Abstract
AIM: Obesity and insulin resistance (IR) are closely related to hepatic steatosis (HS), and adiponectin is a hepatic insulin sensitizer that has important effects in liver function. This study aims at investigating the relationship between serum adiponectin concentration and the presence of HS.
METHODS: We carried out a cross-sectional study in a check-up unit of a University Hospital in Mexico City. We enrolled 196 subjects, comprising 98 subjects with HS (27 women, 71 men) and 98 controls (37 women and 61 men). Anthropometric, metabolic and biochemical variables were measured in the two groups. Serum adiponectin and leptin concentrations were determined, their association with grade of HS tested, and concentrations, according to quartiles, compared between cases and controls. χ2 analysis for linear trends was used to test for a dose-response relationship and logistic regression analysis was conducted to test for a protective effect of adiponectin.
RESULTS: The HS subjects were older and more obese than controls, with a central obesity pattern. In the fourth quartile of adiponectin concentrations, HS was less common and severe. In a multivariate model of the fourth quartile of the adiponectin concentrations, we observed a protective effect (OR = 0.17, 95%CI: 0.04-0.67, P = 0.01). In subjects with more severe HS, we observed higher leptin concentrations, and caloric intakes, total fat and iron consumption were higher than in controls.
CONCLUSION: The results of the present study suggest that a high serum concentration of adiponectin is associated with a protective effect against HS.
Keywords: Adiponectin, Hepatic steatosis, Leptin, Diet
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is an increasingly recognized condition that may progress to end-stage liver disease. The pathological picture resembles that of alcohol-induced liver injury, but it occurs in patients who do not abuse alcohol[1]. Various terms have been used to describe this entity, including fatty-liver hepatitis, nonalcoholic Laënnec’s disease, diabetes hepatitis, alcohol-like liver disease, and nonalcoholic steatohepatitis (NASH)[2]. AFLD is becoming the preferred term, and it refers to a wide spectrum of liver damage, ranging from simple steatosis to steatohepatitis, advanced fibrosis, and cirrhosis[3].
The influence of obesity on liver physiology has been demonstrated in several studies and populations, with the analyses showing the effects of weight reduction on biochemical indicators of liver function[4,5]. Obesity, or indirectly, body mass index (BMI), is a major risk factor for development of liver disease, and the prevalence of NAFLD increases 4.6-fold in obese people[3,6]. Other risk factors associated with NAFLD are waist circumference, hyperinsulinemia, hypertriglyceridemia and impaired glucose tolerance or type 2 diabetes[7,8]. The clinical implications of NAFLD are derived mostly from its common occurrence in the general population and its potential to progress to fibrosis, cirrhosis and liver failure.
The molecular basis of the association between insulin resistance (IR) and hepatic steatosis (HS) remains largely unknown. Adipose tissue represents an important and very active endocrine organ that produces a number of hormones such as leptin and adiponectin, termed adipokines that have been related to the regulation of insulin sensitivity and other physiological processes[7]. Leptin plays an important role in the regulation of food intake, body composition, energy expenditure, and body weight[9], and it has been suggested that leptin plays a role in the pathogenesis of nonalcoholic steatohepatitis. On the other hand, adiponectin has now been added to a list of new and very exciting players in the field of obesity-related IR. The aim of this study was to investigate correlations between leptin and adiponectin concentrations and the presence and degree of HS.
MATERIALS AND METHODS
Population and sample
We conducted a cross-sectional study in the check-up unit of the Diagnostic Clinic at the Medica Sur Clinic & Foundation. This hospital provides care for mainly middle- and high-income individuals from Mexico City and surrounding metropolitan areas. The study was approved by the Human Subjects Committee of the Medica Sur Clinic and Foundation, conforming to the ethical guidelines of the 1983 Declaration of Helsinki, and written informed consent was obtained from all participants before entry into the study. Our sample population was formed from a series of consecutive asymptomatic subjects who were referred to the check-up unit by their companies as an annual employment requirement, not for symptomatic disease. The study included 196 subjects who agreed to participate, 98 subjects found to have HS (27 women, 71 men) and 98 controls (37 women and 61 men without HS). HS cases and controls were a series of consecutive asymptomatic subjects from the check-up unit. Real-time ultrasonographic studies were performed while the subjects were fasting. A 3.5-MHz transducer was used to obtain the following images: sagittal view of the right lobe of the liver and right kidney, transverse view of the left lateral segment of the liver and spleen, transverse view of the liver and pancreas, and any focal areas of altered echotexture (Elegra; Siemens Medical Systems, Mountain Grove, CA). The severity of echogenicity was graded as follows: grade 0, normal echogenicity; grade 1, slight, diffuse increase in fine echoes in liver parenchyma with normal visualization of diaphragm and intrahepatic vessel borders; grade 2, moderate, diffuse increase in fine echoes with slightly impaired visualization of intrahepatic vessels and diaphragm; grade 3, marked increase in fine echoes with poor or nonvisualization of the intrahepatic vessel borders, diaphragm, and posterior right lobe of the liver. Sonographic patterns included the following: 0, homogeneous, normal; 1, hyperechoic nodules; 2, multiple, confluent hyperechoic lesions; 3, hypoechoic skip nodules; 4, irregular hyperechoic and hypoechoic areas; 5, diffuse involvement[10]. No discrepancies were found between the results of the first and second evaluations. In the second evaluation, all studies for each subject were viewed side-by-side in a masked fashion.
Diet history questionnaire
Participants completed a food frequency questionnaire with commonly used portion measures specified. The questionnaire included questions on the frequency and brand of multivitamin and individual vitamin supplements. The answers were subsequently electronically scanned and the daily intake of various nutrients was determined using SNUT software a program developed by the Instituto Nacional de Salud Pública, Mexico City[11], and appropriate to the Mexican population in order to estimate dietary energy; protein; carbohydrate; total, saturated, polyunsaturated and monounsaturated fat; vitamin; mineral; and antioxidant intake.
Physical examination
Body weight was measured, in light clothing and without shoes, to the nearest 0.10 kg. Height was measured to the nearest 0.5 cm. BMI was calculated as weight (kg) divided by height squared (m2). Waist circumference to the nearest 0.1 cm was measured at the midpoint between the lower border of the rib cage and the iliac crest, and hip circumference was similarly obtained at the widest point between hip and buttock. Body fat percentage was measured by bioelectrical impedance (Omron body fat analyzer modelHBF-306INT).
Analytical procedures
Insulin levels were measured using an immunoenzymometric assay (MEIA; Abbott Diagnostics), with inter- and intra-assay coefficients of variation less than 3%.
Plasma glucose in the fasting state was measured in duplicate with an automated analyzer. The coefficient of variation for a single determination was 1.5%. Cholesterol, HDL-cholesterol, and triglycerides concentrations were measured by enzymatic colorimetric methods, using CHOL, HDL-C plus (second generation) and TG assays (Roche Diagnostics Co., Indianapolis, IN) respectively. LDL concentrations were calculated using the Friedewald formula[12].
Assessment of IR was made using the Homeostasis Model Assessment (HOMA-IR). Insulin resistance was assessed using the HOMA-IR originally described by Matthews et al[13]. HOMA-IR was calculated using the following formula: HOMA-IR = fasting insulin (μU/mL) × fasting glucose (mmol/L)/22.5: values >2.522 indicate a high index of IR.
Plasma leptin and adiponectin levels were determined by radio immunoassay using RIA kits (Linco Research, St. Charles, MO, USA). The intra- and inter-assay coefficients of variation are both less than 5%.
Statistical analysis
Mean±SD were used to describe the distributions of continuous variables, comparing cases with controls. The nonparametric Mann-Whitney U-test was applied to compare these variables owing to the abnormal distribution of some variables. Adiponectin and leptin distributions, according to quartiles, were compared between cases (by HS grade) and controls. χ2 testing for linear trends was used to test for a dose-response relationship. Logistic regression analysis was conducted to test the adiponectin distribution by quartiles as a protective main effect in the probability of HS, controlling for potential confounders. Odds ratios (OR) were derived for the exponential of the regression coefficient, and 95% CI were calculated. All statistical analyses were carried out with the statistics program, SPSS/PC v12.0 (Chicago, IL).
RESULTS
We studied 98 cases and 98 controls. Men comprised 72.4% of the cases and 62.2% of the controls (P = 0.17). We observed statistically significant differences between the HS cases and controls in the mean values for age, anthropometric variables (waist, hip, BMI, percentage of body fat), IR, liver enzymes (alanine aminotransferase, aspartate aminotransferase and alkaline phosphatase), and serum leptin and adiponectin concentrations (Table 1). In general, the HS subjects were older, with greater weight, BMI, central obesity, IR, and a more atherogenic profile than controls.
Table 1.
Anthropometric, metabolic, and biochemical variables of cases and controls (mean±SD).
| Variable | Cases (n = 98) | Controls (n = 98) | P1 |
| Age (yr) | 48.5 (11.3) | 44.4 (11.9) | 0.012 |
| Weight (kg) | 82.1 (12.5) | 72.0 (17.4) | <0.00012 |
| Height (cm) | 167.8 (8.9) | 168.1 (9.4) | 0.96 |
| Waist (cm) | 98.7 (9.1) | 85.1 (11.1) | <0.00012 |
| Hip (cm) | 107.4 (9.6) | 99.6 (6.4) | <0.00012 |
| Waist to hip ratio | 0.92 (0.07) | 0.85 (0.09) | <0.00012 |
| BMI | 29.2 (3.7) | 24.7 (3.0) | <0.00012 |
| Body fat (%) | 31.2 (6.7) | 26.3 (6.4) | <0.00012 |
| Alcohol (g/d) | 5.5 (10.9) | 4.5 (6.6) | 0.95 |
| Cigarettes (n/d) | 3.6 (8.2) | 3.6 (9.9) | 0.9 |
| Glucose (mmol/L) | 5.86 (2.26) | 4.91 (0.59) | <0.00012 |
| Insulin (pmol/L) | 65.28 (36.8) | 36.11 (22.91) | <0.00012 |
| HOMA index | 2.5 (1.9) | 1.2 (0.9) | <0.00012 |
| Uric acid (mmol/L) | 374.72 (77.32) | 333.08 (83.27) | 0.0032 |
| Total protein (g/L) | 71 (4) | 70 (5) | 0.56 |
| Albumin (g/L) | 41 (3) | 41 (3) | 0.39 |
| Total bilirubin (mmol/L) | 17.1 (9.91) | 15.56 (6.49) | 0.3 |
| Direct bilirubin (mmol/L) | 2.56 (4.27) | 2.39 (1.19) | 0.39 |
| Indirect bilirubin (mmol/L) | 14.19 (6.32) | 12.99 (6.15) | 0.11 |
| ALT (U/L) | 32.0 (17.2) | 24.6 (7.2) | <0.00012 |
| AST (U/L) | 42.8 (29.5) | 26.6 (14.3) | <0.00012 |
| Alkaline phosphatase (U/L) | 69.7 (23.4) | 63.9 (20.4) | 0.042 |
| Total cholesterol (mmol/L) | 5.61 (1.08) | 5.09 (0.84) | <0.00012 |
| LDL-cholesterol (mmol/L) | 3.57 (0.83) | 3.25 (0.74) | 0.0032 |
| HDL-cholesterol (mmol/L) | 0.96 (0.23) | 1.06 (0.26) | 0.0032 |
| Triglycerides (mmol/L) | 2.56 (2.4) | 1.71 (1.31) | <0.00012 |
| Leptin (mg/mL) | 12.5 (8.5) | 9.10 (5.6) | 0.006 |
| Adiponectin (mg/mL) | 15.3 (9.0) | 20.7 (10.8) | <0.00012 |
1Mann–Whitney U test.
Significant differences.
When diet was analyzed, the HS cases reported a pattern with a greater mean caloric intake for all macronutrients (Table 2). Some mean values for vitamin intake were also higher in the HS cases than the controls.
Table 2.
Dietary variables between cases and controls (mean±SD).
| Variable | Cases (n = 98) | Controls (n = 98) | P1 |
| Calories (Kcal/d) | 2329 (1143) | 1891 (718) | 0.0012 |
| Protein (g/d) | 80 (45) | 68 (24) | 0.032 |
| Carbohydrates (g/d) | 290 (139) | 239 (115) | 0.0032 |
| Fructose (g/d) | 36 (26) | 29 (21) | 0.022 |
| Glucose (g/d) | 30 (22) | 23 (17) | 0.022 |
| Total fat (g/d) | 79 (46) | 64 (25) | 0.0052 |
| Saturated fatty acids (g/d) | 27 (18) | 21 (9) | 0.006 |
| Monounsaturated fatty acids (g/d) | 37 (21) | 30 (11) | 0.006 |
| Polyunsaturated fatty acids (g/d) | 15 (8) | 13 (7) | 0.022 |
| Iron (mg/d) | 14 (6) | 12 (5) | 0.032 |
| Zinc (mg/d) | 17 (8) | 16 (7) | 0.24 |
| Copper (mg/d) | 2 (1) | 2 (1) | 0.55 |
| Manganese (mg/d) | 17 (13) | 18 (36) | 0.032 |
| Selenium (mg/d) | 38 (21) | 36 (21) | 0.24 |
| Vitamin C (mg/d) | 233 (227) | 183 (117) | 0.042 |
| Carotene (UI/d) | 6873 (4185) | 5995 (4818) | 0.032 |
| α-Carotene (mg/d) | 415 (347) | 348 (450) | 0.012 |
| β-Carotene (mg/d) | 3140 (2054) | 2708 (2045) | 0.02 |
| Lutein–xanthine (mg/d) | 1608 (1107) | 1624 (1138) | 0.89 |
| Vitamin E (mg/d) | 8 (4) | 8 (4) | 0.48 |
| Total tocopherol (mg/d) | 24 (12) | 20 (10) | 0.02 |
| α-Tocopherol (mg/d) | 10 (5) | 9 (4) | 0.022 |
| β-Tocopherol (mg/d) | 1 (4) | 1 (5) | 0.012 |
| γ-Tocopherol (mg/d) | 13 (8) | 11 (6) | 0.06 |
| δ-Tocopherol (mg/d) | 2 (2) | 2 (1) | 0.07 |
| Cholesterol (mg/d) | 270 (203) | 222 (118) | 0.09 |
| Alcohol (mg/d) | 3 (7) | 3 (5) | 0.6 |
| Caffeine (mg/d) | 166 (206) | 116 (171) | 0.012 |
1Mann–Whitney U test.
Significant differences.
Adiponectin and leptin concentrations were divided according to quartile distribution. Table 3 shows the differences of this distribution for cases divided by HS grade, and controls. The observed gradient dose–response was more significant for adiponectin than for leptin(Table 4).
Table 3.
Quartile (Q) distribution of adiponectin between cases (by HS grade) and controls.
| Adiponectin quartile |
Cases (HS) |
|||||||
|
Controls |
Grade I |
Grade II |
Grade III |
|||||
| n | % | n | % | n | % | n | % | |
| Q1 | 14 | 14.3 | 14 | 29.2 | 21 | 46.7 | 0 | 0 |
| Q2 | 23 | 23.5 | 15 | 31.3 | 9 | 20 | 2 | 40 |
| Q3 | 29 | 29.6 | 10 | 20.8 | 9 | 20 | 1 | 20 |
| Q4 | 32 | 32.7 | 9 | 18.8 | 6 | 13.3 | 2 | 40 |
| Total | 98 | 100 | 48 | 100 | 45 | 100 | 5 | 100 |
χ2 for linear trend = 11.7, P = 0.001.
Table 4.
Quartile (Q) distribution of leptin between cases (by HS grade) and controls.
| Leptin quartile |
Cases (HS) |
|||||||
|
Controls |
Grade I |
Grade II |
Grade III |
|||||
| n | % | n | % | n | % | n | % | |
| Q1 | 30 | 30.6 | 9 | 18.8 | 9 | 20 | 1 | 20 |
| Q2 | 25 | 25.5 | 15 | 31.3 | 8 | 17.8 | 1 | 20 |
| Q3 | 23 | 23.5 | 11 | 22.9 | 15 | 33.3 | 0 | 0 |
| Q4 | 20 | 20.4 | 13 | 27.1 | 13 | 28.9 | 3 | 60 |
| Total | 98 | 100 | 48 | 100 | 45 | 100 | 5 | 100 |
χ2 for linear trend = 4.8, P = 0.03.
When adiponectin was evaluated as the main effect in multivariate logistic regression analysis, a protective effect was observed after controlling for potential confounders (Table 5). This protective effect for the presence of HS was higher as the quartile increased. Thus, when comparing one patient in the highest adiponectin quartile against one in the lower quartile (reference category), there was a 5.9-fold (inverse of the OR of 0.17) lower probability of the presence of HS. Conversely, high plasma leptin levels appear to increase the probability of the presence of HS.
Table 5.
Multivariate model1 obtained by logistic regression analysis testing adiponectin concentration (by quartile) as a protective main effect.
1Model controlled for: gender (female vs male), age (≥45 vs <45 yr), leptin (quartiles), BMI (<25, 25–29.9, ≥30), caloric intake (kcal/d), total-cholesterol (≥240 vs <240 mg/dL), HDL-cholesterol (<40 vs ≥40 mg/dL), waist (>102 cm in male, >88 cm in female), and HOMA index (≥2.5 vs <2.5).
Significant differences.
DISCUSSION
In this study, we explored the role of serum adiponectin and leptin concentrations in subjects with and without HS. We observed great differences in BMI and abdominal obesity (waist to hip ratio 0.92 vs 0.85). Similar data were observed with insulin sensitivity (HOMA-IR 2.5 vs 1.2), a common characteristic of subjects with NAFLD[14]. In addition, we found that high plasma leptin levels are associated with HS.
However, the major finding in this study was that high levels of adiponectin are associated with a protective effect against HS. How can we explain these results? First, it has been suggested that adiponectin concentrations are regulated mainly by body composition, and the plasma concentrations of this adipokine are negatively correlated with percentage of body fat and body fat mass[15]. Decreased adiponectin concentration, hypoadiponectinemia, has been implicated in the development of IR[16], hyperlipidemia[17] and various diseases associated with increased IR. As the development of IR and hyperlipidemia causes the accumulation of fat in the liver[14,18], hypoadiponectinemia was expected to be related to the development of fatty liver.
Second, adiponectin is reported to suppress fatty acid influx into the liver[19], enhance hepatic insulin actions[20], stimulate peroxisome proliferator-activated receptor α[21], and increase fatty acid oxidation[22]. By these mechanisms, hypoadiponectinemia might increase fatty acid influx into the liver, and reduce its metabolism, resulting in the progression of fatty liver. Furthermore, adiponectin has been demonstrated to prevent the progression of fatty liver in animal models[23].
Third, a recent study showed that hypoadiponectinemia and activation of the tumor necrosis facter-α system occurs in subjects with NASH, when compared to controls matched for age, BMI, and sex. Furthermore, adiponectin levels were lower for individuals with NASH. In addition, Hui et al[24], found that lower adiponectin concentration was also associated with higher grades of HS. In the present study, we found similar results; that is, lower concentrations of adiponectin were seen in subjects with grades 2 and 3 of HS (Figure 1).
Figure 1.
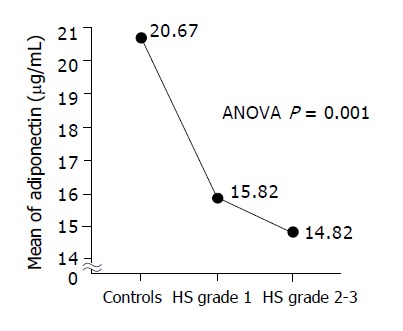
Serum adiponectin concentrations according to HS severity.
Another interesting finding seen in this study is the relationship between serum aminotransferase activities and grades of HS when compared to subjects without HS. Although serum aminotransferase activities have been proposed as markers for liver disease, they have not been universally accepted. Interestingly, Ruhl and Everhart[25] attempted to expand our understanding of liver disease in the US population by presenting an analysis of data from the Third National Health and Nutrition Examination Survey (NHANES III). Using these data, they examine the prevalence of an abnormal alanine aminotransferase (ALT), defined as ALT >43 U/L for men or women. By eliminating individuals with moderate to high alcohol consumption, hepatitis B or C, elevated transferrin saturation or a history of diabetes mellitus, the authors use the elevated ALT as a NAFLD. After these exclusions, they found that 2.8% of the population had an elevated ALT. Elevated ALT was associated with younger age, male sex, Mexican-American ethnicity, impaired glucose metabolism and IR, obesity and measures of central adiposity, as well as higher leptin, triglyceride, and C-peptide concentrations. In multivariate analyses, central adiposity, insulin, and leptin concentrations were the most highly associated factors. They concluded that those factors are the major determinants of the association between elevated ALT concentration and higher body weight. In addition, Yokoyama et al[26], in a recent study carried out in 791 Japanese male workers, found that adiponectin concentrations in subjects with increased transaminase activities are significantly lower than those in subjects with normal transaminase activities, which implies that hypoadiponectinemia contributes to an increase in transaminase activity. The finding was further supported by single regression analyses. Together, these results suggest that hypoadiponectinemia may result in fat accumulation in the liver, with the development of fatty liver causing increased mean transaminase activities while leading to an IR state by attenuation of these events.
Considering the higher body fat composition in subjects with HS, higher leptin concentrations were associated with these patients, specifically those with severe steatosis (Table 3 and Figure 2). An increase in leptin concentration suggests that obesity is the result of leptin resistance, probably an environmental effect[9]. In our study, differences in diet variables are evident, with high consumption of calories, total carbohydrate and total fat (Table 2); however, we cannot be categorical, considering that leptin resistance is likely to be the result of a complex interplay of many factors[9,27]. Subjects with HS (particularly grades II–III) have higher leptin concentrations (Figure 2). This result is similar to other reports[28], however it is not observed in all series. Hui et al[24], found this pattern only in men, but other reports do not agree with this finding[29]. Together this indicates that leptin concentration has an influence on weight gain and IR, but its role in NAFLD is not well understood.
Figure 2.
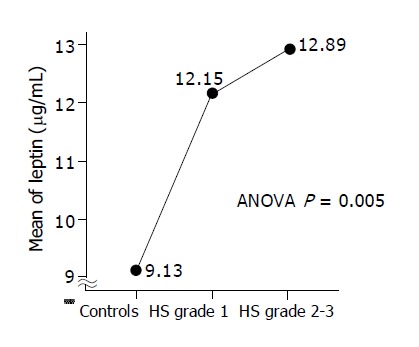
Serum leptin concentrations according to HS severity.
Finally, when we analyzed the subject’s diets, subjects with HS reported a pattern with a greater mean caloric, total fat and iron intake compared with controls. Interestingly, animal and human models suggest that dietary factors can directly affect hepatic fatty infiltration and oxidative damage in different types of liver disease, including alcoholic fatty liver disease[30]. A recent study from Musso and colleagues[4] showed that dietary habits may promote steatohepatitis directly by modulating hepatic triglyceride accumulation and antioxidant activity, as well as indirectly by affecting insulin sensitivity and postprandial triglyceride metabolism. Taking together these observations, we can postulate that it is possible to use specific alimentary interventions to prevent HS.
In conclusion, the results of this study suggest that high levels of adiponectin are associated with a protective effect against HS.
Footnotes
Science Editor Guo SY Language Editor Elsevier HK
References
- 1.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–1110. doi: 10.1002/hep.1840120505. [DOI] [PubMed] [Google Scholar]
- 2.Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, Luketic VA, Shiffman ML, Clore JN. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–1192. doi: 10.1053/gast.2001.23256. [DOI] [PubMed] [Google Scholar]
- 3.Wang RT, Koretz RL, Yee HF. Is weight reduction an effective therapy for nonalcoholic fatty liver? A systematic review. Am J Med. 2003;115:554–559. doi: 10.1016/s0002-9343(03)00449-2. [DOI] [PubMed] [Google Scholar]
- 4.Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, Fagà E, Silli B, Pagano G. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003;37:909–916. doi: 10.1053/jhep.2003.50132. [DOI] [PubMed] [Google Scholar]
- 5.García Monzón C. Non-alcoholic steatohepatitis. Gastroenterol Hepatol. 2001;24:395–402. [PubMed] [Google Scholar]
- 6.Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409–2415. doi: 10.1172/JCI117936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein BJ, Scalia R. Adiponectin: A novel adipokine linking adipocytes and vascular function. J Clin Endocrinol Metab. 2004;89:2563–2568. doi: 10.1210/jc.2004-0518. [DOI] [PubMed] [Google Scholar]
- 8.Day CP, James OF. Hepatic steatosis: innocent bystander or guilty party? Hepatology. 1998;27:1463–1466. doi: 10.1002/hep.510270601. [DOI] [PubMed] [Google Scholar]
- 9.Friedman JM. The function of leptin in nutrition, weight, and physiology. Nutr Rev. 2002;60:S1–S14; discussion S68-S84, S85-S87. doi: 10.1301/002966402320634878. [DOI] [PubMed] [Google Scholar]
- 10.Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, Mullen KD, Cooper JN, Sheridan MJ. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–750. doi: 10.1053/gast.2002.35354. [DOI] [PubMed] [Google Scholar]
- 11.Hernández-Avila M, Romieu I, Parra S, Hernández-Avila J, Madrigal H, Willett W. Validity and reproducibility of a food frequency questionnaire to assess dietary intake of women living in Mexico City. Salud Publica Mex. 1998;40:133–140. doi: 10.1590/s0036-36341998000200005. [DOI] [PubMed] [Google Scholar]
- 12.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 13.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 14.Angulo P. Treatment of nonalcoholic fatty liver disease. Ann Hepatol. 2002;1:12–19. [PubMed] [Google Scholar]
- 15.Hara T, Fujiwara H, Shoji T, Mimura T, Nakao H, Fujimoto S. Decreased plasma adiponectin levels in young obese males. J Atheroscler Thromb. 2003;10:234–238. doi: 10.5551/jat.10.234. [DOI] [PubMed] [Google Scholar]
- 16.Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, Tataranni PA. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab. 2001;86:1930–1935. doi: 10.1210/jcem.86.5.7463. [DOI] [PubMed] [Google Scholar]
- 17.Matsubara M, Maruoka S, Katayose S. Decreased plasma adiponectin concentrations in women with dyslipidemia. J Clin Endocrinol Metab. 2002;87:2764–2769. doi: 10.1210/jcem.87.6.8550. [DOI] [PubMed] [Google Scholar]
- 18.Ryysy L, Häkkinen AM, Goto T, Vehkavaara S, Westerbacka J, Halavaara J, Yki-Järvinen H. Hepatic fat content and insulin action on free fatty acids and glucose metabolism rather than insulin absorption are associated with insulin requirements during insulin therapy in type 2 diabetic patients. Diabetes. 2000;49:749–758. doi: 10.2337/diabetes.49.5.749. [DOI] [PubMed] [Google Scholar]
- 19.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–2556. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 20.Berg AH, Combs TP, Du X, Brownlee M, Scherer PE. The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med. 2001;7:947–953. doi: 10.1038/90992. [DOI] [PubMed] [Google Scholar]
- 21.Maeda N, Takahashi M, Funahashi T, Kihara S, Nishizawa H, Kishida K, Nagaretani H, Matsuda M, Komuro R, Ouchi N, et al. PPARgamma ligands increase expression and plasma concentrations of adiponectin, an adipose-derived protein. Diabetes. 2001;50:2094–2099. doi: 10.2337/diabetes.50.9.2094. [DOI] [PubMed] [Google Scholar]
- 22.Maeda N, Shimomura I, Kishida K, Nishizawa H, Matsuda M, Nagaretani H, Furuyama N, Kondo H, Takahashi M, Arita Y, et al. Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med. 2002;8:731–737. doi: 10.1038/nm724. [DOI] [PubMed] [Google Scholar]
- 23.Xu A, Wang Y, Keshaw H, Xu LY, Lam KS, Cooper GJ. The fat-derived hormone adiponectin alleviates alcoholic and nonalcoholic fatty liver diseases in mice. J Clin Invest. 2003;112:91–100. doi: 10.1172/JCI17797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hui JM, Hodge A, Farrell GC, Kench JG, Kriketos A, George J. Beyond insulin resistance in NASH: TNF-alpha or adiponectin? Hepatology. 2004;40:46–54. doi: 10.1002/hep.20280. [DOI] [PubMed] [Google Scholar]
- 25.Ruhl CE, Everhart JE. Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology. 2003;124:71–79. doi: 10.1053/gast.2003.50004. [DOI] [PubMed] [Google Scholar]
- 26.Yokoyama H, Hirose H, Ohgo H, Saito I. Inverse association between serum adiponectin level and transaminase activities in Japanese male workers. J Hepatol. 2004;41:19–24. doi: 10.1016/j.jhep.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 27.Leibel RL. The role of leptin in the control of body weight. Nutr Rev. 2002;60:S15–S19; discussion S68-S84, S85-S87. doi: 10.1301/002966402320634788. [DOI] [PubMed] [Google Scholar]
- 28.Uygun A, Kadayifci A, Yesilova Z, Erdil A, Yaman H, Saka M, Deveci MS, Bagci S, Gulsen M, Karaeren N, et al. Serum leptin levels in patients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2000;95:3584–3589. doi: 10.1111/j.1572-0241.2000.03297.x. [DOI] [PubMed] [Google Scholar]
- 29.Yannakoulia M, Yiannakouris N, Blüher S, Matalas AL, Klimis-Zacas D, Mantzoros CS. Body fat mass and macronutrient intake in relation to circulating soluble leptin receptor, free leptin index, adiponectin, and resistin concentrations in healthy humans. J Clin Endocrinol Metab. 2003;88:1730–1736. doi: 10.1210/jc.2002-021604. [DOI] [PubMed] [Google Scholar]
- 30.Mezey E. Dietary fat and alcoholic liver disease. Hepatology. 1998;28:901–905. doi: 10.1002/hep.510280401. [DOI] [PubMed] [Google Scholar]


