Abstract
AIM: Intrabiliary rupture (IBR) is a common and serious compli-cation of hepatic hydatid cyst. The incidence varies from 1% to 25%. The treatment of IBR is still controversial. We aimed to design an algorithm for the treatment of hepatic hydatidosis with IBR by reviewing our cases.
METHODS: Eight cases of IBR were analyzed retrospectively. Patients were evaluated according to age, sex, clinical findings, cyst number and stage, abdominal ultrasonography and CT-scan, surgical methods, complica-tions, results and coincidental diseases.
RESULTS: Female/male ratio was 1/7. Mean age was 52.12±18.26 years (range 24-69 years). Right upper quadrant pain, flatulence, palpable hepatic mass were symptoms common in all patients. Cholestatic jaundice was found in four cases. In all patients, cyst evacuation and omento-plasty were performed, followed by either choledochod-uodenostomy, T-tube drainage, intracavitary suturing of the orifice, two cases in each. Whereas in two patients diagnosed post-operatively percutaneous drainage of biliary collection or ERCP and sphincteroplasty were added. Morbidity and hospital stay were higher in these cases.
CONCLUSION: When the diagnosis of IBR can be done pre-or intra-operatively, morbidity decreases. If a biliary fistula is seen post-operatively, endoscopic procedures such as ERCP, sphincteroplasty or nasobiliary drainage can be applied.
Keywords: Intrabiliary rupture, Hepatic hydatidcyst
INTRODUCTION
Intrabiliary rupture (IBR) is the most common and serious complication of hepatic hydatid cyst (HHC). It has also been reported as ‘cystobiliary fistula’ or ‘cystobiliary communication’ in the literature. The incidence varies from 1% to 25% although an incidence of 64.75% has been reported from a multicentric study in Tunisia[1-12].
Obstructive jaundice, fever, right-upper quadrant pain, nausea and vomiting, flatulence, palpable hepatic mass are the most commonly encountered symptoms in intrabiliary rupture[2,3,9].
Although there is some consensus on the medical and surgical treatment of hydatid cyst diseases, the treatment of intrabiliary rupture still remains controversial. Intracystic suturing of the orifice, T-tube drainage, double side drainage, cystobiliary disconnection, choledochoduodenostomy, choledochojejunostomy, endoscopic sphincterotomy and nasobiliary stent application have been used.
In this report, eight cases of intrabiliary rupture were presented and discussed in the light of literature review.
MATERIALS AND METHODS
In this study, eight cases of hepatic hydatid cyst with cystobiliary fistulae treated by our team between 1994 and 2003 were presented. They began to undergo intra-operative ultrasonography (US) in 1997.
All patients’ records were reviewed and evaluated as to the age, sex, clinical findings, cyst number and stages according to Gharbi’s classification, abdominal ultrasono-graphy and CT-scan results, surgical methods, complications, results and coincidental diseases.
RESULTS
Patients’ data
Between 1994 and 2003, a total of 70 cases of hepatic hydatidosis were treated surgically by our team, of these cases eight (11.42%) had cystobiliary fistulae, diagnosed either pre-, intra- or post-operatively. Female/male ratio was 1/7. Mean age was 52.12±18.26 years (range 24-69 years).
Right upper quadrant pain, flatulence, palpable hepatic mass were the symptoms present in all patients. Cholestatic jaundice was found in four cases.
Four patients had one, two patients had two and the other two patients had three or more cysts. The majority of the cysts were in stage III (62.5 %) and stage II (37.5 %) (Table 1). Seven cases had their cysts in the right hepatic lobe, one in the left lobe. The cyst sizes were in the range of 2.5-15 cm. Table 1 summarizes the patients’ data.
Table 1.
Patients’ characteristics (n = 8).
| Mean age | 52.12±18.26 |
| Female/male | 1/7 |
| Symptoms | |
| Right upper quadrant pain, palpable hepatic mass, flatulence | 8 |
| Cholestatic jaundice | 4 |
| Number of cysts | |
| 1 | 4 |
| 2 | 2 |
| 3 or more | 2 |
| Stages of cysts (According to Gharbi’s classification) Stage II | 3 |
| Stage III | 5 |
| Choledochal image at US and CT-scan dilated ( = 2 cm) | 3 |
| Normal | 5 |
Four cases had obstructive jaundice. Total bilirubin was as high as 7 mg/dL. ALT, AST and ALP levels were thrice the normal levels. Four patients had no elevation at bioche-mical analysis (Table 2).
Table 2.
Objectives of the cysts and diagnostic investigations.
| Patient number | ALT, AST, ALP levels | Bilirubin levels (total/conj mg/dL) |
| 1 | High | 7/5 |
| 2 | N | N |
| 3 | N | N |
| 4 | N | N |
| 5 | High | 5/3 |
| 6 | High | 5/3 |
| 7 | High | 11/8 |
| 8 | N | N |
US and CT-scan showed choledochal dilatation of 2 cm in three patients. Biochemical tests of these cases were high.
Treatments of patients
Benzimidazole treatment was started 7-30 d before surgery (mean 14±8.45 d) and continued for 2-5 mo (mean 3.71±1.11 mo) after surgery, in a monthly cyclic protocol.
All cysts were treated by evacuation+omentoplasty+ drainage of the cystic cavity. The cystic cavities were disinfected by 1.7 mg/mL albendazole solution as described previously[13-15]. When choledochotomy was done, all contents in the common bile duct (CBD) were evacuated and biliary tracts were irrigated with 0.9% NaCl solution. Table 3 and Figure 1 show the treatment of intrabiliary rupture.
Table 3.
Diagnosis and treatment of cystobiliary fistulae.
| Patient number | Clinical and diagnostic characteristics of the patients | Treatment of common bile duct |
| 1 | Evidence of obstructive jaundice with cystic contents in large CBD | Choledochoduodenostomy |
| 2 | Bile stained cystic liquid and visible orifice | Suturing orifice |
| 3 | Bile stained cystic liquid and visible orifice | Suturing orifice |
| 4 | Bile in cystic liquid | T-tube drainage |
| 5 | Evidence of obstructive jaundice, invisible orifice, normal caliber choledochus (postop biliary leakage) | Percutaneous drainage under US guidance post-operatively |
| 6 | Evidence of obstructive jaundice with cystic contents in a large CBD | Choledochoduodenostomy |
| 7 | Evidence of obstructive jaundice, hemobilia, enlargement of the CBD with cystic content | T-tube drainage |
| 8 | No suspicion of intrabiliary rupture | ERCP and sphincteroplasty |
Figure 1.
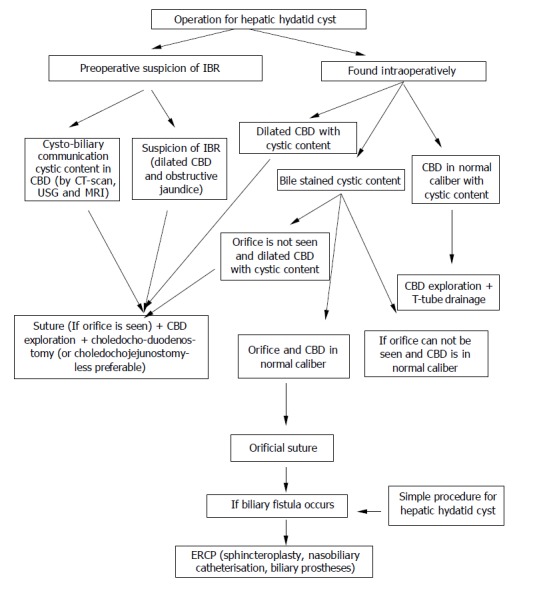
Algorithm in the management of intrabiliary rupture (IBR: intrabiliary rupture, CBD: common bile duct).
Evidence of obstructive jaundice with cystic contents in large common bile duct There were three such cases. Two of them were treated by choledochoduodenostomy. Cystic content and hemobilia were diagnosed in the CBD of the third case in which choledochus was evacuated and T-tube drainage was performed. The specific cause of hemobilia could not be determined.
Evidence of obstructive jaundice, invisible orifice, normal caliber choledochus There was only one such patient. Hyperbilir-ubinemia was 5 mg/dL. There was no bile staining of the cystic liquid. No pathological change was found at the inspection or palpation of the CBD, therefore no surgical procedure was performed for intrabiliary rupture. However, bile leakage in the range of 1000 mL/d was diagnosed in the early post-operative period. Perihepatic biliary collection was also diagnosed later and drainage under US guidance was performed. Bile leakage subsequently regressed and stopped in 2 wk.
The cases with bile stained cystic liquid Two of the three such cases had visible orifices and were treated by suturing with nonabsorbable materials. At last one orifice could not be identified. Choledochotomy was done since it was suspected that there was cystic content in the CBD, but cystic content could not be seen. T-tube drainage was carried out. Biliary fistulae did not occur.
In a case of unsuspected intrabiliary rupture, a cyst, 10 cm in diameter was present in the right lobe. The cystic liquid was not stained by bile. Extrahepatic biliary system was found normal intra-operatively. No orifice could be identified because of difficult localization. A high output (1000 mL/d) biliary fistula occurred on the first post-operative day and continued for a week. ERCP and sphincteroplasty were performed and the biliary fistula stopped at the 4th post-operative week.
T-tubes were removed on the 10th d in patients with a normal caliber choledoch, while the removal was delayed on the 20th d in patients with an enlarged choledoch with daughter vesicles and hemobilia.
Four patients had coincidental diseases. Two of them had cholelithiasis (cholecystectomy was done). One of them had coronary disease. Another patient had coronary disease, hypertension and diabetes mellitus.Perihepatic biliary collection noted above was only a complication.
The mean length of hospital stay was 17±11.63 d (range 10-45 d). In one patient with prolonged biliary fistulae the hospital stay was 45 d. When this patient was excluded, the mean hospital stay was 13±2.94 d.
The mean follow-up period was 57.87±40.47 mo (range 3-120 mo). No morbidity or mortality was seen during this period.
DISCUSSION
Intrabiliary rupture is a common and serious complication of hepatic hydatidosis. It occurs especially in centrally localized and high stage cyst. High intracystic pressure up to 80 cm H2O is a predisposing factor. The cyst rupture can occur in three clinical forms. Contained rupture occurs when the cyst contents are confined within the pericyst. Communicating rupture defines tearing of the pericyst and evacuation of cyst contents into the biliary tract or bronchioles. Direct rupture describes complete tear of the cyst wall and spillage of the cyst contents into the peritoneal or pleural cavity. Small cysto-biliary communications develop in 80-90% of all HHCs[16].
Furthermore, there are two different clinical settings associated with intrabiliary rupture: frank intrabiliary rupture and simple communication. In the former, the cyst content drains to biliary tract and causes cholestatic jaundice. In the latter simple communications are frequently overlooked and could cause biliary fistulae post-operatively[17]. If the cystobiliary opening was less than 5 mm, spontaneous drainage of the cystic content was uncommon and could be treated by suturing under the direct vision[18]. If the CBD diameter was larger than 5 mm, cystic content migration into the biliary tract would occur in 65% of the cases[19]. Vesicles, debris and purulent materials may be found in the biliary collection.
In all patients the most frequent symptoms were right upper quadrant pain and flatulence. Obstructive jaundice and fever have been recorded in 90% and 20% of the cases respectively. Nausea and vomiting were rare[2,3,9,20].
Diagnosis of IBR is difficult and can be established pre-, intra- and post-operatively. When obstructive jaundice is present, US, CT-scan, magnetic resonance imaging (MRI) and scintigraphic investigation can show the cyst and cystobiliary communications, but in patients with no jaundice, a correct diagnosis can be made in only 25%. Radiodiagnostic evaluation can also demonstrate cystic content in the gall bladder[7] and the CBD[1,4,19,21]. On the other hand, cholelit-hiasis and choledocholithiasis are common (81-61.53%) coincidental diseases[6,7]. Laboratory and serological tests can also be helpful for diagnosis.
If obstructive jaundice was not present and cystobiliary connection could not be seen pre-operatively, three findings should raise suspicion of cystobiliary fistulas, namely bile-stained cystic fluid, visualized and sutured bile leak orifice intra-operatively; intra-operative observation of CBD enlarg-ement or the presence of cyst content in the common bile duct; unexpected post-operative bile drainage from the cavity drains[8,22,23].
The orifice of bile leakage could be seen in 11.7-17.07% of the cases during the operation[3,23] while this was difficult in posteriorly localized cysts. In these cases, cholangiography could be done by a catheter pushed into the ductus cysticus or the cystobiliary fistula[3,4,8,22,23]. As an extreme procedure, puncture of choledochus and injection of radioopac solution or methylene blue are helpful to diagnose intrabiliary rupture or to see the orifice. Eleftheriadis[23] emphasized that choledochoscopy could also be helpful in the diagnosis of IBR.
When an intrabiliary rupture is diagnosed pre-or intra-operatively, there are alternative treatment modalities in addition to conventional surgery of hepatic hydatid cyst. Cystic evacuation, removal of germinative layer, disinfection of cystic cavity are necessary. If cystobiliary orifice is seen and no cystic content is observed in a normal caliber choledo-chus, suturing the orifice is sufficient to prevent the compl-ications. Videolaparoscopical suturing of the orifice has been reported in literature[8].
When cystic content is observed in a normal caliber choledochus, choledochotomy+evacuation of cystic content and debris from biliary tree±irrigation with 0.9% NaCl solution and T-tube drainage are enough. If CBD enlarge-ment is diagnosed with cystic content in it or in the gallbladder, choledochoduodenostomy is preferable. Some authors have reported the wide application of T-tube drainage in cases with high morbidity rates[3,4,6,7,9,22,24,25]. On the other hand, Roux and Y hepaticojejunostomy have been reported for the treatment of bile duct stricture associated intrabiliary rupture[20,26]. Open sphincteroplasty was also used in the last decades[25].
The presence of cholangitis has been reported as a risk factor. Even T-tube drainage itself could cause cholestatic icterus[3,17,27] and is also a source of infection[28]. Some auth-ors have used cystojejunostomy albeit the risk that cystic content drainage into the biliary tract could result in obstr-uctive jaundice and cholangitis[21,29].
When intrabiliary rupture was overlooked during the surgical treatment, biliary fistulae (up to 1 000 mL/d) were unavoidable and if this occurred ERCP would be nece-ssary. Post-operative biliary fistula rate was about 20% in all cases[22,23,30,31].
In the cases of overlooked cystobiliary fistulae, transsphincteric evacuation of the CBD and sphincteroplasty could be applied. Nasobiliary drainage could also be done. Usually, the majority of biliary fistulae could be closed in a few weeks[2,8,27,30,32].
The usage of endoprostheses in biliary fistula was not common. This can be considered in either high output bile leakage or for intractable fistulae[31].
The morbidity and mortality rates of all patients were 19.44-43.03% and 1.8-4.5% respectively in literature. The most common causes of deaths were sepsis and hepatic failure[3,4,9,22,23].
Hospital stay was the longest in the T-tube group. The patients undergoing choledochoduodenostomy had longer hospital stay than those undergoing simple orifice suturing[3].
In conclusion, IBR has an algorithm in the diagnosis and treatment. If it is not detected pre- or intra-operatively, a biliary fistula is common, its morbidity and mortality rates are high. Detecting and suturing orifices in cystic wall are the best methods of treatment. When cystic content is found in choledochus or when biliary fistula occurs, more complex procedures are necessary.
References
- 1.Alper A, Ariogul O, Emre A, Uras A, Okten A. Choledochoduodenostomy for intrabiliary rupture of hydatid cysts of liver. Br J Surg. 1987;74:243–245. doi: 10.1002/bjs.1800740405. [DOI] [PubMed] [Google Scholar]
- 2.Atli M, Kama NA, Yuksek YN, Doganay M, Gozalan U, Kologlu M, Daglar G. Intrabiliary rupture of a hepatic hydatid cyst: associated clinical factors and proper management. Arch Surg. 2001;136:1249–1255. doi: 10.1001/archsurg.136.11.1249. [DOI] [PubMed] [Google Scholar]
- 3.Bedirli A, Sakrak O, Sozuer EM, Kerek M, Ince O. Surgical management of spontaneous intrabiliary rupture of hydatid liver cysts. Surg Today. 2002;32:594–597. doi: 10.1007/s005950200107. [DOI] [PubMed] [Google Scholar]
- 4.Daali M, Fakir Y, Hssaida R, Hajji A, Hda A. Hydatid cysts of the liver opening in the biliary tract. Report of 64 cases. Ann Chir. 2001;126:242–245. doi: 10.1016/s0003-3944(01)00507-7. [DOI] [PubMed] [Google Scholar]
- 5.Dawson JL, Stamatakis JD, Stringer MD, Williams R. Surgical treatment of hepatic hydatid disease. Br J Surg. 1988;75:946–950. doi: 10.1002/bjs.1800751004. [DOI] [PubMed] [Google Scholar]
- 6.Lygidakis NJ. Diagnosis and treatment of intrabiliary rupture of hydatid cyst of the liver. Arch Surg. 1983;118:1186–1189. doi: 10.1001/archsurg.1983.01390100056014. [DOI] [PubMed] [Google Scholar]
- 7.Martí-Bonmatí L, Menor F, Ballesta A. Hydatid cyst of the liver: rupture into the biliary tree. AJR Am J Roentgenol. 1988;150:1051–1053. doi: 10.2214/ajr.150.5.1051. [DOI] [PubMed] [Google Scholar]
- 8.Masatsugu T, Shimizu S, Noshiro H, Mizumoto K, Yamaguchi K, Chijiiwa K, Tanaka M. Liver cyst with biliary communication successfully treated with laparoscopic deroofing: a case report. JSLS. 2003;7:249–252. [PMC free article] [PubMed] [Google Scholar]
- 9.Ulualp KM, Aydemir I, Senturk H, Eyuboğlu E, Cebeci H, Unal G, Unal H. Management of intrabiliary rupture of hydatid cyst of the liver. World J Surg. 1995;19:720–724; discussion 728. doi: 10.1007/BF00295913. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz E, Gökok N. Hydatid disease of the liver: current surgical management. Br J Clin Pract. 1990;44:612–615. [PubMed] [Google Scholar]
- 11.Dugalić D, Djukić V, Milićević M, Stevović D, Knezević J, Pantić J. Operative procedures in the management of liver hydatidoses. World J Surg. 1982;6:115–118. doi: 10.1007/BF01656384. [DOI] [PubMed] [Google Scholar]
- 12.Dadoukis J, Gamvros O, Aletras H. Intrabiliary rupture of the hydatid cyst of the liver. World J Surg. 1984;8:786–790. doi: 10.1007/BF01655782. [DOI] [PubMed] [Google Scholar]
- 13.Erzurumlu K, Ozdemir M, Mihmanli M, Cevikbaş U. The effect of intraoperative mebendazole-albendazole applications on the hepatobiliary system. Eur Surg Res. 1995;27:340–345. doi: 10.1159/000129418. [DOI] [PubMed] [Google Scholar]
- 14.Erzurumlu K, Sahin M, Selcuk MB, Yildiz C, Kesim M. Intracystic application of mebendazole solution in the treatment of liver hydatid disease. Preliminary report of two cases. Eur Surg Res. 1996;28:466–470. doi: 10.1159/000129492. [DOI] [PubMed] [Google Scholar]
- 15.Erzurumlu K, Hökelek M, Gönlüsen L, Tas K, Amanvermez R. The effect of albendazole on the prevention of secondary hydatidosis. Hepatogastroenterology. 2000;47:247–250. [PubMed] [Google Scholar]
- 16.Lewall DB, McCorkell SJ. Rupture of echinococcal cysts: diagnosis, classification, and clinical implications. AJR Am J Roentgenol. 1986;146:391–394. doi: 10.2214/ajr.146.2.391. [DOI] [PubMed] [Google Scholar]
- 17.Hankins JR. Management of complicated hepatic hydatid cysts. Ann Surg. 1963;158:1020–1034. doi: 10.1097/00000658-196312000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozmen MM, Coskun F. New technique for finding the ruptured bile duct into the liver cysts: scope in the cave technique. Surg Laparosc Endosc Percutan Tech. 2002;12:187–189. doi: 10.1097/00129689-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Zaouche A, Haouet K, Jouini M, El Hachaichi A, Dziri C. Management of liver hydatid cysts with a large biliocystic fistula: multicenter retrospective study. Tunisian Surgical Association. World J Surg. 2001;25:28–39. doi: 10.1007/s002680020005. [DOI] [PubMed] [Google Scholar]
- 20.Jabbour N, Shirazi SK, Genyk Y, Mateo R, Pak E, Cosenza DC, Peyré CG, Selby RR. Surgical management of complicated hydatid disease of the liver. Am Surg. 2002;68:984–988. [PubMed] [Google Scholar]
- 21.Barros JL. Hydatid disease of the liver. Am J Surg. 1978;135:597–600. doi: 10.1016/0002-9610(78)90043-0. [DOI] [PubMed] [Google Scholar]
- 22.Kayaalp C, Bostanci B, Yol S, Akoglu M. Distribution of hydatid cysts into the liver with reference to cystobiliary communications and cavity-related complications. Am J Surg. 2003;185:175–179. doi: 10.1016/s0002-9610(02)01202-3. [DOI] [PubMed] [Google Scholar]
- 23.Eleftheriadis E, Tzartinoglou E, Kotzampassi K, Aletras H. Choledochoscopy in intrabiliary rupture of hydatid cyst of the liver. Surg Endosc. 1987;1:199–200. doi: 10.1007/BF00591147. [DOI] [PubMed] [Google Scholar]
- 24.Moreno VF, Lopez EV. Acute cholangitis caused by ruptured hydatid cyst. Surgery. 1985;97:249. [PubMed] [Google Scholar]
- 25.Vicente E, Meneu JC, Hervás PL, Nuño J, Quijano Y, Devesa M, Moreno A, Blazquez L. Management of biliary duct confluence injuries produced by hepatic hydatidosis. World J Surg. 2001;25:1264–1269. doi: 10.1007/s00268-001-0107-3. [DOI] [PubMed] [Google Scholar]
- 26.Akkiz H, Akinoglu A, Colakoglu S, Demiryürek H, Yagmur O. Endoscopic management of biliary hydatid disease. Can J Surg. 1996;39:287–292. [PMC free article] [PubMed] [Google Scholar]
- 27.Ovnat A, Peiser J, Avinoah E, Barki Y, Charuzi I. Acute cholangitis caused by ruptured hydatid cyst. Surgery. 1984;95:497–500. [PubMed] [Google Scholar]
- 28.Giouleme O, Nikolaidis N, Zezos P, Budas K, Katsinelos P, Vasiliadis T, Eugenidis N. Treatment of complications of hepatic hydatid disease by ERCP. Gastrointest Endosc. 2001;54:508–510. doi: 10.1067/mge.2001.118256. [DOI] [PubMed] [Google Scholar]
- 29.de Aretxabala X, Perez OL. The use of endoprostheses in biliary fistula of hydatid cyst. Gastrointest Endosc. 1999;49:797–799. doi: 10.1016/s0016-5107(99)70306-8. [DOI] [PubMed] [Google Scholar]
- 30.Dumas R, Le Gall P, Hastier P, Buckley MJ, Conio M, Delmont JP. The role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatid disease. Endoscopy. 1999;31:242–247. doi: 10.1055/s-1999-14209. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez AN, Sánchez del Río AL, Alguacil LV, De Dios Vega JF, Fugarolas GM. Effectiveness of endoscopic sphincterotomy in complicated hepatic hydatid disease. Gastrointest Endosc. 1998;48:593–597. doi: 10.1016/s0016-5107(98)70041-0. [DOI] [PubMed] [Google Scholar]
- 32.Bilsel Y, Bulut T, Yamaner S, Buyukuncu Y, Bugra D, Akyuz A, Sokucu N. ERCP in the diagnosis and management of complications after surgery for hepatic echinococcosis. Gastrointest Endosc. 2003;57:210–213. doi: 10.1067/mge.2003.64. [DOI] [PubMed] [Google Scholar]


