Abstract
AIM: In order to obtain lymphogenous metastasis-associated genes, we compared the transcriptional profiles of mouse hepatocarcinoma cell lines Hca-F with highly lymphatic metastasis potential and Hca-P with low lymphatic metastasis potential.
METHODS: Total RNA was isolated from Hca-F and Hca-P cells and synthesized into double-stranded cDNA. In vitro transcription double-stranded cDNA was labeled with biotin (i.e., biotin-labeled cRNA, used as the probe). The cRNA probes hybridized with Affymetrix GeneChip® MOE430A (containing 22690 transcripts, including 14500 known mouse genes and 4371 ESTs) respectively and the signals were scanned by the GeneArray Scanner. The results were then analyzed by bioinformatics.
RESULTS: Out of the 14500 known genes investigated, 110 (0.8%) were up regulated at least 23 fold. Among the total 4371 ESTs, 17 ESTs (0.4%) (data were not presented) were up regulated at least 23 fold. According to the Gene Ontology and TreeView analysis, the 110 genes were further classified into two groups: differential biological process profile and molecular function profile.
CONCLUSION: Using high-throughput gene chip method, a large number of genes and their cellular functions about angiogenesis, cell adhesion, signal transduction, cell motility, transport, microtubule-based process, cytoskeleton organization and biogenesis, cell cycle, transcription, chaperone activity, motor activity, protein kinase activity, receptor binding and protein binding might be involved in the process of lymphatic metastasis and deserve to be used as potential candidates for further investigation. Cyclin D1, Fosl1, Hsp47, EGFR and AR, and Cav-1 are selected as the possible candidate genes of the metastatic phenotype, which need to be validated in later experiments. ESTs (data were not presented) might indicate novel genes associated with lymphatic metastasis. Validating the function of these genes is helpful to identify the key or candidate gene/pathway responsible for lymphatic metastasis, which might be used as the diagnostic markers and the therapeutic targets for lymphatic metastasis.
Keywords: Hepatocarcinoma, Lymphatic metastasis, Cell lines Hca-F and Hca-P, Gene chip
INTRODUCTION
Metastasis is the major cause of cancer morbidity and mortality[1]. Metastasis formation is a complex process, involving invasion, transport, arrest, adherence, extravasation and tumor cell proliferation[2]. High-throughput methods are needed to display the molecular changes involved in this complicated series of steps. Recent development of cDNA microarray technology has opened a new era in this field[3]. It can provide massive datasets simultaneously. Except this, suitable models for cancer metastasis are necessary for analysis of mechanisms[4]. Because majority of malignant tumors are carcinomas and lymph node metastases often represent the first step in the metastatic process, whereas the molecular mechanism of lymphatic metastasis remains poorly understood, the clones of lymphatic metastasis are prone to be established. A mouse hepatocarcinoma cell line named Hca-F with highly lymphogenous metastatic potential and its syngeneic cell line named Hca-P[5] with low lymphogenous metastatic potential have been isolated from hepatocarcinomas in mice. Using gene chip combination with lymphatic metastasis models, we investigated the transcriptional profiles of the mouse hepatocarcinoma cell lines Hca-F with a metastasis rate over 70% and its syngeneic cell line Hca-P with a metastasis rate less than 30% in order to identify lymphatic metastasis-associated genes. Although several metastasis-associated genes have already been screened with these two cell lines using suppression subtractive hybridization method, we decided to detect the expression profiles of cell lines Hca-F and Hca-P using Affymetrix Genechip® array technology in purpose of extending the panel of candidate genes.
MATERIALS AND METHODS
Animals and cell lines
Hepatocarcinoma cell lines, Hca-F and Hca-P were established and stored by our department. Inbred 615-mice were bred and provided by our department. Forty 615-mice were equally divided into two groups. Hca-F and Hca-P cells were inoculated into 20 mice in each group respectively (2×106 cells per mouse). On the 28th d after inoculation, mice were killed and their lymph nodes were collected and stained using HE and examined by light microscope. Then the lymph node metastasis rates of Hca-F and Hca-P cell lines were calculated and tested.
RNA collection and probe preparation for oligonucleotide array hybridization
Total RNA was isolated from Hca-F and Hca-P cells respectively using TRIzol reagent (Invitrogen Life Technologies, P/N 15596-018) and cleaned with Rneasy Mini Kit (Qiagen, P/N 74104). cDNA was synthesized using the T7-Oligo(dT)24 primer (5’-GGCCAGTGAATTGTAATACGACTCACTATAGGGAGGCGG-(dT)24-3’). Double-stranded cDNA was purified with Phase Lock Gel (Eppendorf, P/N 0032 007.953)-phenol/chloroform extraction (Ambion, P/N 9732). Then in vitro transcription labeling was performed using the Enzo RNA Transcript Labeling Kit (Affymetrix, P/N 900182). The biotin-labeled cRNA was purified with the Qiagen Rneasy Mini Kit and fragmented randomly to an average size of approximately 50-200 bases by mild alkaline treatment at 94 °C for 35 min in fragmentation buffer. The hybridization solution was composed of 0.05 μg/μL fragmented cRNA, 1 μL herring sperm DNA, 1 μL acetylated BSA and 50 μL 2×hybridization buffer. In addition, the hybridization solution contained a mixture of four control cRNAs for bacterial and phage genes (bioB, bioC, bioD and cre at 5, 5, 25 and 100 pmol/L, respectively) to serve as comparison tools for hybridization efficiency between arrays. A biotinylated oligonucleotide B2, which specifically hybridized to features at the center and corners of the chip, was also added to the solution to allow correct orientation and recognition of the probe sets.
Array hybridization and scanning
The hybridization cocktail was heated to 99 °C for 5 min in a heat block, followed by a 45 °C heat block for 5 min and centrifugation for 5 min to remove any insoluble material. Meanwhile, the arrays were wet with appropriate volume 1×hybridization and incubated by 1×hybridization buffer at 45 °C for 10 min with rotation. The buffer solution was then removed from the probe array and the clarified-hybridization cocktail was added. Fragmented cRNA (5 μg) was hybridized to Affymetrix MOE430A array (containing 22690 transcripts, almost 14500 known genes and 4 371 ESTs) for 16 h in Affymetrix® Fluidics Station 400. The arrays were then scanned using the GeneArray Scanner (G2500AgeneArray Scanner, Affymetrix). The cRNA probe was first hybridized to a “test chip” before to the MOE430A array and the quality was confirmed.
Statistical analysis
The data obtained through GeneChip® scanning was analyzed using Affymetrix® Microarray Suit Software 5.0[6,7]. Before the two arrays were compared, the GeneChip® software conducted normalization and scaling of the data for each array. The mRNA expression level of a transcript is directly related to the signal which is a quantitative metric calculated for each probe set and measures the mean difference of fluorescence intensity between perfect match and central mismatch oligonucleotides of a probe set. Signal log ratio, which estimates the magnitude and direction of change of a transcript when two arrays are compared, of at least three (that indicates an increase of the transcript level by 23-fold change), and changing P-value, which measures the probability that the expression levels of a probe set in two different arrays are the same or not, ≤0.05 (that means the expression level in the experiment array is higher than that of the baseline array) were used to select differentially expressed genes. In the following, only up-regulated genes were presented and the assignment “up-regulated” refers to Hca-F in comparison with Hca-P.
RESULTS
The lymph node metastasis rates of Hca-F and Hca-P were 75% (15/20) and 25% (5/20), respectively. The quality of GeneChip® was tested and verified by the positive controls of murine housekeepers β-actin and GAPDH and externally positive controls of spiked bacterial bioB, bioC, bioD and cre (Figure 1). Figure 2A, B indicate the scanning result of real chip (Hca-F and Hca-P, respectively). Figure 3 indicates the comparison of gene expression signal in cell line Hca-F with Hca-P.
Figure 1.
Scanning result of test chip.
Figure 2.
(A) Scanning result of real chip after hybridization with cRNA from Hca-F cell line; (B) Scanning result of real chip after hybridization with cRNA from Hca-P cell line.
Figure 3.
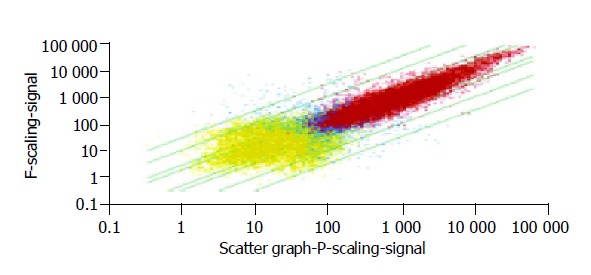
Comparison of gene expression signal in Hca-F cell line with that in Hca-P cell line.
To identify genes associated with the lymphatic metastasis, we analyzed the transcriptional profiles of 14500 mouse genes and 4371 ESTs from highly lymphatic metastasis potential cell line Hca-F and low lymphatic metastasis potential cell line Hca-P using the Affymetrix GeneChip® array method. On the basis of the selection criteria for up-regulated described above, 110 genes (132 transcripts) and 17 ESTs (21 transcripts) (data were not presented) were obtained. The results about differentially expressed genes are presented in Table 1.
Table 1.
Differential gene expression profile in cell lines Hca-F vs Hca-P.
| Gene | Symbol descriptions | F vs P_Signal log ratio |
| Slc38a4 | Solute carrier family 38, member 4 | |
| 1gb: NM_027052 | 9 | |
| gb: AK003626 | 3.4 | |
| Krt2-8 | Keratin complex 2, basic, gene 8 | |
| gb: M21836 | 8.6 | |
| gb: NM_031170 | 4.8 | |
| Krt1-19 | Keratin complex 1, acidic, gene 19 | 7.4 |
| Cldn9 | Claudin 9 | 7.4 |
| Gja1 | Gap junction membrane channel protein alpha 1 | |
| gb: M63801 | 7.2 | |
| gb: BC006894 | 6.4 | |
| Fbp2 | Fructose bisphosphatase 2 | 7.1 |
| R75183 | Expressed sequence R75183 | |
| gb: BC004774 | 7 | |
| gb: BB324973 | 5.5 | |
| Egfr | Epidermal growth factor receptor | |
| gb: AF275367 | 6.9 | |
| gb: U03425 | 3.6 | |
| Lepr | Leptin receptor | 6.7 |
| Tm4sf3 | Transmembrane 4 superfamily member 3 | 6.5 |
| Pla2g1b | Phospholipase A2, group IB, pancreas | 6.4 |
| Ripk3 | Receptor-interacting serine-threonine kinase 3 | 6.4 |
| Igfbp4 | Insulin-like growth factor binding protein 4 | |
| gb: NM_010517 | 6.3 | |
| gb: BC019836 21423756_s_at | 5.8 | |
| gb: BC019836 1423757_x_at | 4.1 | |
| gb: AA119124 | 4 | |
| Piwil2 | Piwi-like homolog 2 (Drosophila) | 6.3 |
| IL24 | Interleukin 24 | 5.9 |
| Daf1 | Decay accelerating factor 1 | 5.9 |
| Cav | Caveolin, caveolae protein | 5.8 |
| Arhgef3 | Rho guanine nucleotide | |
| exchange factor (GEF) 3 | 5.7 | |
| Efna1 | Ephrin A1 | |
| gb: D38146 | 5.7 | |
| gb: BC002046 | 4.2 | |
| Ptpn8 | Protein tyrosine phosphatase, | |
| non-receptor type 8 | 5.6 | |
| Rab3b | RAB3B, member RAS oncogene family | 5.6 |
| 1190003K14Rik | RIKEN cDNA 1190003K14 gene | 5.6 |
| Sh3bp5 | SH3-domain binding protein 5 | |
| (BTK-associated) | 5.5 | |
| Fscn1 | Fascin homolog 1, actin bundling protein | |
| (Strongylocentrotus purpuratus) | ||
| gb: NM_007984 1416514_a_at | 5.4 | |
| gb: BE952057 | 4.2 | |
| gb: NM_007984 1448378_at | 3.7 | |
| Fgf15 | Fibroblast growth factor 15 | 5.4 |
| Ehox | ES cell derived homeobox containing gene | 5.3 |
| Ankrd1 | Ankyrin repeat domain 1 (cardiac muscle) | |
| gb: NM_013468 | 5.3 | |
| gb: AK009959 | 3.6 | |
| 1600023A02Rik | RIKEN cDNA 1600023A02 gene | 5.3 |
| Cd109 | CD109 antigen | 5.3 |
| BC037006 | cDNA sequence BC037006 | 5.3 |
| Ltb4dh | Leukotriene B4 12-hydroxydehydrogenase | 5.2 |
| Krt2-7 | Keratin complex 2, basic, gene 7 | 5.2 |
| Cnn2 | Calponin 2 | 5.2 |
| Sema3b | Sema domain, immunoglobulin domain (Ig), | |
| short basic domain, secreted, (semaphorin) 3B | ||
| gb: BB116052 | 5.1 | |
| gb: NM_009153 | 4.7 | |
| Krt1-18 | Keratin complex 1, acidic, gene 18 | 5.1 |
| Mouse gene for 18S rRNA | 5.1 | |
| Fosl1 | Fos-like antigen 1 | |
| gb: NM_010235 | 5 | |
| gb: U34245 | 4.4 | |
| Sncg | Synuclein, gamma | 5 |
| Col8a1 | Procollagen, type VIII, alpha 1 | 4.9 |
| Pcdhb7 | Protocadherin beta 7 | 4.9 |
| Msln | Mesothelin | 4.9 |
| IL23a | Interleukin 23, alpha subunit p19 | 4.9 |
| Mus musculus adult male tongue cDNA | 4.8 | |
| Ppp1r14a | Protein phosphatase 1, regulatory | |
| (inhibitor) subunit 14A | 4.7 | |
| Csf3 | Colony stimulating factor 3 (granulocyte) | 4.7 |
| Nfil3 | Nuclear factor, interleukin 3, regulated | 4.6 |
| Procr | Protein C receptor, endothelial | 4.6 |
| Nr1d1 | Nuclear receptor subfamily 1, | |
| group D, member 1 | 4.6 | |
| 2810003C17Rik | RIKEN cDNA 2810003C17 gene | 4.6 |
| MGC27770 | Hypothetical protein MGC27770 | 4.5 |
| Eng | Endoglin | 4.5 |
| F2r | Coagulation factor II (thrombin) receptor | 4.5 |
| Cdc42ep5 | CDC42 effector protein | |
| (Rho GTPase binding) 5 | 4.4 | |
| Pla2g7 | Phospholipase A2, group VII | |
| (platelet-activating factor | ||
| acetylhydrolase, plasma) | 4.4 | |
| D18Ertd653e | DNA segment, Chr 18, | |
| ERATO Doi 653, expressed | 4.4 | |
| IL2rg | Interleukin 2 receptor, gamma chain | |
| gb: L20048 1416296_at | 4.3 | |
| gb: L20048 1416295_a_at | 3.3 | |
| Smpd2 | Sphingomyelin phosphodiesterase 2, neutral | 4.3 |
| Areg | Amphiregulin | 4.3 |
| Mcam | Melanoma cell adhesion molecule | 4.2 |
| Rtn2 | Reticulon 2 (Z-band associated protein) | 4.2 |
| Gcnt2 | Glucosaminyltransferase, I-branching enzyme | 4.2 |
| D7Ertd458e | DNA segment, Chr 7, ERATO Doi 458, expressed | |
| gb: NM_009310 | 4.2 | |
| gb: BB049138 1423904_a_at | 4 | |
| gb: BC013673 1451160_s_at | 4 | |
| gb: BB049138 1423905_at | 3.9 | |
| gb: BC013673 1423903_at | 3.8 | |
| Chi3l3 | Chitinase 3-like 3 | 4.1 |
| D4Ertd765e | DNA segment, Chr 4, | |
| ERATO Doi 765, expressed | 4.1 | |
| Ptpr | Protein tyrosine phosphatase, receptor type, R | 4.1 |
| Scn8a | Sodium channel, voltage-gated, type VIII, | |
| alpha polypeptide | 4 | |
| AXL | AXL receptor tyrosine kinase | 4 |
| Serpinh1 | Serine (or cysteine) proteinase inhibitor, | |
| clade H, member 1 | 4 | |
| Panx1 | Pannexin 1 | 3.9 |
| Tm4sf9 | Transmembrane 4 superfamily member 9 | 3.9 |
| Mak | Male germ cell-associated kinase | 3.9 |
| Mus musculus transcribed sequences | 3.8 | |
| 9130017N09Rik | RIKEN cDNA 9130017N09 gene | 3.8 |
| Loxl2 | Lysyl oxidase-like 2 | 3.7 |
| Dok1 | Downstream of tyrosine kinase 1 | 3.6 |
| Abhd3 | Abhydrolase domain containing 3 | 3.6 |
| Ramp3 | Receptor (calcitonin) activity | |
| modifying protein 3 | 3.6 | |
| Fibp | Fibroblast growth factor (acidic) | |
| intracellular binding protein | 3.6 | |
| Wscr5 | Williams-Beuren syndrome chromosome | |
| region 5 homolog (human) | 3.6 | |
| Eppk1 | Epiplakin 1 | 3.6 |
| 2010004A03Rik | RIKEN cDNA 2010004A03 gene | 3.6 |
| Itgb5 | Integrin beta 5 | |
| gb: NM_010580 1417534_at | 3.5 | |
| gb: NM_010580 1417533_a_at | 3.3 | |
| Mlf1 | Myeloid leukemia factor 1 | 3.5 |
| Tnfrsf22 | Tumor necrosis factor receptor | |
| superfamily, member 22 | 3.5 | |
| Zdhhc2 | Zinc finger, DHHC domain containing 2 | 3.5 |
| Tnfaip2 | Tumor necrosis factor, alpha-induced protein 2 | 3.4 |
| Rrad | Ras-related associated with diabetes | 3.4 |
| A530090O15Rik | RIKEN cDNA A530090O15 gene | 3.4 |
| Chi3l4 | Chitinase 3-like 4 | 3.4 |
| Tnfrsf19 | Tumor necrosis factor receptor | |
| superfamily, member 19 | 3.4 | |
| Myo1b | Myosin IB | |
| gb: AI255256 | 3.4 | |
| gb: BI080370 | 3.2 | |
| Tuba4 | Tubulin, alpha 4 | 3.3 |
| Myo1g | Myosin IG | 3.3 |
| Siat10 | Sialyltransferase 10 | |
| (alpha-2,3-sialyltransferase VI) | 3.3 | |
| Nol3 | Nucleolar protein 3 | |
| (apoptosis repressor with CARD domain) | 3.3 | |
| Tpt1h | tRNA splicing 2’ phosphotransferase 1 | |
| homolog (S. cerevisiae) | 3.3 | |
| Igfbp6 | Insulin-like growth factor binding protein 6 | 3.3 |
| Ccnd1 | Cyclin D1 | |
| gb: M64403 | 3.2 | |
| gb: NM_007631 | 3.1 | |
| BC003236 | cDNA sequence BC003236 | 3.2 |
| 2010001C09Rik | RIKEN cDNA 2010001C09 gene | 3.2 |
| Chst1 | Carbohydrate (keratan sulfate Gal-6) | |
| sulfotransferase 1 | 3.2 | |
| Timp1 | Tissue inhibitor of metalloproteinase 1 | 3.2 |
| 4921530G04Rik | RIKEN cDNA 4921530G04 gene | 3.2 |
| Lxn | Latexin | 3.1 |
| Sgk2 | Serum/glucocorticoid regulated kinase 2 | 3.1 |
| 2310047E01Rik | RIKEN cDNA 2310047E01 gene | 3.1 |
| 2200002N01Rik | RIKEN cDNA 2200002N01 gene | 3 |
| Ptpre | Protein tyrosine phosphatase, receptor type, E | 3 |
| Psmb8 | Proteosome (prosome, macropain) subunit, beta | |
| type 8 (large multifunctional protease 7) | 3 | |
| Tm7sf1 | Transmembrane 7 superfamily member 1 | 3 |
According to the Gene Ontology (GO) classification and TreeView analysis, the genes are further divided into two groups: differential biological process profile and molecular function profile, as shown respectively in Tables 2, 3. Biological process refers to a biological objective to which the gene or gene product contributes. Molecular function is defined as the biochemical activity (including specific binding to ligands or structures) of a gene product[8].
Table 2.
Differential biological process profile in cell lines Hca-F vs Hca-P.
| Development | |||
| Itgb5 gb: NM_010580 1417533_a_at 3.3 | Ccnd1 gb: M64403 | 3.2 | |
| Mlf1 gb: NM_010580 1417534_at 3.5 | gb: NM_007631 | 3.1 | |
| Morphogenesis | |||
| Gja1 gb: BC006894 | 6.4 | Sema3b gb: BB116052 | 5.1 |
| gb:M63801 | 7.2 | gb:NM_009153 | 4.7 |
| Tnfaip2 | 3.4 | Tm4sf9 | 3.9 |
| Igfbp6 | 3.3 | Igfbp4 gb: NM_010517 | 6.3 |
| Egfr gb: AF275367 | 6.9 | gb: AA119124 | 4 |
| gb: U03425 | 3.6 | gb: BC019836 1423756_s_at 5.8 | |
| Efna1 gb: D38146 | 5.7 | gb: BC019836 1423757_x_at 4.1 | |
| gb: BC002046 | 4.2 | Eng | 4.5 |
| Cellular process | |||
| Cell communication | |||
| Cell adhesion | |||
| Mcam | 4.2 | Itgb5 gb: NM_010580 1417533_a_at 3.3 | |
| Tm4sf9 | 3.9 | gb: NM_010580 1417534_at 3.5 | |
| D7Ertd | |||
| 45 8e gb: BC013673 1423903_at 3.8 | Col8a1 | 4.9 | |
| gb: BB049138 1423904_a_at 4 | Eng | 4.5 | |
| gb: BB049138 1423905_at 3.9 | Pcdhb7 | 4.9 | |
| gb: NM_009310 4.2 | |||
| gb: BC013673 1451160_s_at 4 | |||
| Cell–cell signaling | |||
| Gja1 gb: BC006894 | 6.4 | ||
| gb: M63801 | 7.2 | ||
| Signal transduction | |||
| IL2rg gb: L20048 1416295_a_at 3.3 | Efna1 gb: BC002046 | 4.2 | |
| gb: L20048 1416296_at 4.3 | gb: D38146 | 5.7 | |
| Itgb5 gb: NM_010580 1417533_a_at 3.3 | Egfr gb: AF275367 | 6.9 | |
| gb: NM_010580 1417534_at 3.5 | gb: U03425 | 3.6 | |
| Dok1 | 3.6 | Fgf15 | 5.4 |
| Ptpre | 3 | Cdc42ep5 | 4.4 |
| Ramp3 | 3.6 | Sh3bp5 | 5.5 |
| Lepr | 6.7 | Ptprr | 4.1 |
| Eng | 4.5 | Ripk3 | 6.4 |
| F2r | 4.5 | R75183 gb: BC004774 | 7 |
| Rrad | 3.3 | gb: BB324973 | 5.5 |
| Rab3b | 5.6 | ||
| Cellular physiological process | |||
| Cell death | |||
| Ripk3 | 6.4 | Nol3 | 3.3 |
| Cell motility | |||
| Tm4sf9 | 3.9 | D7Ertd458e gb: BC013673 1423903_at | 3.8 |
| Cnn2 | 5.2 | gb: BB049138 1423904_a_at 4 | |
| gb: BB049138 1423905_at 3.9 | |||
| gb: NM_009310 4.2 | |||
| gb: BC013673 1451160_s_at 4 | |||
| Cell growth and/or maintenance | |||
| Transport | |||
| Tuba4 | 3.3 | Slc38a4 gb: NM_027052 | 9 |
| Ramp3 | 3.6 | gb: AK003626 | 3.4 |
| Rab3b | 5.6 | Cav | 5.8 |
| Scn8a | 4 | ||
| Cell organization and biogenesis | |||
| Igfbp6 | 3.3 | Igfbp4 gb: NM_010517 | 6.3 |
| Egfr gb: AF275367 | 6.9 | gb: AA119124 | 4 |
| gb: U03425 | 3.6 | gb: BC019836 1423756_s_at 5.8 | |
| AFFX-18SRNAMur | X00686_M_at 5.1 | gb: BC019836 1423757_x_at 4.1 | |
| Microtubule-based process | |||
| Tua4 | 3.3 | ||
| Cytoskeleton organization and biogenesis | |||
| Krt1-19 | 7.4 | Krt2-8 gb: M21836 | 8.6 |
| Tuba4 | 3.3 | gb: NM_031170 | 4.8 |
| Krt2-7 | 5.2 | Myo1b gb: AI255256 | 3.4 |
| Krt1-18 | 5.1 | gb: BI080370 | 3.2 |
| Cell proliferation | |||
| Tm4sf9 | 3.9 | Pla2g1b | 6.4 |
| Cell cycle | |||
| Ccnd1 gb: M64403 | 3.2 | Egfr gb: AF275367 | 6.9 |
| gb: NM_007631 | 3.1 | gb: U03425 | 3.6 |
| Axl | 4 | ||
| Regulation of cellular process | |||
| Igfbp6 | 3.3 | Igfbp4 gb: NM_010517 | 6.3 |
| Ramp3 | 3.6 | gb: AA119124 | 4 |
| gb: BC019836 1423756_s_at 5.8 | |||
| gb: BC019836 1423757_x_at 4.1 | |||
| Cell differentiation | |||
| Ccnd1 gb: M64403 | 3.2 | Mlf1 | 3.5 |
| gb: NM_007631 | 3.1 | ||
| Regulation of biological process | |||
| Regulation of cellular process | |||
| Igfbp6 | 3.3 | Igfbp4 gb: NM_010517 | 6.3 |
| Ramp3 | 3.6 | gb: BC019836 1423756_s_at 5.8 | |
| Sh3bp5 | 5.5 | gb: BC019836 1423757_x_at 4.1 | |
| gb: AA119124 | 4 | ||
| Regulation of physiological process | |||
| Gja1 gb: BC006894 | 6.4 | Procr | 4.6 |
| gb: M63801 | 7.2 | ||
| Behavior | |||
| Scn8a | 4 | ||
| Nr1d1 | 4.6 | ||
| Physiological process | |||
| Metabolism | |||
| Pla2g1b | 6.4 | Pla2g7 | 4.4 |
| Psmb8 | 3 | 2310047E01Rik | 3.1 |
| Fbp2 | 7.1 | 3.3 | |
| Protein metabolism/phosphorus metabolism | |||
| A530090O15Rik | 3.4 | Axl | 4 |
| Ccnd1 gb: M64403 | 3.2 | Egfr gb: AF275367 | 6.9 |
| gb: NM_007631 | 3.1 | gb: U03425 | 3.6 |
| Krt2-8 gb: M21836 | 8.6 | Mak | 3.9 |
| gb: NM_031170 | 4.8 | Ptpn8 | 5.6 |
| Ptpre | 3 | Ptprr | 4.1 |
| Ripk3 | 6.4 | Sgk2 | 3.1 |
| Nucleobase, nucleoside, nucleotide and nucleic acid metabolism | |||
| Nol3 | 3.3 | Lepr | 6.7 |
| Transcription | |||
| Fosl1 gb: NM_010235 | 5 | Ankrd1 gb: NM_013468 | 5.3 |
| gb: U34245 | 4.4 | gb: AK009959 | 3.6 |
| Nfil3 | 4.6 | Nr1d1 | 4.6 |
| Regulation of physiological process | |||
| Gja1 gb: BC006894 | 6.4 | Procr | 4.6 |
| gb: M63801 | 7.2 | ||
| Coagulation | |||
| Procr | 4.6 | F2r | 4.5 |
| Organismal physiological process | |||
| Chi3l3 | 4.1 | Chi3l4 | 3.4 |
| Csf3 | 4.7 | Daf1 | 5.9 |
| F2r | 4.5 | Gja1 gb: BC006894 | 6.4 |
| IL24 | 5.9 | gb: M63801 | 7.2 |
| Pla2g7 | 4.4 | Procr | 4.6 |
| Mus musculus | |||
| transcribed sequences | 3.8 | Psmb8 | 3 |
| Response to stimulus | |||
| Chi3l3 | 4.1 | Chi3l4 | 3.4 |
| Csf3 | 4.7 | Daf1 | 5.9 |
| F2r | 4.5 | IL24 | 5.9 |
| Gja1 gb: BC006894 | 6.4 | Krt2-8 gb: NM_031170 | 4.8 |
| gb: M63801 | 7.2 | gb: M21836 | 8.6 |
| Pla2g1b | 6.4 | Pla2g7 | 4.4 |
| Psmb8 | 3 | Serpinh1 | 4 |
| Mus musculus transcribed sequences | 3.8 | ||
Table 3.
Differential molecular function profile in cell lines Hca-F vs Hca-P.
| Transporter activity | |||
| Gja1 gb: BC006894 | 6.4 | Slc38a4 gb: AK003626 | 3.4 |
| gb: M63801 | 7.2 | gb: NM_027052 | 9 |
| Ramp3 | 3.6 | Rab3b | 5.6 |
| Scn8a | 4 | ||
| Tptih | 3.3 | ||
| Structural molecule activity | |||
| Eppk1 | 3.6 | Cldn9 | 7.4 |
| Col8a1 | 4.9 | Krt1-19 | 7.4 |
| Tuba4 | 3.3 | Krt2-7 | 5.2 |
| Krt2-8 gb: NM_031170 | 4.8 | Krt1-18 | 5.1 |
| gb: M21836 | 8.6 | ||
| Chaperone activity | |||
| Serpinh1 | 4 | Sncg | 5 |
| Motor activity | |||
| Myo1b gb: BI080370 | 3.2 | Myo1g | 3.3 |
| gb: AI255256 | 3.4 | ||
| Catalytic activity | |||
| Gcnt2 | 4.2 | Siat10 | 3.3 |
| Chst1 | 3.2 | Loxl2 | 3.7 |
| Ltb4dh | 5.2 | 2310047E01Rik | 3.1 |
| Hydrolase activity | |||
| Pla2g1b | 6.4 | Smpd2 | 4.3 |
| Abhd3 | 3.6 | Ptpn8 | 5.6 |
| Ptpre | 3 | Chi3l3 | 4.1 |
| Rrad | 3.4 | Rab3b | 5.6 |
| Chi3l4 | 3.4 | Ptprr | 4.1 |
| Pla2g7 | 4.4 | Fbp2 | 7.1 |
| Psmb8 | 3 | ||
| Kinase activity | |||
| Ccnd1 gb: M64403 | 3.2 | Krt2-8 gb: NM_031170 | 4.8 |
| gb: NM_007631 | 3.1 | gb: M21836 | 8.6 |
| A530090O15Rik | 3.4 | ||
| Protein-tyrosine kinase activity | |||
| Sgk2 | 3.1 | Egfr gb: AF275367 | 6.9 |
| Axl | 4 | gb: U03425 | 3.6 |
| Ripk3 | 6.4 | ||
| Transmembrane receptor protein kinase activity | |||
| Egfr gb: AF275367 | 6.9 | ||
| gb: U03425 | 3.6 | ||
| Protein serine/threonine kinase activity | |||
| Sgk2 | 3.1 | Mak | 3.9 |
| Axl | 4 | Egfr gb: AF275367 | 6.9 |
| Ripk3 | 6.4 | gb: U03425 | 3.6 |
| Transferase activity | |||
| A530090O15Rik | 3.4 | Axl | 4 |
| Ccnd1 gb: M64403 | 3.2 | Egfr gb: AF275367 | 6.9 |
| gb: NM_007631 | 3.1 | gb: U03425 | 3.6 |
| Chst1 | 3.2 | Gcnt2 | 4.2 |
| Krt2-8 gb: NM_031170 | 4.8 | Mak | 3.9 |
| gb: M21836 | 8.6 | Ripk3 | 6.4 |
| Sgk2 | 3.1 | Siat10 | 3.3 |
| Enzyme regulator activity | |||
| Ccnd1 gb: M64403 | 3.2 | Lxn | 3.1 |
| gb: NM_007631 | 3.1 | Timp1 | 3.2 |
| Sh3bp5 | 5.5 | Cd109 | 5.9 |
| 1600023A02Rik | 5.3 | Serpinh1 | 4 |
| Binding | |||
| Nucleic acid binding | |||
| Fosl1 gb: NM_010235 | 5 | Ankrd1 gb: NM_013468 | 5.3 |
| gb: U34245 | 4.3 | gb: AK009959 | 3.6 |
| Nr1d1 | 4.6 | ||
| Metal ion binding | |||
| Pla2g1b | 6.4 | Smpd2 | 4.3 |
| Ltb4dh | 5.2 | Scn8a | 4 |
| 2310047E01Rik | 3.1 | Pcdhb7 | 4.9 |
| 2810003C17Rik | 4.6 | Loxl2 | 3.7 |
| Zdhhc2 | 3.5 | ||
| Nucleotide binding | |||
| A530090O15Rik | 3.4 | Axl | 4 |
| Egfr gb: AF275367 | 6.9 | Krt2-8 gb: NM_031170 | 4.8 |
| gb: U03425 | 3.6 | gb: M21836 | 8.6 |
| Mak | 3.9 | Rab3b | 5.6 |
| Myo1b gb: BI080370 | 3.2 | Ripk3 | 6.4 |
| gb: AI255256 | 3.4 | Rrad | 3.4 |
| Scn8a | 4 | Sgk2 | 3.1 |
| Tuba4 | 3.3 | ||
| Receptor binding | |||
| Areg | 4.3 | Csf3 | 4.7 |
| Dok1 | 3.6 | Fgf15 | 5.4 |
| Il24 | 5.9 | Pla2g1b | 6.4 |
| Protein binding | |||
| Ankrd1 gb: NM_013468 | 5.3 | Ccnd1 gb: M64403 | 3.2 |
| gb: AK009959 | 3.6 | gb: NM_007631 | 3.1 |
| Cav | 5.8 | Cdc42ep5 | 4.4 |
| Col8a1 | 4.9 | Eng | 4.5 |
| D7Ertd458e | |||
| gb: BC013673 1423903_at 3.8 | Egfr gb: AF275367 | 6.9 | |
| gb: BB049138 1423904_a_at 4 | gb: U03425 | 3.6 | |
| gb: BB049138 1423905_at 3.9 | Fibp | 3.6 | |
| gb: NM_009310 4.2 | IL2rg gb: L20048 1416295_a_at 3.3 | ||
| gb: BC013673 1451160_s_at 4 | gb: L20048 1416296_at 4.3 | ||
| Itgb5 gb: NM_010580 | 3.5 | Igfbp6 | 3.3 |
| gb: NM_010580 | 3.3 | Lepr | 6.7 |
| Nol3 | 3.3 | Pcdhb7 | 4.9 |
| Procr | 4.6 | Ptpre | 3 |
| Rab3b | 5.6 | Rrad | 3.4 |
| Sh3bp5 | 5.5 | Tnfrsf22 | 3.5 |
| Fscn1 gb: NM_007984 1416514_a_at 5.4 | Myo1b gb: BI080370 | 3.2 | |
| gb: BE952057 | 4.2 | gb: AI255256 | 3.4 |
| gb: NM_007984 1448378_at 3.7 | Cnn2 | 5.2 | |
| Carbohydrate binding | |||
| Chi3l3 | 4.1 | Chi3l4 | 3.4 |
| Signal transducer activity | |||
| Dok1 | 3.6 | Ripk3 | 6.4 |
| Receptor activity | |||
| Axl | 4 | Itgb5 gb: NM_010580.1 | 3.5 |
| D7Ertd458e gb: BC013673 1423903_at 3.8 | gb: NM_010580.1 | 3.3 | |
| gb: BB049138 1423904_a_at 4 | Nr1d1 | 4.6 | |
| gb: BB049138 1423905_at 3.9 | Procr | 4.6 | |
| gb: NM_009310 4.2 | Ptpn8 | 5.6 | |
| gb: BC013673 1451160_s_at 4 | Ptprr | 4.1 | |
| Ramp3 | 3.6 | Tnfrsf19 | 3.4 |
| Tnfrsf22 | 3.5 | Lepr | 6.7 |
| IL2rg | gb: L20048.1 1416295_a_at 3.3 | Egfr gb: AF275367.1 | 6.9 |
| gb: L20048.1 1416296_at 4.3 | gb: U03425.1 | 3.6 | |
| F2r | 4.5 | ||
DISCUSSION
We used an Affymetrix GeneChip® MOE430A to identify lymphatic metastasis-associated genes in two hepatocarcinoma cell lines with different lymphatic metastasis potential. Based on the selection criteria for up-regulated expression discussed in “MATERIALS AND METHODS”, 110 differential genes were observed in the highly lymphogenous metastatic cell line. The over expressed genes were then classified according to the GO classification and TreeView analysis.
In the category development, we found three genes associated with angiogenesis: endoglin (EDG; CD105), ephrin A1 and Tnfaip2. Tumor angiogenesis plays an important role in tumor growth and metastasis[9] and certain angiogenesis markers may be useful as metastasis markers and/or the targets for antiangiogenic therapy[10]. EDG was thought to be a proliferation-associated antigen of endothelial cells and essential for angiogenesis. Elevated serum EDG was associated with metastasis in patients with colorectal, breast, and other solid tumors and chemotherapy exerts a suppression effect on the serum EDG[11,12]. In endometrial carcinoma, EDG counts correlated significantly with the presence of angiolymphatic invasion, lymph nodes metastasis and tumor stage[9]. Ephrin-A1, formerly called B61, was found to be up-regulated during melanoma progression and implicated in angiogenesis[13,14]. Tnfaip2 (B94), originally identified as a tumor necrosis factor alpha-inducible gene in endothelial cells, was highly expressed in marrow from patients with acute myelogenous leukemia French-American-British subtypes M0-M2[15], but its correlation with metastasis requires to be elucidated.
Adaptation of cell adhesion functions of the tumor cells to successfully overcome the different hurdles in the metastatic cascade is a prerequisite for metastasis[16]. We noted up-regulation of MCAM (CD146; Mel-CAM; Muc18) in Hca-F cell line. Mcam, a member of the immunoglobulin superfamily and homologous to several cell adhesion molecules, was associated with tumor progression and the development of metastasis in human malignant melanoma and also was an important determinant in increasing metastasis of human prostate cancer LNCaP cells to distant organs in a nude mouse model[17-19]. We also noted over expression of integrin β5, Col8A1 (procollagen, type VIII, alpha 1) and Pcdhb7 (protocadherin beta) in the Hca-F cell line.
In the category signal transduction, we observed up-regulation of Cdc42ep5 (CEP5; Borg3), Rab3b, Lepr (leptin receptor), Ptprr (protein tyrosine phosphatase, receptor type, R) and F2r (coagulation factor II (thrombin) receptor; Par1; ThrR). Cdc42ep5, one member of CEPs which acts downstream of Cdc42 to induce actin filament assembly leading to cell shape changes, induced pseudopodia formation in NIH-3T3 fibroblasts[20]. In tumor, it might promote the ability of invasiveness and metastasis. In the highly lymphogenous metastatic pancreatic carcinoma cell line BSp73-ASML, the ras-related rab proteins and protein tyrosine phosphatases were all over expressed[16]. Lepr positive correlated significantly with distant metastasis and lower survival in breast cancer[21]. F2r, protease-activated receptor 1, a G protein-coupled receptor for thrombin, was shown to be preferentially expressed in highly lymphogenous metastatic pancreatic carcinoma cell line BSp73-ASML[16] and correlated with breast carcinoma cell invasion and metastasis[22,23]. Booden et al[24] also reported that altered trafficking of proteolytically activated PAR1 (F2r) caused sustained activation of phosphoinositide hydrolysis and extracellular signal-regulated kinase signaling, even after thrombin withdrawal, and enhanced breast carcinoma cellular invasion.
The ability to locomote and migrate is fundamental to the acquisition of invasive and metastatic properties by tumor cells[25]. D7Ertd458e (necl-5), one of the five nectin-like molecules (necls), which have domain structures similar to those of nectins, has recently been identified and appears to play different roles from those of nectins. Experiments showed that enhanced motility and metastasis of V12Ras-NIH3T3 cells (NIH3T3 cells transformed by an oncogenic Ki-Ras) were at least partly the result of up-regulated Necl-5, which does not homophilically trans-interact, but heterophilically trans-interacts with nectin-3, regulates cell migration and adhesion[26,27].
In the category transport, Slc38a4 was detected to overexpress in the highly metastatic cell line. Recent work has considered SLC38 transporters as therapeutic targets in neoplasia[28]. Although to date Slc38a4 has not been reported to be correlated with tumor metastasis straightly, the member of the solute carrier family SLC35, which encodes nucleotide sugar transporters, has been shown to be involved in tumor metastasis[29] and SLC16 and SLC2 were up-regulated in highly lymphogenous metastatic pancreatic carcinoma cell line BSp73-ASML[16]. Meanwhile, the reason Slc38a4 deserves further attention is that it differs most in our study.
The state of tubulin polymerization associates with tumor metastasis and increased depolymerized form of tubulin could promote metastasis. We noted Tuba4 over expression in Hca-F cell line. Changes in the expression of genes for the cytoskeleton organization and biogenesis mediate adaptation to increased motility and invasion of the metastatic tumor cell[16]. Krt1-19 (keratin 19), Krt1-18 (keratin 18), Krt2-7 (keratin 7) and Krt2-8 (keratin 8) were up regulated in the highly metastatic cell line Hca-F. Expressive changes of these genes have been reported to be correlated with the invasive and metastatic phenotype[16,30].
A remarkable feature in our study is the increased steady state level of the mRNA for cyclin D1 in the category cell cycle. Cyclin D1 is a nuclear protein that plays an important role in regulating the cell cycle by promoting entry of cells from the G1 to S phase due to interaction with its catalytic partner cdk4 or with the extradiol receptor. Over expression of cyclinD1 was associated with the liability of lymph node metastasis and the poor prognosis for patient with laryngeal squamous cell carcinoma, esophageal carcinoma, mammary infiltrating duct carcinoma, oral squamous cell carcinoma and papillary thyroid carcinoma[31-35]. mRNA for cyclin D1 was also found to be over expressed in lymph node metastases of breast carcinoma by comparison of gene expression profiles with their primary counterparts[36].
In the category transcription, we observed another feature of our system, i.e., the increased expression of Fosl1 (Fra1; fra-1). Fosl1 encodes a transcription factor, which was found over expressed in highly aggressive breast carcinoma cell lines and lymphogenous metastatic pancreatic carcinoma[16,37]. It was reported that Fosl1 induces transformation and invasiveness of human epithelial adenocarcinoma cells[38]. In addition, we identified up-regulation of NR1D1, a member of the orphan receptor superfamily. It was coexpressed with ERBB2 in 34 breast cancer biopsies and also mapped within the same chromosomal location as the ERBB2 gene[39].
In the present study, we found over expression of heat-shock protein Serpin h1 (HSP47) and SNCG (persyn; breast cancer-specific protein 1) in the category chaperone activity. HSP47 is a stress-inducible glycoprotein of Mr 47000 molecular weight and is assumed to be a collagen-specific molecular chaperone. Tumor cell lines, which were derived from metastatic carcinomas and were still metastatic in animals, synthesized higher levels of HSP47[40]. SNCG, the third member of a neuronal protein family synuclein, is a new chaperone protein in the Hsp-based multiprotein chaperone complex for the stimulation of ligand-dependent ER-alpha signaling and thus stimulates hormone-responsive mammary tumorigenesis, and is also highly associated with breast or ovarian cancer progression[41]. In addition, aberrant SNCG gene expression can occur via CpG island demethylation, and tends to occur during the more progressive stages of gastric carcinogenesis[42].
The motor activity of tumor cell plays an important role in invasiveness and metastasis. Our results revealed the up-regulation of Myosin IB and Myosin IG which are two members of the myosin I family of motor proteins. Myosins are a large family of structurally diverse motor proteins. Each myosin utilizes energy from ATP hydrolysis to generate force for indirectional movement along actin filaments[43]. It has been reported that myosin VI, a motor protein that regulates border cell migration, was abundantly expressed in high-grade ovarian carcinomas but not in normal ovary and ovarian cancers that behave indolently. Inhibiting myosin VI expression in high-grade ovarian carcinoma cells impeded cell spreading and migration in vitro[44].
Another hallmark of our system is the overexpression of mRNAs coding for kinase activity, such as Sgk2, AXL, Mak and EGFR. EGFR belongs to the family of type I receptor tyrosine kinase. Over expression of EGFR often correlates with an aggressive tumor phenotype and poor prognosis[16,45-49]. AXL, another member of a family of receptor tyrosine kinases, has been described to act as a mitogenic factor along with its ligand Gas-6 and has also shown to have a role in apoptosis, cell adhesion, and chemotaxis. There was a significant increase in the steady-state levels of Axl or its mRNA in a variety of cancers. Meanwhile, in colon cancer Axl receptor tyrosine kinase was expressed highly in a peritoneal metastatic nodule than in primary malignant tissues and in papillary thyroid carcinomas solid component and invasive front tended to over express Axl[50-54]. These indicated that Axl might be related to the tumorigenesis and tumor progression. Sgk, a serine/threonine protein kinase, was found up-regulation in the tumorigenic HeLa cells compared to nontumorigenic HeLa cells which came from fusion of tumorigenic HeLa cells with human skin fibroblasts[55]. Male germ cell-associated kinase (Mak) was shown to be up-regulated in prostate cancer cell lines than those of normal prostate epithelial cells[56].
In the category binding, Loxl2 gene expression was up regulated. Loxl2, a copper-containing amine oxidase, belongs to the LOX family which functions as extracellular matrix modulating enzyme. LOX and LOX family members LOXL2, LOXL3, and LOXL4 were observed only in breast cancer cells with a highly invasive/metastatic phenotype but not in poorly invasive/nonmetastatic breast cancer cells[57]. We also found Areg (AR) over expressed in the highly metastatic hepatocarcinoma cell line. Areg is one of the ligands of EGFR. Concomitant presence of the EGF receptor and its ligands EGF, TGF-alpha, and/or amphiregulin Areg is associated with enhanced tumor aggressiveness and shorter postoperative survival[16,58-60]. EGF and AR might modulate invasion by increasing the expression of MMPs[61] or stimulating directional (chemotactic) and/or random (chemokinetic) motility in malignant cells[62]. In addition, the mRNA for caveolin (Cav; Cav-1) was up regulated in the highly metastatic cell line. Cav-1 is a major structural component of caveolae of plasma membranes. It was identified as a metastasis-related gene and/or a worse prognostic predictor in prostate carcinoma, renal cell carcinoma, esophageal squamous cell carcinoma, lung adenocarcinoma and colorectal cancer[63-68]. Cav-1 was reported to be necessary for mediating filopodia formation in lung adenocarcinoma, which may enhance the invasive ability of cancer cells[67]. In an other study, caveolin-1 was shown to affect angiogenesis during the progression of clear cell renal cell carcinoma[69].
Taken together, we found that the metastatic phenotype of the highly metastatic mouse hepatocarcinoma cell line Hca-F is accompanied by marked differences in its transcriptional profile in comparison with the low metastatic cell line Hca-P. A large number of genes and their cellular functions, such as angiogenesis, cell adhesion, signal transduction, cell motility, transport, microtubule-based process, cytoskeleton organization and biogenesis, cell cycle, transcription, chaperone activity, motor activity, protein kinase activity, receptor binding and protein binding, might be involved in the process of lymphatic metastasis and deserve to be used as potential candidates for further investigation. We selected cyclin D1, Fosl1, Hsp47, EGFR and AR, and Cav-1 as the possible candidate/key genes of the metastatic phenotype, which needed to be validated in later experiments. Besides these genes, several other genes which have not been validated to contribute to enhanced tumor metastatic properties straightly deserve further attention, for example, Slc38a4 and Cldn9. ESTs (data were not presented) might indicate novel genes associated with lymphatic metastasis and also need attention. Our next work is to identify the candidate genes/pathway responsible for lymphogenous metastasis, because although a large number of genes are associated with the metastasis, some of the changes are believed to be the secondary events; the expression changes as a result of metastasis rather than as an initiator of the metastasis event[1]. The elucidation of the candidate genes/pathway might not only provide useful diagnostic markers for tumor lymphogenous metastasis, but also more importantly, provide novel therapeutic targets.
Footnotes
Supported by the National Natural Science Foundation of China, No. 30371583
Edited by Guo SY Language Editor Elsevier HK
References
- 1.Cheung ST, Chen X, Guan XY, Wong SY, Tai LS, Ng IO, So S, Fan ST. Identify metastasis-associated genes in hepatocellular carcinoma through clonality delineation for multinodular tumor. Cancer Res. 2002;62:4711–4721. [PubMed] [Google Scholar]
- 2.Fidler IJ. Critical factors in the biology of human cancer metastasis: twenty-eighth G.H.A. Clowes memorial award lecture. Cancer Res. 1990;50:6130–6138. [PubMed] [Google Scholar]
- 3.Iizuka N, Oka M, Yamada-Okabe H, Mori N, Tamesa T, Okada T, Takemoto N, Tangoku A, Hamada K, Nakayama H, et al. Comparison of gene expression profiles between hepatitis B virus- and hepatitis C virus-infected hepatocellular carcinoma by oligonucleotide microarray data on the basis of a supervised learning method. Cancer Res. 2002;62:3939–3944. [PubMed] [Google Scholar]
- 4.Masui T, Nakanishi H, Inada K, Imai T, Mizoguchi Y, Yada H, Futakuchi M, Shirai T, Tatematsu M. Highly metastatic hepatocellular carcinomas induced in male F344 rats treated with N-nitrosomorpholine in combination with other hepatocarcinogens show a high incidence of p53 gene mutations along with altered mRNA expression of tumor-related genes. Cancer Lett. 1997;112:33–45. doi: 10.1016/s0304-3835(96)04543-0. [DOI] [PubMed] [Google Scholar]
- 5.Hou L, Li Y, Jia YH, Wang B, Xin Y, Ling MY, Lü S. Molecular mechanism about lymphogenous metastasis of hepatocarcinoma cells in mice. World J Gastroenterol. 2001;7:532–536. doi: 10.3748/wjg.v7.i4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang MC, Ruan QG, Yang JJ, Eckenrode S, Wu S, McIndoe RA, She JX. A statistical method for flagging weak spots improves normalization and ratio estimates in microarrays. Physiol Genomics. 2001;7:45–53. doi: 10.1152/physiolgenomics.00020.2001. [DOI] [PubMed] [Google Scholar]
- 7.Li C, Wong WH. Model-based analysis of oligonucleotide arrays: expression index computation and outlier detection. Proc Natl Acad Sci USA. 2001;98:31–36. doi: 10.1073/pnas.011404098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saad RS, Jasnosz KM, Tung MY, Silverman JF. Endoglin (CD105) expression in endometrial carcinoma. Int J Gynecol Pathol. 2003;22:248–253. doi: 10.1097/01.PGP.0000070852.25718.37. [DOI] [PubMed] [Google Scholar]
- 10.Seon BK, Takahashi N, Haba A, Matsuno F, Haruta Y, She XW, Harada N, Tsai H. Angiogenesis and metastasis marker of human tumors. Rinsho Byori. 2001;49:1005–1013. [PubMed] [Google Scholar]
- 11.Takahashi N, Kawanishi-Tabata R, Haba A, Tabata M, Haruta Y, Tsai H, Seon BK. Association of serum endoglin with metastasis in patients with colorectal, breast, and other solid tumors, and suppressive effect of chemotherapy on the serum endoglin. Clin Cancer Res. 2001;7:524–532. [PubMed] [Google Scholar]
- 12.Li C, Guo B, Wilson PB, Stewart A, Byrne G, Bundred N, Kumar S. Plasma levels of soluble CD105 correlate with metastasis in patients with breast cancer. Int J Cancer. 2000;89:122–126. doi: 10.1002/(sici)1097-0215(20000320)89:2<122::aid-ijc4>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 13.Straume O, Akslen LA. Importance of vascular phenotype by basic fibroblast growth factor, and influence of the angiogenic factors basic fibroblast growth factor/fibroblast growth factor receptor-1 and ephrin-A1/EphA2 on melanoma progression. Am J Pathol. 2002;160:1009–1019. doi: 10.1016/S0002-9440(10)64922-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Easty DJ, Hill SP, Hsu MY, Fallowfield ME, Florenes VA, Herlyn M, Bennett DC. Up-regulation of ephrin-A1 during melanoma progression. Int J Cancer. 1999;84:494–501. doi: 10.1002/(sici)1097-0215(19991022)84:5<494::aid-ijc8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 15.Rusiniak ME, Yu M, Ross DT, Tolhurst EC, Slack JL. Identification of B94 (TNFAIP2) as a potential retinoic acid target gene in acute promyelocytic leukemia. Cancer Res. 2000;60:1824–1829. [PubMed] [Google Scholar]
- 16.Tarbé N, Lösch S, Burtscher H, Jarsch M, Weidle UH. Identification of rat pancreatic carcinoma genes associated with lymphogenous metastasis. Anticancer Res. 2002;22:2015–2027. [PubMed] [Google Scholar]
- 17.Sers C, Kirsch K, Rothbächer U, Riethmüller G, Johnson JP. Genomic organization of the melanoma-associated glycoprotein MUC18: implications for the evolution of the immunoglobulin domains. Proc Natl Acad Sci USA. 1993;90:8514–8518. doi: 10.1073/pnas.90.18.8514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu GJ, Peng Q, Fu P, Wang SW, Chiang CF, Dillehay DL, Wu MW. Ectopical expression of human MUC18 increases metastasis of human prostate cancer cells. Gene. 2004;327:201–213. doi: 10.1016/j.gene.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Wu GJ, Varma VA, Wu MW, Wang SW, Qu P, Yang H, Petros JA, Lim SD, Amin MB. Expression of a human cell adhesion molecule, MUC18, in prostate cancer cell lines and tissues. Prostate. 2001;48:305–315. doi: 10.1002/pros.1111. [DOI] [PubMed] [Google Scholar]
- 20.Hirsch DS, Pirone DM, Burbelo PD. A new family of Cdc42 effector proteins, CEPs, function in fibroblast and epithelial cell shape changes. J Biol Chem. 2001;276:875–883. doi: 10.1074/jbc.M007039200. [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa M, Kitayama J, Nagawa H. Enhanced expression of leptin and leptin receptor (OB-R) in human breast cancer. Clin Cancer Res. 2004;10:4325–4331. doi: 10.1158/1078-0432.CCR-03-0749. [DOI] [PubMed] [Google Scholar]
- 22.Even-Ram S, Uziely B, Cohen P, Grisaru-Granovsky S, Maoz M, Ginzburg Y, Reich R, Vlodavsky I, Bar-Shavit R. Thrombin receptor overexpression in malignant and physiological invasion processes. Nat Med. 1998;4:909–914. doi: 10.1038/nm0898-909. [DOI] [PubMed] [Google Scholar]
- 23.Henrikson KP, Salazar SL, Fenton JW, Pentecost BT. Role of thrombin receptor in breast cancer invasiveness. Br J Cancer. 1999;79:401–406. doi: 10.1038/sj.bjc.6690063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Booden MA, Eckert LB, Der CJ, Trejo J. Persistent signaling by dysregulated thrombin receptor trafficking promotes breast carcinoma cell invasion. Mol Cell Biol. 2004;24:1990–1999. doi: 10.1128/MCB.24.5.1990-1999.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nabi IR, Watanabe H, Raz A. Autocrine motility factor and its receptor: role in cell locomotion and metastasis. Cancer Metastasis Rev. 1992;11:5–20. doi: 10.1007/BF00047599. [DOI] [PubMed] [Google Scholar]
- 26.Takai Y, Irie K, Shimizu K, Sakisaka T, Ikeda W. Nectins and nectin-like molecules: roles in cell adhesion, migration, and polarization. Cancer Sci. 2003;94:655–667. doi: 10.1111/j.1349-7006.2003.tb01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ikeda W, Kakunaga S, Takekuni K, Shingai T, Satoh K, Morimoto K, Takeuchi M, Imai T, Takai Y. Nectin-like molecule-5/Tage4 enhances cell migration in an integrin-dependent, Nectin-3-independent manner. J Biol Chem. 2004;279:18015–18025. doi: 10.1074/jbc.M312969200. [DOI] [PubMed] [Google Scholar]
- 28.Mackenzie B, Erickson JD. Sodium-coupled neutral amino acid (System N/A) transporters of the SLC38 gene family. Pflugers Arch. 2004;447:784–795. doi: 10.1007/s00424-003-1117-9. [DOI] [PubMed] [Google Scholar]
- 29.Ishida N, Kawakita M. Molecular physiology and pathology of the nucleotide sugar transporter family (SLC35) Pflugers Arch. 2004;447:768–775. doi: 10.1007/s00424-003-1093-0. [DOI] [PubMed] [Google Scholar]
- 30.Wauters CC, Smedts F, Gerrits LG, Bosman FT, Ramaekers FC. Keratins 7 and 20 as diagnostic markers of carcinomas metastatic to the ovary. Hum Pathol. 1995;26:852–855. doi: 10.1016/0046-8177(95)90006-3. [DOI] [PubMed] [Google Scholar]
- 31.Lim SC. Role of COX-2, VEGF and cyclin D1 in mammary infiltrating duct carcinoma. Oncol Rep. 2003;10:1241–1249. [PubMed] [Google Scholar]
- 32.Zhang L, Xu Y, Ge Y, Yu Y, Yu L. Expression of p27 protein and cyclinD1 in laryngeal carcinoma. LinChuang ErBiYanHouKe ZaZhi. 2002;16:646–647. [PubMed] [Google Scholar]
- 33.Nakashima S, Natsugoe S, Matsumoto M, Kijima F, Miyazono F, Ishigami S, Baba M, Takao S, Aikou T. Biological properties of biopsy specimens are useful for predicting lymph node micrometastasis in esophageal carcinoma. Anticancer Res. 2002;22:2951–2956. [PubMed] [Google Scholar]
- 34.Khoo ML, Beasley NJ, Ezzat S, Freeman JL, Asa SL. Overexpression of cyclin D1 and underexpression of p27 predict lymph node metastases in papillary thyroid carcinoma. J Clin Endocrinol Metab. 2002;87:1814–1818. doi: 10.1210/jcem.87.4.8353. [DOI] [PubMed] [Google Scholar]
- 35.Miyashita H, Uchida T, Mori S, Echigo S, Motegi K. Expression status of Pin1 and cyclins in oral squamous cell carcinoma: Pin1 correlates with Cyclin D1 mRNA expression and clinical significance of cyclins. Oncol Rep. 2003;10:1045–1048. [PubMed] [Google Scholar]
- 36.Hao X, Sun B, Hu L, Lähdesmäki H, Dunmire V, Feng Y, Zhang SW, Wang H, Wu C, Wang H, et al. Differential gene and protein expression in primary breast malignancies and their lymph node metastases as revealed by combined cDNA microarray and tissue microarray analysis. Cancer. 2004;100:1110–1122. doi: 10.1002/cncr.20095. [DOI] [PubMed] [Google Scholar]
- 37.Zajchowski DA, Bartholdi MF, Gong Y, Webster L, Liu HL, Munishkin A, Beauheim C, Harvey S, Ethier SP, Johnson PH. Identification of gene expression profiles that predict the aggressive behavior of breast cancer cells. Cancer Res. 2001;61:5168–5178. [PubMed] [Google Scholar]
- 38.Kustikova O, Kramerov D, Grigorian M, Berezin V, Bock E, Lukanidin E, Tulchinsky E. Fra-1 induces morphological transformation and increases in vitro invasiveness and motility of epithelioid adenocarcinoma cells. Mol Cell Biol. 1998;18:7095–7105. doi: 10.1128/mcb.18.12.7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dressman MA, Baras A, Malinowski R, Alvis LB, Kwon I, Walz TM, Polymeropoulos MH. Gene expression profiling detects gene amplification and differentiates tumor types in breast cancer. Cancer Res. 2003;63:2194–2199. [PubMed] [Google Scholar]
- 40.Morino M, Tsuzuki T, Ishikawa Y, Shirakami T, Yoshimura M, Kiyosuke Y, Matsunaga K, Yoshikumi C, Saijo N. Specific expression of HSP47 in human tumor cell lines in vitro. In Vivo. 1997;11:17–21. [PubMed] [Google Scholar]
- 41.Jiang Y, Liu YE, Goldberg ID, Shi YE. Gamma synuclein, a novel heat-shock protein-associated chaperone, stimulates ligand-dependent estrogen receptor alpha signaling and mammary tumorigenesis. Cancer Res. 2004;64:4539–4546. doi: 10.1158/0008-5472.CAN-03-3650. [DOI] [PubMed] [Google Scholar]
- 42.Yanagawa N, Tamura G, Honda T, Endoh M, Nishizuka S, Motoyama T. Demethylation of the synuclein gamma gene CpG island in primary gastric cancers and gastric cancer cell lines. Clin Cancer Res. 2004;10:2447–2451. doi: 10.1158/1078-0432.ccr-03-0107. [DOI] [PubMed] [Google Scholar]
- 43.Voigt H, Olivo JC, Sansonetti P, Guillén N. Myosin IB from Entamoeba histolytica is involved in phagocytosis of human erythrocytes. J Cell Sci. 1999;112(Pt 8):1191–1201. doi: 10.1242/jcs.112.8.1191. [DOI] [PubMed] [Google Scholar]
- 44.Yoshida H, Cheng W, Hung J, Montell D, Geisbrecht E, Rosen D, Liu J, Naora H. Lessons from border cell migration in the Drosophila ovary: A role for myosin VI in dissemination of human ovarian cancer. Proc Natl Acad Sci USA. 2004;101:8144–8149. doi: 10.1073/pnas.0400400101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McKay JA, Murray LJ, Curran S, Ross VG, Clark C, Murray GI, Cassidy J, McLeod HL. Evaluation of the epidermal growth factor receptor (EGFR) in colorectal tumours and lymph node metastases. Eur J Cancer. 2002;38:2258–2264. doi: 10.1016/s0959-8049(02)00234-4. [DOI] [PubMed] [Google Scholar]
- 46.Ito R, Nakayama H, Yoshida K, Matsumura S, Oda N, Yasui W. Expression of Cbl linking with the epidermal growth factor receptor system is associated with tumor progression and poor prognosis of human gastric carcinoma. Virchows Arch. 2004;444:324–331. doi: 10.1007/s00428-004-0982-8. [DOI] [PubMed] [Google Scholar]
- 47.Deng Z, Ge D, Zhang D, Tan Y, Bai C, Xu Y. The expression of erbB/HER family in lung cancer. Zhonghua JieHe He HuXi ZaZhi. 2002;25:207–209. [PubMed] [Google Scholar]
- 48.Kopp R, Rothbauer E, Mueller E, Schildberg FW, Jauch KW, Pfeiffer A. Reduced survival of rectal cancer patients with increased tumor epidermal growth factor receptor levels. Dis Colon Rectum. 2003;46:1391–1399. doi: 10.1007/s10350-004-6756-1. [DOI] [PubMed] [Google Scholar]
- 49.Niu Y, Fu X, Lv A, Fan Y, Wang Y. Potential markers predicting distant metastasis in axillary node-negative breast carcinoma. Int J Cancer. 2002;98:754–760. doi: 10.1002/ijc.10136. [DOI] [PubMed] [Google Scholar]
- 50.Chung BI, Malkowicz SB, Nguyen TB, Libertino JA, McGarvey TW. Expression of the proto-oncogene Axl in renal cell carcinoma. DNA Cell Biol. 2003;22:533–540. doi: 10.1089/10445490360708946. [DOI] [PubMed] [Google Scholar]
- 51.Sun WS, Fujimoto J, Tamaya T. Coexpression of growth arrest-specific gene 6 and receptor tyrosine kinases Axl and Sky in human uterine endometrial cancers. Ann Oncol. 2003;14:898–906. doi: 10.1093/annonc/mdg257. [DOI] [PubMed] [Google Scholar]
- 52.Ito M, Nakashima M, Nakayama T, Ohtsuru A, Nagayama Y, Takamura N, Demedchik EP, Sekine I, Yamashita S. Expression of receptor-type tyrosine kinase, Axl, and its ligand, Gas6, in pediatric thyroid carcinomas around chernobyl. Thyroid. 2002;12:971–975. doi: 10.1089/105072502320908303. [DOI] [PubMed] [Google Scholar]
- 53.Berclaz G, Altermatt HJ, Rohrbach V, Kieffer I, Dreher E, Andres AC. Estrogen dependent expression of the receptor tyrosine kinase axl in normal and malignant human breast. Ann Oncol. 2001;12:819–824. doi: 10.1023/a:1011126330233. [DOI] [PubMed] [Google Scholar]
- 54.Craven RJ, Xu LH, Weiner TM, Fridell YW, Dent GA, Srivastava S, Varnum B, Liu ET, Cance WG. Receptor tyrosine kinases expressed in metastatic colon cancer. Int J Cancer. 1995;60:791–797. doi: 10.1002/ijc.2910600611. [DOI] [PubMed] [Google Scholar]
- 55.Tsujimoto H, Nishizuka S, Redpath JL, Stanbridge EJ. Differential gene expression in tumorigenic and nontumorigenic HeLa x normal human fibroblast hybrid cells. Mol Carcinog. 1999;26:298–304. doi: 10.1002/(sici)1098-2744(199912)26:4<298::aid-mc8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 56.Xia L, Robinson D, Ma AH, Chen HC, Wu F, Qiu Y, Kung HJ. Identification of human male germ cell-associated kinase, a kinase transcriptionally activated by androgen in prostate cancer cells. J Biol Chem. 2002;277:35422–35433. doi: 10.1074/jbc.M203940200. [DOI] [PubMed] [Google Scholar]
- 57.Kirschmann DA, Seftor EA, Fong SF, Nieva DR, Sullivan CM, Edwards EM, Sommer P, Csiszar K, Hendrix MJ. A molecular role for lysyl oxidase in breast cancer invasion. Cancer Res. 2002;62:4478–4483. [PubMed] [Google Scholar]
- 58.Friess H, Kleeff J, Korc M, Büchler MW. Molecular aspects of pancreatic cancer and future perspectives. Dig Surg. 1999;16:281–290. doi: 10.1159/000018737. [DOI] [PubMed] [Google Scholar]
- 59.Panico L, D'Antonio A, Salvatore G, Mezza E, Tortora G, De Laurentiis M, De Placido S, Giordano T, Merino M, Salomon DS, et al. Differential immunohistochemical detection of transforming growth factor alpha, amphiregulin and CRIPTO in human normal and malignant breast tissues. Int J Cancer. 1996;65:51–56. doi: 10.1002/(SICI)1097-0215(19960103)65:1<51::AID-IJC9>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 60.Kopp R, Rothbauer E, Mueller E, Schildberg FW, Jauch KW, Pfeiffer A. Reduced survival of rectal cancer patients with increased tumor epidermal growth factor receptor levels. Dis Colon Rectum. 2003;46:1391–1399. doi: 10.1007/s10350-004-6756-1. [DOI] [PubMed] [Google Scholar]
- 61.Kondapaka SB, Fridman R, Reddy KB. Epidermal growth factor and amphiregulin up-regulate matrix metalloproteinase-9 (MMP-9) in human breast cancer cells. Int J Cancer. 1997;70:722–726. doi: 10.1002/(sici)1097-0215(19970317)70:6<722::aid-ijc15>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 62.Liu Z, Klominek J. Chemotaxis and chemokinesis of malignant mesothelioma cells to multiple growth factors. Anticancer Res. 2004;24:1625–1630. [PubMed] [Google Scholar]
- 63.Yang G, Truong LD, Timme TL, Ren C, Wheeler TM, Park SH, Nasu Y, Bangma CH, Kattan MW, Scardino PT, et al. Elevated expression of caveolin is associated with prostate and breast cancer. Clin Cancer Res. 1998;4:1873–1880. [PubMed] [Google Scholar]
- 64.Li L, Yang G, Ebara S, Satoh T, Nasu Y, Timme TL, Ren C, Wang J, Tahir SA, Thompson TC. Caveolin-1 mediates testosterone-stimulated survival/clonal growth and promotes metastatic activities in prostate cancer cells. Cancer Res. 2001;61:4386–4392. [PubMed] [Google Scholar]
- 65.Horiguchi A, Asano T, Asakuma J, Asano T, Sumitomo M, Hayakawa M. Impact of caveolin-1 expression on clinicopathological parameters in renal cell carcinoma. J Urol. 2004;172:718–722. doi: 10.1097/01.ju.0000130943.23317.08. [DOI] [PubMed] [Google Scholar]
- 66.Kato K, Hida Y, Miyamoto M, Hashida H, Shinohara T, Itoh T, Okushiba S, Kondo S, Katoh H. Overexpression of caveolin-1 in esophageal squamous cell carcinoma correlates with lymph node metastasis and pathologic stage. Cancer. 2002;94:929–933. [PubMed] [Google Scholar]
- 67.Ho CC, Huang PH, Huang HY, Chen YH, Yang PC, Hsu SM. Up-regulated caveolin-1 accentuates the metastasis capability of lung adenocarcinoma by inducing filopodia formation. Am J Pathol. 2002;161:1647–1656. doi: 10.1016/S0002-9440(10)64442-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lin SY, Yeh KT, Chen WT, Chen HC, Chen ST, Chang JG. Promoter CpG methylation of caveolin-1 in sporadic colorectal cancer. Anticancer Res. 2004;24:1645–1650. [PubMed] [Google Scholar]
- 69.Joo HJ, Oh DK, Kim YS, Lee KB, Kim SJ. Increased expression of caveolin-1 and microvessel density correlates with metastasis and poor prognosis in clear cell renal cell carcinoma. BJU Int. 2004;93:291–296. doi: 10.1111/j.1464-410x.2004.04604.x. [DOI] [PubMed] [Google Scholar]


