Abstract
The aim of the present study was to perform a systematic review of the literature on the effects of low-level laser therapy in the treatment of TMD, and to analyze the use of different assessment tools. [Subjects and Methods] Searches were carried out of the BIREME, MEDLINE, PubMed and SciELO electronic databases by two independent researchers for papers published in English and Portuguese using the terms: “temporomandibular joint laser therapy” and “TMJ laser treatment”. [Results] Following the application of the eligibility criteria, 11 papers were selected for in-depth analysis. The papers analyzed exhibited considerable methodological differences, especially with regard to the number of sessions, anatomic site and duration of low-level laser therapy irradiation, as well as irradiation parameters, diagnostic criteria and assessment tools. [Conclusion] Further studies are needed, especially randomized clinical trials, to establish the exact dose and ideal parameters for low-level laser therapy and define the best assessment tools in this promising field of research that may benefit individuals with signs and symptoms of TMD.
Key words: Temporomandibular joint disorder, Electromyography, Laser
Introduction
Temporomandibular (TMD) disorder refers to a set of clinical conditions involving the masticatory muscles, temporomandibular joint (TMJ) and associated structures1). Pain is one of the most common and limiting clinical manifestations of this disorder2,3,4) and can compromise quality of life5, 6), sleep7, 8), and psychological aspects, leading to anxiety, stress and even depression. The multifactor etiology of TMD requires a multidisciplinary team of health professionals9), including a physiotherapist. A number of studies have addressed physical therapy modalities for the treatment of TMD, such as electrotherapy10, 11), laser therapy12, 13) and manual therapy14,15,16).
Low-level laser therapy (LLLT) has been widely used in the health field for therapeutic purposes and biostimulation, due to its characteristics of low-intensity energy, and wavelengths capable of penetrating tissues and exerting an influence on the synthesis, release and metabolism of numerous signaling substances involved in analgesia17, 18). Besides these neuro-pharmacological effects, there is evidence that LLLT leads to reductions in the inflammatory process, C-fiber activity, and the excitability of the nervous system, as well as an increase in blood circulation19, 20).
The present systematic review of the literature was motivated by the wide diversity of information on LLLT in the treatment of TMDs, the variety of application parameters and the different assessment tools used in different studies. Systematic reviews are highly valued studies that provide evidence that can contribute to the establishment of guidelines and enhance the quality of clinical research21). The present review was carried out to determine the different types of experimental procedures used to study the effects of LLLT in the treatment of TMD, and distinguish which studies provide evidence of the benefits of this form of therapy, as well as to identify and analyze the different assessment tools employed, to offer health professionals in this field a better understanding of the technique.
Subjects and Methods
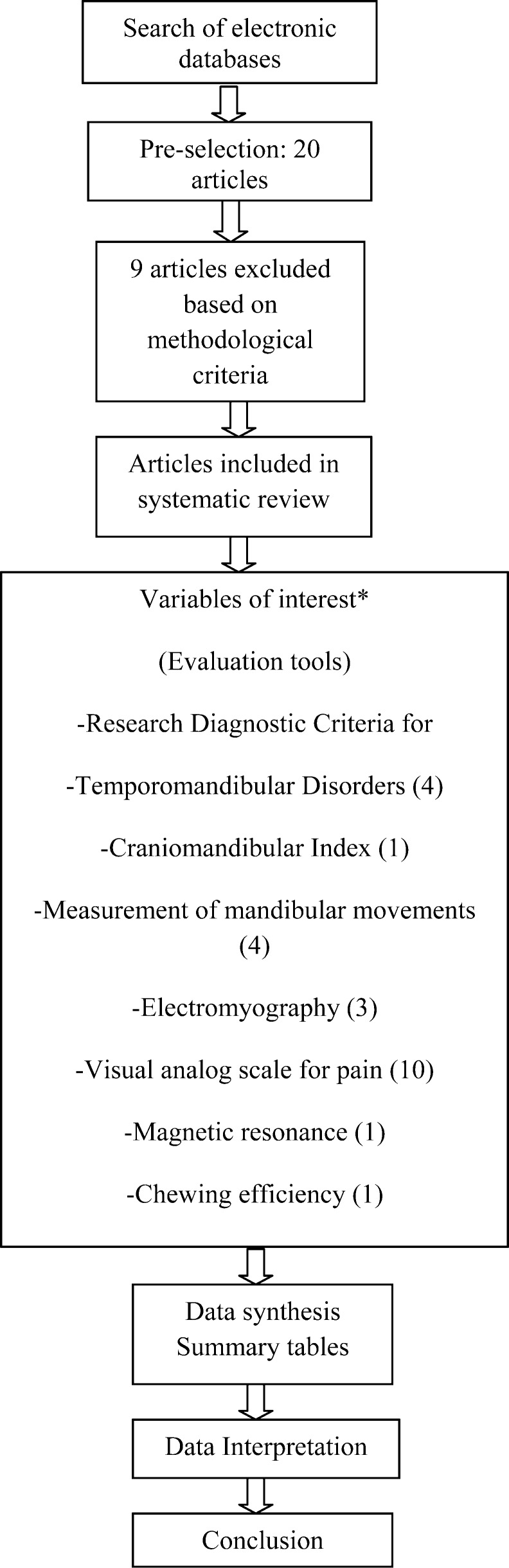
Searches were carried out of the BIREME, MEDLINE, PubMed and SciELO electronic databases by two independent researchers for papers published in English and Portuguese during the period from 2008 to 2013. The searches began on October 1st and ended on December 20th, 2013. The search terms used were “temporomandibular joint laser therapy” and “TMJ laser treatment”. An overview of the systematic review process is presented in Fig. 1.
Fig. 1.
Articles included in this review *The sum of articles in each category totals more than the number of articles included in the review due to the fact that some studies reported more than one outcome.
Methods
Clinical trials published between 2008 and 2013 that investigated the effect of LLLT in the treatment of TMD were included in this review. Thus, the findings of the most recent studies are presented, taking into consideration the use of LLLT in clinical practice and different evaluation methods. Each study needed to describe the type of laser, application time, administration parameters and assessment tools in order to allow the identification of the different protocols and compare the respective findings. Papers that failed to meet these criteria and reviews of the literature were excluded from the initial analysis (Fig. 1).
The Physiotherapy Evidence Database (PEDro) scale, which is based on the Delphi list, was used to evaluate the methodological quality of the papers. Articles with higher levels of clinical evidence were selected using this scale, the reliability of which has been empirically supported. A total score of up to 10 points was attributed to each paper based on the total number of criteria met22).
Two researchers who had undergone training in the use of the PEDro scale performed the reading and scoring of the papers. Neither researcher had knowledge of the scores given by the other. Agreement between the two researchers was then analyzed. In cases of disagreement, the papers were read again and the final score was determined by consensus.
A plus symbol (+) was placed on the chart for every criterion met and a minus symbol (−) was used when a criterion was not met. A question mark (?) indicated the non-scoring of a criterion due to a lack of certainty regarding whether the criterion was met. The final score was determined by summing the number of criteria met, excluding the first criterion, which is not considered in the scoring process. Papers with a final score of 4 or more points were placed in tables with descriptions of their respective variables analyzed and outcomes.
RESULTS
After the search of BIREME, MEDLINE, PubMed and SciELO electronic databases and the application of the eligibility criteria, 11 studies were selected for analysis (Tables 1 and 2). Graph 1 shows the scores for each role in the PEDro scale. The scores range from 4 to 7 points.
Table 1. Phototherapy parameters in randomized controlled clinical trials.
| Author/year of publication |
No of subjects |
Sex and age |
Type of laser and manufacturer |
Energy density (ED) | Power density (PD) | Application time |
Application sites |
Frequency and number of sessions |
|---|---|---|---|---|---|---|---|---|
| Venezian et al.31) | 48 | 5 men/43 women age 18–60 (mean 41.58) |
AsGaAl/Twin laser – MM Optics/780 nm |
25 J/cm² and 60 J/cm² of dose | 50 mW and 60 mW |
20 and 40 s | Muscles: 3 points on masseter and 1 point on temporal |
8 sessions; 2x/week for 4 weeks |
| Shirani et al.34) | 16 | 12 women/4 men, age 16–37 years (mean 23.8) |
InGaAlP/AZOR- 2K/660 nm and AsGa/AZOR-2K/890 nm |
6.2 J/cm² and 1 J/cm² | 17.3 mW and 9.8 mW |
360 s; 600 s | Trigger points of masticatory muscles |
6 sessions: 2x/week for 3 weeks |
| Emshoff et al.35) | 52 | Age 18–58 years (mean 42.9) |
HeNe/Helbo Medizintechnik/ 632.8 nm |
1.5 J/cm² | 30 mw | 120 s | Approx. 1 cm in front of joint |
20 sessions: 2 to 3x/ weeks for 8 weeks |
| Carvalho et al.36) | 74 | 15 men/59 women, age 46.3 ± 14.6 years |
? /Biowave, Kondortech/660 nm + ? /Twin Flex, MM Optics/780 nm, 790 nm or 830 nm |
1 to 2 J/cm² 14.2±6.8 J/cm² mean dose per session 8 J/cm2) | 30/40 mW; 40/50 mw | Indicated by equipment based on ED and PD. | 4 points near TMJ | 12 sessions: 2x/weeks for 6 weeks |
| Salmos-Brito et al.37) | 58 | 8 men/50 women, age 19–86 years | AsGa (Thera Laser, DMC) 830 nm | 40 mW | 60 s | 5 points around painful TMJ and condyle | 12 sessions: 2x/weeks for 6 weeks | |
| Marini et al.41) | 99 | 74 women/ 25 men, age 15–50 years | AsGa (LUMIX 2 HFPL Fisioline) 910 nm, pulse time < 200 ns and 50 kHz | ? | 400 mW (mean power) | 3 steps: 20 kHz for 10 min; 18 kHz for 5 min; 16 kWz for 5min | In right and left TMJ | 10 consecutive days (5 d/wk) |
| Da Cunha LA et al.38) | 40 | 39 women/1 man, age 20–68 years | AsGa (laser – Biolux, Bio-Art, São Carlos, SP, Brazil) 830 nm | 4 J/point | 500 mW | 20 seconds on each area | Directly over painful area | 1 x per week for 4 consecutive weeks |
| Frare et al.39) | 18 | Women, mean age 27 ± 7 years | GaAs laser, 904 nm (Laserplus), | 6 J/cm2 | 15 mW continuous | 16 s per point | Pre-auricular region and outer acoustic meatus | 2x per week for 4 weeks (8 sessions) |
| Hotta et al.32) | 10 | 9 women/1 man, mean age 35.3 years (15–67 years) | GaAs Twin Laser, MM Optics, São Carlos-SP, Brazil) 780 nm. | 35 J/cm2 | 70 mW | 20 s | Points employed in acupuncture | Once a week, 10 sessions |
| Shinozaki et al.33) | 13 | Women, 18–36 years | GaAs laser Bio-wave device (Kondortech) 790 nm. | 1.5 J/cm2 for TMJ, 2.5 J/cm2 for auriculo-temporal nerve, 3 J/cm2 for masseter | 40 mW | ? | TMJ, region of auriculo-temporal nerve and masseter | Single session |
| Carrasco et al.40) | 14 | ? | AsGaAl/Twin laser MM Optics/780 nm | Resulting in a dose of 105 J/cm² | 70 mW | 60 s | TMJ | 8 sessions: 2x/week for 4 weeks |
TMJ temporomandibular joint.
Table 2. Methods, assessment tools and outcomes of randomized controlled clinical trials.
| Author/year of publication | Aspect evaluated | Assessment tools | Evaluations | Outcomes | Pedro Score |
|---|---|---|---|---|---|
| Venezian et al.31 | Pain upon palpation, masseter and temporal muscle activity | RDC/TMD, VAS, EMG | Before, immediately after, and 30 days after treatment | No differences in EMG between groups, before and after treatment. Reduction in pain in laser group for all muscles palpated, but no statistically significant difference in comparison to placebo group. Reduction in pain lasted 30 days after end of treatment in laser group with 25 J/cm², but returned after 30 days in group with 60 J/cm². | 6 |
| Shirani et al.34 | Pain | VAS | Before and after 1 week, and 3 weeks of treatment | Reduction in pain in both groups, with laser proving more effective. One patient reported return of pain 1 month after end of treatment. | 6 |
| Emshoff et al.35 | Pain during muscle function | RDC/TMD, VAS | Before and after 2, 4, and 8 weeks of treatment | Reduction in pain in TMJ during jaw function in both groups. No statistically significant difference between groups. | 7 |
| Carvalho et al.36 | Pain | VAS | At the end of each of 12 sessions (comparisons only at end of treatment) | 64% of patients were asymptomatic or had improved after treatment. Combination of two wavelengths (red and infrared) achieved significant reduction in pain. | 4 |
| Salmos-Brito et al.37 | Pain, range of motion | RDC/TMD, VAS, digital ruler | Before first session and on second day after last session (12 sessions) | Significant improvements in pain intensity and maximal mouth opening after LLLT in groups with acute and chronic TMD. Greater improvements in group with acute TMD. | 6 |
| Da Cunha LA et al.38 | Pain, range of motion | Craniomandibular Index, VAS | Before first session and after last session (4 sessions) | Significant reduction in pain in both groups after treatment according to VAS scores (p < 0.05). No significant difference between groups regarding pain and symptoms of TMD according to craniomandibular index. | 7 |
| Frare et al.39 | Pain | RDC/TMD, clinical evaluation, VAS | Before and after therapy | Statistically significant reductions in VAS scores among sessions in treated group (p < 0.05). Significant reduction in VAS score between first and last session only in control group (p < 0.05). | 7 |
| Hotta et al.32 | Pain, range of motion, muscle activity | Mandibular range of motion, VAS, EMG | Before and after each treatment session | Statistically significant improvements in pain and muscle activity in masseter muscles in habitual occlusion after laser applications (p < 0.01), but no significant improvement in measures of mandibular movements (p = 0.05 + ¼). | 5 |
| Shinozaki et al.33 | Muscle activity | EMG | Before, immediately after, and 5 and 20 min after treatment | Reduction in EMG activity in masseter and temporal muscles in laser group. Laser therapy promoted significant relaxation of masseter muscles immediately after application. | 5 |
| Carrasco et al.40 | Pain, chewing efficiency | VAS, colorimetric method involving chewing capsule | After eighth application and 30 days after last application | Reduction in pain in laser group. Fewer symptoms and greater chewing efficiency after 8 sessions of laser therapy. | 5 |
| Marini et al.41 | Pain, range of motion | VAS, ruler, magnetic resonance | VAS: 2, 5, 10, and 15 days after treatment. Range of motion: after 15 days and 1 month of treatment. Magnetic resonance: before and after treatment | Significant reduction in pain in comparison to group using non-steroidal anti-inflammatory drugs. Magnetic resonance revealed disappearance of effusion in laser group. Mean measures of active and passive mouth opening and lateral excursion greater in laser group after treatment and 1 month later. | 5 |
RDC/TMD: Clinical Diagnostic Criteria for Temporomandibular Disorders, VAS: visual analog scale, EMG: electromyography
A number of assessment tools are described in the literature for the evaluation of TMD, including questionnaires23), patient history indices24, 25), clinical indices24, 26, 27), and diagnostic criteria2, 28). Each assessment tool has advantages, disadvantages, and limitations, as well as distinct applicability. Thus, clinicians and researchers need to be aware of the data obtained using each tool in order to employ it properly. Surface electromyography (EMG) is a valuable method for the characterization and diagnosis of individuals with orofacial and occlusal abnormalities29). This noninvasive tool allows the objective determination of muscle activity through electric signals with the muscle at rest or during contraction. In the investigation of TMD, surface EMG has been mainly used to evaluate the temporal and masseter muscles30). Moreover, a number of reliable tools are available for the quantification of pain intensity, such as the visual analog scale (VAS), which allows the comparison of subjective pain intensity, and monitoring the effects of treatment. An algometer is another tool used in the semi-quantitative measurement of pain that allows locating trigger points and quantifying changes in different pain syndromes.
Venezian et al.31) used the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD), and both the VAS and electromyography to perform evaluations prior to treatment, immediately after, and 30 days after LLLT. The authors found no significant difference in EMG activity before and after treatment. Hotta et al.32) also used EMG and found statistically significant improvements (p < 0.01) in both pain and activity of the masseter muscle in habitual occlusion following LLLT, but no significant improvement in mandibular movements using points employed in orofacial acupuncture. In contrast, Venezian et al.31) used three points on the masseter and one point on the temporal muscle, and Shinozaki et al.33) applied LLLT over the TMJ, region of the auriculotemporal nerve and masseter muscle in a single session. Both groups of researchers found a reduction in EMG activities of the masseter and temporal muscles.
Shirani et al.34), Emshoff et al.35) and Carvalho et al.36) only used the VAS in the evaluation and found a reduction in pain. However, the reduction was not significant in the study by Emshoff et al.35), who performed evaluations at baseline and after two, four and eight weeks covering a total of 20 treatment sessions. However, it should be pointed out that the LLLT was applied at a distance of 1 cm over the TMJ, differing from the other authors cited, who used trigger points of the masticatory muscles. Salmos-Brito et al.37) also used trigger points around the TMJ, employing the RDC/TMD for diagnosis and the VAS and a digital ruler for the evaluations, which is useful for the measurement of range of motion, and found significant differences in pain intensity and maximum mouth opening after treatment.
Da Cunha et al.38) employed the craniomandibular index and the VAS for evaluation and found a significant reduction in pain following treatment in both groups when using the VAS (p < 0.05), but no significant differences in pain or symptoms of TMD when using the craniomandibular index. This index was developed by Fricton et al.26) to allow the evaluation of signs and symptoms of TMD with greater precision. Frare et al.39) used different evaluations in the selection of cases, comparing a clinical evaluation using a chart based on Okeson, the screening questionnaire recommended by the American Academy of Orofacial Pain, and the VAS. Carrasco et al.40) employed the VAS and a colorimetric method involving the chewing of a capsule, and found that laser therapy led to a reduction in pain as well as enhanced chewing efficiency.
The LLLT application site was the treatment condition that most differed among the studies. LLLT was applied to the TMJ in five studies17, 35, 37, 39, 40), the masticatory muscles in three studies31, 34), both the TMJ and masticatory muscles in three studies33, 36, 38), and the points employed in acupuncture in one study32). Among the studies in which LLLT was applied to the TMJ, some papers reported positive results in comparison to a placebo group. Among the studies in which LLLT was applied to the masticatory muscles, two papers reported positive results34, 38). However, Venezian et al.31), who used three points on the masseter and one point on the temporal muscle, found a significant difference in VAS scores, but not in EMG. In a study of LLLT for both the TMJ and masticatory muscles, significant reductions were found in both pain and EMG activity after a single session33). The study by Emshoff et al.35), which received one of the highest PEDro scores from both assessors due to its excellent methodology, found a similar pain reduction effects in the laser therapy and placebo groups following LLLT over the TMJ, but the reduction in pain was not significant, which is in disagreement with results reported in other studies.
The number of applications differed considerably among the studies, ranging from a single application to 20 applications (2 to 3 application per week over 8 weeks). Emshoff et al.35) employed the greatest number of sessions, and found a reduction in pain in the TMJ during jaw function, but there was no significant difference between the LLLT and placebo groups. Shinozaki et al.33) employed a single session on the masticatory muscles and found a significant reduction in EMG activity in the masseter and temporal muscles.
The duration of each application varied from 16 seconds39) to 20 seconds31, 32, 38) and as much as 10 minutes17, 34). Based on the findings of these studies, it seems that an increase in duration does not lead to enhanced effectiveness when the LLLT is applied to the TMJ. However, positive results were achieved when the LLLT was applied to the masticatory muscles for 360 seconds or more. Moreover, the findings demonstrate that while positive results were reported after a single session, no study has demonstrated how long the effects of a single session last. In a study involving eight sessions of LLLT, Venezian et al.31) reported that the reduction in pain was maintained 30 days after the end of treatment.
Pain was assessed using the VAS, the number of trigger points or the craniomandibular index. Jaw function was assessed through the measure of maximum mouth opening, protrusion and lateral mandibular movements, joint sounds, chewing efficiency and muscle activity (EMG). Investigating the correlation between mandibular range of motion and pain, Salmos-Brito et al.37) and Marini et al.17) found improvements in both variables following treatment. Carrasco et al.40) found enhanced chewing efficiency and a greater reduction in pain in comparison to a placebo group. These findings indicate that pain intensity exerts a direct influence on jaw function. Further studies are needed on the treatment of TMD, as pain is the main symptom of this disorder10, 11, 15, 16). Moreover, muscle and/or joint impairment is prevalent among affected individuals41), which can have a significant impact on quality of life and activities of daily living, such as eating, speaking, yawning and smiling42).
The literature offers a wide variety of tools for the diagnosis and evaluation of TMD. The tool of choice should be based on a grounded judgment and the specific intentions of the researcher or clinician. The studies analyzed herein demonstrate the importance of a more objective evaluation involving EMG, magnetic resonance imaging, the measure of mandibular range of motion, etc., as well as other evaluations regarding the efficacy of treatment with the use of the VAS to enhance the credibility of LLLT treatment and guide clinical conduct.
DISCUSSION
As a disorder with a multifactor etiology, a number of modalities have been proposed for the treatment of signs and symptoms of TMD, such as bite plate usage, acupuncture, kinesiology, massage therapy, joint manipulation, drug therapy and LLLT11, 15, 16, 31, 43). LLLT has been studied since 1905, when Albert Einstein proposed the theory of stimulated emission. In 1960, this became reality with the first emitter (ruby), developed by Theodore Maiman44), and emitted a light with coherence, monochromaticity and a low degree of divergence.
According to Pinto et al.45), LLLT is comprised of electromagnetic waves (either visible or invisible) of low intensity energy and wavelengths capable of penetrating tissues and influencing the synthesis, release and metabolism of numerous signaling substances involved in analgesia17, 18). Since the publication of the first randomized clinical trial investigating the effects of LLLT on rheumatoid arthritis in the 1980s46), a number of positive effects have been reported in studies involving other musculoskeletal disorders. Despite the lack of clear scientific evidence regarding the action mechanisms of LLLT47, 48), theories have been put forth to explain the therapeutic effects capable of altering cell functions, such as reduction in bradykinin expression, edema, pain substances and inflammation time as well as increases in beta-endorphins and blood flow, the release of histamine and the promotion of muscle relaxation35, 37).
In the interpretation of the data, discrepancies are evident in the administration parameters, number of sessions, and application sites of LLLT. A wide array of diagnostic and assessment tools for TMD is described in the literature. The choice of the most appropriate tool should be based on the specific objectives of the researcher or clinician. However, the literature offers little evidence of local and systemic analgesia following the administration of LLLT using pressure algometry as the evaluation tool49).
The complexity of LLLT in the treatment of TMD and the lack of methodological quality in the clinical trials analyzed limits the indication of this physiotherapeutic modality17, 31,32,33,34,35,36,37,38,39,40). Thus, further investigations with an good study design and adequate methodology (better control of the variables and the assurance of reproducibility) are needed to identify the benefits of LLLT in the treatment of TMD.
LLLT is effective in the treatment of TMD, especially in the reduction of muscle pain. However, there is an evident lack of standardization in the parameters employed, which limits our ability to draw more definitive conclusions. The visual analog scale for pain and a clinical evaluation are the most widely used tools for the assessment of the effects of LLLT. Further studies are needed, especially randomized clinical trials, to establish the exact dose and ideal parameters for LLLT, and to define the best assessment tools in this promising field of therapy that appears to offer many benefits to individuals with signs and symptoms of TMD.
Conflict of competing interests
Professor Ernesto Cesar Pinto Leal-Junior receives research support from Multi Radiance Medical (Solon, OH, USA), a laser device manufacturer. Multi Radiance Medical had no role in the planning, study design, data collection and analysis, the decision to publish, or the preparation of this manuscript. The remaining authors declare that they have no conflict of interest.
REFERENCES
- 1.De Leeuw R: Orofacial pain: guidelines for assessment, diagnosis and management, 4th ed. The American Academy of Orofacial Pain. Chicago: Quintessence, 2008. [Google Scholar]
- 2.Truelove EL, Sommers EE, LeResche L, et al. : Clinical diagnostic criteria for TMD. New classification permits multiple diagnoses. J Am Dent Assoc, 1992, 123: 47–54. [DOI] [PubMed] [Google Scholar]
- 3.Orlando B, Manfredini D, Bosco M: Efficacy of physical therapy in the treatment of masticatory myofascial pain: a literature review. Minerva Stomatol, 2006, 55: 355–366. [PubMed] [Google Scholar]
- 4.Gonçalves DA, Dal Fabbro AL, Campos JA, et al. : Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain, 2010, 24: 270–278. [PubMed] [Google Scholar]
- 5.Moreno BG, Maluf SA, Marques AP, et al. : Clinical and quality-of-life assessment among women with temporomandibular disorder. Rev Bras Fisioter, 2009, 13: 210–214. [Google Scholar]
- 6.Karacayli U, Mumcu G, Cimilli H, et al. : The effects of chronic pain on oral health related quality of life in patients with anterior disc displacement with reduction. Community Dent Health, 2011, 28: 211–215. [PubMed] [Google Scholar]
- 7.Yatani H, Studts J, Cordova M, et al. : Comparison of sleep quality and clinical and psychologic characteristics in patients with temporomandibular disorders. J Orofac Pain, 2002, 16: 221–228. [PubMed] [Google Scholar]
- 8.Smith MT, Wickwire EM, Grace EG, et al. : Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep, 2009, 32: 779–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Issa JP, Silva MA, Silva AM: Disfunções temporomandibulares e suas implicações clínicas. Rev Dor, 2005, 6: 573–578. [Google Scholar]
- 10.Rodrigues-Bigaton D, Almeida AF, Berni KC, et al. : Use of different electrical stimulations for treating pain in women with temporomandibular disorders. Braz J Phys Ther, 2008, 12: 476–481. [Google Scholar]
- 11.Gomes NC, Berni-Schwarzenbeck KC, Packer AC, et al. : Effect of cathodal high-voltage electrical stimulation on pain in women with TMD. Rev Bras Fisioter, 2012, 16: 10–15. [PubMed] [Google Scholar]
- 12.Bjordal JM, Couppé C, Chow RT, et al. : A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother, 2003, 49: 107–116. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigues JH, Biasotto-Gonzalez DA, Bussadori SK, et al. : Signs and symptoms of temporomandibular disorders and their impact on psychosocial status in non-patient university student’s population. Physiother Res Int, 2012, 17: 21–28. [DOI] [PubMed] [Google Scholar]
- 14.McNeely ML, Armijo Olivo S, Magee DJ: A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther, 2006, 86: 710–725. [PubMed] [Google Scholar]
- 15.Arruda EE, Amaral AP, Politti F, et al. : Immediate effects of mandibular mobilization on static balance in individuals with temporomandibular disorder pilot study. Clin Exp Med Lett, 2012, 53: 165–169. [Google Scholar]
- 16.Amaral AP, Politti F, Hage YE, et al. : Immediate effect of nonspecific mandibular mobilization on postural control in subjects with temporomandibular disorder: a single-blind, randomized, controlled clinical trial. Braz J Phys Ther, 2013, 17: 121–127. [DOI] [PubMed] [Google Scholar]
- 17.Marini I, Gatto MR, Bonetti GA: Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain, 2010, 26: 611–616. [DOI] [PubMed] [Google Scholar]
- 18.Andrade TN, Frade JC: Estudo comparativo entre os efeitos de técnicas de terapia manuais isoladas e associadas á laserterapia de baixa potência sobre a dor em pacientes com disfunção temporomandibular. Rev Gaucha Odontol, 2008, 56: 287–295. [Google Scholar]
- 19.Reddy GK: Photobiological basis and clinical role of low-intensity lasers in biology and medicine. J Clin Laser Med Surg, 2004, 22: 141–150. [DOI] [PubMed] [Google Scholar]
- 20.Vinck E, Cagnie B, Coorevits P, et al. : Pain reduction by infrared light-emitting diode irradiation: a pilot study on experimentally induced delayed-onset muscle soreness in humans. Lasers Med Sci, 2006, 21: 11–18. [DOI] [PubMed] [Google Scholar]
- 21.Marque AP, Peccin MS: Pesquisa em Fisioterapia: a prática baseada em evidências e modelos de estudos. Fisioterapia Pesquisa, 2005, 10: 43–48. [Google Scholar]
- 22.Maher CG, Sherrington C, Herbert RD, et al. : Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther, 2003, 83: 713–721. [PubMed] [Google Scholar]
- 23.Okeson JP: Dor orofacial: guia de avaliação, diagnóstico e tratamento. São Paulo: Quintessence, 1998. [Google Scholar]
- 24.Helkimo M: Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr, 1974, 67: 101–121. [PubMed] [Google Scholar]
- 25.Fonseca DM, Bonfate G, Valle AL, et al. : Diagnóstico pela anamnese da disfunção craniomandibular. Rev Gaucha Odontol, 1994, 42: 23–28. [Google Scholar]
- 26.Fricton JR, Schiffman EL: The craniomandibular index: validity. J Prosthet Dent, 1987, 58: 222–228. [DOI] [PubMed] [Google Scholar]
- 27.Pehling J, Schiffman E, Look J, et al. : Interexaminer reliability and clinical validity of the temporomandibular index: a new outcome measure for temporomandibular disorders. J Orofac Pain, 2002, 16: 296–304. [PubMed] [Google Scholar]
- 28.Dworkin SF, LeResche L: Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord, 1992, 6: 301–355. [PubMed] [Google Scholar]
- 29.De Felício CM, Sidequersky FV, Tartaglia GM, et al. : Electromyographic standardized indices in healthy Brazilian young adults and data reproducibility. J Oral Rehabil, 2009, 36: 577–583. [DOI] [PubMed] [Google Scholar]
- 30.Armijo-Olivo S, Gadotti I, Kornerup M, et al. : Quality of reporting masticatory muscle electromyography in 2004: a systematic review. J Oral Sci, 2004, 10: 484–491. [DOI] [PubMed] [Google Scholar]
- 31.Venezian GC, da Silva MA, Mazzetto RG, et al. : Low level laser effects on pain to palpation and electromyographic activity in TMD patients: a double-blind, randomized, placebo-controlled study. Cranio, 2010, 28: 84–91. [DOI] [PubMed] [Google Scholar]
- 32.Hotta PT, Hotta TH, Bataglion C, et al. : Emg analysis after laser acupuncture in patients with temporomandibular dysfunction (TMD). Implications for practice. Complement Ther Clin Pract, 2010, 16: 158–160. [DOI] [PubMed] [Google Scholar]
- 33.Shinozaki EB, Dos Santos MB, Okazaki LK, et al. : Clinical assessment of the efficacy of low-level laser therapy on muscle pain in women with temporomandibular dysfunction, by surface electromyography. Braz J Oral Sci, 2010, 9: 434–438. [Google Scholar]
- 34.Shirani AM, Gutknecht N, Taghizadeh M, et al. : Low-level laser therapy and myofacial pain dysfunction syndrome: a randomized controlled clinical trial. Lasers Med Sci, 2009, 24: 715–720. [DOI] [PubMed] [Google Scholar]
- 35.Emshoff R, Bösch R, Pümpel E, et al. : Low-level laser therapy for treatment of temporomandibular joint pain: a double-blind and placebo-controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 105: 452–456. [DOI] [PubMed] [Google Scholar]
- 36.Carvalho CM, de Lacerda JÁ, dos Santos Neto FP, et al. : Wavelength effect in temporomandibular joint pain: a clinical experience. Lasers Med Sci, 2010, 25: 229–232. [DOI] [PubMed] [Google Scholar]
- 37.Salmos-Brito JA, de Menezes RF, Teixeira CE, et al. : Evaluation of low-level laser therapy in patients with acute and chronic temporomandibular disorders. Lasers Med Sci, 2013, 28: 57–64. [DOI] [PubMed] [Google Scholar]
- 38.da Cunha LA, Firoozmand LM, da Silva AP, et al. : Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J, 2008, 58: 213–217. [DOI] [PubMed] [Google Scholar]
- 39.Frare JC, Nicolau RA: Clinical analysis of the effect of laser photobiomodulation (GaAs − 904 nm) on temporomandibular joint dysfunction. Braz J Phys Ther, 2008, 12: 37–42. [Google Scholar]
- 40.Carrasco TG, Mazzetto MO, Mazzetto RG, et al. : Low intensity laser therapy in temporomandibular disorder: a phase II double-blind study. Cranio, 2008, 26: 274–281. [DOI] [PubMed] [Google Scholar]
- 41.Manfredini D, Winocur E, Ahlberg J, et al. : Psychosocial impairment in temporomandibular disorders patients. RDC/TMD axis II findings from a multicentre study. J Dent, 2010, 38: 765–772. [DOI] [PubMed] [Google Scholar]
- 42.Türp JC, Motschall E, Schindler HJ, et al. : In patients with temporomandibular disorders, do particular interventions influence oral health-related quality of life? A qualitative systematic review of the literature. Clin Oral Implants Res, 2007, 18: 127–137. [DOI] [PubMed] [Google Scholar]
- 43.El Hage Y, Politti F, Herpich CM, et al. : Effect of facial massage on static balance in individuals with temporomandibular disorder—a pilot study. Int J Ther Massage Bodyw, 2013, 6: 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Almeida P, Lopes-Martins RA, Tomazoni SS, et al. : Low-level laser therapy improves skeletal muscle performance, decreases skeletal muscle damage and modulates mRNA expression of COX-1 and COX-2 in a dose-dependent manner. Photochem Photobiol, 2011, 87: 1159–1163. [DOI] [PubMed] [Google Scholar]
- 45.Pinto MV, Da Costa DA, Rocha LL, et al. : Comparative study of the effects of the Ga-As (904 nm, 150 mW) laser and the pulsed ultrasound of 1 MHz in inflammation of tibialis muscle of wistar rats. Braz. Arch Biotechnology (N Y), 2008, 51: 225–230. [Google Scholar]
- 46.Goldman JA, Chiapella J, Casey H, et al. : Laser therapy of rheumatoid arthritis. Lasers Surg Med, 1980, 1: 93–101. [DOI] [PubMed] [Google Scholar]
- 47.Conti PC: Low level laser therapy in the treatment of temporomandibular disorders (TMD): a double-blind pilot study. Cranio, 1997, 15: 144–149. [DOI] [PubMed] [Google Scholar]
- 48.Pinheiro AL, Cavalcanti ET, Pinheiro TI, et al. : Low-level laser therapy in the management of disorders of the maxillofacial region. J Clin Laser Med Surg, 1997, 15: 181–183. [DOI] [PubMed] [Google Scholar]
- 49.Schuhfried M, Korpan V, Silig Y: Helium- Neon laser irradiation: effect on the experimental pain threshold. Lasers Med Sci, 2000, 15: 169–173. [Google Scholar]