Abstract
The peripheral nervous system refers to parts of the nervous system outside the brain and spinal cord. Systemic autoimmune diseases can affect both the central and peripheral nervous systems in a myriad of ways and through a heterogeneous number of mechanisms leading to many different clinical manifestations. As a result, neurological complications of these disorders can result in significant morbidity and mortality. The most common complication of peripheral nervous system (PNS) involvement is peripheral neuropathy, with symptoms of numbness, sensory paresthesias, weakness, or gait imbalance. The neuropathy may be multifocal and asymmetric or, less frequently, distal and symmetric.
Keywords: systemic autoimmune diseases, peripheral nervous system, neurological complications
BACKGROUND
The term peripheral nerve refers to the part of a spinal nerve distal to the root and plexus. Peripheral neuropathy is damage or disease affecting nerves (1-3). Neuropathy affecting just one nerve is called "mononeuropathy" and neuropathy involving multiple nerves in roughly the same areas on both sides of the body is called "symmetrical polyneuropathy" or simply "polyneuropathy" (4-5). When two or more (typically just a few, but sometimes many) separate nerves in disparate areas of the body are affected it is called "mononeuritis multiplex," "multifocal mononeuropathy" or "multiple mononeuropathy." Neuropathies may complicate many different systemic autoimmune diseases (6). There are a number of causes of systemic vasculitis that can affect peripheral nerves, and many times the vasculitis may be isolated to the peripheral nerves. Mononeuritis multiplex is caused by, or associated with vasculitides: polyarteritis nodosa, Wegener's granulomatosis, and Churg-Strauss syndrome; immune-mediated diseases like rheumatoid arthritis, systemic lupus erythematosus (SLE); sarcoidosis; cryoglobulinemia. Individuals who are affected may manifest with mononeuropathy, multiple mononeuropathies, and overlapping mononeuropathies, or even as a generalized symetric sensorimotor polyneuropathy (7). Symptoms often start gradually, and then get worse. It is important to take a detailed medical history for disorders that may be associated with vasculitis. Peripheral nervous system disorders are often suspected based on clinical findings (e.g., stocking-glove distribution, hyporeflexia, distal muscle weakness and wasting, localization to a peripheral nerve distribution) (8).
Systemic lupus erythematosus
The incidence of peripheral neuropathy in patients with systemic lupus erythematosus (SLE) varies according to the criteria used for its diagnosis. By nerve conduction parameters 25 to 50% of the patients appear to have neuropathy, but with clinical diagnosis criteria a significantly lower number of patients are detected with it (9,10). The neuropathy, in the great majority of the cases, is a distal, symmetric, axonal type with mild clinical manifestations. Rare cases of a severe motor neuropathy, mononeuritis multiplex and inflammatory demyelinating neuropathy are described. Epineural vasculitis has been found though, inconsistently in nerve biopsy (11,12).
Vasculitic neuropathy
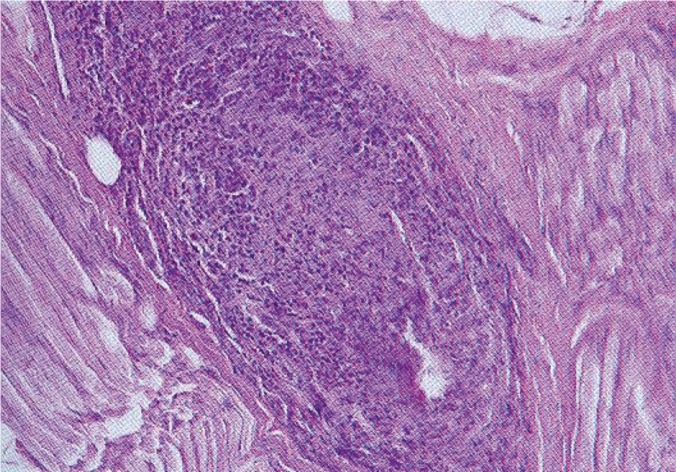
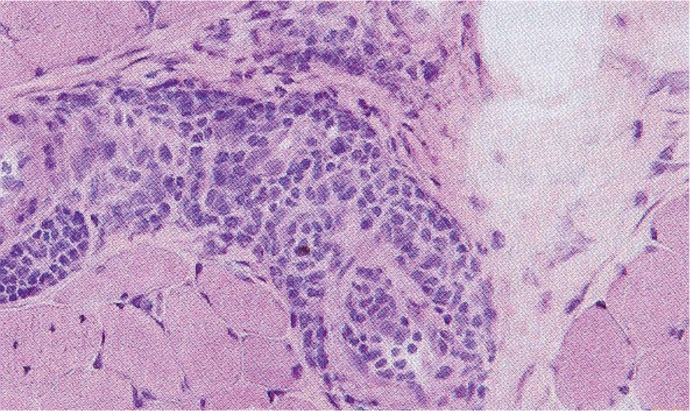
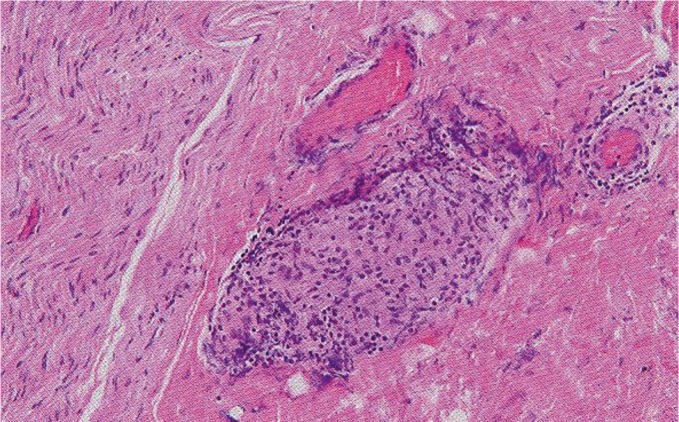
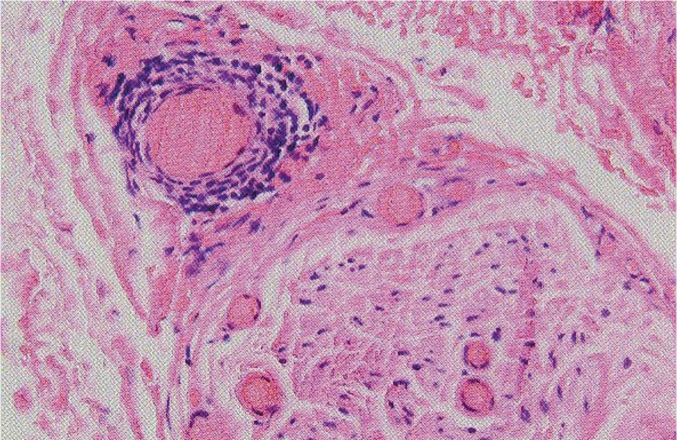
Vasculitis of PNS occurs either in the context of systemic vasculitis or isolated (non-systemic vasculitic neuropathy) (13-16). Systemic vasculitis is categorized as either primary, for which there is no known cause (Takayasu syndrome, giant cell arteritis, classical panarteritis nodosa, thrombangitis obliterans, Kawasaki disease, Churg-Strauss syndrome, Wegener granulomatosis, cryoglobulinemic vasculitis, Behçet's disease, microscopic polyangitis, Henoch-Schöenlein purpura), or secondary as a complication of an autoimmune connective tissue disorder (17-21). Peripheral nervous system vasculitis can present as a mononeuropathy or multiple mononeuropathies, overlapping mononeuropathies, or distal symmetric polyneuropathies. Peripheral neuropathy is an important, and often the presenting clinical feature of the vasculitis (22-26). Mononeuritis multiplex is the somewhat exotic term has been used to describe the classical and most frequent pattern of vasculitic neuropathy. It implies the sequential involvement of individual nerves or trunks usually in a distal to proximal pattern in an asymmetrical fashion (27-32). The neuropathy is often abrupt, preceded by pain in the field of the affected nerve, showing involvement of both motor and sensory modalities. Temporal arteritis and Takayasu arteritis are the two forms of giant cell arteritis, but peripheral neuropathy only occurs in the setting of temporal arteritis. Patients may develop multiple mononeuropathies, radiculopathies, plexopathies, or a generalized sensorimotor peripheral neuropathy (33-36) (Figure 1, 2).
Figure 1. Vasculitis. Superficial peroneal nerve biopsy demonstrates transmural inflammatory cell infiltrate with near obliteration of the lumen. Paraffin section stained with hematoxylin and eosin (H&E) ob. 20.
Figure 2. Vasculitis. The peroneus brevis muscle biopsy demonstrates vasculitis. Paraffin section stained with hematoxylin and eosin (H&E) ob. 20.
Behçet disease
In Behçet's disease studies evaluating peripheric nervous system is not usual. Behçet patients may have subclinical peripheral nerve involvement. Conventional electrophysiologic nerve conduction studies are recommended in routine examination to diagnose early neuropathy in Behçet patients without evident neurologic symptoms. The nerve dysfunction or peripheral neuropathy of BD is an axonal type of distal polyneuropathy and predominantly involves the lower extremities. (31-34)
Scleroderma
A distal symmetric, mainly sensory, polyneuropathy complicates 5-67% of cases. Cranial mononeuropathies can also develop, most commonly the trigeminal nerve, leading to numbness and dysesthesias in the face. Occasionally, seventh and ninth cranial neuropathies develop. Mutiple mononeuropathies have been described in a small percentage (1-2%) of patients with CREST syndrome. The electrophysiological and histological features of nerve biopsies are those of an axonal sensory greater than motor polyneuropathy (4,5,37,38).
Wegener's granulomatosis
Neurologic involvement has been reported in 30-55% of patients with Wegener's granulomatosis (WG). The most frequent complication is peripheral neuropathy, occurring in 16% of patients with WG. Cranial neuropathies have been reported in up to 11.7% of patients with WG, with the ophthalmic nerve most often affected. The other commonly affected cranial nerves were the abducens and facial nerves. The vasculitic neuropathy presents with mononeuritis often with cranial nerve involvement. Granulomatous lesions can also produce single or multiple cranial palsies (39-41).
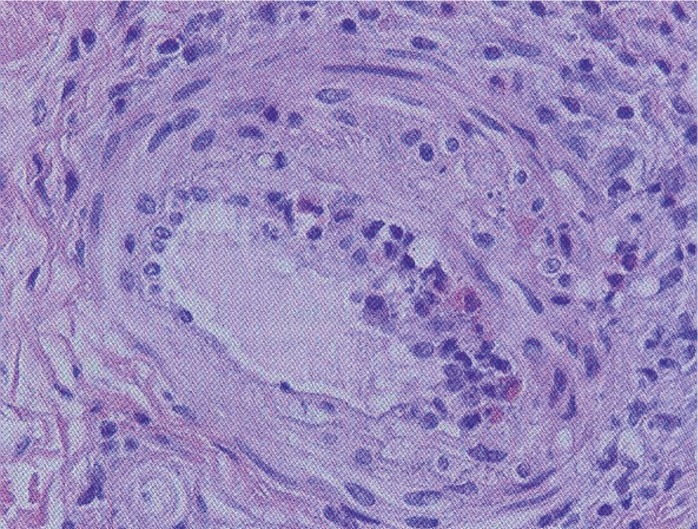
Churg-Strauss syndrome
Churg-Strauss syndrome is one of many forms of vasculitis. Peripheral neuropathy occurs very frequently in Churg-Strauss syndrome, due to epineurial necrotizing vasculitis with resulting axonal ischemia, and affects 50-80% of patients. Peripheral neuropathy mainly consists of mononeuritis multiplex (60-75% of patients with peripheral nerve involvement), but asymmetric or symmetric sensory or sensorimotor polyneuropathies or, more rarely, Guillain-Barré-like syndromes can also be observed (42-45) (Figure 3).
Figure 3. Churg-Strauss syndrome. Nerve biopsy demonstrates transmural infiltration of vessel wall that includes eosinophils and obliteration of the lumen. Paraffin section stained with H&E ob. 20.
Cryoglobulinemia
Elevated cryoglobulin levels may develop secondary to autoimmune disease. Neurologic manifestations predominantly affect the PNS and include painful sensorimotor polyneuropathy, pure sensory neuropathy, or mononeuritis multiplex. The most frequent distribution is distal sensory or sensorimotor polyneuropathy (46,47).
Vasculitic neuropathy associated with hepatitis
Hepatitis B and C have been associated with polyarteritis nodosa (PAN). Immune complexes to viral proteins are detected in these patients. A mononeuritis multiplex, or even symmetrical neuropathy in patients with abnormal liver tests should lead to the investigation of hepatitis B and C. Not infrequently the patients may also present with normal liver functions. Hepatitis can also be associated with a mixed cryoglobulinemia which can produce both a symmetrical as well as a mononeuritic polyneuropathy. Hepatitis C without cryoglobulinemia can also be independently associated with vasculitis. These patients have a PAN type of vasculitic neuropathy with systemic involvement. Variants with non-systemic vasculitis have been detected (48-51).
Polyarteritis nodosa
Peripheral neuropathy has been recognized as one of the most frequent clinical manifestation. Fifty to seventy percent of the diagnosed cases have neuropathy, which in many of the clinical series remains as the most frequent clinical manifestation. The neuropathy is asymmetric involving sensory and motor functions, affecting most frequently the lower extremities. Two percent of the patients showed cranial nerve involvement. Sensory complaints can vary from dysesthesia to pain. Motor deficits usually present abruptly. As in other vasculites with neuropathy the clinical evolution can mimic a distal symmetric neuropathy due to the summation of the peripheral nerve deficit (52,53).
Sjögren's syndrome
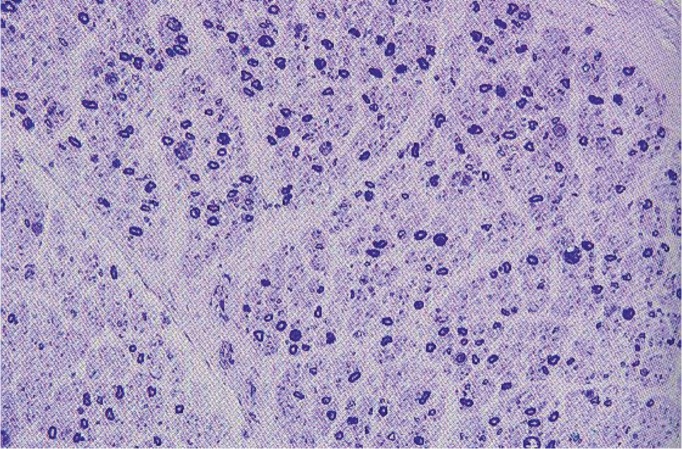
Peripheral nervous involvement in Sjogren's syndrome (SS) occurs in 5 to 10% of the patients. This is mostly manifested as a symmetrical distal, sensory neuropathy, sensory neuronopathy, autonomic neuropathy and trigeminal sensory neuropathy. Mononeuritis multiplex, chronic inflammatory demyelinating neuropathy and motor neuropathy are less common. The neuropathy may precede the onset of the disease and be the initial diagnostic clue (54-56). It is presumed to be related to autoimmune-mediated vascular damage is. Primary SS has been reported to affect PNS in up to 32% of the patients. PNS manifestations usually include a sensory or mixed sensorimotor polyneuropathy characterized by numbness, paraesthesias, and, rarely, pain. Distal weakness may occur and is usually mild. Carpal tunnel syndrome is well described with this disorder, and cranial neuropathies have been reported, especially of the trigeminal nerve (57-59) (Figure 4).
Figure 4. Sjögren syndrome. Sural nerve biopsy demonstrates a moderate reduction of large and sall myelinated nerve fibers and evidence of axonal degeneration. Plastic section stained with toluidine ob. 20.
Inflammatory bowel diseases
It seems that involvement of the PNS occurs mostly in ulcerative colitis (UC), whereas myopathy and myelopathy characterize Crohn's disease (CD). Peripheral neuropathy is the most common neurological complication associated with CD. Polyneuropathy can be associated with chronic inflammatory bowel diseases. Symptoms of neuropathy usually do not develop for roughly 10 years after the onset of CD. An inflammatory neuropathy may be seen in as many as 1.5% of CD patients. This is predominantly axonal (60,61).
Sarcoidosis
A number of studies reports on affection of the PNS in sarcoidosis (sarcoid neuropathy, sarcoid myopathy). Neurological manifestations of sarcoidosis are relatively rare but constitute a treatable cause of central and peripheral neurological manifestations. Vasculitic neuropathy in sarcoidosis presents as sensorimotor polyneuropathy, mononeuritis multiplex, painful mononeuropathies, or as CIDP. Palsy of the facial nerve (cranial nerve VII) is the single most frequent neurologic manifestation of sarcoidosis. It develops in 25-50% of all patients with neurosarcoidosis. Although usually unilateral, bilateral facial palsy also can occur, presenting with either simultaneous or sequential paralysis. More than half of all patients with facial palsy also have other forms of nervous system involvement (62-65) (Figure 5).
Figure 5. Sarcoidosis. Superficial peroneal nerve biopsy reveals a noncaseating granuloma in the epineurium and perivascular inflammation. Paraffin section stained with H&E ob. 20.
Rheumatoid arthritis
Peripheral nerve disorders in rheumatoid arthritis (RA) include entrapment neuropathies, multiple mononeuritis, sensorimotor neuropathy and mild sensory neuropathy. Neuropathies are usually related either to nerve compression by rheumatoid nodules, swollen synovium, aponeurosis or bony exostoses or vasculitis. Mononeuritis multiplex due to vasculitis in RA patients is a rare occurrence. More common are entrapment neuropathies and a chronic, many times asymptomatic, distal symmetric neuropathy. However, a minority of the RA patients can develop a serious, rapidly progressive vasculitic neuropathy similar to the one in PAN. This occurs in the context of the so-called rheumatoid vasculitis which presents with a systemic picture. Some RA patients will develop carpal tunnel syndrome or other mild forms of peripheral neuropathy (66,67) (Figure 6). ❑
Figure 6. Rheumatoid arthritis. Sural nerve biopsy reveals an epineurial vessel perivascular inflammation and scattered perineurial and endoneurial dilated capillaries with thickened walls. Paraffin section stained with H&E ob. 20.
CONCLUSION
It is always important to take a detailed medical history and examination to assess for an underlying systemic autoimmune diseases that may be associated with the neuropathy.
The connective tissue diseases, such as rheumatoid arthritis, Sjögren's syndrome, systemic lupus erythematosus, systemic sclerosis, and vasculitis, may cause various disorders of the peripheral nervous system.
Larger, prospective studies are needed to further assess the characteristics and etiology of the neuropathy.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Norman L. American Academy of Neurology Press Demos Medical; New York: 2007. Peripheral Neuropathy: When the Numbness, Weakness, and Pain Won't Stop. [Google Scholar]
- 2.Hughes RAC. Clinical review: Peripheral neuropathy. British Medical Journal. 2002;324:466–466. [Google Scholar]
- 3.Mendell JR, Sahenk Z. Clinical practice. Painful sensory neuropathy [review]. N Engl J Med. 2003;348:1243–55. doi: 10.1056/NEJMcp022282. [DOI] [PubMed] [Google Scholar]
- 4.Rosenbaum R. Neuromuscular complications of connective tissue diseases. Muscle Nerve. 2001;24:154–69. doi: 10.1002/1097-4598(200102)24:2<154::aid-mus20>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 5.Poncelet AN, Connolly MK. Peripheral neuropathy in scleroderma. Muscle Nerve. 2003;28(3):330–5. doi: 10.1002/mus.10439. [DOI] [PubMed] [Google Scholar]
- 6.Servioli L, Pérez C, Consani S, et al. Prevalence and characteristics of immuno-mediated neuropathies in a group of patients with autoimmune diseases. J Clin Neuromuscul Dis. 2007;9:285–90. doi: 10.1097/CND.0b013e318157614b. [DOI] [PubMed] [Google Scholar]
- 7.Shannon KM, Goetz CG. In: Neurology and General Medicine. Ed 3 Edited by Aminoff MJ. Churchill Livingstone; Philadelphia: 2001. Connective tissue diseases and the nervous system. pp. 459–81. [Google Scholar]
- 8.Rosenbaum R. Neuromuscular complications of connective tissue diseases. Muscle Nerve. 2001;24:154–69. doi: 10.1002/1097-4598(200102)24:2<154::aid-mus20>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 9.Ilniczky S, Kamondi A, Arányi Z, et al. Simultaneous central and peripheral nervous system involvement in systemic lupus erythematosus. Ideggyogy Sz. 2007;60:398–402. [PubMed] [Google Scholar]
- 10.Omdal R, Mellgren SI, Goransson L, et al. Small nerve fiber involvement in systemic lupus erythematosus: a controlled study. Arthritis Rheum. 2002;46:1228–32. doi: 10.1002/art.10303. [DOI] [PubMed] [Google Scholar]
- 11.Rafai MA, Fadel H, Boulaajaj FZ, et al. Peripheral neuropathy in systemic lupus erythematosus with epineural vasculitis and antiphospholipid antibodies. Rev Neurol (Paris) 2007;163:103–6. doi: 10.1016/s0035-3787(07)90363-x. [DOI] [PubMed] [Google Scholar]
- 12.Shoshtary J, Adib M. Peripheral neuropathy in systemic lupus erythematosus in Southern Iran. Electromyogr Clin Neurophysiol. 2005;45:145–8. [PubMed] [Google Scholar]
- 13.Seo JH, Ryan HF, Claussen GC, et al. Sensory neuropathy in vasculitis: a clinical, pathologic, and electrophysiologic study. Neurology. 2004;63:874–8. doi: 10.1212/01.wnl.0000137017.45065.3e. [DOI] [PubMed] [Google Scholar]
- 14.Younger D. Vasculitis and the nervous system. Curr Opin Neurol. 2004;17:317–36. doi: 10.1097/00019052-200406000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Said G, Lacroix C. Primary and secondary vasculitic neuropathy. J Neurol. 2005;252:633–41. doi: 10.1007/s00415-005-0833-9. [DOI] [PubMed] [Google Scholar]
- 16.Lacomis D, Zivkovic SA. Approach to vasculitic neuropathies. J Clin Neuromuscul Dis. 2007;9:265–76. doi: 10.1097/CND.0b013e31815202b3. [DOI] [PubMed] [Google Scholar]
- 17.Collins MP, Kissel JT. In Neurological Therapeutics: Principles and Practice. Edited by Noseworthy JH. Martin Dunitz; London: 2003. Vasculitis of the peripheral nervous system. pp. 2078–2110. [Google Scholar]
- 18.Griffin J. Vasculitic neuropathy. Rheum Clin. 2003;27:751–9. [Google Scholar]
- 19.Said G, Lacroix C. Primary and secondary vasculitic neuropathy. J Neurol. 2005;252:633–41. doi: 10.1007/s00415-005-0833-9. [DOI] [PubMed] [Google Scholar]
- 20.Burns TM, Schaublin GA, Dyck PJ. Vasculitic neuropathies. Neurol Clin. 2007;25:89–113. doi: 10.1016/j.ncl.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Gorson KC. Vasculitic neuropathies: an update. Neurologist. 2007;13:12–9. doi: 10.1097/01.nrl.0000252942.14928.17. [DOI] [PubMed] [Google Scholar]
- 22.Collins MP, Periquet MI. Non-systemic vasculitic neuropathy. Curr Opin Neurol. 2004;17:587–98. doi: 10.1097/00019052-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Kararizou E, Davaki D, Karandreas N, et al. Nonsystemic vasculitic neuropathy: A clinicopathological study of 22 cases. J Rheumatol. 2005;32:853–8. [PubMed] [Google Scholar]
- 24.Finsterer J. Systemic and non-systemic vasculitis affecting the peripheral nerves. Acta Neurol. Belg. 2009;109:100–13. [PubMed] [Google Scholar]
- 25.Pagnoux C, Guillevin L. Peripheral neuropathy in systemic vasculitides. Curr Opin Rheumatol. 2005;17:41–8. doi: 10.1097/01.bor.0000145518.91595.2f. [DOI] [PubMed] [Google Scholar]
- 26.Genta MS, Genta RM, Gabay C. Systemic rheumatoid vasculitis: a review. Semin Arthritis Rheum. 2006;36:88–98. doi: 10.1016/j.semarthrit.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Lacomis D, Zivkovic SA. Approach to vasculitic neuropathies. J Clin Neuromusc Dis. 2007;9:265–76. doi: 10.1097/CND.0b013e31815202b3. [DOI] [PubMed] [Google Scholar]
- 28.Jeruc J, Popovic M, Vizjak A, et al. Multiple mononeuropathy due to vasculitis associated with anticardiolipin antibodies: a case report. Folia Neuropathol. 2006;44:140–3. [PubMed] [Google Scholar]
- 29.Collins MP, Periquet MI, Mendell JR, et al. Nonsystemic vasculitic neuropathy: insights from a clinical cohort. Neurology. 2003;61:623–30. doi: 10.1212/01.wnl.0000082715.48844.3e. [DOI] [PubMed] [Google Scholar]
- 30.Heuss D, Probst-Cousin S, Kayser C, et al. Cell death in vasculitic neuropathy. Muscle Nerve. 2000;23:999–1004. doi: 10.1002/1097-4598(200007)23:7<999::aid-mus1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 31.Akbulut L, Gur G, Bodur H, et al. Peripheral neuropathy in Behçet disease: an electroneuro-physiological study. Clin Rheumatol. 2007;26:1240–4. doi: 10.1007/s10067-006-0466-0. [DOI] [PubMed] [Google Scholar]
- 32.Atasoy HT, Tunc TO, Unal AE, et al. Peripheral nervous system involvement in patients with Behçet disease. Neurologist. 2007;13:225–30. doi: 10.1097/NRL.0b013e31805778d1. [DOI] [PubMed] [Google Scholar]
- 33.Akbulut L, Gur G, Bodur H, et al. Peripheral neuropathy in Behçet disease: an electroneurophysiological study. Clin Rheumatol. 2007;26:1240–4. doi: 10.1007/s10067-006-0466-0. [DOI] [PubMed] [Google Scholar]
- 34.Burol A, Ulkatan S, Koçak M, et al. Peripheral neuropathy in Behçet's disease. J Dermatol. 2004;31:455–9. doi: 10.1111/j.1346-8138.2004.tb00531.x. [DOI] [PubMed] [Google Scholar]
- 35.Bulun A, Topaloglu R, Duzova A, et al. Ataxia and peripheral neuropathy: rare manifestations in Henoch-Schönlein purpura. Pediatr Nephrol. 2001;16:1139–41. doi: 10.1007/s004670100048. [DOI] [PubMed] [Google Scholar]
- 36.Mutsukura K, Tsuboi Y, Fujiki F, et al. Acute motor sensory axonal neuropathy associated with Henoch-Schönlein purpura. J Neurol Sci. 2007;263:169–73. doi: 10.1016/j.jns.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 37.Poncelet AN, Connolly MK. Peripheral neuropathy in scleroderma. Muscle Nerve. 2003;28:330–5. doi: 10.1002/mus.10439. [DOI] [PubMed] [Google Scholar]
- 38.Allanore Y, Zuber M, Kahan A. Brachial plexopathy associated with systemic sclerosis. Clin Rheumatol. 2002;21:401–2. doi: 10.1007/s100670200106. [DOI] [PubMed] [Google Scholar]
- 39.Pleasure D. Peripheral neuropathy as the first clinical manifestation of Wegener granulomatosis. Arch Neurol. 2001;58:1204–1204. doi: 10.1001/archneur.58.8.1204. [DOI] [PubMed] [Google Scholar]
- 40.Nagashima T, Maguchi S, Terayama Y, et al. P-ANCA-positive Wegener's granulomatosis presenting with hyperthrophic pachymeningitis and multiple cranial neuropathy: case report and review of literature. Neuropathology. 2000;20:23–30. doi: 10.1046/j.1440-1789.2000.00282.x. [DOI] [PubMed] [Google Scholar]
- 41.Cattaneo L, Chierici E, Pavone L, et al. Peripheral neuropathy in Wegener's granulomatosis, Churg-Strauss syndrome and microscopic polyangiitis. J Neurol Neurosurg Psychiatry. 2007;78:1119–23. doi: 10.1136/jnnp.2006.111013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wolf J, Bergner R, Mutallib S, et al. Neurologic complications of Churg-Strauss syndrome - a prospective monocentric study. Eur J Neurol. 2009;17:582–8. doi: 10.1111/j.1468-1331.2009.02902.x. [DOI] [PubMed] [Google Scholar]
- 43.Hattori N, Mori K, Misu K, et al. Mortality and morbidity in peripheral neuropathy associated Churg-Strauss syndrome and microscopic polyangiitis. J Rheumatol. 2002;29:1408–14. [PubMed] [Google Scholar]
- 44.Tyvaert L, Devos P, Deloizy M, et al. Peripheral and central neurological manifestations in a case of Churg Strauss syndrome. Rev Neurol (Paris) 2004;160:89–92. doi: 10.1016/s0035-3787(04)70853-x. [DOI] [PubMed] [Google Scholar]
- 45.Djukic M, Schmidt H, Mazurek C, et al. A patient with Churg-Strauss syndrome presenting as Guillain-Barré syndrome. Nervenarzt. 2008;79:457–61. doi: 10.1007/s00115-007-2377-y. [DOI] [PubMed] [Google Scholar]
- 46.Saadoun D, Bieche I, Authier FJ, et al. Role of matrix metalloproteinases, pro-inflammatory cytokines, and oxidative stress derived molecules in hepatitis C virus-associated mixed cryoglobulinemia vasculitis neuropathy. Arthritis Rheum. 2007;56:1315–24. doi: 10.1002/art.22456. [DOI] [PubMed] [Google Scholar]
- 47.Nemni R. Peripheral neuropathy in hepatitis C virus infection with and without cryoglobulinemia. J Neurol Neurosurg Psychiatry. 2003;74:1267–71. doi: 10.1136/jnnp.74.9.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nemni R, Sanvito L, Quattrini A, et al. Peripheral neuropathy in hepatitis C virus infection with and without cryoglobulinaemia. J Neurol Neurosurg Psychiatry. 2003;74:1267–71. doi: 10.1136/jnnp.74.9.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tada M, Naruse S, Arai A, et al. An autopsy case of systemic vasculitis associated with hepatitis C virus-related mixed cryoglobulinemia presenting severe peripheral neuropathy. Rinsho Shinkeigaku. 2004;44:686–90. [PubMed] [Google Scholar]
- 50.Vincent D, Gombert B, Vital A, et al. A case of mononeuropathy multiplex with type II cryoglobulinemia, necrotizing vasculitis and low grade B cell lymphoma. Clin Neuropathol. 2007;26:28–31. doi: 10.5414/npp26028. [DOI] [PubMed] [Google Scholar]
- 51.Takeshita S, Nakamura H, Kawakami A, et al. Hepatitis B-related polyarteritis nodosa presenting necrotizing vasculitis in the hepatobiliary system successfully treated with lamivudine, plasmapheresis and glucocorticoid. Intern Med. 2006;45:145–9. doi: 10.2169/internalmedicine.45.1460. [DOI] [PubMed] [Google Scholar]
- 52.Harada K, Hirayama K, Hori M, et al. Sensory ataxic dominant neuropathy associated with polyarteritis nodosa. Intern Med. 2000;39:847–851. doi: 10.2169/internalmedicine.39.847. [DOI] [PubMed] [Google Scholar]
- 53.Sugiura M, Koike H, Iijima M, et al. Clinicopathologic features of nonsystemic vasculitic neuropathy and microscopic polyangiitis-associated neuropathy: a comparative study. J Neurol Sci. 2006;241:31–7. doi: 10.1016/j.jns.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 54.Birnbaum J. Peripheral nervous system manifestations of Sjögren syndrome: clinical patterns, diagnostic paradigms, etiopathogenesis, and therapeutic strategies. Neurologist. 2010;16:287–97. doi: 10.1097/NRL.0b013e3181ebe59f. [DOI] [PubMed] [Google Scholar]
- 55.Mori K, Iijima M, Koike H, et al. The wide spectrum of clinical manifestations in Sjögren's syndrome associated neuropathy. Brain. 2005;128:2518–34. doi: 10.1093/brain/awh605. [DOI] [PubMed] [Google Scholar]
- 56.Gorson KC, Ropper AH. Positive salivary gland biopsy, Sjögren syndrome, and neuropathy: Clinical implications. Muscle Nerve. 2003;28:553–60. doi: 10.1002/mus.10470. [DOI] [PubMed] [Google Scholar]
- 57.Lopate G, Pestronk A, Al-Lozi M, et al. Peripheral neuropathy in an outpatient cohort of patients with Sjögren's syndrome. Muscle Nerve. 2006;33:672–6. doi: 10.1002/mus.20514. [DOI] [PubMed] [Google Scholar]
- 58.Mori K, Iijima M, Koike H, et al. The wide spectrum of clinical manifestations in Sjögren's syndrome-associated neuropathy. Brain. 2005;128:2518–34. doi: 10.1093/brain/awh605. [DOI] [PubMed] [Google Scholar]
- 59.Chai J, Herrmann DN, Stanton M, et al. Painful small-fiber neuropathy in Sjogren syndrome. Neurology. 2005;659:925–7. doi: 10.1212/01.wnl.0000176034.38198.f9. [DOI] [PubMed] [Google Scholar]
- 60.Moormann B, Herath H, Mann O, et al. Involvement of the peripheral nervous system in Crohn disease. Nervenarzt. 1999;70:1107–11. doi: 10.1007/s001150050547. [DOI] [PubMed] [Google Scholar]
- 61.Zois CD, Katsanos KH, Kosmidou M, et al. Neurologic manifestations in inflammatory bowel diseases: Current knowledge and novel insights. Journal of Crohn's and Colitis. 2010;4:115–24. doi: 10.1016/j.crohns.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 62.Allen RK, Sellars RE, Sandstrom PA. A prospective study of 32 patients with neurosarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2003;20:118–25. [PubMed] [Google Scholar]
- 63.Vital A, Lagueny A, Ferrer X, et al. Sarcoid neuropathy: clinico-pathological study of 4 new cases and review of the literature. Clin Neuropathol. 2008;27:96–105. doi: 10.5414/npp27096. [DOI] [PubMed] [Google Scholar]
- 64.Said G, Lacroix C, Plante-Bordeneuve V, et al. Nerve granulomas and vasculitis in sarcoid peripheral neuropathy: a clinicopathological study of 11 patients. Brain. 2002;125:264–75. doi: 10.1093/brain/awf027. [DOI] [PubMed] [Google Scholar]
- 65.Said G, Lacroix C, Plante-Bordeneuve V, et al. Nerve granulomas and vasculitis in sarcoid peripheral neuropathy: A clinicopathological study of 11 patients. Brain. 2002;125:264–75. doi: 10.1093/brain/awf027. [DOI] [PubMed] [Google Scholar]
- 66.Agarwal V, Singh R, Chauhan S, et al. A clinical, electrophysiological, and pathological study of neuropathy in rheumatoid arthritis. Clin Rheumatol. 2008;27:841–4. doi: 10.1007/s10067-007-0804-x. [DOI] [PubMed] [Google Scholar]
- 67.Muramatsu K, Tanaka H, Taguchi T. Peripheral neuropathies of the forearm and hand in rheumatoid arthritis: diagnosis and options for treatment. Rheumatol Int. 2008;28:951–7. doi: 10.1007/s00296-008-0630-8. [DOI] [PubMed] [Google Scholar]