Galea J, Chunga D, Alcantara J. Alcohol consumption and unprotected anal intercourse among Peruvian MSM: Results from an STI clinic-based survey. Paper presented at the XVII International AIDS Conference; Mexico city, Mexico. 2008. [Google Scholar]
- Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, Nachega JB. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: Evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–833. W-284, W-285, W-286, W-287, W-288, W-289, W-290, W-291, W-292, W-293, W-294. doi: 10.1059/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC. Scaling up mHealth: Where is the evidence? PLoS Med. 2013;10(2):e1001382. doi: 10.1371/journal.pmed.1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Peru launches campaign to increase HIV testing among men 2012 [Google Scholar]
- Wood E, Hogg RS, Yip B, Harrigan PR, O’Shaughnessy MV, Montaner JS. The impact of adherence on CD4 cell count responses among HIV-infected patients. J Acquir Immune Defic Syndr. 2004;35(3):261–268. doi: 10.1097/00126334-200403010-00006. [DOI] [PubMed] [Google Scholar]
- Wood E, Montaner JS, Yip B, Tyndall MW, Schechter MT, O’Shaughnessy MV, Hogg RS. Adherence to antiretroviral therapy and CD4 T-cell count responses among HIV-infected injection drug users. Antivir Ther. 2004;9(2):229–235. [PubMed] [Google Scholar]
- Yoon KH, Kim HS. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Res Clin Pract. 2008;79(2):256–261. doi: 10.1016/j.diabres.2007.09.007. [DOI] [PubMed] [Google Scholar]