Abstract
Introduction and Aims
Crack pipe sharing is a risky practice that has been associated with the transmission of Hepatitis C and other harms. While previous research has exclusively focused on this phenomenon among adults, this study examines crack pipe sharing among street-involved youth.
Design and Methods
From May 2006 to May 2012, data were collected from the At-Risk Youth Study, a cohort of street-involved youth age 14–26 in Vancouver, Canada. Survey data from active crack smokers were analysed using generalised estimating equations logistic regression.
Results
Over the study period, 567 youth reported smoking crack cocaine and contributed 1288 observations, among which 961 (75%) included a report of crack pipe sharing. In multivariate analysis, factors that were associated with crack pipe sharing included: difficulty accessing crack pipes (adjusted odds ratio [AOR] =1.58, 95% confidence interval [CI] 1.13–2.20); homelessness (AOR =1.87, 95%CI 1.43–2.44); regular employment (AOR =1.53, 95%CI 1.15–2.04); daily non-injection crystal methamphetamine use (AOR =2.04, 95%CI 1.11–3.75); daily crack smoking (AOR =1.37, 95%CI 1.01–1.85); encounters with the police (AOR =1.42, 95%CI 1.01–1.99); and reporting unprotected sex (AOR =1.95, 95%CI 1.47–2.58).
Discussion and Conclusions
The prevalence of crack pipe sharing was high among our sample and independently associated with structural factors including difficulty accessing crack pipes and homelessness. Crack pipe sharing was also associated with high intensity drug use and a number of other markers of risk and vulnerability. Collectively, these findings highlight opportunities for health services to better engage with this vulnerable group and reduce this risky behaviour.
Keywords: crack cocaine, street-involved youth, harm reduction, risk behaviour, police
INTRODUCTION
High rates of crack cocaine use have been reported among groups of street-involved youth, although exact figures vary. North American researchers have found the lifetime prevalence of crack smoking among street-involved youth to be as low as 5.8% across Canada [1], to 36% among homeless youth in New York City [2], and as high as 52% among a cohort of street-involved youth in Montreal [3]. This is particularly concerning given that crack cocaine smoking poses numerous public health concerns due to the health-related harms associated with its use. Crack cocaine smoking has previously been linked to blisters, sores, and cuts on the lips and oral cavities of young and adult drug-users [4,5] and infection transmission, including sexually transmitted infections [6], Hepatitis C [7,8], and HIV [9,10]. Although high risk sexual practices have been associated with stimulant drug use [11–13], the use of glass crack pipes and sharing those pipes with others also poses risks for disease transmission and have been implicated in the transmission of Hepatitis C in particular [7,8]. Specifically, sharing inhalation implements has been found to be more strongly associated with Hepatitis C infection than duration of crack use [8], suggesting that crack pipe sharing may be an independent source of risk.
Despite high numbers of street-involved youth using crack, there is very little data on crack pipe sharing among this group. Previous research on crack pipe sharing has found that this practice is common and has been increasing among adult drug-users in many North American settings [14,15]. Difficulty accessing crack pipes has been positively associated with sharing pipes [14] and conversely, the distribution of safer crack-smoking materials has been found to reduce pipe sharing [15]. The same study from Ontario, Canada also reported a decrease in the frequency of intravenous drug consumption associated with crack pipe distribution [15]. In spite of these positive benefits, programs to distribute crack pipes to individuals who use drugs are controversial and many programs in Canada have faced political and community resistance which has limited their potential reach and impact [16,17]. In Vancouver, Canada, the British Columbia Centre for Disease Control and the local health authority have distributed a limited number of low or no cost Pyrex crack pipes, and unlimited plastic mouthpieces and wooden push sticks [10,14]. However, these distribution efforts have been largely focused on adult drug use epicentre neighbourhoods, such as Vancouver’s Downtown Eastside [18], and not neighbourhoods where street-involved youth are known to congregate, such as the Downtown South of Vancouver [19].
Given the health-related harms associated with sharing crack cocaine pipes, and lack of data about this practice among groups of young drug-users, the current study investigates the frequency of crack pipe sharing and associated risk factors among a cohort of street-involved youth who use illicit drugs in Vancouver. We hypothesise that the youth in our sample will have a high prevalence of crack pipe sharing, and individual and structural level factors will be associated with this risky practice.
METHODS
Data for this study was obtained from the At-Risk Youth Study (ARYS), a prospective cohort study of street-involved youth in Vancouver, Canada. The cohort began in 2005 and has been described in detail previously [20]. In brief, snowball sampling and extensive street-based outreach methods were employed. To be eligible, participants at recruitment had to be aged 14–26 years, use illicit drugs other than marijuana in the past 30 days, provide written informed consent, and be considered “street-involved”. In this study, “street-involved” was defined as being recently homeless, having used services designated for street-youth, or heavily participating in street-life through buying and selling drugs and/or sex and engaging in crime [20–23]. At enrolment, and on a bi-annual basis, participants completed an interviewer-administered questionnaire that included questions related to demographic information and drug use patterns. Participants also met with a study nurse and provided a blood sample for serologic testing. At each study visit, participants were provided with a stipend ($20 CDN) for their time. The University of British Columbia’s Research Ethics Board has approved the study, and it conforms to the provisions of the Declaration of Helsinki.
For the present analyses, ARYS participants were eligible if they completed a survey between May 2006 and May 2012 and were considered at-risk for sharing crack pipes. Specifically, study visits with a report of crack smoking in the past six months were included in our analyses, and study visits with no report of crack smoking in the past six months were excluded. Our main outcome of interest was crack pipe sharing, defined as responding ‘yes’ to the following question: “In the last six months, have you borrowed or lent a crack cocaine pipe/mouthpiece?” Those reporting sharing a crack cocaine pipe were compared with those who indicated that they had not shared a crack cocaine pipe in the last six months. Participants were also asked about the frequency of sharing pipes and mouthpieces over a 6-month period (never, once, 2–5 times, 6–10 times, 11–100 times or over 100 times). In addition, reports of initiating, increasing, decreasing, and terminating crack pipe sharing were assessed. Participants who indicated that they had not shared crack pipes at baseline, but then reported sharing at some point over study follow-up were considered to have “initiated” crack pipe sharing. An increase in crack pipe sharing was defined as an increase in the frequency of pipe sharing over two consecutive study visits. Conversely, a decrease in crack pipe sharing was defined as less frequent crack pipe sharing over two consecutive study visits. Crack pipe sharing cessation was defined as a report of crack pipe sharing at one study visit, and then two subsequent consecutive study visits with no reports of crack pipe sharing.
Participants were also asked about who their crack pipe sharing partners were (regular sex partner, casual sex partner, close friend, casual friend/acquaintance, family member, an unknown person, inmate or other), where they obtained crack pipes (new pipes from the street, used pipes from the street, new pipes from a corner store, any person, homemade, public health outreach service, exchange site, health clinic, Insite or other) and whether they experienced any physical or mental health issues as a result of their crack use (burns on lips, mouth sores, cuts or sores on fingers, raw throat, coughing blood, coughing fits, breathing problems, irritability, paranoia, psychosis, weight loss, sleep problems or other) in the past six months.
To identify factors associated with sharing a crack cocaine pipe, we considered a number of potential explanatory variables of interest including the following socio-demographic factors: gender (female vs. male); age (per year older); and ethnicity (Caucasian vs. other). We also considered a number of time-variant factors including: being in a stable relationship, defined as being legally married, common law, or having a regular partner (yes vs. no); homelessness, defined as having no fixed address, sleeping on the street, couch surfing, or staying in a shelter or hostel (yes vs. no); regular employment, defined as having at least one source of income from a regular job (distinguished from temporary, casual, and non-legal forms of income generation by separate response options) (yes vs. no); and ever dropping out of high school or elementary school (yes vs. no). Drug use variables were also time-variant and included: heavy alcohol use, defined as having more than four drinks per day (yes vs. no); daily crack cocaine smoking (yes vs. no); daily non-injection heroin use (yes vs. no); daily non-injection cocaine use (yes vs. no); daily non-injection crystal methamphetamine use (yes vs. no); any injection drug use (yes vs. no); binge drug use, defined as a period of using drugs more often than usual (yes vs. no); and smoking crack cocaine in public (yes vs. no). Other time-variant variables considered included: having encounters with police, defined as being stopped, searched or detained by police (yes vs. no); difficulty accessing crack pipes, defined as “finding it hard to get new pipes when you need them” (yes vs. no); Hepatitis C infection, defined as testing positive for Hepatitis C at baseline or testing positive over study follow-up (yes vs. no); and engaging in unprotected sex, defined as vaginal or anal sex without always using a condom (yes vs. no). All drug use and behavioural variables refer to activities in the past six months.
To model factors associated with sharing crack cocaine pipes over time and analyse longitudinal correlated within-subject data [24,25], a generalised estimating equation (GEE) was used. The GEE uses each observation as the unit of analysis and examines factors that are correlated with times when crack pipe sharing did and did not occur within individuals and between individuals. Consequently, the GEE analyses the clustering of observations for each participant, and also compares these clusters to those of other participants. This approach has been used in another cohort study of drug-using youth [26], and is appropriate for longitudinal research that uses a repeated measure binary dependent variable. These methods provided standard errors adjusted by multiple observations per person using an exchangeable correlation structure. Therefore, data from every participant follow-up visit were considered in this analysis. Missing data were addressed through the GEE estimating mechanism which uses all available pairs method to encompass the missing data from dropouts or intermittent missing data. All non-missing pairs of data are used in the estimators of the working correlation parameters. As a first step, GEE bivariate analyses were used to determine factors associated with sharing crack cocaine pipes. To adjust for potential confounding variables and to identify factors that were independently associated with our outcome of interest, variables significant at the P <0.10 threshold in bivariate analyses were entered in a multivariate GEE model using a backwards model selection process. The model with the best overall fit was determined using the lowest quasilikelihood under the independence model criterion value [27]. All statistical analyses were performed using SAS software version 9.3 (SAS, Cary, NC). All P values are two sided.
RESULTS
Among 898 street-involved youth recruited into ARYS during the study period, 331 participants were excluded because they were not at-risk for sharing crack pipes (i.e. did not use crack cocaine in the previous six months at any study visit). The final analytic sample comprised of 567 participants, among whom 166 (29%) were female, 371 (65%) were of Caucasian ethnicity, and the median age was 22 years (interquartile range [IQR] = 20–24). This sample of 567 participants were under study follow-up for a median number of 18 months (IQR = 11–30) and completed a median of two study visits (IQR = 1–3). Each of the 567 participants reported smoking crack cocaine at some point over study follow-up and 497 (88%) reported sharing crack pipes at some point during the study period. Over the entire study period this sample contributed 2125 observations and 1288 (61%) included a report of crack cocaine smoking and were therefore included in this analysis. Among these eligible observations, 961 (75%) included a report of crack pipe sharing.
Analyses of changes in crack pipe sharing over the study period among the 567 crack smoking participants found that 466 (82%) participants shared crack pipes at baseline, 31 (5%) participants initiated crack pipe sharing over study follow-up, and 70 (12%) did not share crack pipes at any point during the study. Among the 215 participants with at least three study visits, 22 (10%) increased their frequency of crack pipe sharing over follow-up, 65 (30%) decreased their frequency, and 39 (18%) ceased sharing crack pipes. Figure 1 displays: reported frequencies of crack pipe sharing; the individuals who youth report sharing crack pipes with; and the locations where crack pipes are acquired. These figures are based on 961 observations across all study visits that include a report of crack pipe sharing.
Figure 1.
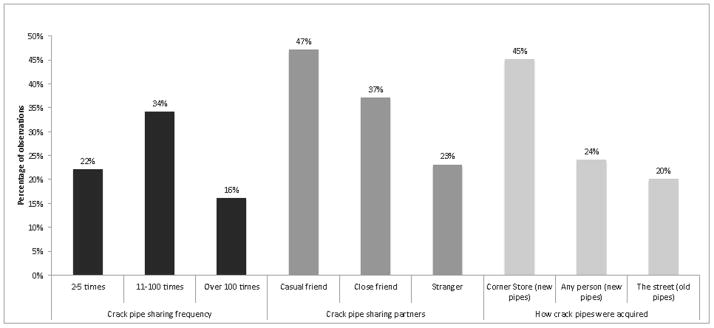
Crack pipe acquisition and sharing patterns among 961 study observations.
Experiencing health problems due to crack cocaine use was reported in 47% of study observations over the study period (n = 603). Among the 603 observations that included reports of health problems among crack cocaine smokers, paranoia was the most frequent health problem (63%, n = 380), followed by irritability (44%, n = 264), raw throat (42%, n = 251), coughing fits (38%, n = 227), sores on fingers (38%, n = 230), breathing problems (34%, n = 208) and psychosis (34%, n = 206).
The prevalence of our covariates across the full study period, along with the bivariate and multivariate GEE analyses of socio-demographic, behavioural, and other risk variables associated with sharing crack cocaine pipes are presented in Table 1.
Table 1.
Prevalence of characteristics, and bivariate and multivariate GEE analysis of factors associated with crack pipe sharing among 567 participants who contributed 1,288 observations.
| Crack Pipe Sharing | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Characteristic | Yes (%) (n = 961)° | No (%) (n = 327)° | Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value |
| Age (per year older) | — | — | 0.96 (0.90 – 1.03) | 0.241 | ||
| Gender (female vs. male) | 273 (28.41) | 99 (30.28) | 0.98 (0.70 – 1.36) | 0.893 | ||
| Ethnicity (Caucasian vs. Other) | 618 (64.31) | 168 (51.38) | 1.54 (1.13 – 2.09) | 0.006 | 1.34 (0.98 – 1.83) | 0.070 |
| Stable relationship‡ | 298 (31.01) | 108 (33.03) | 0.93 (0.69 – 1.26) | 0.642 | ||
| Homelessness*‡ | 654 (68.05) | 162 (49.54) | 2.07 (1.60 – 2.69) | <0.001 | 1.87 (1.43 – 2.44) | <0.001 |
| Regular employment*‡ | 409 (42.56) | 115 (35.17) | 1.36 (1.03 – 1.80) | 0.030 | 1.53 (1.15 – 2.04) | 0.003 |
| School dropout‡ | 795 (82.73) | 253 (77.37) | 1.34 (0.92 – 1.96) | 0.126 | ||
| Heavy alcohol use*‡ | 122 (12.70) | 40 (12.23) | 1.01 (0.68 – 1.49) | 0.977 | ||
| Binge drug use*†‡ | 448 (46.62) | 139 (42.51) | 1.28 (0.98 – 1.67) | 0.070 | ||
| Daily crack smoking*†‡ | 313 (32.57) | 95 (29.05) | 1.32 (0.97 – 1.79) | 0.073 | 1.37 (1.01 – 1.85) | 0.043 |
| Daily heroin use*†‡ | 47 (4.89) | 19 (5.81) | 0.87 (0.45 – 1.68) | 0.684 | ||
| Daily cocaine use*†‡ | 23 (2.39) | 7 (2.14) | 1.37 (0.54 – 3.49) | 0.510 | ||
| Daily crystal meth use*†‡ | 92 (9.57) | 15 (4.59) | 2.04 (1.13 – 3.66) | 0.017 | 2.04 (1.11 – 3.75) | 0.022 |
| Any injection drug use*‡ | 332 (34.55) | 88 (26.91) | 1.34 (0.98 – 1.84) | 0.070 | 1.30 (0.95 – 1.79) | 0.103 |
| Public crack smoking*‡ | 607 (63.16) | 177 (54.13) | 1.18 (0.91 – 1.53) | 0.201 | ||
| Encounters with police*‡ | 305 (31.74) | 74 (22.63) | 1.53 (1.10 – 2.13) | 0.011 | 1.42 (1.01 – 1.99) | 0.043 |
| Difficulty accessing pipes*‡ | 241 (25.08) | 62 (18.96) | 1.60 (1.12 – 2.26) | 0.009 | 1.58 (1.13 – 2.20) | 0.007 |
| Hepatitis C infection*‡ | 160 (16.65) | 54 (16.51) | 0.87 (0.59 – 1.29) | 0.496 | ||
| Unprotected sex*‡ | 546 (56.82) | 118 (36.09) | 2.06 (1.56 – 2.73) | <0.001 | 1.95 (1.47 – 2.58) | <0.001 |
°Refers to number of observations
Refers to activities in the last six months
Refers to non-injection drug use
Comparison is yes vs. no
CI, confidence interval; GEE, generalised estimating equation.
DISCUSSION
Our results demonstrate a high rate of crack cocaine pipe sharing, with 75% of observations from crack cocaine smoking youth including reports of engaging in pipe sharing. Although participants were more likely to decrease the frequency of pipe sharing over the study period, 16% (n = 155) of observations of pipe sharing indicated that individuals engaged in this behaviour over 100 times in the last six months which suggests this risk behaviour is widespread among vulnerable youth. Indeed, the prevalence of crack pipe sharing in this study is much higher than among drug-using adults, which has previously been reported at 37–47% [14,15] vs. 88% among this sample. Similar to adults [14], youth in our sample who experienced difficulty accessing crack pipes were significantly more likely to share crack pipes. These results point to a critical gap in public health services for street-involved youth, and suggest that the limited availability of free or low cost crack pipes to this sample may be contributing to the prevalence of this risk behaviour.
Only 8% of all study observations indicated that participants in this study acquired their crack cocaine pipes from some type of health service, which is consistent with previous research that found a similar low rate of acquiring crack pipes through a health service and higher rates of acquiring pipes through corner stores among adults [14]. Although corner stores provide a means for crack users to acquire new pipes, these stores typically sell inexpensive low-quality pipes which have been found to facilitate health-related harms such as oral burns [28,29], and are more likely to fracture and consequently cut users with the shards; Pyrex pipes distributed by health programs are more durable and safer to use [30]. The absence of formal crack pipe distribution programs may contribute to youth continuing to use pipes that are more likely to lead to health-related harms and perpetuates the lack of availability of these pipes, which is particularly concerning since our results show a positive association between having difficulty obtaining crack pipes and sharing them. Collectively, our findings suggest missed opportunities to engage youth with public health services, and given that 57% of youth reported health problems associated with crack use, better linkages between youth and health services are critical. This aligns with previous studies that suggest that increasing the availability of crack pipes through public health services is associated with important benefits, such as reduced crack pipe sharing and drug injecting frequency, and increased contact with public health services [15,31]. Indeed, distributing safer crack kits has previously been suggested as one mechanism for connecting those who smoke crack and health professionals [10], and targeting youth may achieve this in addition to promoting safer smoking practices. Furthermore, engagement in public health programs has been linked with improvements in peripheral health behaviours such as condom use [32], and also provides an additional opportunity for healthcare professionals to facilitate entry into addiction treatment and other health and social support services [33,34]. These linkages are particularly important since youth in our study who reported having regular employment were significantly more likely to share crack pipes, suggesting that employment in itself is not enough to reduce risk behaviours. Given these findings, crack pipe distribution programs in this setting may also serve to facilitate access to and uptake of health services and sexually transmitted infection screening. It is also noteworthy that among adults in this study setting, smoking crack cocaine has been linked to HIV incidence [10], further highlighting the importance of linking youth who smoke crack cocaine with the public health system. Although public health officials may be hesitant to implement crack pipe distribution programs aimed at young people who use drugs, such a program may provide critical links between public health services and street-involved youth, similar to the way that needle exchange programs and supervised injection facilities have been able to engage people who use injection drugs with health systems [35–38].
This study also found that homelessness was significantly associated with an increased likelihood of crack pipe sharing. Prior studies in this setting have demonstrated that structural factors, such as a lack of stable housing, are associated with high risk drug use and sexual behaviours among youth [39–42], suggesting that addressing the housing needs of this vulnerable group may lead to a reduction in risky drug use practices such as crack pipe sharing. The ‘Housing First’ model of service is well-suited to provide street-involved youth who use illicit drugs with safe, stable housing environments that may serve to reduce engagement in risky drug use practices [43–45].
Our finding that encounters with police are associated with crack pipe sharing is of concern. Prior research in our study setting found that police commonly confiscate youths’ drug paraphernalia without arresting them [46], and this practice of confiscation has been shown to increase the likelihood of sharing others’ crack cocaine pipes and syringes [30,47,48]. Past research also suggests that fear of being identified as a drug user can deter individuals from carrying sterile drug use equipment and engaging with harm reduction programs [49–51]. Given these findings, efforts should be made to develop policing practices that are more compatible with public health objectives [52,53]. Indeed, law enforcement personnel are able to encourage safe drug-using practices among illicit drug users, as police in Vancouver’s Downtown Eastside refer individuals who are publicly injecting drugs to Insite, a medically supervised injection facility [54].
There are several limitations to this study. First, the ARYS cohort is a community-recruited non-randomised sample of at-risk and street-involved youth in Vancouver, and therefore the generalisability of this study may be limited. However, the demographics of the sample are consistent with other samples of street-involved youth in Vancouver [55,56]. Second, our findings are also subject to response biases as a limitation of using self-report surveys [57]. Although previous research has found that self-reporting among drug-using populations is generally congruent with actual behaviour [58–60], we expect that any response biases from participants in this study would underestimate the prevalence of some risk behaviours and therefore bias our results towards the null. Third, due to limitations of the survey instrument, it is unclear whether participants shared a crack pipe but used their own mouthpiece, which is less risky.
Our study indicates that crack pipe sharing is common among street-involved youth who smoke crack in Vancouver, and that youth who had difficulty accessing crack pipes as well as those with markers of vulnerability and risk including homelessness, high intensity drug use, and unprotected sex were more likely to engage in this risky practice. It was also found that only 5% of study participants obtained clean crack pipes from health care centres yet 57% report experiencing health problems associated with crack smoking. This highlights a missed opportunity to connect health professionals with high-risk youth. Targeted interventions to facilitate access to crack pipes via public health services should be explored to better serve the health needs of vulnerable street-involved youth.
Acknowledgments
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. We would specifically like to thank Cody Callon, Deborah Graham, Peter Vann, Steve Kain, Tricia Collingham, and Carmen Rock for their research and administrative assistance. The study was supported by the US National Institutes of Health (R01DA021525) and the Canadian Institutes of Health Research (MOP–102742). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr Evan Wood. Dr Kora DeBeck is supported by a MSFHR/St. Paul’s Hospital Foundation-Providence Health Care Career Scholar Award. Funding sources had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Institution where work was carried out: British Columbia Centre for Excellence in HIV/AIDS, Vancouver, Canada
References
- 1.Public Health Agency of Canada. Street Youth in Canada: Findings from Enhanced Surveillance of Canadian Street Youth, 1999–2003. Ottawa: Government of Canada; 2006. [Google Scholar]
- 2.Clatts MC, Davis WR, Sotheran JL, Atillasoy A. Correlates and distribution of HIV risk behaviors among homeless youths in New York City: implications for prevention and policy. Child Welfare. 1998;77:195–207. [PubMed] [Google Scholar]
- 3.Haley N, Leclerc P, Lemire N, Boivin J, Frappier J, Claessens C. Prevalence of HIV infection and risk behaviours among Montreal street youth. Int J STD AIDS. 2000;11:241–7. doi: 10.1258/0956462001915778. [DOI] [PubMed] [Google Scholar]
- 4.Porter J, Bonilla L. Crack users’ cracked lips: an additional HIV risk factor. Am J Public Health. 1993;83:1490–1. doi: 10.2105/ajph.83.10.1490-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faruque S, Edlin BR, McCoy CB, Word CO, Larsen SA, Schmid DS, et al. Crack Cocaine smoking and oral sores in three inner-city neighborhoods. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13:87–92. doi: 10.1097/00042560-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Wilson T, DeHovitz JA. STDs, HIV, and crack cocaine: a review. AIDS Patient Care STDS. 1997;11:62–6. doi: 10.1089/apc.1997.11.62. [DOI] [PubMed] [Google Scholar]
- 7.Scheinmann R, Hagan H, Lelutiu-Weinberger C, Stern R, Jarlais DCD, Flom PL, et al. Non-injection drug use and Hepatitis C Virus: A systematic review. Drug Alcohol Depend. 2007;89:1–12. doi: 10.1016/j.drugalcdep.2006.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Macías J, Palacios RB, Claro E, Vargas J, Vergara S, Mira JA, et al. High prevalence of hepatitis C virus infection among noninjecting drug users: association with sharing the inhalation implements of crack. Liver Int. 2008;28:781–6. doi: 10.1111/j.1478-3231.2008.01688.x. [DOI] [PubMed] [Google Scholar]
- 9.Edlin BR, Irwin KL, Faruque S, McCoy CB, Word C, Serrano Y, et al. Intersecting epidemics - crack cocaine use and HIV infection among inner-city young adults. N Engl J Med. 1994;331:1422–7. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- 10.DeBeck K, Kerr T, Li K, Fischer B, Buxton J, Montaner J, et al. Smoking of crack cocaine as a risk factor for HIV infection among people who use injection drugs. CMAJ. 2009;181:585–9. doi: 10.1503/cmaj.082054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansergh G, Shouse R, Marks G, Guzman R, Rader M, Buchbinder S, et al. Methamphetamine and sildenafil (Viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. Sexy Transm Infect. 2006;82:131–4. doi: 10.1136/sti.2005.017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quirk A, Rhodes T, Stimson G. ‘Unsafe protected sex’: qualitative insights on measures of sexual risk. AIDS Care. 1998;10:105–14. doi: 10.1080/713612349. [DOI] [PubMed] [Google Scholar]
- 13.Zule WA, Costenbader E, Coomes CM, Meyer WJ, Riehman K, Poehlman J, et al. Stimulant use and sexual risk behaviors for HIV in rural North Carolina. J Rural Health. 2007;23(s1):73–8. doi: 10.1111/j.1748-0361.2007.00127.x. [DOI] [PubMed] [Google Scholar]
- 14.Ti L, Buxton J, Wood E, Zhang R, Montaner J, Kerr T. Difficulty accessing crack pipes and crack pipe sharing among people who use drugs in Vancouver, Canada. Subst Abuse Treat Prev Policy. 2011;6:34. doi: 10.1186/1747-597X-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leonard L, DeRubeis E, Pelude L, Medd E, Birkett N, Seto J. “I inject less as I have easier access to pipes”: injecting, and sharing of crack-smoking materials, decline as safer crack-smoking resources are distributed. Int J Drug Policy. 2008;19:255–64. doi: 10.1016/j.drugpo.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Dormer D. Province shuts down free crack pipe program. Calgary Sun. 2011 [Google Scholar]
- 17.Keller J. Vancouver to launch clean crack-pipe distribution project. The Globe and Mail. 2012 [Google Scholar]
- 18.Olivier C. Vancouver health body begins free crack pipe program for addicts. National Post. 2011 [Google Scholar]
- 19.Fast D, Shoveller J, Shannon K, Kerr T. Safety and danger in downtown Vancouver: understandings of place among young people entrenched in an urban drug scene. Health Place. 2010;16:51–60. doi: 10.1016/j.healthplace.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: the ARYS study. Harm Reduct J. 2006;3:18. doi: 10.1186/1477-7517-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall BD. The contextual determinants of sexually transmissible infections among street-involved youth in North America. Cult Health Sex. 2008;10:787–99. doi: 10.1080/13691050802295719. [DOI] [PubMed] [Google Scholar]
- 22.Roy É, Haley N, Leclerc P, Sochanski B, Boudreau J-F, Boivin J-F. Mortality in a cohort of street youth in Montreal. JAMA. 2004;292:569–74. doi: 10.1001/jama.292.5.569. [DOI] [PubMed] [Google Scholar]
- 23.DeMatteo D, Major C, Block B, Coates R, Fearon M, Goldberg E, et al. Toronto street youth and HIV/AIDS: prevalence, demographics, and risks. J Adolesc Health. 1999;25:358–66. doi: 10.1016/s1054-139x(99)00059-2. [DOI] [PubMed] [Google Scholar]
- 24.Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organizational Research Methods. 2004;7:127–50. [Google Scholar]
- 25.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–75. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 26.Roy É, Boudreau J-F, Leclerc P, Boivin J-F, Godin G. Trends in injection drug use behaviors over 10 years among street youth. Drug Alcohol Depend. 2007;89:170–5. doi: 10.1016/j.drugalcdep.2006.12.025. [DOI] [PubMed] [Google Scholar]
- 27.Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001;57:120–5. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- 28.Haydon E, Fischer B. Crack use as a public health problem in Canada. Can J Public Health. 2005;9:185–8. doi: 10.1007/BF03403687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fischer B, Powis J, Cruz MF, Rudzinski K, Rehm Hepatitis C virus transmission among oral crack users: viral detection on crack paraphernalia. Eur J Gastroenterol Hepatol. 2008;20:29–32. doi: 10.1097/MEG.0b013e3282f16a8c. [DOI] [PubMed] [Google Scholar]
- 30.Ivsins A, Roth E, Nakamura N, Krajden M, Fischer B. Uptake, benefits of and barriers to safer crack use kit (SCUK) distribution programmes in Victoria, Canada - A qualitative exploration. Int J Drug Policy. 2011;22:292–300. doi: 10.1016/j.drugpo.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Boyd S, Johnson JL, Moffat B. Opportunities to learn and barriers to change: crack cocaine use in the Downtown Eastside of Vancouver. Harm Reduct J. 2008;5:34. doi: 10.1186/1477-7517-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marshall BD, Wood E, Zhang R, Tyndall MW, Montaner JS, Kerr T. Condom use among injection drug users accessing a supervised injecting facility. Sex Transm Infect. 2009;85:121–6. doi: 10.1136/sti.2008.032524. [DOI] [PubMed] [Google Scholar]
- 33.Samet JH, Friedmann P, Saitz R. Benefits of linking primary medical care and substance abuse services: Patient, provider, and societal perspectives. Arch Intern Med. 2001;161:85–91. doi: 10.1001/archinte.161.1.85. [DOI] [PubMed] [Google Scholar]
- 34.Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med. 2003;138:256–61. doi: 10.7326/0003-4819-138-3-200302040-00034. [DOI] [PubMed] [Google Scholar]
- 35.DeBeck K, Kerr T, Bird L, Zhang R, Marsh D, Tyndall M, et al. Injection drug use cessation and use of North America’s first medically supervised safer injecting facility. Drug Alcohol Depend. 2011;113:172–6. doi: 10.1016/j.drugalcdep.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wood E, Tyndall MW, Zhang R, Montaner JS, Kerr T. Rate of detoxification service use and its impact among a cohort of supervised injecting facility users. Addiction (Abingdon, England) 2007;102:916–9. doi: 10.1111/j.1360-0443.2007.01818.x. [DOI] [PubMed] [Google Scholar]
- 37.Strathdee SA, Celentano DD, Shah N, Lyles C, Stambolis VA, Macalino G, et al. Needle-exchange attendance and health care utilization promote entry into detoxification. J Urban Health. 1999;76:448–60. doi: 10.1007/BF02351502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abuse Treat. 2000;19:247–52. doi: 10.1016/s0740-5472(00)00104-5. [DOI] [PubMed] [Google Scholar]
- 39.Feng C, Debeck K, Kerr T, Mathias S, Montaner JS, Wood E. Homelessness independently predicts injection drug use initiation among street-involved youth in a Canadian setting. J Adolesc Health. 2012;52:499–501. doi: 10.1016/j.jadohealth.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marshall BD, Kerr T, Shoveller JA, Patterson TL, Buxton JA, Wood E. Homelessness and unstable housing associated with an increased risk of HIV and STI transmission among street-involved youth. Health Place. 2009;15:753–60. doi: 10.1016/j.healthplace.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weir BW, Bard RS, O’Brien K, Casciato CJ, Stark MJ. Uncovering patterns of HIV risk through multiple housing measures. AIDS Behav. 2007;11(6 Suppl):31–44. doi: 10.1007/s10461-007-9284-x. [DOI] [PubMed] [Google Scholar]
- 42.Weber A, Boivin J-F, Blais L, Haley N, Roy É. HIV risk profile and prostitution among female street youths. J Urban Health. 2002;79:525–35. doi: 10.1093/jurban/79.4.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Padgett DK, Stanhope V, Henwood BF, Stefancic A. Substance use outcomes among homeless clients with serious mental illness: Comparing Housing First with Treatment First programs. Community Ment Health J. 2011;47:227–32. doi: 10.1007/s10597-009-9283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gulcur L, Stefancic A, Shinn M, Tsemberis S, Fischer SN. Housing, hospitalization, and cost outcomes for homeless individuals with psychiatric disabilities participating in continuum of care and housing first programmes. Journal of Community & Applied Social Psychology. 2003;13:171–86. [Google Scholar]
- 45.Gurstein P, Small D. From housing to home: reflexive management for those deemed hard to house. Housing Studies. 2005;20:717–35. [Google Scholar]
- 46.Ti L, Wood E, Shannon K, Feng C, Kerr T. Police confrontations among street-involved youth in a Canadian setting. Int J Drug Policy. 2013;24:46–51. doi: 10.1016/j.drugpo.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Werb D, Wood E, Small W, Strathdee SA, Li K, Montaner J, et al. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Int J Drug Policy. 2008;19:332–8. doi: 10.1016/j.drugpo.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Small W, Kerr T, Charette J, Schechter MT, Spittal PM. Impacts of intensified police activity on injection drug users: Evidence from an ethnographic investigation. Int J Drug Policy. 2006;17:85–95. [Google Scholar]
- 49.Aitken C, Moore D, Higgs P, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. Int J Drug Policy. 2002;13:193–202. [Google Scholar]
- 50.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005;61:673–84. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 51.Maher L, Dixon D. Policing and public health: Law enforcement and harm minimization in a street-level drug market. British Journal of Criminology. 1999;39:488–512. [Google Scholar]
- 52.Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: A review of the evidence. Int J Drug Policy. 2005;16:210–20. [Google Scholar]
- 53.Wood E, Spittal PM, Small W, Kerr T, Li K, Hogg RS, et al. Displacement of Canada’s largest public illicit drug market in response to a police crackdown. CMAJ. 2004;170:1551–6. doi: 10.1503/cmaj.1031928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.DeBeck K, Wood E, Zhang R, Tyndall M, Montaner J, Kerr T. Police and public health partnerships: evidence from the evaluation of Vancouver’s supervised injection facility. Subst Abuse Treat Prev Policy. 2008;3:11. doi: 10.1186/1747-597X-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Miller CL, Strathdee SA, Kerr T, Li K, Wood E. Factors associated with early adolescent initiation into injection drug use: implications for intervention programs. J Adolesc Health. 2006;38:462–4. doi: 10.1016/j.jadohealth.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 56.Ochnio JJ, Patrick D, Ho M, Talling DN, Dobson SR. Past infection with hepatitis A virus among Vancouver street youth, injection drug users and men who have sex with men: Implications for vaccination programs. CMAJ. 2001;165:293–7. [PMC free article] [PubMed] [Google Scholar]
- 57.Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J Appl Psychol. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 58.Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. Am J Epidemiol. 1995;141:575–80. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- 59.Darke S. Self-report among injecting drug users: A review. Drug Alcohol Depend. 1998;51:253–63. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- 60.Rosenbaum JE. Truth or Consequences: The Intertemporal Consistency of Adolescent Self-report on the Youth Risk Behavior Survey. Am J Epidemiol. 2009;169:1388–97. doi: 10.1093/aje/kwp049. [DOI] [PMC free article] [PubMed] [Google Scholar]


