Abstract
Medicine is continually evolving; the new technologies of diagnosis and treatment continue to improve the life expectancy and lead to new information concerning various pathologies. The autopsy is viewed more and more as an ultimate branch of medicine and used only in extreme cases or for forensic purposes. Nevertheless, many studies, including this one, prove the utility and indispensability of the autopsies, without which a complete and accurate diagnosis cannot be made. Finally, the autopsy followed by histopathological examination of the tissues remains the ultimate and most important step for the apprehension of the diseases and for further evolution of medicine. This study reveals the correspondence rate between the clinical and the postmortem diagnosis, as well as between macroscopic and histopathological diagnosis.
Keywords: autopsy, clinical diagnosis, correspondence rate, postmortem diagnosis
INTRODUCTION
The autopsy is recognized as a necessary part of medicine. Apart from establishing the final diagnosis, the autopsy relates the cause of death to the associated pathologies and explains the interaction between the two. There are two main types of autopsies: forensic and clinical. The first one is performed in case of suspicious, violent or unknown cause of death. The second is performed in the hospital, by the pathologist, based on the consent of the deceased's next of kin in order to find and better understand the causes of death.
The autopsy represents the examination of the body after its death in order to determine the cause and manner of death as well as to evaluate any disease or injury that may be present. The term "autopsy" derives from Greek "autopsia" meaning "to see for oneself". It is composed of two words, autos, meaning "self" and opsis - "eye" (1). The first autopsies date from 3000 BC, in Ancient Egypt. At that time they had rather a religious role than medical in the context of mummification. The autopsy's history continues in Ancient Greek and after, documents revealing this practice existing in France and Germany of the Middle Ages. Karl Rokitansky who implemented the bases of each organ examination regardless the preexisting pathology, is considered to be the father of modern autopsy. Also in the 19th century, Rudolph Virchow extended the pathology at a cellular level.
In the 20th century the rate of autopsies decreased significantly. The cause seems to be the newest diagnosis technologies and the clinician's lack of interest in determination of the postmortem diagnosis. In the United States the autopsy rate decreased from 17% in 1980 (2) to 11.5% in 1989 (3) reaching 8.3% in 2003. In Australia, the rate decreased by 50% from 1992 to 2003 (4). We should note that this abatement is not local or transitional; this phenomenon is an appanage of modern medicine worldwide. Among the causes of this decrease we mention the clinician's lack of interest, the increasing confidence in the ante-mortem diagnosis, the more complex legislation regarding the human tissue procedures and, last but not least, an insufficient priority given to autopsies by the pathologists burned with increasing workloads of surgical resections, biopsies and cytology (5). Not to be neglected is the risk of the procedure, the risk of different infections and diseases that the pathologist is exposed to. Furthermore, the new molecular and imaging technologies which are less or totally non-invasive tend to replace the classic autopsy. However, many studies revealed a low correspondence rate between the diagnosis of these new types of autopsies and the classic ones. The classic autopsy with the external and internal examination of each organ, followed by the tissue sampling examination continues to represent the most complete method for a final diagnosis.
Although medicine improved to a great extent, and ante-mortem diagnosis is much more accurate and thorough, there still are significant discrepancies between clinical and post-mortem diagnosis. In this respect, the agreement may vary between 18% up to 45% in the last years. This agreement depends on a great deal on the type of hospital and also on the period of hospitalization of the patient.
The purpose of this paper is to find the agreement rate between the clinical and post-mortem diagnoses, as well as the existence of the associated pathologies which could influence the cause of death and the clinician's misdiagnosis. ❑
MATERIAL AND METHODS
The study herein included 112 autopsies performed over a 5 year period, between July 2009 and July 2013 in the Department of Pathology at the Emergency University Hospital of Bucharest. The data was collected from the special registers of the same department and entered in its own database. The collection and process of the data was made through Microsoft Office Excel 2007. We recorded demographic data (age, gender, residence), clinical data (department and the diagnosis from the medical record) and pathological findings (the diagnosis after macroscopic and histopathological examination of the tissue). All the diagnoses were categorized depending on the affected system. The correspondence rate between clinical and post-mortem diagnoses was also classified into three categories: total agreement, representing a correspondence between the majority of the diagnoses, partial agreement, when maximum two diagnoses were correspondent, and total disagreement when no clinical diagnosis matched the post-mortem one. The same classification was applied for the correspondence between macroscopical and microscopical findings. The autopsies were performed in the morgue of the Emergency University Hospital after the consent of the deceased's next of kin. ❑
RESULTS
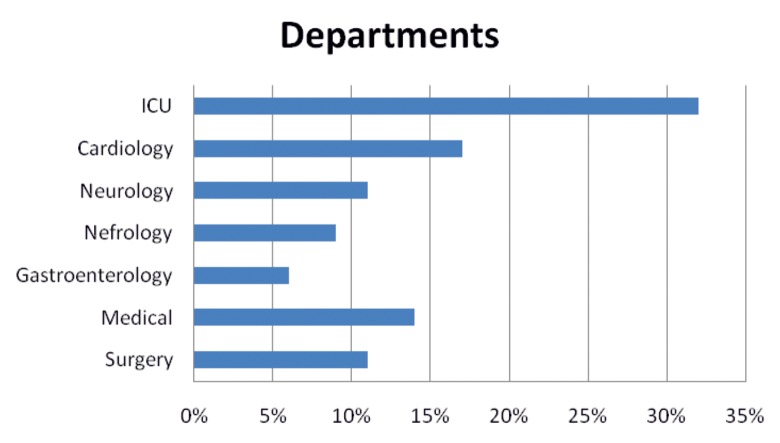
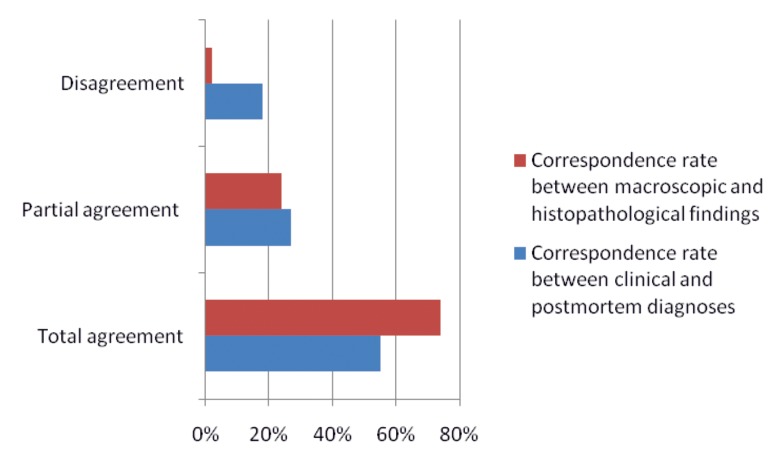
Out of the 112 patients, 48.21% were women and 51.79% men; the majority was included in the 7th (25%) and 8th (24.11%) decade of life. The 6th and 9th decades were found with a frequency of 18.75% and 16.07%, followed by the 4th and 5th decades with a percentage of 5.36% and 7.14% (Figure 1). Most of the patients were from urban areas (83.93%), only 16.07% from rural areas. Most of the patients died in the intensive care unit (32.14%), 16.96% in the Department of Cardiology and 14.29% came from the Medical Department. A percentage of 10.71 was registered from the Department of Neurology and from the Surgery Department, and 8.93% from the Department of Nephrology. Only 6.25% of the cases came from the Department of Gastroenterology (Figure 2).
Figure 1. The frequency of cases in age of patients.
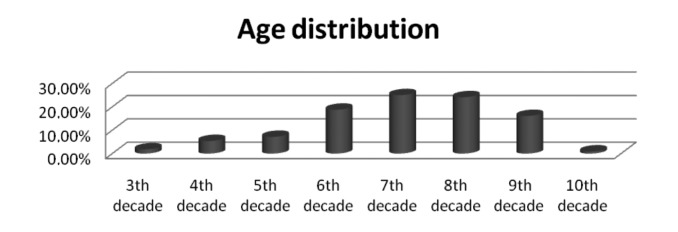
Figure 2. The frequency of the patients from clinical departments.
The majority of the deaths were due to infectious pathology (29.33%) and cardiac arrest (20.67%). Within the infectious pathology, in 54.54% of the cases the clinical diagnosis corresponded entirely with the macroscopical diagnosis; in 27.27 % of the cases there was a partial correspondence and in 18.18% of the cases there was total disagreement. As regards the cardiac pathology, only 41.9% of the cases had a correct and complete diagnosis, in 38.7% of the cases there was partial correspondence and in 19.35% of the cases there was total disagreement. At the same time, 11.33% of the deaths were due to gastrointestinal hemorrhage which led to hemorrhage failure, 10% of the patients died from pulmonary embolism and the same percentage from strokes. As regards the neurologic pathology, we emphasize that none of the cases were misdiagnosed; from an overall of 15 deaths only in 3 cases a partial correspondence was found. As for pulmonary embolism, 38.46 % of the cases came with a totally different diagnosis and in 46.15% of cases the clinical diagnosis corresponded with the post-mortem diagnosis.
Only 6% of the patients suffered from a neoplasia and 6.67 % died from mesenteric ischemia (Table 1). 33 patients presented with more pathologies, therefore the cause of death could not be accurate.
Table 1.
The main causes of deaths
| Causes of deaths | |
|---|---|
| Infectious Pathology | 29.33% |
| Cardiac Arrest | 20.67% |
| Gastrointestinal hemorrhage | 11.33% |
| Pulmonary Embolism | 10% |
| Strokes | 10% |
| Neoplasia | 6% |
| Mesenteric Ischemia | 6.67% |
As regards the overall correspondence rate between the clinical and post-mortem diagnoses, in 55.36 % of the cases there was total agreement, 26.79 % were partially correlated and 17.86% of the cases presented with a different diagnoses. 74.11 % of the cases had a total agreement between the post-mortem macroscopical examination and histopathological findings, 24.11 % had a partial agreement and 1.79 % the histopathological findings showed a different diagnosis than the macroscopical one (Figure 3).
Figure 3. Correspondence rates between clinical and postmortem diagnoses and macroscopic and histopathological findings.
The majority of the cases presented with associated diseases, with or without a correspondence with the cause of death, mostly represented by the cardiovascular pathology (81.25%); only 24.1% of the cases had neurological pathologies in the past. On the other hand, 78.57% of the deceased appeared to had suffered from pulmonary pathologies as chronic stasis or pneumonia frequently associated with pleurisy. At the same time, 91% of patients suffered from different gastrointestinal affections like stasis and fat liver disease (68.75%) or hemorrhaged or atrophied gastritis (47.32%). 60.7% of all cases presented with various renal affections like nefroangiosclerosis, renal ischemia or different renal infections (Table 2).
Table 2.
Associated diseases found among deceased patients.
| Associated diseases | |
|---|---|
| Cardiovascular Pathology | 81.25% |
| Neurological Pathology | 24.1% |
| Pulmonary Pathology (chronic stasis, pneumonia frequently associated with pleurisy) | 78.57% |
| Gastrointestinal Pathology (stasis, fat liver disease, hemorrhaged or atrophied gastritis) | 91% |
| Renal Pathology (nefroangiosclerosis, renal ischemia or different renal infections) | 60.7% |
Most of the patient initially diagnosed with cardiac arrest, hemorrhage failure or multiple organ dysfunction syndrome proved to have pulmonary embolism, various infections, especially pneumonia with different agents or respiratory insufficiency due to different degrees of chronic bronchitis or emphysema. Patients with pulmonary edema had a history of cardiac pathology, even cardiac arrest or renal pathologies, most of them associated with hypertension. In what concerns the deaths which occurred after hemorrhage failure due to different gastrointestinal pathologies, only a minority of the cases were clinically diagnosed with mesenteric ischemia or hemorrhagic gastritis; most of the patients were considered to have cardiac infarct or different arrhythmias, such as atrial fibrillation, flutter or bunch branch blocks. As regards the cases with pulmonary embolism, most of the clinical diagnoses varied between cardiac arrest, infectious causes or renal pathologies. ❑
DISCUSSION
The present study included 112 autopsies performed over a 5 year period proving once more the decrease of the number of such procedures in the hospitals. Most of the causes which led to this decreased rate of autopsies are generally applicable in the study herein, the decease rate of the hospital being significantly higher than the autopsy rate. The main cause of death found in the study herein appears to be the infectious pathology. Nevertheless, the majority of the patients presented severe chronic illnesses leading to susceptibility for this kind of affection. Furthermore, this association between different pathologies can significantly change the classic symptoms frequently leading to misdiagnoses. The majority of the patients were hospitalized more than 24 hours in intensive care units where they undergone different invasive procedures at a pulmonary level, hence resulting a high number of pulmonary and infectious pathologies.
The total correspondence rate which resulted within this study was of 55.36%, a percentage similar to those found within other studies (6-10). The partial correspondence rate meaning the agreement of one or two diagnoses was of 26.79% and the rate of disagreement was 17.86%. There is only one similar study performed in Romania (11). In that study the rate of agreement found was of 45% and the disagreement rate was 55%, percentages similar with the ones found in our study. Within other studies the numbers vary from 18-45%, depending on the type of the hospital or the period of hospitalization of the patient (12). Similar to our cases, patients with long periods of hospitalization, or those hospitalized in Medical Departments, Gastroenterology Department or Nephrology Department presented the lowest mortality rate and the most accurate and complex diagnosis. At the same time, the patients with advanced chronic pathologies who came with a complete diagnosis had the cause of death frequently misdiagnosed as a direct consequence of the interactions between different pathologies of various systems.
The correspondence rate between macroscopical and microscopical findings was 74.11%. Many studies raised the question of the necessity of microscopical examination of the tissue samples that had already been examined macroscopically (13-15). This problem was raised because of the high correspondence rate proved in many other papers. However, there is no general accord over this issue, many other studies proving otherwise; therefore, it remains a problem to be solved in the future. The high correspondence rate found within our study is partially due to a well-directed examination of the affected organ. At the same time, in 24.11% of the cases the histopathological findings brought more information than macroscopical examination and in 1.79% of the cases the histopathological findings rectified the macroscopical diagnosis.
The highest disagreement rate between clinical and post-mortem diagnoses as well as the highest misdiagnosed rate were found for pulmonary embolism. Furthermore, high percentage for disagreement rate was found within the infectious pathology and also for the cases diagnosed in the end with cardiac arrest. Many of this pathologies can be found with various rates of disagreement in the literature, depending on the pre-existing affections of the patient (16,17).
In what concerns the differences between diagnoses, we have to emphasize that the association of the various chronic diseases with either acute or fulminant evolution, corroborated with the overall respiratory and hemodynamic status of the patient makes the final diagnoses, as well as the pathophysiology of the diseases, heavy to clarify. In that matter, the differential diagnosis should be made with all the pathologies listed so far, including complications of diabetes mellitus, nephroangiosclerosis, fat liver disease, primary hypertension, obesity or gastrointestinal affections. ❑
CONCLUSION
The study herein emphasizes once more the importance of the autopsy, not only from medico-legal reasons but for a better understanding of the final diagnosis (18). As already seen, the correspondence rate between the clinical and post-mortem diagnoses is not very high, admitting future interpretations. The disagreement rate between the two diagnoses is important not only for the clinicians and for their future patients, but for the overall evolution of medicine and also for the relief of the deceased's relatives. Moreover the histopathological examination remains the main step for a complete and solid diagnosis for different pathologies found among patients (19). Like many other studies already ascertained, we qualify to bring out the necessity of this procedures. The autopsy, followed by microscopical examination of the tissue samplings remains an important step towards the improvement and development of medicine. It also remains the most certain way of finding an accurate and complete diagnosis for any known or suspected pathology.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Rothenberg K. In Ayn Embar-seddon, Allan D. Pass (eds.). Forensic Science. Salem Press; 2008. The Autopsy through History. pp. 100–100. [Google Scholar]
- 2.Centers for Disease Control, Current Trends Autopsy Frequency - United States, 1980-1985. Morbidity and Mortality Weekly Report. 1988;37:191–4. [PubMed] [Google Scholar]
- 3.Pollock DA, O'Neil JM, Parrish RG, et al. Temporal and geographic trends in the autopsy frequency of blunt and penetrating trauma deaths in the United States. JAMA. 1993;269:1525–31. [PubMed] [Google Scholar]
- 4.Burton E, Collins K – Autopsy Rate and Physician Attitudes Toward Autopsy, http://emedicine.medscape.com/article/1705948-overview#a1, Updated: Feb 11, 2014
- 5.Cohen M. The Hospital Autopsy, A Manual of fundamental Autopsy Practice. 3th Edition. Hodder Arnold; London: 2010. Fetal, perinatal and infant autopsies in Burton LJ, Rutty NG. pp. 184–202. [Google Scholar]
- 6.Nath P, Collins AK – Medicolegal Issues and the autopsy, http://emedicine.medscape.com/article/1975045-overview#a30, Updated: Jul 25, 2013
- 7.Souder E, Laws Terry T, Mrak ER. Autopsy 101. Geriatr Nurs. doi: 10.1016/j.gerinurse.2003.09.007. http://www.medscape.com/viewarticle/466795_7. [DOI] [PubMed] [Google Scholar]
- 8.Tavora F, Crowder DC, Sun CC, et al. Discrepancies Between Clinical and Autopsy Diagnoses: A Comparison of University, Community, and Private Autopsy Practices. Am J Clin Pathol. 2008;129:102–109. doi: 10.1309/9M7DFE62RTDKHH4D. http://www.medscape.com/viewarticle/568994_4. [DOI] [PubMed] [Google Scholar]
- 9.González-Franco MV, Ponce-Camacho MA, Barboza-Quintana O, et al. Discrepancies between clinical and autopsy diagnosis, A study of 331 autopsies performed over a 7 years period. Medicina Universitaria. 2012;14:54–54. [Google Scholar]
- 10.Maris C, Martin B, Creteur J, et al. Comparison of clinical and post-mortem findings in intensive care unit patients. Virchows Arch. 2007;450:329–333. doi: 10.1007/s00428-006-0364-5. [DOI] [PubMed] [Google Scholar]
- 11.Ioan B, Alexa T, Alexa ID. Do we still need the autopsy? Clinical diagnosis versus autopsy diagnosis. Rom J Leg Med. 2012;20:307–312. [Google Scholar]
- 12.Vougiouklakis T, Fragkouli K, Mitselou A, et al. A comparison of the provisional clinical diagnosis of death with autopsy findings. Rom J Leg Med. 2011;19:177–182. [Google Scholar]
- 13.Pastores MS, Dulu A, Voigt L, et al. BioMed Central Ltd; 2007. Premortem clinical diagnoses and postmortem autopsy findings: discrepancies in critically ill cancer patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roulson J, Benbow EW, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology;a meta-analysis and review, Histopathology. 2005;47:551–559. doi: 10.1111/j.1365-2559.2005.02243.x. [DOI] [PubMed] [Google Scholar]
- 15.Sington JD, Cottrell BJ. Analysis of the sensitivity of death certificates in 440 hospital deaths: a comparison with necropsy findings. J Clin Pathol. 2002;55:499–502. doi: 10.1136/jcp.55.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grade MHC, Zucoloto S, Kajiwara JK, et al. Trends of accuracy of clinical diagnoses of the basic cause of death in a university hospital. J Clin Pathol. 2004;57:369–373. doi: 10.1136/jcp.2003.013235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perkins DG, McAuley FD, Davies S, et al. Discrepancies between clinical and postmortem diagnoses in clinically ill patients: an observational study, Critical Care. 2003;7:R129–R132. doi: 10.1186/cc2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zaitoun AM, Fernandez C. The value of histological examination in the audit of hospital autopsies: a quantitative approach. Pathology. 1998;30:100–4. doi: 10.1080/00313029800169036. [DOI] [PubMed] [Google Scholar]
- 19.Pakis I, Polat O, Yayci N, et al. Comparison of the clinical diagnosis and subsequent autopsy findings in medical malpractice. Am J Forensic Med Pathol. 2010;31:218–21. doi: 10.1097/PAF.0b013e3181e040d4. [DOI] [PubMed] [Google Scholar]