Abstract
AIM: To determine common NOD2/CARD15 mutations and TLR4 D299G polymorphism in Hungarian patients with CD.
METHODS: A total of 527 unrelated patients with CD (male/female: 265/262, age: 37.1 (SD 7.6) years) and 200 healthy subjects were included. DNA was screened for possible NOD2/CARD15 mutations by denaturing high-performance liquid chromatography (confirmed by direct sequencing). TLR4 D299G was tested by PCR-RFLP.
RESULTS: NOD2/CARD15 mutations were found in 185 patients (35.1%) and in 33 controls (16.5%, P<0.0001). SNP8/R702W (10.8% vs 6%, P = 0.02), SNP13/3020insC (19.4% vs 5%, P<0.0001) and exon4 R703C (2.1% vs 0%, P = 0.02) mutations were more frequent in CD, while the frequency of SNP12/G908R was not increased. The frequency of TLR4 D299G was not different (CD: 9.9% vs controls: 12.0%). Variant NOD2/CARD15 allele was associated with an increased risk for CD (ORhet = 1.71, 95%CI = 1.12-2.6, P = 0.0001, ORtwo-risk alleles = 25.2, 95%CI = 4.37-∞, P<0.0001), early disease onset (carrier: 26.4 years vs non-carrier: 29.8 years, P = 0.0006), ileal disease (81.9% vs 69.5%, OR = 1.99, 95%CI = 1.29-3.08, P = 0.02, presence of NOD2/CARD15 and TLR4: 86.7% vs 64.8%), stricturing behavior (OR = 1.69, 95%CI = 1.13-2.55, P = 0.026) and increased need for resection (OR=1.71, 95%CI: 1.13-2.62, P = 0.01), but not with duration, extra-intestinal manifestations, familial disease or smoking. TLR4 exhibited a modifier effect: age of onset in wt/TLR4 D299G carriers: 27.4 years vs NOD2mut/TLR D299G: 23 years (P = 0.06), in NOD2mut/wt: 26.7 years.
CONCLUSION: These results confirm that variant NOD2/CARD15 (R702W, R703C and 3020insC) alleles are associated with earlier disease onset, ileal disease, stricturing disease behavior in Hungarian CD patients. In contrast, although the frequency of TLR4 D299G polymorphism was not different from controls, NOD2/TLR4 mutation carriers tended to present at earlier age.
Keywords: Crohn’s disease, NOD2, CARD15, TLR4, Extraintestinal manifestation, Phenotype
INTRODUCTION
Inflammatory bowel disease (IBD) is a multifactorial polygenic disease with probable genetic heterogeneity. In addition to genetic predisposition, various environmental and host factors (e.g., genetic, epithelial, immune and non-immune factors) play a major role in the pathogenesis of IBD. Crohn’s disease (CD) is a chronic inflammatory disorder of the gastrointestinal tract. Extensive heterogeneity is observed in terms of disease presentation, behavior, and response to treatment[1,2]. Attempts have been made to define clinical subgroups on the basis of age at onset, disease location, extent (diffuse or localized) and behavior (primary inflammatory, fistulating, or fibrostenotic).
CD has a strong genetic component, with a lifetime risk of 10-20% to develop IBD in the presence of an affected first-degree relative[1]. The concordance rate of affected siblings for age at onset, disease site, behavior and presence of extra-intestinal manifestation is as high as 80%. Since the first report of Hugot et al[3] in 1996, seven IBD loci have been identified on chromosomes 16q12 (IBD1), 12q13 (IBD2), 6p13 (IBD3), 14q11 (IBD4), 5q31-33 (IBD5), 19p13 (IBD6) and 1p (IBD7)[4-6]. These seven loci are convincingly replicated. Some genetic markers increase the risk of ulcerative colitis or CD while others are associated with a particular phenotypic expression like disease location and/or behavior. The NOD2/CARD15 gene is located in the IBD1 region. NOD2/CARD15 is a cytoplasmatic protein expressed in peripheral blood monocytes, Paneth cells and intestinal epithelial cells and is related structurally to the well-described R proteins in plants, which mediate host resistance to microbial pathogens[7] and induce the NF-κB pathway[8]. Variant alleles result in reduced NF-κB activity[9]. Variant NOD2/CARD15 alleles are also associated with reduced α-defensin release from Paneth cells in response to bacteria[10]. Of particular importance is the C-terminus leucine-rich repeat domain, reportedly the major structural motif that functions as a pattern-recognition receptor for broad types of microbial components, such as bacterial lipopolysaccharides (LPS) and peptidoglycan (including MDP)[11].
Two single nucleotide polymorphisms of NOD2/CARD15 (SNP8: Arg702Trp and SNP12: Gly908Arg) and a frame shift mutation (SNP13: Leu1007insC) have been shown by three independent groups to be associated with susceptibility to CD[12-14]. The presence of one variant allele increases the risk for developing CD 1.5-4.3-fold, and the presence of two copies up to 20-40-fold[13-15]. It has also been suggested that the presence of variant alleles is associated with ileal disease and fibrostenosing or fistulizing behavior in some[15,16], but not in all the studies[17,18].
However, there are significant geographical differences in the frequency of these alleles. They are not found in Japan and China[19,20] and are less frequent in Finland[21] than in Western Europe. There are only limited data in patients from Central-Eastern European countries like Hungary. The incidence of CD in Hungary has been steadily elevat in the last decades (from 0.41 in 1977-1981 to 4.68 in 1997-2001), now reaching that of Western European countries.
Toll-like receptors (TLRs) expressed in myeloid cells play a major role both in detecting microbes and in initiating innate immune responses. In contrast, little is known concerning the expression, distribution and function of TLRs in epithelial cells per se. Toll-like receptor 4 (TLR4) is also expressed in the Golgi apparatus of intestinal epithelial cells. Thus, LPS recognition in intestinal epithelial cells may occur in the Golgi apparatus and require LPS internalization[22]. Recently it has been suggested that the interaction of LPS with TLR4/MD2 contributes to the perpetuation of the inflammatory epithelial cell injury via TNFα-induced alterations of enterocyte turnover in an autoparacrine/paracrine manner[23]. TLRs may also influence the nature of the immune response, in particular by skewing T cells toward a Th1 or Th2 profile. Myeloid cells are exquisitely sensitive to TLR ligands and produce significant IL-12p40 and appear to play key roles in the initiation and possibly the Th1/Th2 skewing of inflammatory responses. In this model the inflammation would normally be controlled by myeloid or lymphocyte-derived IL-10 acting through Stat3 in myeloid cells to block further production of IL-12/IL-23 and skewing to Th1 response[24].
TLR4 is upregulated in the intestinal epithelial cells in patients with CD. In contrast, the expressions of TLR2 and TLR5 are unchanged, while TLR3 is down-regulated[25]. The D299G (Asp299Gly) polymorphism of TLR4 gene is associated with LPS hyporesponsiveness[26] and recently an association between TLR4 mutation and CD was reported in one study[27], but not in another[28].
In view of the limited data on the prevalence of NOD2/CARD15 mutations in Eastern European countries, our aim was to investigate the presence of the common three and other exon4 variants of NOD2/CARD15 as well as the presence of functional D299G polymorphism of the TLR4 gene in three large cohorts of Hungarian patients with CD. We also aimed to investigate the possible association between genotype and clinical characteristics of the disease.
MATERIALS AND METHODS
Patients
A total of 527 unrelated Hungarian patients with CD [male/female: 265/262, age: 37.1 (SD 7.6) years] were investigated. The patients were recruited from three Hungarian IBD centers (Szeged [n = 167], Budapest [n = 185], Veszprem [n = 175]). CD patients, with a follow-up time of at least one year were included. The diagnosis was based on the Lennard-Jones criteria[29]. The clinical characteristics of the patients are summarized in Table 1. The disease phenotype (age at onset, duration, location and behavior) was determined according to the Vienna classification[30]. Perianal involvement, presence of extraintestinal manifestations (EIM; arthritis: peripheral and axial; ocular manifestations: conjunctivitis, uveitis, iridocyclitis; skin lesions: erythema nodosum, pyoderma gangrenosum; hepatic manifestations: primary sclerosing cholangitis [PSC]), frequency of flare-ups (frequent flare-up: >1/year), therapeutic effectiveness (e.g., steroid and/or immunosuppressive resistance), need for surgery (resections). Presence of familial IBD and smoking habits were investigated by filling in a questionnaire.
Table 1.
Clinical characteristics of the different cohorts of Crohn’s disease (CD) patients.
| Budapest (n = 185) | Veszprem (n = 175) | Szeged (n = 167) | |
| Male/Female | 98/87 | 88/87 | 79/88 |
| Age (yr) | 35.6±11.4 | 37.8±13.3 | 37.1±12.7 |
| Age at presentation (yr) | 27.2±10.3 | 30.2±12.4 | 28.9±10.9 |
| Duration (yr) | 8.9±6.6 | 7.7±6.8 | 8.0±7.3 |
| Familial IBD, n (%) | 63 (11.9) | 38 (11.1) | 25 (13.5) |
| Location (n) L1 | 43 | 54 | 39 |
| L2 | 37 | 47 | 52 |
| L3 | 103 | 74 | 74 |
| L4 | 2 | 0 | 2 |
| Behavior (n) B1 | 88 | 65 | 62 |
| B2 | 40 | 39 | 49 |
| B3 | 56 | 71 | 56 |
| Perianal disease, n (%) | 41 (22.1) | 49 (28.0) | 50 (29.9) |
| Frequent relapse, n (%) | 59 (31.9) | 72 (41.1) | 64 (38.6) |
| Extraintestinal manifestations, n (%) | 67 (36.2) | 61 (34.8) | 47 (28.2) |
| Operation, n (%) | 77 (41.6) | 76 (43.4) | 67 (40.1) |
| Smoking habits (n) No | 115 | 96 | 98 |
| Yes | 55 | 61 | 55 |
| Previous | 15 | 20 | 14 |
The control group for mutation analysis consisted of 200 age- and gender-matched healthy subjects [male/female: 102/98, age: 38.05 (SD 10.7) years]. The study was approved by the Semmelweis University Regional and Institutional Committee of Science and Research Ethics (81/2003). Each patient was informed of the nature of the study and signed the informed consent form.
Detection of NOD2/CARD15 SNP8, 12, 13 and exon4 mutations
Genomic DNA was isolated from whole blood according to the QIAamp DNA blood mini kit (QIAGEN GmbH, Germany). Each exon was amplified by PCR using previously published primer sequences[17]. The initial denaturation step (at 94 °C for 7 min) was to activate AmpliTaq Gold (Applied Biosystems, Foster City, CA, USA), followed by 33 cycles (at 94 °C for 20 s, at 61 °C for 30 s, at 72 °C for 25 s) with a final extension step at 72 °C for 7 min. Then denaturing high-performance liquid chromatography (dHPLC, wave DNA fragment analysis system, Transgenomic Limited, UK) were performed to analyze the exons. PCR products were denatured as a last step at 94 °C for 5 min to induce heteroduplex formation during the following 30 min of slowly cooling down to room temperature. Five microliters of these PCR products were then automatically loaded onto the DNASep cartridge (Transgenomic Limited, UK) in the wave system. The specific acetonitrile gradient to elute each exon was established by using the WaveMaker 3.4.4 software. The particular run temperature for the detection of each SNP was determined using positive controls, which were kindly provided by Dirk Seegert from Kiel, Germany.
Finally, when a sequence variation was observed in the dHPLC profile, the relevant PCR product was sequenced on both strands to confirm the alteration. Sequencing reactions were performed with the ABI BigDye terminator cycle sequencing kit v1.1 (Applied Biosystems) and samples were sequenced on an ABI Prism 310 genetic analyzer (Applied Biosystems).
Detection of TLR4 D299G polymorphism
The TLR4 D299G polymorphism was detected by PCR-RFLP (PTC-200 thermocycler, MJ Research Inc., MA, USA) using previously published primers and conditions[31]. For the overnight digestion of the amplified DNA, NcoI enzyme (New England Biolabs, London, UK) was used and the fragments were separated and visualized by gel electrophoresis (3% NuSieve® GTG agarose gel BMA, Rockland, ME, USA).
Statistical analysis
Variables were tested for normality by Shapiro Wilk’s W test. t-test with separate variance estimates, χ2-test and χ2-test with Yates correction were used to test differences between patients with CD and controls, and also within subgroups of CD patients. Odds ratios (OR) and logistic regression were calculated to compare genetic and clinical data. P<0.05 was considered statistically significant. For the statistical analysis, Statistica 6.1 (Statsoft Inc., OK, USA) was used.
RESULTS
NOD2/CARD15 mutations were more frequently found in CD patients (185/527; 35.1%) than those in controls (16.5%, P<0.0001, Table 2, 3). Heterozygous (ORhet = 1.71; 95%CI = 1.12-2.6, P = 0.0001), homozygous (ORhom = 14.43; 95%CI = 2.47-∞, P = 0.0003) or compound heterozygous (ORcompound = 12.92; 95%CI = 2.2-∞, P = 0.0006) carriage of a variant allele was associated with increased risk for CD. The OR for carrying two variant alleles was 25.2 (95%CI: 4.35-∞, P<0.0001). SNP8 (11.6% vs controls: 6%) and SNP13 (19.4% vs controls: 5%, P<0.0001) mutations were more frequent in CD (Table 4), while the frequency of SNP12 variant allele was not different, but consistent in different cohorts (Table 5). The carriage of SNP8, SNP13 (ORSNP8 allele = 2.41; 95%CI = 1.30-4.44, ORSNP13 allele = 4.78; 95%CI = 2.50-9.11) and a further exon4 variant allele (R703CCD: 2.1% vs controls: 0%, OR = 6.89; 95%CI = 1.18-∞, P = 0.02) were identified as risk factors for CD (Tables 4 and 6).
Table 2.
NOD2/CARD15 genotype in patients with Crohn’s disease (CD) and controls, n (%).
| A |
NOD2 genotype |
||||
| Non-carrier | All carrier | Heterozygous | Homozygous | Compound heterozygous | |
| Controls (n = 200) | 167 (83.5) | 33 (16.5) | 33 (16.5) | 0 | 0 |
| CD (n = 527) | 342 (64.9) | 185 (35.1) | 133 (25.2)1 | 30 (5.7)2 | 26 (4.9)3 |
P<0.0001 between CD patients and controls,
ORhet = 1.71 (1.12–2.60),
ORhom = 14.43 (2.47–∞),
ORcompound = 12.92 (2.2–∞).
Table 3.
TLR4 D299G genotype in patients with Crohn’s disease (CD) and controls, n (%).
| B |
TLR4 D299G |
||||
| Non-carrier | All carrier | Heterozygous | Homozygous | ||
| Controls (n = 200) | 176 (88.0) | 24 (12.0) | 23(11.5) | 1 (0.5) | |
| CD (n = 527) | 475 (90.1) | 52 (9.9) | 50 (9.5) | 2(0.4) | |
Table 4.
NOD2/CARD15 SNP8, 12 and 13 in patients with Crohn’s disease (CD) and controls.
|
R702W (SNP8)1 |
G908R(SNP12) |
3020insC (SNP13)1 |
||||
| CD n (%) | Controls n (%) | CD n (%) | Controls n (%) | CD n (%) | Controls n (%) | |
| Wild type | 466 (88.4) | 188 (94.0) | 494 (96.7) | 193 (96.5) | 425 (80.6) | 190 (95.0) |
| All carriers | 61 (11.6) | 12 (6.0) | 33 (6.3) | 7 (3.5) | 102 (19.4) | 10 (5.0) |
| Heterozygous | 45 (8.5) | 12 (6.0) | 33 (6.3) | 7 (3.5) | 89 (16.9) | 10 (5.0) |
| Homozygous | 16 (3.1) | 0 | 0 | 0 | 13 (2.5) | 0 |
P = 0.02 and P<0.0001 between patients and controls for genotype frequency by χ2-test, ORSNP8 allele = 2.41 (1.30–4.44), ORSNP13 allele = 4.78 (2.50–9.11).
Table 5.
NOD2/CARD15 and TLR4 D299G mutations in different cohorts of CD patients, n (%).
Table 6.
Further exon4 mutations in patients with Crohn’s disease (CD) and controls.
| CD (n = 527) | Controls (n = 200) | |
| R703C1 | 11 (1 homozygous) | 0 |
| R713C | 1 | 0 |
| A755V | 2 | 1 |
| E778K | 0 | 1 |
| R791Q | 5 | 1 |
| V793M | 2 | 1 |
P = 0.02 between patients and controls for allele frequency, ORR703C = 6.89 (1.18–∞).
More homozygous (60%) or compound heterozygous (69.2%) patients tended to be females compared to heterozygous (46.6%) patients and non-carriers (49.1%). The use of immunosuppressive drugs (P = 0.04) and the need for surgery (resection, P = 0.006) were more frequent in carriers of the mutation (Table 7). The percentage of patients with resection was even higher in compound heterozygous patients (65.4%, 17/26, P = 0.006 compared to non-carriers by Fischer exact test). The presence of variant NOD2/CARD15 allele affected disease phenotype and was associated with earlier disease onset (26.4 vs 29.8 years, P = 0.0006), the site of involvement (ileal involvement: 81.6% vs non-carriers: 69.0%, OR = 1.99, 95%CI: 1.29-3.08, P = 0.02) and with stricturing behavior (OR = 1.69, 95%CI: 1.13-2.55, P = 0.02, Tables 7, 8). The presence of NOD2/CARD15 variant alleles was not associated with the presence of perianal manifestation associated disease duration, more frequent relapses, familial disease and presence of EIMs or smoking habits. EIMs were tendentiously even less frequent in patients carrying two mutant alleles.
Table 7.
Clinical characteristics of CD patients, with respect to the presence or absence of NOD2/CARD15 mutations.
| Total (n = 527) | Non carrier (n = 342) | Carrier (n = 185) | 1 allele (n = 133) | 2 alleles (n = 52) | ||
| Male/Female | 265/262 | 174/168 | 91/94 | 71/62 | 20/32 | |
| Age (yr) | 36.9±9.1 | 37.9±13.0 | 34.9±11.61 | 35.2±11.7 | 34.3±11.4 | |
| Age at presentation (yr) | 37.1±7.6 | 29.8±12.1 | 26.4±9.71 | 26.4±9.6 | 26.5±10.2 | |
| Duration (yr) | 8.2±5.0 | 8.1±7.0 | 8.5±6.7 | 8.8±7.0 | 7.9±5.8 | |
| Familiar IBD n (%) | 63 (11.9) | 38 (11.1) | 25 (13.5) | 17 (12.8) | 8 (15.4) | |
| Location (n) | L1 | 136 | 84 | 521 | 362 | 162 |
| L2 | 136 | 103 | 33 | 26 | 7 | |
| L3 | 251 | 152 | 99 | 71 | 28 | |
| L4 | 4 | 3 | 1 | 0 | 1 | |
| Behavior (n) | B1 | 216 | 151 | 651 | 483 | 17 |
| B2 | 128 | 71 | 57 | 42 | 15 | |
| B3 | 183 | 120 | 63 | 43 | 20 | |
| Perianal disease n (%) | 140 (26.6) | 89 (26.0) | 51 (27.6) | 36 (27.1) | 15 (28.9) | |
| Frequent relapse n (%) | 195 (37.1) | 126 (36.9) | 69 (37.3) | 47 (35.3) | 22 (42.3) | |
| Extraintestinal manifestations n (%) | 175 (33.2) | 117 (34.2) | 58 (31.3) | 45 (33.8) | 13 (25) | |
| Arthritis n (%) | 147 (27.9) | 98 (28.7) | 49 (26.5) | 36 (27.1) | 13 (25) | |
| Occular n (%) | 27 (5.1) | 18 (5.2) | 9 (4.9) | 9 (6.8) | 0 | |
| Erythema nodosum/Pyoderma n (%) | 48 (9.1) | 30 (8.8) | 18 (9.7) | 15 (11.3) | 3 (5.8) | |
| PSCa | 18 (3.4) | 15 (4.4) | 3 (1.6) | 3 (2.3) | 0 | |
| Steroid use/ | 440 (83.5)/ | 282 (82.4)/ | 158 (85.4)/ | 114 (85.7)/ | 44 (84.6)/ | |
| refractory n (%) | 44 (10) | 28 (9.3) | 16 (10.1) | 10 (8.8) | 6 (13.6) | |
| Azathioprine use/ | 337 (64.1)/ | 208 (60.8)/ | 129 (69.7)1/ | 89 (66.9)/ | 40 (76.9)4/ | |
| refractory n (%) | 19 (5.6) | 10 (4.8) | 9 (7.0) | 7 (7.8) | 2 (5) | |
| Operation n (%) | 220 (41.8) | 128 (37.4) | 92 (49.7)1 | 66 (49.6)2 | 26 (50.0)2 | |
| Smoking (n) | Never | 308 | 191 | 117 | 80 | 37 |
| Active | 170 | 115 | 55 | 42 | 13 | |
| Previous | 49 | 36 | 13 | 11 | 2 |
P<0.03 between carriers and non-carriers,
P<0.03 between patients carrying one or two mutant allele and non-carriers,
P = 0.043 between patients carrying one mutant allele and non-carriers,
P = 0.025 between patients carrying two mutant allele and non-carriers.
Table 8.
Genotype–phenotype associations with particular NOD2/CARD15 alleles in CD patients.
| None (n = 342) | SNP8 (n = 61) | SNP12 (n = 33) | SNP13 (n = 102) | ||
| Male/Female | 174/168 | 28/33 | 14/19 | 51/51 | |
| Age (yr) | 37.9±13.0 | 35.9±13.0 | 37.1±11.4 | 33.7±10.41 | |
| Age at presentation (yr) | 29.8±12.1 | 26.6±10.9 | 28.8±10.0 | 26.0±8.41 | |
| Duration (yr) | 8.1±7.0 | 9.3±7.6 | 11.4±6.42 | 7.7±6.1 | |
| Familiar IBD n (%) | 38 (11.1) | 9 (14.8) | 7 (21.1) | 11 (10.8) | |
| Location | L1 | 84 | 16 | 7 | 322 |
| L2 | 103 | 12 | 5 | 16 | |
| L3 | 152 | 33 | 20 | 53 | |
| L4 | 3 | 0 | 1 | 1 | |
| Behavior | B1 | 151 | 22 | 8 | 34 |
| B2 | 71 | 15 | 13 | 31 | |
| B3 | 120 | 14 | 12 | 37 | |
| Perianal disease n (%) | 89 (26.0) | 18 (29.5) | 7 (21.1) | 32 (31.4) | |
| Frequent relapse n (%) | 126 (36.9) | 24 (39.3) | 13 (39.4) | 38 (37.3) | |
| Extraintestinal manifestations n (%) | 117 (34.2) | 17 (27.8) | 14 (42.4) | 31 (30.4) | |
| Arthritis n (%) | 98 (28.7) | 16 (26.2) | 14 (42.2) | 24 (23.5) | |
| Occular n (%) | 18 (5.2) | 1 (1.6) | 2 (6.1) | 4 (3.9) | |
| Erythema nodosum/ | |||||
| Pyoderma n (%) | 30 (8.8) | 5 (8.2) | 4 (12.1) | 7 (6.9) | |
| PSC n (%) | 15 (4.4) | 1 (1.6) | 0 | 2 (1.9) | |
| Steroid use/ | 282 (82.4)/ | 51 (83.6)/ | 31 (93.9)/ | 88 (86.3)/ | |
| refractory n (%) | 28 (9.3) | 7 (13.7) | 2 (16.1) | 6 (6.8) | |
| Azathioprine use/ refractory n (%) | 208 (60.8)/ | 38 (62.3)/ | 32 (97)1/ | 69 (67.6)/ | |
| 10 (4.8) | 4 (10.5) | 2 (11.1) | 3 (4.3) | ||
| Operationn (%) | 128 (37.4) | 27 (44.3) | 23 (69.7)1 | 53 (52.0)2 | |
| Smoking habits | Never | 191 | 44 | 21 | 65 |
| Active | 115 | 12 | 9 | 33 | |
| Previous | 36 | 5 | 3 | 4 |
P<0.001 between carriers and non-carriers;
P<0.03 between carriers and non-carriers.
The TLR4 D299G mutation was not different between patients and controls (9.9% vs 12.0%, P = NS). The frequency of familial IBD tended to be lower in patients with TLR4 mutation (5.7% vs without 12.6%, P = NS). However, the presence of variant TLR4 allele strengthened genotype-phenotype associations (Figure 1; for age of onset: non-carriers [n = 305]: 30.2 years, only TLR4 carriers [n = 37]: 27.4 years, only NOD2/CARD15 carriers [n = 170]: 26.7 years, both NOD2 and TLR4 carriers [n = 15]: 23 years, P = 0.03 for NOD2/CARD15 variant allele, and P = 0.06 for TLR4 variant allele by multiple regression and for ileal involvement; in patients with TLR4 and NOD2/CARD15 mutations: 86.7% vs non-carriers: 64.8%).
Figure 1.
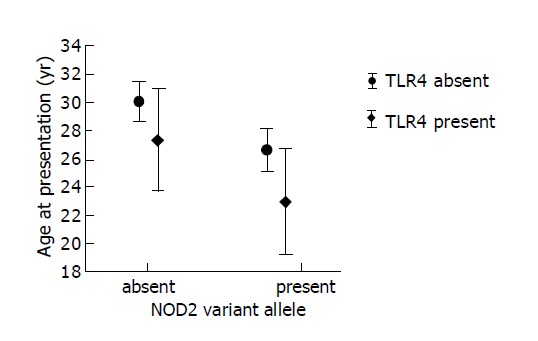
Association between genetics and age at presentation in patients with CD.
In a logistic regression model, exploring the effect of NOD2, TLR4 carriage, age at presentation, location, behavior and smoking, presence of NOD2 mutation (coefficient = 0.54, OR = 1.71, 95%CI: 1.13-2.62, P = 0.01) and non-inflammatory behavior (coefficient = 1.26, OR = 3.53, 95%CI: 2.76-4.51, P = 0.001) but not location, smoking or carriage of TLR4 variant allele were independently associated with the need for surgery. However, the percentage of multiple resections was not different between carriers and non-carriers (13.0% vs 11.1%, P = NS).
DISCUSSION
This is the first report on the prevalence of NOD2/CARD15 mutations and TLR4 D299G polymorphism in patients with CD from a Central Eastern European country. The reported rates of 35.1% of patients carrying NOD2/CARD15 mutations in CD and 16.5% in controls are in concordance with previously reported rates of 30-50% in CD and 7-20% in controls from other European regions[12,15-17,32-35]. Only in Finland (which by language is related to Hungary), the rate of NOD2 mutations was considerably lower (8.7% vs 3.5% in controls)[21]. Similar low frequencies were found in other Northern European countries (8% in Denmark, and 8.9% in patients from Norway)[28]. The prevalence of SNP8, 12 and 13 was 3.3, 0.6 and 4.8% in the Finish study (in controls it was 1.8%, 0 and 1.7%) with only the SNP13 being more common in CD compared to controls. In our study, the rates were 11.6, 6.3 and 19.4%, which are in concordance with other studies from Europe (6.7-12.5%, 3.3-6.1% and 6.6-16% in CD and 3.5-6.9%, 0.6-3.0% and 1.0-4.4% in controls)[17,33].
The phenotype-genotype correlations in our cohort were also similar to those reported in various European countries[6,17,36]. Ileal involvement in Hungarian patients was more frequent in NOD2 mutation carriers (81.6%), while disease confined to the colon alone was less frequent (17.8%), especially in patients with two alleles, in the presence of SNP13 or TLR4 variant allele. Like in other countries, in our study, carriage of variant NOD2/CARD15 allele was associated with stricturing disease (30.8% vs 20.8%), while variant alleles were less frequent in patients with inflammatory disease. More patients with stricturing disease carried a mutant NOD2/CARD15 allele (44.5%) than patients without strictures (32.1%, P<0.01). Steroid use and efficacy were similar in mutation carriers and non-carriers, but a higher percentage of patients carrying NOD2/CARD15 variant allele needed azathioprine during the course of the disease, especially in the presence of two risk alleles. There are conflicting data on the association of NOD2/CARD15 mutations and need for surgery in CD patients: association[37] and also lack of association[16,17] have been reported.
In a French follow-up study[18], ileal location was associated with early development of stricturing disease while a high number of flares was associated with a penetrating pattern, but this was not affected by the presence of variant NOD2/CARD15 allele. Active smoking was also associated with early development of penetrating disease. In our study there was no difference in the proportion of smokers between carriers and non-carriers of NOD2/CARD15 variant allele.
The importance of TLR4 D299G polymorphism in CD is less clear. In contrast to Franchimont et al[27] who reported a two-fold elevation in allele frequency of TLR4 D299G (11% vs 5%, OR = 2.31), we found no difference in the prevalence of TLR4 D299G polymorphism in CD patients and controls, suggesting that this polymorphism is not essential in the development of the disease. There is also no difference in TLR4 allele frequency between IBD patients and controls in concordance with the preliminary results of the EC-IBD study group[28]. However, the rate of variant allele is higher in the Hungarian controls compared to the study of Franchimont et al[27]. We also found a tendency of decreased frequency of the TLR4 D299G variant allele in patients with familial disease (6% vs sporadic 13%, P = NS).
In our study, no clear-cut phenotype-genotype associations were observed in TLR4 D299G carriers. The presence of variant TLR4 allele tendencially associated with early disease onset (P = 0.06), along with a gene-dosage effect. The earliest onset (23 years) was observed in carriers of both variant NOD2/CARD15 and TLR4 alleles (vs non-carriers 30.2 years, P = 0.01). The presence of TLR4 variant allele did not affect disease behavior (in patients with variant TLR4 allele, stricturing disease was present in 33.3% of NOD2 carriers vs 17.1% of NOD2/CARD15 non-carriers).
In summary, this is the first report on the prevalence of NOD2/CARD15 mutations and TLR4 D299G polymorphism in patients with CD from a Central Eastern European country. It confirms that the risk for CD is increased in carriers of R702W, R703C and 3020insC mutations, while the presence of G908R or TLR4 D299G polymorphism is not different from the controls. The presence of variant NOD2/CARD15 alleles is associated with early disease onset, ileal disease and stricturing disease behavior and increases need for surgery, while the presence of TLR4 D299G variant allele exhibits a disease modifier effect.
ACKNOWLEDGEMENTS
The authors thank Dr. Peter Vargha for performing the statistical analysis.
Footnotes
Edited by Wang XL and Guo SY Language Editor Elsevier HK
References
- 1.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 2.Lakatos L, Mester G, Erdelyi Z, Balogh M, Szipocs I, Kamaras G, Lakatos PL. Striking elevation in incidence and prevalence of inflammatory bowel disease in a province of western Hungary between 1977-2001. World J Gastroenterol. 2004;10:404–409. doi: 10.3748/wjg.v10.i3.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hugot JP, Laurent-Puig P, Gower-Rousseau C, Olson JM, Lee JC, Beaugerie L, Naom I, Dupas JL, Van Gossum A, Orholm M, et al. Mapping of a susceptibility locus for Crohn's disease on chromosome 16. Nature. 1996;379:821–823. doi: 10.1038/379821a0. [DOI] [PubMed] [Google Scholar]
- 4.Colombel JF. The CARD15 (also known as NOD2) gene in Crohn's disease: are there implications for current clinical practice? Clin Gastroenterol Hepatol. 2003;1:5–9. doi: 10.1053/jcgh.2003.50002. [DOI] [PubMed] [Google Scholar]
- 5.Bonen DK, Cho JH. The genetics of inflammatory bowel disease. Gastroenterology. 2003;124:521–536. doi: 10.1053/gast.2003.50045. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad T, Tamboli CP, Jewell D, Colombel JF. Clinical relevance of advances in genetics and pharmacogenetics of IBD. Gastroenterology. 2004;126:1533–1549. doi: 10.1053/j.gastro.2004.01.061. [DOI] [PubMed] [Google Scholar]
- 7.Berrebi D, Maudinas R, Hugot JP, Chamaillard M, Chareyre F, De Lagausie P, Yang C, Desreumaux P, Giovannini M, Cézard JP, et al. Card15 gene overexpression in mononuclear and epithelial cells of the inflamed Crohn's disease colon. Gut. 2003;52:840–846. doi: 10.1136/gut.52.6.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Girardin SE, Hugot JP, Sansonetti PJ. Lessons from Nod2 studies: towards a link between Crohn's disease and bacterial sensing. Trends Immunol. 2003;24:652–658. doi: 10.1016/j.it.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Bonen DK, Ogura Y, Nicolae DL, Inohara N, Saab L, Tanabe T, Chen FF, Foster SJ, Duerr RH, Brant SR, et al. Crohn's disease-associated NOD2 variants share a signaling defect in response to lipopolysaccharide and peptidoglycan. Gastroenterology. 2003;124:140–146. doi: 10.1053/gast.2003.50019. [DOI] [PubMed] [Google Scholar]
- 10.Aldhous MC, Nimmo ER, Satsangi J. NOD2/CARD15 and the Paneth cell: another piece in the genetic jigsaw of inflammatory bowel disease. Gut. 2003;52:1533–1535. doi: 10.1136/gut.52.11.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Philpott DJ, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278:8869–8872. doi: 10.1074/jbc.C200651200. [DOI] [PubMed] [Google Scholar]
- 12.Hugot JP, Chamaillard M, Zouali H, Lesage S, Cézard JP, Belaiche J, Almer S, Tysk C, O'Morain CA, Gassull M, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 13.Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Britton H, Moran T, Karaliuskas R, Duerr RH, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 14.Hampe J, Cuthbert A, Croucher PJ, Mirza MM, Mascheretti S, Fisher S, Frenzel H, King K, Hasselmeyer A, MacPherson AJ, et al. Association between insertion mutation in NOD2 gene and Crohn's disease in German and British populations. Lancet. 2001;357:1925–1928. doi: 10.1016/S0140-6736(00)05063-7. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad T, Armuzzi A, Bunce M, Mulcahy-Hawes K, Marshall SE, Orchard TR, Crawshaw J, Large O, de Silva A, Cook JT, et al. The molecular classification of the clinical manifestations of Crohn's disease. Gastroenterology. 2002;122:854–866. doi: 10.1053/gast.2002.32413. [DOI] [PubMed] [Google Scholar]
- 16.Brant SR, Picco MF, Achkar JP, Bayless TM, Kane SV, Brzezinski A, Nouvet FJ, Bonen D, Karban A, Dassopoulos T, et al. Defining complex contributions of NOD2/CARD15 gene mutations, age at onset, and tobacco use on Crohn's disease phenotypes. Inflamm Bowel Dis. 2003;9:281–289. doi: 10.1097/00054725-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Lesage S, Zouali H, Cézard JP, Colombel JF, Belaiche J, Almer S, Tysk C, O'Morain C, Gassull M, Binder V, et al. CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002;70:845–857. doi: 10.1086/339432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Louis E, Michel V, Hugot JP, Reenaers C, Fontaine F, Delforge M, El Yafi F, Colombel JF, Belaiche J. Early development of stricturing or penetrating pattern in Crohn's disease is influenced by disease location, number of flares, and smoking but not by NOD2/CARD15 genotype. Gut. 2003;52:552–557. doi: 10.1136/gut.52.4.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inoue N, Tamura K, Kinouchi Y, Fukuda Y, Takahashi S, Ogura Y, Inohara N, Núñez G, Kishi Y, Koike Y, et al. Lack of common NOD2 variants in Japanese patients with Crohn's disease. Gastroenterology. 2002;123:86–91. doi: 10.1053/gast.2002.34155. [DOI] [PubMed] [Google Scholar]
- 20.Leong RW, Armuzzi A, Ahmad T, Wong ML, Tse P, Jewell DP, Sung JJ. NOD2/CARD15 gene polymorphisms and Crohn's disease in the Chinese population. Aliment Pharmacol Ther. 2003;17:1465–1470. doi: 10.1046/j.1365-2036.2003.01607.x. [DOI] [PubMed] [Google Scholar]
- 21.Heliö T, Halme L, Lappalainen M, Fodstad H, Paavola-Sakki P, Turunen U, Färkkilä M, Krusius T, Kontula K. CARD15/NOD2 gene variants are associated with familially occurring and complicated forms of Crohn's disease. Gut. 2003;52:558–562. doi: 10.1136/gut.52.4.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hornef MW, Normark BH, Vandewalle A, Normark S. Intracellular recognition of lipopolysaccharide by toll-like receptor 4 in intestinal epithelial cells. J Exp Med. 2003;198:1225–1235. doi: 10.1084/jem.20022194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruemmele FM, Beaulieu JF, Dionne S, Levy E, Seidman EG, Cerf-Bensussan N, Lentze MJ. Lipopolysaccharide modulation of normal enterocyte turnover by toll-like receptors is mediated by endogenously produced tumour necrosis factor alpha. Gut. 2002;51:842–848. doi: 10.1136/gut.51.6.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boone DL, Ma A. Connecting the dots from Toll-like receptors to innate immune cells and inflammatory bowel disease. J Clin Invest. 2003;111:1284–1286. doi: 10.1172/JCI18545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cario E, Podolsky DK. Differential alteration in intestinal epithelial cell expression of toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect Immun. 2000;68:7010–7017. doi: 10.1128/iai.68.12.7010-7017.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okayama N, Fujimura K, Suehiro Y, Hamanaka Y, Fujiwara M, Matsubara T, Maekawa T, Hazama S, Oka M, Nohara H, et al. Simple genotype analysis of the Asp299Gly polymorphism of the Toll-like receptor-4 gene that is associated with lipopolysaccharide hyporesponsiveness. J Clin Lab Anal. 2002;16:56–58. doi: 10.1002/jcla.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franchimont D, Vermeire S, El Housni H, Pierik M, Van Steen K, Gustot T, Quertinmont E, Abramowicz M, Van Gossum A, Devière J, et al. Deficient host-bacteria interactions in inflammatory bowel disease? The toll-like receptor (TLR)-4 Asp299gly polymorphism is associated with Crohn's disease and ulcerative colitis. Gut. 2004;53:987–992. doi: 10.1136/gut.2003.030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riis LB, Wolters F, Solberg C. Regional differences in the prevalence of single nucleotide polymorphisms in CARD15/NOD2 but not in toll-like receptor 4 (TLR4) Asp299Gly polymorphism in patients with inflammatory bowel disease (IBD) across Europe: Results from the EC-IBD study group. Gastroenterology. 2004;126(Suppl S):M1539. [Google Scholar]
- 29.Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6; discussion 16-9. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- 30.Gasche C, Scholmerich J, Brynskov J, D'Haens G, Hanauer SB, Irvine EJ, Jewell DP, Rachmilewitz D, Sachar DB, Sandborn WJ, et al. A simple classification of Crohn's disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998. Inflamm Bowel Dis. 2000;6:8–15. doi: 10.1097/00054725-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Lorenz E, Frees KL, Schwartz DA. Determination of the TLR4 genotype using allele-specific PCR. Biotechniques. 2001;31:22–24. doi: 10.2144/01311bm01. [DOI] [PubMed] [Google Scholar]
- 32.Annese V, Palmieri O, Latiano A, Ardizzone S, Castiglione F, Cottone M, D'Incà R, Gionchetti P, Papi C, Riegler G, et al. Frequency of NOD2/CARD15 variants in both sporadic and familial cases of Crohn's disease across Italy. An Italian Group for Inflammatory Bowel Disease Study. Dig Liver Dis. 2004;36:121–124. doi: 10.1016/j.dld.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 33.Cuthbert AP, Fisher SA, Mirza MM, King K, Hampe J, Croucher PJ, Mascheretti S, Sanderson J, Forbes A, Mansfield J, et al. The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. Gastroenterology. 2002;122:867–874. doi: 10.1053/gast.2002.32415. [DOI] [PubMed] [Google Scholar]
- 34.Abreu MT, Taylor KD, Lin YC, Hang T, Gaiennie J, Landers CJ, Vasiliauskas EA, Kam LY, Rojany M, Papadakis KA, et al. Mutations in NOD2 are associated with fibrostenosing disease in patients with Crohn's disease. Gastroenterology. 2002;123:679–688. doi: 10.1053/gast.2002.35393. [DOI] [PubMed] [Google Scholar]
- 35.Heresbach D, Gicquel-Douabin V, Birebent B, D'halluin PN, Heresbach-Le Berre N, Dreano S, Siproudhis L, Dabadie A, Gosselin M, Mosser J, et al. NOD2/CARD15 gene polymorphisms in Crohn's disease: a genotype- phenotype analysis. Eur J Gastroenterol Hepatol. 2004;16:55–62. doi: 10.1097/00042737-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Török HP, Glas J, Lohse P, Folwaczny C. Alterations of the CARD15/NOD2 gene and the impact on management and treatment of Crohn's disease patients. Dig Dis. 2003;21:339–345. doi: 10.1159/000075357. [DOI] [PubMed] [Google Scholar]
- 37.Büning C, Genschel J, Bühner S, Krüger S, Kling K, Dignass A, Baier P, Bochow B, Ockenga J, Schmidt HH, et al. Mutations in the NOD2/CARD15 gene in Crohn's disease are associated with ileocecal resection and are a risk factor for reoperation. Aliment Pharmacol Ther. 2004;19:1073–1078. doi: 10.1111/j.1365-2036.2004.01967.x. [DOI] [PubMed] [Google Scholar]


