Abstract
AIM: To present a case of acute mesenteric and portal vein thrombosis treated with thrombolytic therapy in a patient with ulcerative colitis in acute phase and to review the literature on thrombolytic therapy of mesenteric-portal system. Treatment of acute portal vein thrombosis has ranged from conservative treatment with thrombolysis and anticoagulation therapy to surgical treatment with thrombectomy and/or intestinal resection.
METHODS: We treated our patient with intraportal infusion of plasminogen activator and then heparin through a percutaneous transhepatic catheter.
RESULTS: Thrombus resolved despite premature interruption of the thrombolytic treatment for neurological complications, which subsequently resolved.
CONCLUSION: Conservative management with plasminogen activator, could be considered as a good treatment for patients with acute porto-mesenteric thrombosis.
Keywords: Acute mesenteric, Portal vein thrombosis
INTRODUCTION
Acute portal vein thrombosis in non-cirrhotic patients is a rare event (3-10% of all of portal hypertension)[1,2] and there are only a few cases described in the literature.
The etiology is multifactorial, and includes local, systemic and iatrogenic causes.
Acute systemic inflammatory diseases is one of the systemic causes of acute portal vein thrombosis.
In patients with chronic inflammatory bowel diseases the incidence of thrombo-embolic complications ranges from 1.3 to 39% and in the majority of cases the initial event is deep venous thrombosis of the lower extremities, pulmonary embolism and retinal artery thrombosis[3]. Thrombosis of the splenic-mesenteric-portal system is a rare event. In a study from the Mayo Clinic[3], the incidence of thrombo-embolic complications among 7199 patients with inflammatory bowel disease was 1.3%. Only eight cases of mesenteric thrombosis were found, and only three of those patients had ulcerative colitis. In this group of patients the mortality rate was 50%.
Recently local thrombolytic treatment of a few cases of acute portal vein thrombosis in the porto-mesenteric system has been described[4-9].
In this article we reported a case of mesenteric and portal vein thrombosis associated with ulcerative colitis, who was treated with local fibrinolytic recombinant tissue plasminogen activator (rt-PA) via transhepatic route. We also reviewed the literature on thrombolytic therapy of the mesenteric-portal system in non- cirrhotic patients.
CASE REPORT
A 40-year old female without any significant past medical history was admitted for severe vomiting and diarrhea associated with bloody stools and fever. On physical examination she was found to have signs of ascites, hepato-splenomegaly and abdominal distension without peritoneal signs.
She was hemodynamically stable. Her laboratory results revealed: mild anemia (Hgl: 9.6 g/dL), low platelet count (50000/mL), abnormalities in her liver test (AST: 135 U/L, ALT: 191 U/L) and coagulopathy: INR: 2.19, factor VII: 46% (nl: 70-130%), factor XI: 32% (nl: 50-150%), von Willebrand factor>120 IU/dL (nl: 60-150 IU/dL), and factor VIII:192% (nl: 50-150%), and a significant decrease in AT III: 54% (nl: 70-120%) and fibrinogen: 1.06 g/L (nl: 1.5-4.5 g/L), as well as elevated D-dimers: 2.71 mg/L (nl: <0.25 mg/L). Antiphospholipid antibodies were negative. These results suggested the presence of disseminated intravascular coagulation (DIC).
A colonoscopy was performed which showed evidence of active ulcerative colitis with erosions, ulcers and pseudopolyps. Colonic biopsies confirmed the endoscopic findings of inflammatory bowel disease. An abdominal CT-angiogram demonstrated complete occlusion of the right branch and partial occlusion of the main portal vein, while the left branch was patent. The proximal portion of the superior mesenteric vein was completely occluded while the splenic vein was patent. There was partial flow in the portal and mesenteric veins (Figure 1). A Doppler US of the abdominal vessels showed hyperechogenic thrombi indicating a recent event. Since the thrombosis appeared to be the result of an acute event, and occurred in a hemodynamically stable patient without any sign of intestinal infarction, a decision was made to use local thrombolytic therapy. The portal branch of the fourth segment was cannulated via an anterior, transhepatic route using a 5 F catheter. Angiography confirmed the CT scan and ultrasonographic findings (Figure 2).
Figure 1.
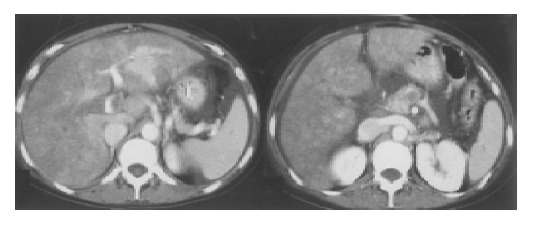
Partial occlusion of the main portal vein (left) and complete occlusion of prossimal superior mesenteric vein (right) shown on abdominal CT-angiogram.
Figure 2.
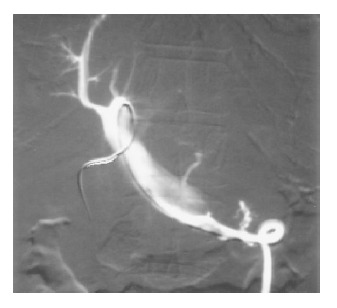
Complete occlusion of the right branch and partial occlusion of the main portal vein and proximal portion of superior mesenteric vein shown by angiography via transhepatic cathether.
Alteplase- (rt-PA) was administered at the following doses: an initial 10 mg bolus in ten minutes was followed by 40 mg in 100 mL of saline solution at 1.5 mL/min in the first hour and 50 mg in 100 mL of saline solution at 0.8 mL/min in the successive 2 h. Two hours following the administration of the initial dose (at a cumulative dose of 75 mg) the patient developed tonic-clonic seizure and rectal bleeding. Cerebral hemorrhage was suspected and therefore the thrombolytic therapy was halted. Head CT showed a small ischemic lesion with an area of hemorrhage in the white matter in the centre of the left semi-ovale. On electroencephalography diffuse cerebral irritability was noted. The symptoms completely resolved in 24 h after conservative management, without any residual signs. A 48 h follow up angiography showed complete resolution of the superior mesenteric and main portal vein thrombosis, and partial resolution of the thrombi in the right portal branch (Figure 3).
Figure 3.
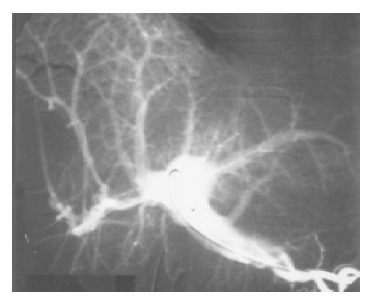
Complete resolution of superior mesenteric and main portal vein thrombosis and partial resolution of thrombi in right portal branch shown by angiography via transhepatic cathether (48 h follow up).
As the patient became stable, the neurologic signs resolved and the coagulation profile normalized, anticoagulation was started using a transhepatic approach with continuous heparin infusion at a low dose of 15000 IU/ d for 9 d. At the completion of the transhepatic heparin treatment, the portography showed resolution of the residual thrombi and patency of the mesenteric-portal-splenic system, including the right portal branch. The transhepatic catheter was removed 11 d after insertion using haemostatic material without any hemorrhagic complications. Low molecular weight heparin anti Xa nadroparin 0.4 mL (3800 IU) was continued for six months. The patient was discharged 20 d following admission without any residual neurologic sign, and in good overall clinical condition. A 6-mo follow-up CT scan demonstrated complete resolution of the thrombi in the portal, superior mesenteric and splenic veins. At the 5-year follow up visit the patient was asymptomatic, and a follow-up abdominal Doppler US showed patent portal, mesenteric and splenic veins. Her ulcerative colitis was in clinical remission while the patient was on maintenance treatment with sulfasalazinea. Repeated colonoscopy and biopsies were negative for active acute or chronic inflammatory bowel disease.
DISCUSSION
Thrombosis of the portal system is a rare event in non-cirrhotic patients. As it frequently presents with nonspecific symptoms, it remains a diagnostic challenge for the clinicians. There is no specific standard treatment for such cases.
Thromboembolic events are a well-known complication in patients with inflammatory bowel disease with incidence of 1.3-39%[3]. Thrombosis of the portal-mesenteric system is a rare event with a high mortality rate (50%) in patients with ulcerative colitis. In the majority, thrombosis is associated with a hypercoagulable state associated with increased levels of thromboplastin, fibrinogen, factor VIII and elevated platelet count. Accelerated spontaneous platelet aggregation and possibly protein S and C deficiencies caused by vitamin K malabsorption are also common findings[10]. Acute thrombosis can result in intestinal ischemia and venous infarction. The treatment of choice is surgical resection of the affected bowel. When thrombosis is not complicated with infarction, and the patient is hemodynamically stable, the use of systemic or local thrombolysis has been a well-described therapeutic option[11,12].
Surgical intervention is associated with a high mortality rate (up to 59%)[13] with a high number of reinterventions and postoperative complications, such as short bowel syndrome, pulmonary embolism, sepsis and wound infections. When surgical intervention is combined with systemic anticoagulation, the mortality rate appears lower (22-39%), while the use of systemic anticoagulation alone decreases the mortality only to 44%. This latter approach is also associated with a higher recurrence rate (71%) when compared with the combined approach (32%)[14].
Local thrombolysis has been proposed as a therapeutic modality to lower the mortality and morbidity rate in these patients. We are not aware of any fatality following local thrombolytic therapy, although this therapeutic option has been used in highly selected and less complicated cases. The route of administration of local fibrinolysis could be arterial or venous. The arterial approach allows thrombolysis either in intramural venous branches or in marginal veins of the intestine, and is best suited for the collateral veins[15]. The venous one has a more intense and direct thrombolytic effect. The venous use of the rt-PA reduces the risk of hemorrhage, due to the fast hepatic metabolism of the drug and consequently less systemic effects. Direct portal administration of the drug has been described by various percutaneous techniques[11]. The thrombolytic agents utilized are urokinase and rt-PA. The latter has the advantage of a high selectivity for fibrin, and a more efficacious dissolution rate of the thrombi[16,17].
A review of the literature revealed only three cases of porto-mesenteric thrombosis in patients with ulcerative colitis[7,18,19]. Two of them were treated with either surgical intervention (colectomy) and the thrombi were resolved 3 mo after the intervention[18] or systemic anticoagulation which resulted in portal cavernoma[19]. The only case treated with local thrombolysis was a patient with ulcerative colitis and portal thrombosis (main trunk and intrahepatic branches). The therapeutic regimen was systemic thrombolysis with urokinase for 7 d followed by local thrombolysis. This approach was applied due to hemorrhagic complications of systemic anticoagulation and treatment failure (no resolution of the thrombi). Rt-PA 3000 UI (5 mg) was administered over 30 min, followed again by urokinase for 6 d using the transhepatic approach to resolve the thrombi[7].
The use of rt-PA as a thrombolytic agent in porto-mesenteric thrombosis was described in two other cases associated with other underlying etiologies[20-22]. In the case reported by Tsujikawa et al[20], the thrombolytic agent was urokinase given via a catheter positioned in the superior mesenteric artery. The dose of urokinase was 1600000 IU bolus in the first hour (2 mg) followed by a continuous urokinase infusion (120000 UI/d for 14 d) for 14 d. In the other case described by Demertzis et al[6], the portal and mesenteric thrombosis was treated with 50 mg rt-PA administered through the portal vein during surgical intervention followed by 200 mg rt-PA in 48 h through a catheter positioned in the superior mesenteric artery. No hemorrhagic complications were reported.
We used thrombolytic therapy with the same protocol used for the treatment of myocardial infarction, and it was stopped because of the hemorrhagic event. As the hemorrhagic complication resolved, we used continuous low dose local heparin treatment for 9 d, and then low molecular weight heparin for 6 mo. Despite the fact that the thrombolytic treatment was prematurely terminated, thrombosis resolved and did not recur during a long term follow-up. Based on our experience and review of the literature (Table 1), we believe that local thrombolytic therapy given through the portal vein using the percutaneous approach should be considered as a feasible, efficacious and safe treatment of choice for patients with acute porto-mesenteric thrombosis without intestinal ischemia. This treatment modality has a low complication rate, and a low mortality. Further studies are needed to determine the exact dose and administration modalities of rt-PA in order to minimize its side effects, while maintaining its efficacy.
Table 1.
Acute mesenterico-portal thrombosis treated with local thrombolytic therapy.
| Author | Year | Etiology | Thrombus site | Access | Treatment | Complications | Outcome |
| Yankes JR | 1988 | Pancreatic cancer | Superior mesenteric vein (SMV) | Transhepatic | Urokinase for 4 h then angioplastic dilatation and systemic heparin | Laparotomy with ileal resection 2 wk after treatment | Thrombus resolution |
| Bilbao JI | 1989 | Splenectomy | Portal vein (PV) and SMV | Tranhepatic | Urokinase for 12 h then systemic heparin | None | Thrombus resolution |
| Demertzis S | 1994 | Non noted | PV and SMV | Mesenteric | Surgical thrombectomy, reintervention, local rTPA for 48 h then local heparin for 4 d | None | Thrombus resolution |
| Miyazaki Y | 1995 | Ulcerative colitis | PV and PV branches | Transhepatic | Systemic urokinase and local rTPA for 30’ then urokinase for 6 d | None | Thrombus resolution |
| Poplausky MR | 1996 | Gastric cancer | Portal and superior mesenteric vein | Arterial | Urokinase for 48 h with systemic heparin | None | Partial thrombus |
| Tsuijikawa T | 1996 | Crohn’s disease | PV, SMV and splenic vein (SV) | Arterial | rTPA 1 h and urokinase for 14 d and systemic heparin and serin-protease inhibitors | None | Thrombus resolution resolution |
| Ludwig DJ | 1999 | Protein S deficiency | PV, SMV, and SV | Arterial | Urokinase for 4 d and systemic heparin | None | Thrombus resolution |
| Sze DY | 2000 | Protein S deficiency | PV, right PV branch, SMV and SV | Arterial | Urokinasefor 16 h and sistemic heparin | GI bleeding, exploratory laparotomy and jejunum resection | Thrombus resolution after transjugular mechanical thrombolysis |
| Antoch G1 | 2001 | Protein C deficiency (n = 1) | PV and SMV | Arterial | Urokinase for 8 d then systemic heparin | Bleeding at the catheter site after 5 d of therapy in one case | Thrombus resolution (?) |
| Tateishi A | 2001 | Down syndrome and protein S deficiency | Pv, SMV and SV | Arterial | Systemic thrombolysis, with heparin sc, than local urokinase for 11 d | Evolution to portal cavernoma | Reduction of the thrombus |
| Aytekin C | 2001 | Chronic Pancreatitis | Partial PV | Transhepatic | 4 cycles of systemic thrombolysis, then local thrombolysis with urokinase | None | Thrombus resolution |
| Kercher KW | 2002 | Splenectomy | PV, PV branches, SMV and SV | Transjugular | Local thrombolysis: mechanical attempt followed by urokinase for 45 h, then systemic heparin | Epistaxis and hematuria | Persistent thrombus in the right PV branch and PV partial occlusion |
(13 cases).
Footnotes
Science Editor Wang XL Language Editor Elsevier HK
References
- 1.Boughton BJ. Hepatic and portal vein-thrombosis. BMJ. 1991;302:192–193. doi: 10.1136/bmj.302.6770.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belli L, Romani F, Riolo F, Rondinara G, Aseni P, Di Stefano M, Contorni L, Bini M. Thrombosis of portal vein in absence of hepatic disease. Surg Gynecol Obstet. 1989;169:46–49. [PubMed] [Google Scholar]
- 3.Talbot RW, Heppell J, Dozois RR, Beart RW. Vascular complications of inflammatory bowel disease. Mayo Clin Proc. 1986;61:140–145. doi: 10.1016/s0025-6196(12)65200-8. [DOI] [PubMed] [Google Scholar]
- 4.Yankes JR, Uglietta JP, Grant J, Braun SD. Percutaneous transhepatic recanalization and thrombolysis of the superior mesenteric vein. AJR Am J Roentgenol. 1988;151:289–290. doi: 10.2214/ajr.151.2.289. [DOI] [PubMed] [Google Scholar]
- 5.Bilbao JI, Rodriguez-Cabello J, Longo J, Zornoza G, Páramo J, Lecumberri FJ. Portal thrombosis: percutaneous transhepatic treatment with urokinase--a case report. Gastrointest Radiol. 1989;14:326–328. doi: 10.1007/BF01889228. [DOI] [PubMed] [Google Scholar]
- 6.Demertzis S, Ringe B, Gulba D, Rosenthal H, Pichlmayr R. Treatment of portal vein thrombosis by thrombectomy and regional thrombolysis. Surgery. 1994;115:389–393. [PubMed] [Google Scholar]
- 7.Miyazaki Y, Shinomura Y, Kitamura S, Hiraoka S, Tomoda K, Nezu R, Kamiike W, Nakamura H, Matsuzawa Y. Portal vein thrombosis associated with active ulcerative colitis: percutaneous transhepatic recanalization. Am J Gastroenterol. 1995;90:1533–1534. [PubMed] [Google Scholar]
- 8.Aytekin C, Boyvat F, Kurt A, Yologlu Z, Coskun M. Catheter-directed thrombolysis with transjugular access in portal vein thrombosis secondary to pancreatitis. Eur J Radiol. 2001;39:80–82. doi: 10.1016/s0720-048x(01)00289-3. [DOI] [PubMed] [Google Scholar]
- 9.Kercher KW, Sing RF, Watson KW, Matthews BD, LeQuire MH, Heniford BT. Transhepatic thrombolysis in acute portal vein thrombosis after laparoscopic splenectomy. Surg Laparosc Endosc Percutan Tech. 2002;12:131–136. doi: 10.1097/00129689-200204000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Lichtenstein DR, Park PD, Lichtenstein GR. Extraintestinal manifestations of inflammatory biwel disease. Vol. 2. In: Problems in General Surgery. Lippincott Williams & Wilkin, Inc., Philadelphia; 1999. pp. 23–39. [Google Scholar]
- 11.Sze DY, O'Sullivan GJ, Johnson DL, Dake MD. Mesenteric and portal venous thrombosis treated by transjugular mechanical thrombolysis. AJR Am J Roentgenol. 2000;175:732–734. doi: 10.2214/ajr.175.3.1750732. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig DJ, Hauptmann E, Rosoff L, Neuzil D. Mesenteric and portal vein thrombosis in a young patient with protein S deficiency treated with urokinase via the superior mesenteric artery. J Vasc Surg. 1999;30:551–554. doi: 10.1016/s0741-5214(99)70083-2. [DOI] [PubMed] [Google Scholar]
- 13.Abdu RA, Zakhour BJ, Dallis DJ. Mesenteric venous thrombosis--1911 to 1984. Surgery. 1987;101:383–388. [PubMed] [Google Scholar]
- 14.Rhee RY, Gloviczki P, Mendonca CT, Petterson TM, Serry RD, Sarr MG, Johnson CM, Bower TC, Hallett JW, Cherry KJ. Mesenteric venous thrombosis: still a lethal disease in the 1990s. J Vasc Surg. 1994;20:688–697. doi: 10.1016/s0741-5214(94)70155-5. [DOI] [PubMed] [Google Scholar]
- 15.Antoch G, Taleb N, Hansen O, Stock W. Transarterial thrombolysis of portal and mesenteric vein thrombosis: a promising alternative to common therapy. Eur J Vasc Endovasc Surg. 2001;21:471–472. doi: 10.1053/ejvs.2001.1355. [DOI] [PubMed] [Google Scholar]
- 16.Derad I, Stierle U, Giannitsis E, Potratz J, Born J, Djonlagic H, Fehm HL. Accelerated ST-segment reduction after thrombolytic therapy with recombinant tissue plasminogen activator (rtPA) compared to urokinase. Jpn Heart J. 1996;37:33–41. doi: 10.1536/ihj.37.33. [DOI] [PubMed] [Google Scholar]
- 17.Mahler F, Schneider E, Hess H. Recombinant tissue plasminogen activator versus urokinase for local thrombolysis of femoropopliteal occlusions: a prospective, randomized multicenter trial. J Endovasc Ther. 2001;8:638–647. doi: 10.1177/152660280100800618. [DOI] [PubMed] [Google Scholar]
- 18.Hagimoto T, Seo M, Okada M, Shirotani T, Tanaka K, Tomita A, Oda T, Iida T. Portal vein thrombosis successfully treated with a colectomy in active ulcerative colitis: report of a case. Dis Colon Rectum. 2001;44:587–590. doi: 10.1007/BF02234334. [DOI] [PubMed] [Google Scholar]
- 19.Farkas LM, Nelson RL, Abcarian H. A case of portal venous system thrombosis in ulcerative colitis. J Am Coll Surg. 2000;190:94. doi: 10.1016/s1072-7515(99)00236-7. [DOI] [PubMed] [Google Scholar]
- 20.Tsujikawa T, Ihara T, Sasaki M, Inoue H, Fujiyama Y, Bamba T. Effectiveness of combined anticoagulant therapy for extending portal vein thrombosis in Crohn's disease. Report of a case. Dis Colon Rectum. 1996;39:823–825. doi: 10.1007/BF02054451. [DOI] [PubMed] [Google Scholar]
- 21.Poplausky MR, Kaufman JA, Geller SC, Waltman AC. Mesenteric venous thrombosis treated with urokinase via the superior mesenteric artery. Gastroenterology. 1996;110:1633–1635. doi: 10.1053/gast.1996.v110.pm8613072. [DOI] [PubMed] [Google Scholar]
- 22.Tateishi A, Mitsui H, Oki T, Morishita J, Maekawa H, Yahagi N, Maruyama T, Ichinose M, Ohnishi S, Shiratori Y, et al. Extensive mesenteric vein and portal vein thrombosis successfully treated by thrombolysis and anticoagulation. J Gastroenterol Hepatol. 2001;16:1429–1433. doi: 10.1046/j.1440-1746.2001.02557.x. [DOI] [PubMed] [Google Scholar]


