Abstract
AIM: To ascertain the molecule mechanism of nuclear factor-κB (NF-κB) inhibitor curcumin preventive and therapeutic effects in rats’ colitis induced by trinitrobenzene sulfonic acid (TNBS).
METHODS: Sixty rats with TNBS-induced colitis were treated with 2.0% curcumin in the diet. Thirty positive control rats were treated with 0.5% sulfasalazine (SASP). Thirty negative control rats and thirty model rats were treated with general diet. Changes of body weight together with histological scores were evaluated. Survival rates were also evaluated. Cell nuclear NF-κB activity in colonic mucosa was evaluated by using electrophoretic mobility shift assay. Cytoplasmic IκB protein in colonic mucosa was detected by using Western Blot analysis. Cytokine messenger expression in colonic tissue was assessed by using semiquantitative reverse-transcription polymerase chain reaction.
RESULTS: Treatment with curcumin could prevent and treat both wasting and histopathologic signs of rats with TNBS-induced intestinal inflammation. In accordance with these findings, NF-κB activation in colonic mucosa was suppressed in the curcumin-treated groups. Degradations of cytoplasmic IκB protein in colonic mucosa were blocked by curcumin treatment. Proinflammatory cytokine messenger RNA expression in colonic mucosa was also suppressed.
CONCLUSION: This study shows that NF-κB inhibitor curcumin could prevent and improve experimental colitis in murine model with inflammatory bowel disease (IBD). The findings suggest that NF-κB inhibitor curcumin could be a potential target for the patients with IBD.
Keywords: IBD, Curcumin, TNBS, NF-κB
INTRODUCTION
Intestinal mucosa has functions of excretion, absorbability, immunity and barrier. Mucosal barrier function is composed of intestinal epithelial cells, components outside cells and immune system. They can block deleterious matter from entering the body. Mucosal barrier function is preternatural when intestinal inflammation occurs. Pathogenesis of inflammatory bowel disease (IBD) is ambiguous. IBD includes ulcerative colitis (UC) and Crohn’s disease (CD) in the clinic. Both of them are characterized by mucosal inflammation in pathologic histology[1,2]. The common point in mucosal inflammation research has been offered for preventing and treating IBD. It is important for scientists in the digestive domain. Intestinal mucosal inflammation induced by environment, descendiblity and immunity. Immunity is crucial above all. Homeostasis of TH1/TH2 type cytokines is important in intestinal mucosal immunity. Proinflammatory cytokines were significantly enhanced and anti-inflammatory cytokines were decreasing in intestinal inflammation.
Incidence of IBD is high in the western countries. It is increasing in countries of Asia year after year. Treatments for IBD in clinic cause big side effects. Their aims are ambiguous and they are costly. Their curative effects are not satisfying. Filtrating high effects and low toxicity of natural anti-inflammatory medications are desired for the treatment of patients with IBD. Curcumin is a natural plant phenolic active component. Spice curcumin has different pharmacologic effects, including antitumor, antioxidation and anti-inflammatory modulation of immunity functions[3-6]. The pleiotropic effects of curcumin owe to inhibition of transcriptional factor nuclear NF-κB. A study had shown that curcumin blocks a signal upstream of NF-κB-inducing kinase and IκB kinase in intestinal epithelial cells[7]. The study was promising to ascertain via molecule mechanism whether NF-κB inhibitor curcumin prevents and cures intestinal mucosal inflammation in IBD. Using rats colitis model induced by TNBS, this research is to ascertain preventive and therapeutic effects of NF-κB inhibitor curcumin. At the same time, it is also to ascertain its molecule mechanism of pharmacologic effects in intestinal mucosal inflammation.
MATERIALS AND METHODS
Animals and grouping
In this study, 10-12 wk old and 200-250 g male SPF Wistar rats were used. All rats were bred under clean barrier conditions in Animal Laboratorial Center of First Military Medical University. Rats were randomly divided into 5 groups: negative control group, positive model group, treatment positive control group, curcumin preventive group, curcumin therapeutic group.
Model of colitis and treatment
To induce intestinal inflammation model by portion of 50 mg hapten TNBS (Sigma Company) in 2 mL 50% ethanol. 2 mL mixed liquor was fleetly injected into the intestine of each group of Wistar rats while negative control rats received 2 mL 50% ethanol.
Curcumin (purity, 95%) was purchased from BDH Company in England. For dietary administration, curcumin was mixed with the feed to concentrations 2.0%. Preventive group rats were administered 2.0% curcumin starting 3 d before administration of TNBS (group 4, 2.0% CUR-P). Therapeutic group rats were administered 2.0% curcumin just after administration of TNBS (group 5, 2.0% CUR-A). Sulfasalazine (SASP) was mixed with the feed to a concentration of 0.5%. Treatment positive control rats were treated with 0.5% SASP starting 3 d before administration of TNBS (group 3, 0.5% SASP). Negative control rats were treated with general feed after administration of 50% ethanol (group 1, ETHA). Positive model rats were treated with general feed (group 2, TNBS). Two weeks after administration of TNBS, all the rats were killed.
Histological analysis and grades
For histological analysis, rats’ colons were fixed in 40 g/L formaldehyde, and paraffin-embedded tissue sections were stained with HE (hematoxylin and eosin) using standard techniques. Histological changes were graded[8]: 0, no signs of inflammation; 1, very low level of leukocyte infiltration; 2, low level of leukocyte infiltration; 3, high level of leukocyte infiltration, high vascular density, and thickening of the colon wall; 4, leukocyte transmural infiltration, loss of goblet cells, high vascular density and thickening of the colon wall.
NF-κB activation analysis
Proteins extracts were prepared according to the method of the Nuclear Extract Kit (Active Motif Company). The Nuclear Extract Kit has been developed for the preparation of nuclear, cytoplasmic extracts from rat’s tissue. Protein was stored at -80 °C. Protein concentrations were measured by Bradford assay.
For electrophoretic mobility shift assay to monitor NF-κB activation of intestinal mucosa, 10 μg of nuclear extracts was preincubated- in 10 μL reaction buffer [2 ng poly dI_dC (Sigma Company), 25% glycerol, 1 mol/L NaCl, 10 mmol/L MgCl2, 10 mmol/L DTT, 0.2 mol/L Tris HCl, 10 mmol/L EDTA] for 15 min at room temperature. As a controlmeasure, 1 μL 200-fold molar excess of cold NF-κB competitor oligonucleotide probe was added during preincubation. After pre-incubation, 25000-50000 CPM 32P end-labeled NF-κB oligonucleotide hot probe (5’-AGTTGGGGACTTTCCCAGGC-3’; 3’-CTCCCCTGAAAGGGTCCGTTGA-5’; composed by Shanghai Sangon Biological Engineering Company) was added to the reaction mixture and incubated for 30 min. The reaction mixture was loaded onto a 8% polyacrylamide gel containing Tris-borate-ethylenediamine-tetraacetic acid buffer and electrophoresis was performed at 130 V for 3 h. Gels were dried and exposed to Kodak X-ray film.
IκB degradations analysis
Using the same technique as herein before narrated for cytoplasmic protein extracts and protein concentrations measure. Using Western blot analysis to monitor degradations of cytoplasmic IκB protein of intestinal mucosa. For each sample, equal amounts (50 μg, 20 μL) of protein lysates were heated to 97 °C for 5 min and loaded onto 12% SDS-PAGE gel. Proteins were electrotransfered to PVDF membranes (Bio-Rad Company) by BIO-RAD TRANS-BLOT SEMI-DRY TRANSGER CELL apparatus, blocked in Blocking Buffer (1×TBS, 0.1% Tween with 50 g/L nonfat dry milk) for 1 h at room temperature, and then incubated membrane and 1:500 rabbit polyclonal anti-IκBα primary antibody overnight at 4 °C. (Santa Cruz Biotechnology Company). Incubated membrane with 1:5000 Peroxidase-Conjugated (HRP-conjugated) secondary antibodies for 1 h at room temperature, and then to detect protein marker in ECL Western blotting detection reagents (Amersham Company). Exposed to Kodak X-ray film are developed.
Cytokine IL1β and IL10 mRNA analysis
Semi-quantitative RT-PCR analysis of IL1β and IL10 mRNA was extracted from total RNA from 50 to 100 mg colon mucosa with TRIzol Reagent (Invitrogen Company). The 1 μg RNA was converted to complementary DNA using random hexonucleotides in 10 μL of reverse-transcription reaction solution and then used for polymerase chain reaction, and then using Oligo-dT Primer and M-MuLV reverse transcriptases (Promega Company). For PCR amplification, one-fourth of the reverse transcription product and 10 mmol/L of each oligonucleotide as primers were used. After one denaturation step at 95 °C for 5 min, 30 cycles of amplification were performed: denaturation at 94 °C for 30 s, annealing at 47 °C for 45 s, synthesis at 72 °C for 1 min, and extension at 72 °C for 5 min. The primers used were as follows: to check cDNA quality, GAPDH sense: 5’-ACCACAGTCCATGCCATCAC-3’, GAPDH antisense 5’-TCCACCACCCTGTTGCTGTA-3’ (452 bp); IL1β sense: 5’-CTTCTTCTTTGGGTATTGTT-3’, IL1β antisense: 5’-CCTCTGTGACTCGTGGGA-3’ (325 bp); IL10 sense: 5’-GCAGACAAACAATACGC-3’ IL10 antisense: 5’-ACTTGCCCTCATCCC-3’ (264 bp). One-tenth of the amplified products was run on 1% agarose gels in 1×Tris-borate-ethylenediamine-tetraacetic acid buffer and visualized with ethidium bromide.
Statistics analysis
The results of rats’ body weight were expressed as mean±SE. The Survival rates comparison was determined by the χ2 test, with P<0.05 considered significant. Statistics of histologic scores were determined by Two-Independent Samples Tests, with P<0.05 was considered significant. All data were automatically performed by statistical software.
RESULTS
Effects of curcumin on the survival rate of rats with TNBS-induced colitis
As shown in Figure 1, the survival-rate of positive model rats with TNBS-induced colitis was 60%. The survival rate of negative control rats with 50% ethanol was 100%. In preventive and therapeutic model, the survival rates of rats were 93.33% and 80%. The survival rate of positive control rats treated with 0.5% SASP was 76.67%. Compared to that of rats with colitis, the survival rate of rats treated with medicine was significantly higher. However, the survival rate of 2.0% curcumin preventive mode is particular (against group 2, P<0.02). According to the data, preventive treatment with curcumin is capable of increasing the survival rate of rats with colitis induced by TNBS.
Figure 1.

Effects of curcumin on the survival rate of rats with TNBS-induced colitis. Group 1: 50% ethanol group. Group 2: TNBS group. Group 3: 0.5 % SASP group. Group 4: 2.0% curcumin preventive group. Group 5: 2.0% curcumin therapeutic group.
Effects of curcumin on body weight of rat with TNBS-induced colitis
As shown in Figure 2, body weights of positive model rats, with TNBS-induced colitis, had obviously decreased (more than 15% after 2 d); body weights had recovered gradually from d 6 but not fully to the initial weights in 2 wk. Negative control rats receiving 50% ethanol without TNBS had gained weights. However, body weights had increased to 113.3% of the initial weights in 2 wk. In all groups of rats with treatment, body weights recovered from d 2. Body weights were significantly higher than those of untreated positive model rats on d 2-14. Body weights in the group of 50% ethanol were significantly higher than those of other groups (P<0.05). Body weights in the group of TNBS were significantly lower than those of other groups (P<0.05). Body weights in three groups of treated rats had no significant difference (P>0.05).
Figure 2.

Effects of curcumin on body weights of rats with TNBS-induced colitis. ■: 50%ethanol group. ●: TNBS group. 〇: 0.5 % SASP group. ◆: 2.0% curcumin preventive group. ▲: 2.0% curcumin therapeutic group.
Effects of curcumin on histologic scores of rats with TNBS-induced colitis
We have characterized the histological features of colitis in rats subjected to TNBS enema by staining with HE (Figures 3A-E). Then we evaluated the effects of curcumin on TNBS-induced colon lesions on histologic scores. The results of histologic scores were shown in Table 1. In the mucosa of rats with TNBS-induced colitis, many dispersive and focal ulcers were detected. Dilapidation of tissues epithelium induced inflammatory infiltration. There was a very high level of leukocyte infiltration accompanied with obvious tissues putrescence. In the mucosa of rats of 2.0% curcumin preventive and therapeutic groups, low level of inflammation was detected. Mucosal inflammation of curcumin groups was significantly decreasing than that of untreated groups. In this experiment, the histologic scores of 2.0% curcumin and 0.5% SASP-treated rats were significantly lower than that of untreated rats with colitis (50% ethanol group against TNBS group P<0.01, TNBS group against three medication groups P<0.05).
Figure 3.

Results are shown as the intestinal histologic features of each group rats stained with HE. A: 50% ethanol group; B: TNBS group; C: 0.5 % SASP group; D: 2.0% curcumin preventive group; E: 2.0% curcumin therapeutic group.
Table 1.
Histologic scores of rats with TNBS-induced colitis.
| Group | Cases |
Histologic Scores |
||||
| 0Grade | 1Grade | 2Grade | 3Grade | 4Grade | ||
| ETHA | 30 | 9b | 17b | 3b | 1b | 0b |
| TNBS | 18 | 0 | 2 | 4 | 5 | 7 |
| 0.5%SASP | 23 | 0a | 6a | 9a | 6a | 2a |
| 2%CUR-P | 28 | 1a | 14a | 9a | 3a | 1a |
| 2%CUR-A | 24 | 0a | 7a | 10a | 5a | 2a |
| Count | 123 | 10 | 46 | 35 | 20 | 12 |
P<0.05 ,
P<0.01 vs TNBS group.
Effects of curcumin on NF-κB activity of colonic mucosa in rats with TNBS-induced colitis
As shown in Figure 4, we performed electrophoretic mobility shift assay using nuclear extracts of colonic mucosa from each model rat. Unlabeled specific oligonucleotides of 200-fold molar excess inhibited NF-κB mobility shift (Lane 2), indicating that the DNA-protein complex is specific. This land was cold probe control for the other lands. Unlabeled probes of 200-fold molar excess were added to the reaction mixture of lane 3 (Lane 2). The administration of 50% ethanol had not activated NF-κB DNA binding activity of nuclear extracts in the colonic mucosa. The administration of TNBS alone had enhanced NF-κB DNA binding activity (Lanes 3, 4), which was suppressed by treatment with 0.5% SASP (Lane 5) and 2.0% curcumin (Lanes 6, 7).
Figure 4.

Effects of curcumin on NF-κB activity of colonic mucosa in rats with TNBS-induced colitis. Lane 1: 50% ethanol group; lane 2: cold probe control group; lanes 3 and 4: TNBS group; lane 5: 0.5 % SASP group; lane 6: 2.0% curcumin preventive group; lane 7: 2.0% curcumin therapeutic group.
Effects of curcumin on cytoplasmic IκB degradations
Since NF-κB activity is controlled by the steady state level of IκB, we further investigated the effect of curcumin on IκB degradation in rat’s colonic mucosa. As shown in Figure 5, IκB protein levels were analyzed by Western blotting, respectively using cytoplasmic extracts of colonic mucosa from each model rat. 50% ethanol groups had a high level of cytoplasmic IκB (Lanes 1, 2). Intestinal inflammation of TNBS group induced significative IκB degradation (Lane 3). IκB degradations were both blocked by 0.5% SASP and 2% curcumin treatment (Lanes 4, 5, 6).
Figure 5.
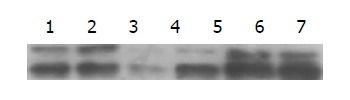
Results are shown as effects of curcumin on IκB degradations. Lanes 1, 2: 50% ethanol group; lane 3: TNBS group; lane 4: 0.5% SASP group; lane 5: 2.0% curcumin preventive group; lane 6: 2.0% curcumin therapeutic group.
Effects of curcumin on expression of cytokine genes in the colonic mucosa in TNBS-induced colitis
By reverse-transcription polymerase chain reaction analysis, our results showed that mRNA levels of proinflammatory cytokine, such as IL-1β, in colon specimens from rats with TNBS-induced colitis, was significantly higher than that in normal controls. Anti-inflammatory cytokine IL-10 level in colon specimens from rats with TNBS-induced colitis was relatively lower than that in normal control, but there was no significant difference between the two groups. High IL-1β mRNA expression was observably suppressed in colon specimens from curcumin-treated and SASP-treated rats with TNBS-induced colitis. Low IL-1β mRNA expression was observably increased in colon specimens from curcumin-treated and SASP-treated rats with TNBS-induced colitis (Figure 6).
Figure 6.

Effects of curcumin on expression of cytokine IL-1β mRNA(A) and IL-10 mRNA(B) in the colonic mucosa in TNBS-induced colitis. Lane M: DNA MARKER. Lane 1: 50% ethanol group; lane 2: TNBS group; Land 3: 0.5% SASP group; lane 4: 2.0% curcumin preventive group; Land 5: 2.0% curcumin therapeutic group.
DISCUSSION
Homeostasis of TH1/TH2 type cytokines is important in intestinal mucosal immunity. T helper cells excrete a lot of cytokines and chemokines in normal intestinal tissue. They induce other types of cell infiltration, such as leukocytes, monocytes, macrophages and other lymphocytes. They induce inflammatory and immune responses aiming nosogenesis outside cells which could straightly or indirectly cause damage of intestinal epithelial cells. Most notable CD and UC and other chronic evolutional intestinal inflammation are all mediated by proinflammatory immune responses induced by diversified antigens. However, studies had made sure that TH1 type cytokines play a predominant role in intestinal mucosal immunity either in various animal models of IBD or in patients with IBD. Proinflammatory cytokines were significantly high expression and anti-inflammatory cytokines were low expression. Expression of proinflammatory cytokines in TH1 type immune response such as IL-1β, IL-6, IL-12, IL-18 , TNF-α and IFN-γ in intestinal mucosa of animal models and humans IBD were significantly enhanced[9-12]. Expression of anti-inflammatory cytokines such as IL-4, IL-5 and IL-10 were low level[12-15].
In our animal experimental model of IBD induced by TNBS, treatment with 2% curcumin and 0.5% SASP can suppress proinflammatory cytokine IL-1β mRNA high expression and increase anti-inflammatory cytokine IL-10 mRNA low expression in colonic mucosa.
Canonical pathway of NF-κB activation selectively regulates diversified inflammatory cytokines chemotactic cytokines and conglutinant cytokines[16,17]. The movement of activation NF-κB into the cellular nucleus is controlled by the targeted phosphorylation and subsequent degradation of IκB. Studies have elaborated several important and unexpected findings that explain mechanisms of NF-κB activation. In the nucleus, NF-κB dimers bind to target DNA elements and activate transcription of genes encoding proteins involved with immune or inflammation responses and with cell growth control[18].
Previous observations provide evidence for IBD that NF-κB activation is significantly elevated in UC and CD[19]. SASP, mesalamine, and corticosteroids having been used in different formulations for the treatment of patients with both acute and chronic IBD in clinic during the past decades, which all are NF-κB inhibitors[3,20-22]. They have sundry defects such as steroid dependence and steroid resistance, decreasing glucose tolerance, hypohepatia and pancreatitis. Now, more potent and selective treatment strategies with anti-sense p65 for IBD, aim at the prevention of NF-κB activation in mucosal macrophages and T lymphocytes. However, NF-κB regulated genes are also involved in survival responses of epithelial cells[20].
Curcumin is the major constituent of turmeric powder extracted from the rhizomes of the plant Curcuma longa Linn. Curcumin is used as a spice to give the specific flavor and yellow color to curry[23]. As a traditional medicine, turmeric has also been widely used for centuries to treat inflammatory disorders in its original countries[24]. In our report, we analyzed the effect of NF-κB inhibitor curcumin on preventing and curing TNBS-induced colitis in rats. Scientists had understood curcumin mechanism of action in regulating the NF-κB/IκB pathway. Phosphorylation of IκB on serines 32 and 36 is necessary for its degradation and consequent NF-κB activation[25-28]. Curcumin could inhibit the activation of NF-κB in different type of cells[7,29-31]. Curcumin blocks a signal upstream of NF-κB-inducing kinase and IκB kinase using intestinal epithelial cells[7]. Our report indicated that curcumin and SASP are acting on a common component in the signaling pathways. Blockade of IκB degradation by them could involve decrease of IκB phosphorylation or inhibition of various kinases activity. We studied preventive and therapeutic effects of NF-κB inhibitor curcumin in rats with TNBS-induced colitis. Preventive treatment with curcumin could evidently increase survival rate of colitis rats and ameliorate histopathologic signs of TNBS-induced intestinal inflammation. This study provides a strong rational base of curcumin preventing IBD. We suggested that curcumin be applied for patients with IBD in clinic in the near future.
ACKNOWLEDGEMENTS
Thanks are due to Professor Wen-Li Ma and Dr. Bao Zhang for assistance with the experiments in Chinese PLA Institute of Molecular Biology, First Military Medical University.
Footnotes
Supported by the National Natural Science Foundation of China, No. 30270078 and the Guangdong Traditional Chinese and Medicine Bureau Foundation of China, No. 1040191
References
- 1.Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115:182–205. doi: 10.1016/s0016-5085(98)70381-6. [DOI] [PubMed] [Google Scholar]
- 2.Targan SR, Murphy LK. Clarifying the causes of Crohn's. Nat Med. 1995;1:1241–1243. doi: 10.1038/nm1295-1241. [DOI] [PubMed] [Google Scholar]
- 3.Zhou S, Lim LY, Chowbay B. Herbal modulation of P-glycoprotein. Drug Metab Rev. 2004;36:57–104. doi: 10.1081/dmr-120028427. [DOI] [PubMed] [Google Scholar]
- 4.Ambegaokar SS, Wu L, Alamshahi K, Lau J, Jazayeri L, Chan S, Khanna P, Hsieh E, Timiras PS. Curcumin inhibits dose-dependently and time-dependently neuroglial cell proliferation and growth. Neuro Endocrinol Lett. 2003;24:469–473. [PubMed] [Google Scholar]
- 5.Kang G, Kong PJ, Yuh YJ, Lim SY, Yim SV, Chun W, Kim SS. Curcumin suppresses lipopolysaccharide-induced cyclooxygenase-2 expression by inhibiting activator protein 1 and nuclear factor kappab bindings in BV2 microglial cells. J Pharmacol Sci. 2004;94:325–328. doi: 10.1254/jphs.94.325. [DOI] [PubMed] [Google Scholar]
- 6.Chueh SC, Lai MK, Liu IS, Teng FC, Chen J. Curcumin enhances the immunosuppressive activity of cyclosporine in rat cardiac allografts and in mixed lymphocyte reactions. Transplant Proc. 2003;35:1603–1605. doi: 10.1016/s0041-1345(03)00377-4. [DOI] [PubMed] [Google Scholar]
- 7.Jobin C, Bradham CA, Russo MP, Juma B, Narula AS, Brenner DA, Sartor RB. Curcumin blocks cytokine-mediated NF-kappa B activation and proinflammatory gene expression by inhibiting inhibitory factor I-kappa B kinase activity. J Immunol. 1999;163:3474–3483. [PubMed] [Google Scholar]
- 8.Neurath MF, Fuss I, Kelsall BL, Stüber E, Strober W. Antibodies to interleukin 12 abrogate established experimental colitis in mice. J Exp Med. 1995;182:1281–1290. doi: 10.1084/jem.182.5.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strober W, Fuss IJ, Ehrhardt RO, Neurath M, Boirivant M, Lúdvíksson BR. Mucosal immunoregulation and inflammatory bowel disease: new insights from murine models of inflammation. Scand J Immunol. 1998;48:453–458. [PubMed] [Google Scholar]
- 10.Boismenu R, Chen Y. Insights from mouse models of colitis. J Leukoc Biol. 2000;67:267–278. doi: 10.1002/jlb.67.3.267. [DOI] [PubMed] [Google Scholar]
- 11.Rogler G, Andus T. Cytokines in inflammatory bowel disease. World J Surg. 1998;22:382–389. doi: 10.1007/s002689900401. [DOI] [PubMed] [Google Scholar]
- 12.Maerten P, Shen C, Colpaert S, Liu Z, Bullens DA, van Assche G, Penninckx F, Geboes K, Vanham G, Rutgeerts P, et al. Involvement of interleukin 18 in Crohn's disease: evidence from in vitro analysis of human gut inflammatory cells and from experimental colitis models. Clin Exp Immunol. 2004;135:310–317. doi: 10.1111/j.1365-2249.2004.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li MC, He SH. IL-10 and its related cytokines for treatment of inflammatory bowel disease. World J Gastroenterol. 2004;10:620–625. doi: 10.3748/wjg.v10.i5.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart AL, Kamm MA, Knight SC, Stagg AJ. Quantitative and functional characteristics of intestinal-homing memory T cells: analysis of Crohn's disease patients and healthy controls. Clin Exp Immunol. 2004;135:137–145. doi: 10.1111/j.1365-2249.2004.02347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melgar S, Yeung MM, Bas A, Forsberg G, Suhr O, Oberg A, Hammarstrom S, Danielsson A, Hammarstrom ML. Over-expression of interleukin 10 in mucosal T cells of patients with active ulcerative colitis. Clin Exp Immunol. 2003;134:127–137. doi: 10.1046/j.1365-2249.2003.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnes PJ, Karin M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997;336:1066–1071. doi: 10.1056/NEJM199704103361506. [DOI] [PubMed] [Google Scholar]
- 17.Monaco C, Andreakos E, Kiriakidis S, Mauri C, Bicknell C, Foxwell B, Cheshire N, Paleolog E, Feldmann M. Canonical pathway of nuclear factor kappa B activation selectively regulates proinflammatory and prothrombotic responses in human atherosclerosis. Proc Natl Acad Sci USA. 2004;101:5634–5639. doi: 10.1073/pnas.0401060101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baldwin AS. The NF-kappa B and I kappa B proteins: new discoveries and insights. Annu Rev Immunol. 1996;14:649–683. doi: 10.1146/annurev.immunol.14.1.649. [DOI] [PubMed] [Google Scholar]
- 19.Monteleone G, Mann J, Monteleone I, Vavassori P, Bremner R, Fantini M, Del Vecchio Blanco G, Tersigni R, Alessandroni L, Mann D, et al. A failure of transforming growth factor-beta1 negative regulation maintains sustained NF-kappaB activation in gut inflammation. J Biol Chem. 2004;279:3925–3932. doi: 10.1074/jbc.M303654200. [DOI] [PubMed] [Google Scholar]
- 20.Farrell RJ, Kelleher D. Glucocorticoid resistance in inflammatory bowel disease. J Endocrinol. 2003;178:339–346. doi: 10.1677/joe.0.1780339. [DOI] [PubMed] [Google Scholar]
- 21.Dijkstra G, Moshage H, Jansen PL. Blockade of NF-kappaB activation and donation of nitric oxide: new treatment options in inflammatory bowel disease? Scand J Gastroenterol Suppl. 2002;236:37–41. doi: 10.1080/003655202320621436. [DOI] [PubMed] [Google Scholar]
- 22.Nikolaus S, Fölscn U, Schreiber S. Immunopharmacology of 5-aminosalicylic acid and of glucocorticoids in the therapy of inflammatory bowel disease. Hepatogastroenterology. 2000;47:71–82. [PubMed] [Google Scholar]
- 23.Calabrese V, Scapagnini G, Colombrita C, Ravagna A, Pennisi G, Giuffrida Stella AM, Galli F, Butterfield DA. Redox regulation of heat shock protein expression in aging and neurodegenerative disorders associated with oxidative stress: a nutritional approach. Amino Acids. 2003;25:437–444. doi: 10.1007/s00726-003-0048-2. [DOI] [PubMed] [Google Scholar]
- 24.Jain SK. Ethnobotany and research on medicinal plants in India. Ciba Found Symp. 1994;185:153–164; discussion 164-168. [PubMed] [Google Scholar]
- 25.Brown K, Gerstberger S, Carlson L, Franzoso G, Siebenlist U. Control of I kappa B-alpha proteolysis by site-specific, signal-induced phosphorylation. Science. 1995;267:1485–1488. doi: 10.1126/science.7878466. [DOI] [PubMed] [Google Scholar]
- 26.Chen Z, Hagler J, Palombella VJ, Melandri F, Scherer D, Ballard D, Maniatis T. Signal-induced site-specific phosphorylation targets I kappa B alpha to the ubiquitin-proteasome pathway. Genes Dev. 1995;9:1586–1597. doi: 10.1101/gad.9.13.1586. [DOI] [PubMed] [Google Scholar]
- 27.Chen ZJ, Parent L, Maniatis T. Site-specific phosphorylation of IkappaBalpha by a novel ubiquitination-dependent protein kinase activity. Cell. 1996;84:853–862. doi: 10.1016/s0092-8674(00)81064-8. [DOI] [PubMed] [Google Scholar]
- 28.Scherer DC, Brockman JA, Chen Z, Maniatis T, Ballard DW. Signal-induced degradation of I kappa B alpha requires site-specific ubiquitination. Proc Natl Acad Sci USA. 1995;92:11259–11263. doi: 10.1073/pnas.92.24.11259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh S, Aggarwal BB. Activation of transcription factor NF-kappa B is suppressed by curcumin (diferuloylmethane) [corrected] J Biol Chem. 1995;270:24995–25000. doi: 10.1074/jbc.270.42.24995. [DOI] [PubMed] [Google Scholar]
- 30.Kumar A, Dhawan S, Hardegen NJ, Aggarwal BB. Curcumin (Diferuloylmethane) inhibition of tumor necrosis factor (TNF)-mediated adhesion of monocytes to endothelial cells by suppression of cell surface expression of adhesion molecules and of nuclear factor-kappaB activation. Biochem Pharmacol. 1998;55:775–783. doi: 10.1016/s0006-2952(97)00557-1. [DOI] [PubMed] [Google Scholar]
- 31.Bierhaus A, Zhang Y, Quehenberger P, Luther T, Haase M, Müller M, Mackman N, Ziegler R, Nawroth PP. The dietary pigment curcumin reduces endothelial tissue factor gene expression by inhibiting binding of AP-1 to the DNA and activation of NF-kappa B. Thromb Haemost. 1997;77:772–782. [PubMed] [Google Scholar]


