Abstract
AIM: To study the effect of a number of chemotherapeutic drugs on five human intrahepatic cholangiocarcinoma (CCA) cell lines. The expressions of genes that have been proposed to influence the resistance of chemotherapeutic drugs including thymidylate synthase (TS), dihydropyrimidine dehydrogenase (DPD), glutathione-S-transferase P1 (GSTP1), multidrug resistance protein (MDR1) and multidrug resistance-associated proteins (MRPs) were also determined.
METHODS: Five human CCA cell lines (KKU-100, KKU-M055, KKU-M156, KKU-M214 and KKU-OCA17) were treated with various chemotherapeutic drugs and growth inhibition was determined by 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay. Semi-quantitative levels of gene expression were determined by a reverse transcriptase polymerase chain reaction (RT-PCR). Results of IC50 values and the ratios of gene expression were analyzed by linear regression to predict their relationship.
RESULTS: Among five CCA cell lines, KKU-M055 was the most sensitive cell line towards all chemotherapeutic drugs investigated, particularly taxane derivatives with IC50 values of 0.02-3 nmol/L, whereas KKU-100 was apparently the least sensitive cell line. When compared to other chemotherapeutic agents, doxorubicin and pirarubicin showed the lowest IC50 values (<5 μmol/L) in all five CCA cell lines. Results from RT-PCR showed that TS, MRP1, MRP3 and GSTP1 were highly expressed in these five CCA cell lines while DPD and MRP2 were only moderately expressed. It should be noted that MDR1 expression was detected only in KKU-OCA17 cell lines. A strong correlation was only found between the level of MRP3 expression and the IC50 values of etoposide, doxorubicin and pirarubicin (r = 0.86-0.98, P<0.05).
CONCLUSION: Sensitivity to chemotherapeutic agents is not associated with the histological type of CCA. Choosing of the appropriate chemotherapeutic regimen for the treatment of CCA requires knowledge of drug sensitivity. MRP3 was correlated with resistance of CCA cell lines to etoposide, doxorubicin and pirarubicin, whereas other chemotherapeutic drugs showed no association. The role of this multidrug resistance-associated protein, MRP3, in chemotherapeutic resistance in CCA patients needs to be further investigated.
Keywords: Cholangiocarcinoma, Chemotherapeutic agents, Drug sensitivity, Drug resistance, Multidrug resistance protein, MRP
INTRODUCTION
Cholangiocarcinoma (CCA) is a bile duct tumor which accounts for an approximate 15% of liver cancers worldwide[1]. This cancer can be classified into three major groups including intrahepatic, perihilar and distal extrahepatic CCA. The highest incidence of this cancer has been reported in Laos and Northeastern Thailand[2]. Intrahepatic type is the most common case of CCA in these countries and infestation of Opisthorchis viverrini has been classified as a definite risk factor of the disease[3]. It has recently been reported that the incidence of CCA in developed countries is now increasing. The incidence of intrahepatic CCA in the USA during 1975-1999 was examined using data from the Surveillance Epidemiology and End Result Program[4]. The results revealed that there was a major increase in incidence after 1985 by 165% over the entire period. However, the risk factors of CCA in that population are still unclear. At present, only surgical resection of all detectable tumors is correlated with the improvement in 5-year survival[5,6]. Evidence from clinical studies demonstrated that the response rate of this cancer to chemotherapy is relatively poor in which partial responses have been observed in only approximately 10-20% of cases[7-9]. Improvement in the survival of CCA patients will probably not only rely on more aggressive or advanced surgical techniques but also from the improvement in treatment with chemotherapy. When compared to other cancers, data concerning drug sensitivity and drug resistance in CCA are still limited, this may be due to the fact that this cancer has previously been considered as a rare cancer in developed countries[10-13].
Resistance of cancerous cells to chemotherapeutic drugs is a major cause of the chemotherapeutic failure of chemotherapy[14-16]. Several factors have been hypothesized to play a role in chemotherapeutic drug resistance in cancers including high expression of drug efflux pumps (e.g. multidrug resistance protein [MDR1] and multidrug resistance-associated proteins [MRPs][17]), an increase in detoxification of chemotherapeutic drugs (e.g. glutathione S-transferases [GST][18] and dihydropyrimidine dehydrogenase [DPD][19]), alteration of drug targets and suppression of drug-induced apoptosis[20]. Several lines of evidence suggest that both MDR1 and MRP1 are the major contributors of the multidrug resistance phenotypes observed in a number of tumor cells[21-25].
It has been demonstrated in a CCA cell line, SK-ChA-1, that the resistance of this CCA cell line to 5-FU resulted from an increase in activity of thymidylate synthase (TS), a target enzyme for 5-FU[26]. DPD, the initial and rate-limiting enzyme in catabolism of 5-FU has also been proposed as a predictable marker of 5-FU treatment in several cancers such as colon cancer and hepatocellular carcinoma[26-28]. Association between 5-FU resistance and mRNA expression or high activity of DPD in colorectal tumors has been reported in which high activity and high mRNA expression of DPD have resulted in low sensitivity to 5-FU[19,29,30]. Although 5-FU is the most common chemotherapeutic drug used in the treatment of CCA, the roles of TS and DPD in that cancer are not clear[26-28]. Moreover, glutathione S-transferase P1 (GSTP1) has been found to be associated with drug resistance in some cancers including CCA[13,31].
In order to improve the efficacy of chemotherapy in CCA patients, better understanding in drug sensitivity and the mechanism of drug resistance of this cancer is essential. In the present study, we have screened the effect of a number of chemotherapeutic drugs against five intrahepatic CCA cell lines that represent different histological types. Moreover, the expression of genes that have been proposed to influence chemotherapeutic drug resistance was analyzed in order to characterize the molecular mechanism of drug resistance in CCA.
MATERIALS AND METHODS
Reagents
All chemotherapeutic drugs used in this study were obtained as commercial pharmaceutical products. 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS), oligo(dT)15, rRNasin ribonucleotide inhibitor and M-MLV reverse transcriptase were obtained from Promega, Madison, WI, USA. Ham’s F12, trypsin-EDTA, penicillin G, streptomycin and Taq polymerase were obtained from Invitrogen, Carlsbad, CA, USA. Heat-inactivated fetal calf serum was purchased from Seromed Biochrom AG, Berlin, Germany. Other chemicals used were obtained from Sigma Chemical Co. Ltd., St Louis, MO, USA.
Human CCA cell lines
Five human intrahepatic CCA cell lines; namely KKU-100, KKU-M055, KKU-M156, KKU-M214 and KKU-OCA17 were used in this study. All cell lines were established in our institute from CCA patients residing in opisthorchiasis endemic areas in Northeastern Thailand. KKU-100 was developed from a patient with poorly-differentiated adenocarcinoma. KKU-M055 was also from a patient with a primary tumor of poorly differentiated adenocarcinoma while KKU-M156 and KKU-M214, and KKU-OCA17 were derived from patients with moderately and well-differentiated adenocarcinoma, respectively. All cell lines were cultured in either Ham’s F12, containing 100 U/mL penicillin and 100 µg/mL streptomycin with 10% fetal bovine serum at 37 °C with 50 mL/L CO2. The presence of Mycoplasma contamination was periodically checked. These cell lines have been maintained in our laboratory for more than 5 years.
Cytotoxicity assay
Sensitivity of CCA cell lines to chemotherapeutic drugs was determined by MTS assay as described in a previous study[32]. Briefly, 100 μL of cell suspension (1×105 cells/mL) were added to each well of 96-well flat-bottomed microtiter plates and incubated for 24 h at 37 °C in a humidified 50 mL/L CO2 atmosphere. After incubation, 100 μL of medium containing drug or complete medium for untreated controls were distributed in the 96-well plates and plates were then incubated at 37 °C for 72 h. The culture medium was subsequently removed and 100 μL medium containing 20 μL MTS solution (20 mg/mL) was added to each culture well. The cultures were further incubated for 2 h at 37 °C in a humidified 50 mL/L CO2 atmosphere. Absorbency was measured at 492 nm using a microplate reader (Tecan Austria GmbH, Salburg, Austria). The concentration of drug required to inhibit cell proliferation by 50% (IC50) was determined by plotting the percentage of cell growth inhibition vs the chemotherapeutic drug concentration as previously described[33].
RNA extraction and semi-quantitative RT-PCR reaction
Total RNA was extracted from the human CCA cell lines (2×106 cells) using an RNAeasy Mini Kit (QIAgen, Hilden, Germany), following the manufacturer’s instructions and quantified by spectrophotometry. Total RNA (5 μg) from each cell line was reverse-transcribed in 50 μL containing 250 pmoL of oligo(dT)15 primer, 40 units of rRNasin ribonuclease inhibitor and 250 units of M-MLV reverse trancriptase in 50 mmol/L Tris-HCl, 75 mmol/L KCl, 3 mmol/L MgCl2, 10 mmol/L DTT, and 0.5 mmol/L dNTPs. Initially, RNA and oligo(dT)15 were mixed together and heated at 70 °C for 10 min and immediately chilled on ice for 5 min. Other reagents were then added and incubated for 15 min at 30 °C. First-strand cDNAs were synthesized at 42 °C for 60 min. PCR amplification was performed using specific primers for the gene of interest. The PCR primer sequences are shown in Table 1. Optimization for the number of PCR cycles and first strand cDNA concentration was determined for linear amplification conditions. The expression levels of mRNA were measured using human GAPDH mRNA as an internal control by being co-amplified with each gene in order to minimize tube-to-tube variation in the efficiency of PCR[34].
Table 1.
Primer sequences used in RT-PCR analysis.
| Gene | Size of PCR (bp) | Forward primer | Reverse primer |
| DPD | 514 | TCCTCCAGGTATGCAGTGCCA | GTTATGGTGGGCAGGTGGGTT |
| GAPDH | 328 | CAACAGCCTCAAGATCATCAGC | TTCTAGACGGCAGGTCAGGTC |
| GSTP1 | 199 | TACGGGCAGCTCCCCAAGTT | TGCCCGCCTCATAGTTGGTG |
| MDR1 | 206 | GTCTTTGGTGCCATGGCCGT | ATGTCCGGTCGGGTGGGATA |
| MRP1 | 262 | CTGACAAGCTAGACCATGAATGT | CCTTTGTCCAAGACGATCACCC |
| MRP2 | 202 | GCCAGATTGGCCCAGCAAA | AATCTGACCACCGGCAGCCT |
| MRP3 | 452 | GGGACCCTGCGCATGAACCTG | TAGGCAAGTCCAGCATCTCTGG |
| TS | 579 | GAATCACATCGAGCCACTGAAA | GTGTTACTCAGCTCCCTCAGA |
PCR was carried out in a final volume of 25 μL containing first-strand cDNA, 10 pmoL of each primer, 2 pmoL of each GAPDH primer, 1.25 units of Taq polymerase in 2.5 μL of 10×Taq buffer, 2 mmol/L MgCl2 and 0.2 mmol/L dNTPs, using a RoboCycler gradient 40 (Stratagene, La Jolla, CA, USA). An initial denaturation step at 94 °C for 3 min was followed by 28 cycles comprising a denaturation step at 94 °C for 1 min, annealing at 62 °C (for GSTP1, MRP1, MRP2 and MDR1) or at 56 °C (for TS, DPD and MRP3) for 1 min and extension at 72 °C for 1 min. The final extension was subsequently performed at 72 °C for 10 min. The PCR products were separated on 2% agarose gel electrophoresis containing 100 ng/mL of ethidium bromide. Gels were visualized and photographed on an Electronic Dual Light Transilluminator (Ultralum, Carson, CA, USA). The DNA bands were scanned with an image scanner (Canon Electronics Inc., Saitama, Japan) and analyzed with Image Master 1D (Ambersham Pharmacia Biotech, Piscataway, NJ, USA). The relative amount of mRNA of the gene of interest was expressed as a ratio to GAPDH mRNA.
Statistical analysis
The IC50 values for each chemotherapeutic agent as tested in each of the five CCA cell lines were expressed as mean±SD. Student’s t-test was used for statistical analysis. Association between gene expression profiles and the IC50 for the five CCA cell lines was examined using the linear regression analysis. A P value <0.05 was considered as statistically significant.
RESULTS
Cytotoxic effect
The results for cytotoxic effects of 13 chemotherapeutic agents on five human intrahepatic CCA cell lines are shown in Table 2. Among these cell lines, KKU-M055 showed the highest sensitivity to all of the chemotherapeutic drugs investigated with the IC50 values <5 μmol/L (except for 5-FU). In addition, KKU-100 appeared to be the most resistant cell line to 5-FU (with the IC50 value >1000 μmol/L) and to taxane compounds (with IC50 values of 40 μmol/L). All cell lines were sensitive to anthracycline compounds, doxorubicin and pirarubicin with IC50 values ranging from 0.04-2.3 μmol/L. In the case of platinum derivatives, KKU-M055 was highly sensitive to cisplatin, carboplatin and oxaliplatin (IC50 values <0.3 μmol/L) whereas KKU-M156 appeared to be resistant to cisplatin and carboplatin (IC50 values >200 μmol/L). With respect to vinca alkaloids, KKU-M055, KKU-M156 and KKU-OCA17 were sensitive to both vincristine and vinorabine (IC50 values <2 μmol/L) whereas KKU-M214 was appeared to be the least sensitive cell line (IC50 values ranging from 85 to 164 μmol/L). Most of the cell lines except for KKU-M214 were apparently sensitive to vinorabine, a new vinca alkaloid. In contrast to KKU-M055, the other four cell lines were apparently resistant to etoposide and mitomycin C. With regards to irenotican, most of the cell lines were moderately sensitive to this agent (IC50 values ranging from 3 to 43 μmol/L).
Table 2.
IC50 values of chemotherapeutic agents on CCA cell lines.
| Drug |
IC50 (mmol/L) |
||||
|
Poorly differentiated |
Moderately differentiated |
Well differentiated |
|||
| KKU-100 | KKU-M055 | KKU-M156 | KKU-M214 | KKU-OCA17 | |
| Anthracyclins | |||||
| Doxorubicin | 2.3±0.8b | 0.04±0.02 | 1.8±1.0b | 0.25±0.05 | 0.84±0.83 |
| Pirarubicin | 0.27±0.22a | 0.01±0.01 | 0.35±0.06b | 0.17±0.03b | 0.13±0.05b |
| Platinum derivatives | |||||
| Cisplatin | 37±3b | 0.05±0.01 | 222±38b | 130±12b | 6.22±0.19b |
| Carboplatin | 13±3b | 0.26±0.01 | 229±36b | 107±4b | 10.4±2.7a |
| Oxaliplatin | 71.7±38.7a | 0.11±0.00 | 7.0±4.7 | 38.0±6.7b | 6.8±1.3b |
| Pyrimidine analog | |||||
| 5-Fluorouracil | 1 018±326d | 46±42c | 144±55d | 29.1±17.6b | 3.46±0.91 |
| Taxanes | |||||
| Paclitaxel | 39.0±6.8b | 0.0030±0.0001 | 10.9±5.8a | 2.62±0.75a | 12.5±1.9b |
| Docetaxel | 41.2±7.2b | 0.00002±0.00002 | 0.80±0.36a | 12.4±3.7a | 1.3±0.3b |
| Vinca-alkaloids | |||||
| Vincristine | 216.2±52.1d | 2.05±0.68c | 0.97±0.64 | 85±19d | 0.82±0.17 |
| Vinorabine | 2.1±0.2b | 0.13±0.01 | 0.23±0.01a | 164±120 | 0.64±0.17a |
| Others | |||||
| Etoposide | 416±131b | 0.04±0.01 | 274±217b | 54±26a | 126±88a |
| Irinotecan | 23±6a | 3.41±0.51 | 13.1±2.1b | 43±9b | 3.60±1.16 |
| Mitomycin C | 45±2b | 0.01±0.00 | 187±0b | 78±32a | 5.07±0.17b |
Data represents mean±SD of at least three experiments.
P<0.05,
P<0.01 vs KKU-M055;
P<0.05,
P<0.01 vs KKU-OCA17.
Expression of mRNAs for TS, DPD, GSTP1, MDR1 and MRPs in CCA cell lines
Expression of TS, DPD, GSTP1, MDR1 and MRPs in five CCA cell lines were investigated by semi-quantitative RT-PCR using specific primers. As shown in Figure 1, mRNA for TS, DPD, GSTP1, and MRP1-MRP3 were detected in all CCA cell lines. High levels of MDR1 expression were observed only in KKU-OCA17. All CCA cell lines expressed low levels of MRP2 as compared to MRP1 and MRP3. Strong correlations were found between MRP3 mRNA expression and the IC50 value of etoposide (r = 0.98, P<0.05), doxorubicin (r = 0.96, P<0.05) and pirarubicin (r = 0.86, P<0.05) (Figure 2). On the other hand, no significant correlations were observed between the levels of GSTP1, MRP1 and MRP2 expression and IC50 values of all chemotherapeutic drugs investigated. Neither the expression levels of TS nor DPD in the CCA cell lines were significantly correlated with IC50 values of 5-FU.
Figure 1.
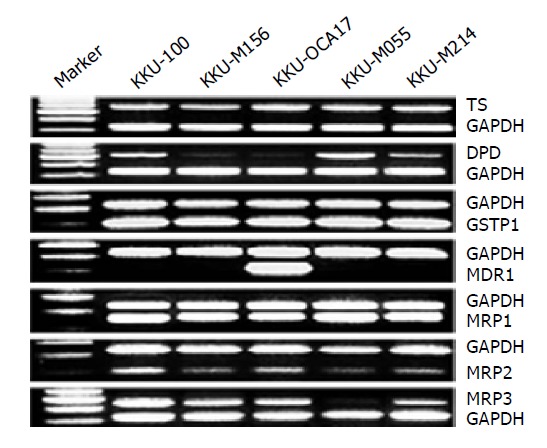
Expressions of TS, DPD, GSTP1, MDR1 and MRPs mRNA in five CCA cell lines determined by semi-quantitative RT-PCR analysis. Total RNA was extracted and used for RT-PCR. Each lane was loaded with 25 μL of PCR product. mRNA of the gene of interest was co-amplified with GAPDH mRNA as an internal control. Lane 1 is 100 bp DNA marker, lane 2-6 are PCR products from KKU-100, KKU-M156, KKU-OCA17, KKU-M055 and KKU-M214, respectively.
Figure 2.
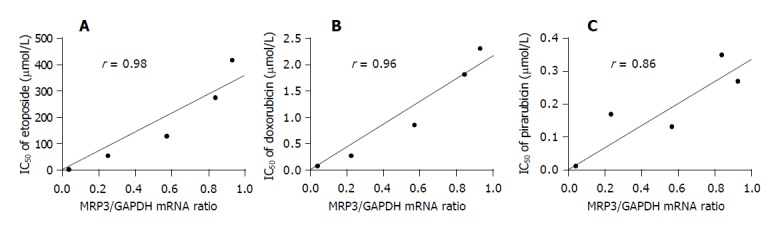
Relationships between the relative mRNA expression of MRP3 and the IC50 value of etoposide. (A) doxorubicin; (B) and pirarubicin; (C) in five CCA cell lines.
DISCUSSION
We have investigated the sensitivity of five CCA cell lines in response to a number of different classes of chemotherapeutic agents including the drugs that are commonly used in CCA patients (i.e. 5-FU, mitomycin C and doxorubicin)[7,35], as well as new chemotherapeutic drugs in order to provide a preclinical rationale for treatment of this cancer. Our results demonstrated that variations in the sensitivity to chemotherapeutic drugs were observed among these five intrahepatic CCA cell lines and sensitivity to chemotherapeutic drugs was not associated with the histological type of CCA. However, all CCA cell lines investigated in this study were apparently sensitive to new chemotherapeutic drugs including anthracyclins (pirarubicin and doxorubicin), vinca-alkaloid (vinorabine), taxanes (docetaxel, paclitaxel) and the campthothecin derivative (irinotecan). Although 5-FU is the most common drug used for treatment of CCA, poor response rates have been reported in CCA patients[7,36]. It should be noted that the IC50 values of 5-FU for CCA cell lines, particularly KKU-100 and KKU-M156, were much higher than those previously reported in colon carcinoma cell lines (i.e. HCC-48 and COLO20 with IC50 values of 8.6 and 16 μmol/L, respectively[28]) and in the cervical squamous carcinoma cell lines (i.e. SiHa and HeLa with IC50 values of 11.4 μmol/L[37] and 2.8 μmol/L[38], respectively).
The expression of genes that have been reported to be involved in chemotherapeutic drug resistance has also been investigated in the present study (Figure 2). TS, DPD, GSTP1, MRP1, MRP2 and MRP3 were expressed in all CCA cell lines albeit at different levels while MDR1 expression was detected only in one cell line. To determine whether these genes could be candidates for determining drug-resistance-phenotypes in CCA, linear regression analysis was performed and results demonstrated that the expression of MRP3 was significantly correlated with the resistance of these CCA cell lines to etoposide, doxorubicin and pirarubicin. Consistent with our finding, a strong association between MRP3 mRNA levels and response to doxorubicin has been reported in lung cancer[39].
In contrast to the previous report in a metastatic CCA cell line, SK-ChA-1[26], we did not find any association between the sensitivity to 5-FU and the levels of TS and DPD expression among the CCA cell lines investigated. The level of expression of a detoxifying enzyme, GSTP1 mRNA, was markedly elevated in all CCA cell lines and this may explain why CCA is quite resistant to chemotherapeutic drugs. The MDR1 gene was highly expressed only in KKU-OCA17 but not observed in other cell lines suggesting that MDR1 is not constitutively expressed in most of CCA cells.
The levels of MDR1 expression in these five CCA cell lines were not correlated with the IC50 value of any anticancer drug tested. These findings were inconsistent with those previously reported in 60 diverse cancer cell lines[24]. Unlike MDR1, all three MRPs investigated were expressed in these five CCA cell lines. MRP1 which presents in non-expressing MDR1 tumor cells[40] was also detected in our CCA cell lines that lacked MDR1 expression. The levels of MRP2 expression observed in these five CCA cell lines were markedly lower than the level of MRP1 expression. Consistent with those expressions found in proliferative cholangiocytes[41], MRP3 was also expressed in CCA cell lines. The level of MRP3 expression was significantly correlated with IC50 values of etoposide, doxorubicin and pirarubicin. These drugs have previously been reported to induce MDR1 and MRP1 expression in several tumor cell lines[38,42-47].
In conclusion, the data obtained from this in vitro drug screening will be useful for selection of chemotherapeutic treatment in CCA patients. The role of MRP3 in the mechanism of chemotherapeutic drug resistance in CCA patients needs to be further investigated.
ACKNOWLEDGMENTS
We would like to thank Professor Prapon Wilairat, Faculty of Sciences, Mahidol University, Thailand and Professor James Will, University of Wisconsin, USA, for their valuable comments and critical review of the manuscript. The support from the Liver Fluke and Cholangiocarcinoma Research Center, Faculty of Medicine, Khon Kaen University, Thailand is also appreciated.
Footnotes
Supported by the Research Grants From the Thailand Research Fund and Khon Kaen University, Thailand
Co-first-authors: Nisana Tepsiri and Liengchai Chaturat
Science Editor Guo SY Language Editor Elsevier HK
References
- 1.Parkin DM, Ohshima H, Srivatanakul P, Vatanasapt V. Cholangiocarcinoma: epidemiology, mechanisms of carcinogenesis and prevention. Cancer Epidemiol Biomarkers Prev. 1993;2:537–544. [PubMed] [Google Scholar]
- 2.Vatanasapt V, Martin N, Sriplung H, Chindavijak K, Sontipong S, Sriamporn H, Parkin DM, Ferlay J. Cancer incidence in Thailand, 1988-1991. Cancer Epidemiol Biomarkers Prev. 1995;4:475–483. [PubMed] [Google Scholar]
- 3.Watanapa P, Watanapa WB. Liver fluke-associated cholangiocarcinoma. Br J Surg. 2002;89:962–970. doi: 10.1046/j.1365-2168.2002.02143.x. [DOI] [PubMed] [Google Scholar]
- 4.Blendis L, Halpern Z. An increasing incidence of cholangiocarcinoma: why? Gastroenterology. 2004;127:1008–1009. doi: 10.1053/j.gastro.2004.07.035. [DOI] [PubMed] [Google Scholar]
- 5.Uttaravichien T, Bhudhisawasdi V, Pairojkul C, Pugkhem A. Intrahepatic cholangiocarcinoma in Thailand. J Hepatobiliary Pancreat Surg. 1999;6:128–135. doi: 10.1007/s005340050095. [DOI] [PubMed] [Google Scholar]
- 6.Ohtsuka M, Ito H, Kimura F, Shimizu H, Togawa A, Yoshidome H, Shimamura F, Shimizu Y, Miyazaki M. Extended hepatic resection and outcomes in intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2003;10:259–264. doi: 10.1007/s00534-002-0724-8. [DOI] [PubMed] [Google Scholar]
- 7.Patt YZ, Hassan MM, Lozano RD, Waugh KA, Hoque AM, Frome AI, Lahoti S, Ellis L, Vauthey JN, Curley SA, et al. Phase II trial of cisplatin, interferon alpha-2b, doxorubicin, and 5-fluorouracil for biliary tract cancer. Clin Cancer Res. 2001;7:3375–3380. [PubMed] [Google Scholar]
- 8.Martin R, Jarnagin W. Intrahepatic cholangiocarcinoma. Current management. Minerva Chir. 2003;58:469–478. [PubMed] [Google Scholar]
- 9.Lee MA, Woo IS, Kang JH, Hong YS, Lee KS. Epirubicin, cisplatin, and protracted infusion of 5-FU (ECF) in advanced intrahepatic cholangiocarcinoma. J Cancer Res Clin Oncol. 2004;130:346–350. doi: 10.1007/s00432-003-0534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olnes MJ, Erlich R. A review and update on cholangiocarcinoma. Oncology. 2004;66:167–179. doi: 10.1159/000077991. [DOI] [PubMed] [Google Scholar]
- 11.Yamagiwa Y, Marienfeld C, Meng F, Holcik M, Patel T. Translational regulation of x-linked inhibitor of apoptosis protein by interleukin-6: a novel mechanism of tumor cell survival. Cancer Res. 2004;64:1293–1298. doi: 10.1158/0008-5472.can-03-2517. [DOI] [PubMed] [Google Scholar]
- 12.Taniai M, Grambihler A, Higuchi H, Werneburg N, Bronk SF, Farrugia DJ, Kaufmann SH, Gores GJ. Mcl-1 mediates tumor necrosis factor-related apoptosis-inducing ligand resistance in human cholangiocarcinoma cells. Cancer Res. 2004;64:3517–3524. doi: 10.1158/0008-5472.CAN-03-2770. [DOI] [PubMed] [Google Scholar]
- 13.Nakajima T, Takayama T, Miyanishi K, Nobuoka A, Hayashi T, Abe T, Kato J, Sakon K, Naniwa Y, Tanabe H, et al. Reversal of multiple drug resistance in cholangiocarcinoma by the glutathione S-transferase-pi-specific inhibitor O1-hexadecyl-gamma-glutamyl-S-benzylcysteinyl-D-phenylglycine ethylester. J Pharmacol Exp Ther. 2003;306:861–869. doi: 10.1124/jpet.103.052696. [DOI] [PubMed] [Google Scholar]
- 14.Tannock IF. Tumor physiology and drug resistance. Cancer Metastasis Rev. 2001;20:123–132. doi: 10.1023/a:1013125027697. [DOI] [PubMed] [Google Scholar]
- 15.Krishan A, Arya P. Monitoring of cellular resistance to cancer chemotherapy. Hematol Oncol Clin North Am. 2002;16:357–372, vi. doi: 10.1016/s0889-8588(01)00016-8. [DOI] [PubMed] [Google Scholar]
- 16.Lønning PE. Study of suboptimum treatment response: lessons from breast cancer. Lancet Oncol. 2003;4:177–185. doi: 10.1016/s1470-2045(03)01022-2. [DOI] [PubMed] [Google Scholar]
- 17.Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer. 2002;2:48–58. doi: 10.1038/nrc706. [DOI] [PubMed] [Google Scholar]
- 18.Tew KD. Glutathione-associated enzymes in anticancer drug resistance. Cancer Res. 1994;54:4313–4320. [PubMed] [Google Scholar]
- 19.Nita ME, Tominaga O, Nagawa H, Tsuruo T, Muto T. Dihydropyrimidine dehydrogenase but not thymidylate synthase expression is associated with resistance to 5-fluorouracil in colorectal cancer. Hepatogastroenterology. 1998;45:2117–2122. [PubMed] [Google Scholar]
- 20.Stavrovskaya AA. Cellular mechanisms of multidrug resistance of tumor cells. Biochemistry (Mosc) 2000;65:95–106. [PubMed] [Google Scholar]
- 21.Ambudkar SV, Kimchi-Sarfaty C, Sauna ZE, Gottesman MM. P-glycoprotein: from genomics to mechanism. Oncogene. 2003;22:7468–7485. doi: 10.1038/sj.onc.1206948. [DOI] [PubMed] [Google Scholar]
- 22.Larkin A, O'Driscoll L, Kennedy S, Purcell R, Moran E, Crown J, Parkinson M, Clynes M. Investigation of MRP-1 protein and MDR-1 P-glycoprotein expression in invasive breast cancer: a prognostic study. Int J Cancer. 2004;112:286–294. doi: 10.1002/ijc.20369. [DOI] [PubMed] [Google Scholar]
- 23.Nies AT, König J, Pfannschmidt M, Klar E, Hofmann WJ, Keppler D. Expression of the multidrug resistance proteins MRP2 and MRP3 in human hepatocellular carcinoma. Int J Cancer. 2001;94:492–499. doi: 10.1002/ijc.1498. [DOI] [PubMed] [Google Scholar]
- 24.Szakács G, Annereau JP, Lababidi S, Shankavaram U, Arciello A, Bussey KJ, Reinhold W, Guo Y, Kruh GD, Reimers M, et al. Predicting drug sensitivity and resistance: profiling ABC transporter genes in cancer cells. Cancer Cell. 2004;6:129–137. doi: 10.1016/j.ccr.2004.06.026. [DOI] [PubMed] [Google Scholar]
- 25.Young LC, Campling BG, Cole SP, Deeley RG, Gerlach JH. Multidrug resistance proteins MRP3, MRP1, and MRP2 in lung cancer: correlation of protein levels with drug response and messenger RNA levels. Clin Cancer Res. 2001;7:1798–1804. [PubMed] [Google Scholar]
- 26.Habara K, Ajiki T, Kamigaki T, Nakamura T, Kuroda Y. High expression of thymidylate synthase leads to resistance to 5-fluorouracil in biliary tract carcinoma in vitro. Jpn J Cancer Res. 2001;92:1127–1132. doi: 10.1111/j.1349-7006.2001.tb01068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kogure T, Ueno Y, Iwasaki T, Shimosegawa T. The efficacy of the combination therapy of 5-fluorouracil, cisplatin and leucovorin for hepatocellular carcinoma and its predictable factors. Cancer Chemother Pharmacol. 2004;53:296–304. doi: 10.1007/s00280-003-0725-6. [DOI] [PubMed] [Google Scholar]
- 28.Nishiyama M, Yamamoto W, Park JS, Okamoto R, Hanaoka H, Takano H, Saito N, Matsukawa M, Shirasaka T, Kurihara M. Low-dose cisplatin and 5-fluorouracil in combination can repress increased gene expression of cellular resistance determinants to themselves. Clin Cancer Res. 1999;5:2620–2628. [PubMed] [Google Scholar]
- 29.Salonga D, Danenberg KD, Johnson M, Metzger R, Groshen S, Tsao-Wei DD, Lenz HJ, Leichman CG, Leichman L, Diasio RB, et al. Colorectal tumors responding to 5-fluorouracil have low gene expression levels of dihydropyrimidine dehydrogenase, thymidylate synthase, and thymidine phosphorylase. Clin Cancer Res. 2000;6:1322–1327. [PubMed] [Google Scholar]
- 30.Shirota Y, Ichikawa W, Uetake H, Yamada H, Nihei Z, Sugihara K. Intratumoral dihydropyrimidine dehydrogenase messenger RNA level reflects tumor progression in human colorectal cancer. Ann Surg Oncol. 2002;9:599–603. doi: 10.1007/BF02573898. [DOI] [PubMed] [Google Scholar]
- 31.Cullen KJ, Newkirk KA, Schumaker LM, Aldosari N, Rone JD, Haddad BR. Glutathione S-transferase pi amplification is associated with cisplatin resistance in head and neck squamous cell carcinoma cell lines and primary tumors. Cancer Res. 2003;63:8097–8102. [PubMed] [Google Scholar]
- 32.Cory AH, Owen TC, Barltrop JA, Cory JG. Use of an aqueous soluble tetrazolium/formazan assay for cell growth assays in culture. Cancer Commun. 1991;3:207–212. doi: 10.3727/095535491820873191. [DOI] [PubMed] [Google Scholar]
- 33.Mizutani Y, Nakanishi H, Yoshida O, Fukushima M, Bonavida B, Miki T. Potentiation of the sensitivity of renal cell carcinoma cells to TRAIL-mediated apoptosis by subtoxic concentrations of 5-fluorouracil. Eur J Cancer. 2002;38:167–176. doi: 10.1016/s0959-8049(01)00339-2. [DOI] [PubMed] [Google Scholar]
- 34.Li J, Xu LZ, He KL, Guo WJ, Zheng YH, Xia P, Chen Y. Reversal effects of nomegestrol acetate on multidrug resistance in adriamycin-resistant MCF7 breast cancer cell line. Breast Cancer Res. 2001;3:253–263. doi: 10.1186/bcr303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen JS, Lin YC, Jan YY, Liau CT. Mitomycin C with weekly 24-h infusion of high-dose 5-fluorouracil and leucovorin in patients with biliary tract and periampullar carcinomas. Anticancer Drugs. 2001;12:339–343. doi: 10.1097/00001813-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Hasuike Y, Motoori M, Hattori T, Fujita J, Mishima H, Sawamura T, Nishishou I, Kikkawa N, Sai H, Hosoki T, et al. A case report: successful resection of advanced intrahepatic cholangiocarcinoma responding to preoperative hepatic artery infusion of 5-FU. Gan To Kagaku Ryoho. 1999;26:1909–1912. [PubMed] [Google Scholar]
- 37.Laochariyakul P, Ponglikitmongkol M, Mankhetkorn S. Functional study of intracellular P-gp- and MRP1-mediated pumping of free cytosolic pirarubicin into acidic organelles in intrinsic resistant SiHa cells. Can J Physiol Pharmacol. 2003;81:790–799. doi: 10.1139/y03-061. [DOI] [PubMed] [Google Scholar]
- 38.Iida N, Takara K, Ohmoto N, Nakamura T, Kimura T, Wada A, Hirai M, Sakaeda T, Okumura K. Reversal effects of antifungal drugs on multidrug resistance in MDR1-overexpressing HeLa cells. Biol Pharm Bull. 2001;24:1032–1036. doi: 10.1248/bpb.24.1032. [DOI] [PubMed] [Google Scholar]
- 39.Young LC, Campling BG, Voskoglou-Nomikos T, Cole SP, Deeley RG, Gerlach JH. Expression of multidrug resistance protein-related genes in lung cancer: correlation with drug response. Clin Cancer Res. 1999;5:673–680. [PubMed] [Google Scholar]
- 40.Loe DW, Deeley RG, Cole SP. Biology of the multidrug resistance-associated protein, MRP. Eur J Cancer. 1996;32A:945–957. doi: 10.1016/0959-8049(96)00046-9. [DOI] [PubMed] [Google Scholar]
- 41.Scheffer GL, Kool M, de Haas M, de Vree JM, Pijnenborg AC, Bosman DK, Elferink RP, van der Valk P, Borst P, Scheper RJ. Tissue distribution and induction of human multidrug resistant protein 3. Lab Invest. 2002;82:193–201. doi: 10.1038/labinvest.3780411. [DOI] [PubMed] [Google Scholar]
- 42.Uchiyama-Kokubu N, Watanabe T. Establishment and characterization of adriamycin-resistant human colorectal adenocarcinoma HCT-15 cell lines with multidrug resistance. Anticancer Drugs. 2001;12:769–779. doi: 10.1097/00001813-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Nagata J, Kijima H, Hatanaka H, Asai S, Miyachi H, Takagi A, Miwa T, Mine T, Yamazaki H, Nakamura M, et al. Reversal of cisplatin and multidrug resistance by ribozyme-mediated glutathione suppression. Biochem Biophys Res Commun. 2001;286:406–413. doi: 10.1006/bbrc.2001.5399. [DOI] [PubMed] [Google Scholar]
- 44.Kubota T, Furukawa T, Tanino H, Suto A, Otan Y, Watanabe M, Ikeda T, Kitajima M. Resistant mechanisms of anthracyclines--pirarubicin might partly break through the P-glycoprotein-mediated drug-resistance of human breast cancer tissues. Breast Cancer. 2001;8:333–338. doi: 10.1007/BF02967534. [DOI] [PubMed] [Google Scholar]
- 45.Marbeuf-Gueye C, Salerno M, Quidu P, Garnier-Suillerot A. Inhibition of the P-glycoprotein- and multidrug resistance protein-mediated efflux of anthracyclines and calceinacetoxymethyl ester by PAK-104P. Eur J Pharmacol. 2000;391:207–216. doi: 10.1016/s0014-2999(00)00047-9. [DOI] [PubMed] [Google Scholar]
- 46.Lorico A, Rappa G, Finch RA, Yang D, Flavell RA, Sartorelli AC. Disruption of the murine MRP (multidrug resistance protein) gene leads to increased sensitivity to etoposide (VP-16) and increased levels of glutathione. Cancer Res. 1997;57:5238–5242. [PubMed] [Google Scholar]
- 47.Harvie RM, Davey MW, Davey RA. Increased MRP expression is associated with resistance to radiation, anthracyclines and etoposide in cells treated with fractionated gamma-radiation. Int J Cancer. 1997;73:164–167. doi: 10.1002/(sici)1097-0215(19970926)73:1<164::aid-ijc25>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]


