Abstract
Background
Trauma centers (TC) have been shown to decrease mortality in adults, but this has not been demonstrated at a population-level in all children. We hypothesized that seriously injured children would have increased survival in a TC vs. non-trauma center (nTC), but there would be no increased benefit from pediatric-designated vs. adult TC care.
Methods
This was a retrospective study of the unmasked California Office of Statewide Health and Planning Department patient discharge database (1999–2011). International Classification of Disease, Ninth Revision (ICD-9) diagnostic codes indicating trauma were identified for children (0–18) and injury severity was calculated from ICD-9 codes using validated algorithms. To adjust for hospital case mix, we selected patients with ICD-9 codes that were capable of causing death, and which appeared at both TCs and nTCs. Instrumental variable analysis using differential distance between the child’s residence to a trauma center and to the nearest hospital was applied to further adjust for unobservable differences in TC and nTC populations. IV regression models analyzed the association between mortality and TC vs. nTC care, as well as for pediatric vs. adult TC designations, adjusting for demographic and clinical variables.
Results
Unadjusted mortality for the entire population of children with nontrivial trauma (n=445,236) was 1.2%. In the final study population (n=77,874), mortality was 5.3%; 3.8% in nTCs and 6.1% in TCs. IV regression analysis demonstrated a 0.79 percentage point (95% CI −0.80 to −0.30; p=.044) decrease in mortality for children cared for in TC vs. nTC. No decrease in mortality was demonstrated for children cared for in pediatric vs. adult TCs.
Conclusion
Our IV TC outcome models use improved injury severity and case mix adjustment to demonstrate decreased mortality for seriously injured California children treated in TCs. These results can be used to take evidence-based steps to decrease disparities in pediatric access to, and subsequent outcomes for, trauma care.
Level of Evidence
Level III Therapeutic/Care Management.
Keywords: Injury outcome, Pediatric trauma, Designated trauma centers, Trauma systems, Injury mortality, Instrumental variable analysis
Background
Trauma is a leading cause of morbidity and mortality in the United States and the number one cause of mortality in young people.1 Regionalized trauma systems have potential to improve the quality and outcomes of trauma care by organizing and coordinating all aspects of emergency care, and by assuring that seriously injured patients have access to the appropriate level of care. 2 Outcomes attributable to the trauma system as a whole are difficult to measure, as the trauma system includes: Emergency medical system (EMS) dispatch, initial assessment, stabilization and transport from the field to a hospital emergency department (ED); transfer to a higher level of care when required; definitive treatment in a trauma center (TC); as well as continuing services such as rehabilitation and preventative public health measures. However, one component of the trauma system, specialized trauma center care, has been demonstrated to decrease injury mortality in adults.3
The exact benefits of TC care for children of all ages, however, has not been definitively demonstrated at a population level. Children have different patterns of injury than adults as well as unique treatment, expertise and equipment requirements. All “adult” TCs (aTCs) are equipped to resuscitate and stabilize children with serious trauma, but pediatric trauma centers (pTC) exist to provide further subspecialty care. Ultimately, however, both aTCs and pTCs are non-uniformly concentrated in urban areas, and pTCs are few in number. Because of these factors, we believe that pediatric trauma care outcomes rely more on the success of the trauma system as a whole than do adult outcomes. However, there are also low absolute numbers of severe injuries and deaths in children compared with adults, making outcome measures based on mortality challenging. In addition, the multiple players involved in this system, and the lack of a uniform data source accounting for the different arenas of care, render the benefit of trauma center care difficult to demonstrate for the entire pediatric population.
Our objective was to utilize a population-based, statewide administrative data source to assess the treatment effect (decreased mortality) for children cared for in designated TCs compared to non-trauma centers (nTCs); and to secondarily assess the treatment effect of subspecialty pTC care compared to aTC care. We hypothesized that seriously injured children would have decreased mortality in a TC vs. nTC but that this decreased mortality would not be apparent in pTCs compared to aTCs.
Methods
Study Design and Data
We conducted a retrospective cohort study of the unmasked California Office of Statewide Health Planning and Development (OSHPD) patient discharge data (PDD) from 1999–2011. All California licensed hospitals are required to submit discharge records biannually to OSHPD with demographic, diagnostic and financial variables for each patient.4 One primary diagnosis and up to 24 additional ICD-9 diagnostic codes are listed for each patient. Procedures performed, disposition (including length of stay and expected source of payment) are reported. The administrative panel on human subjects at our university, and the California Health Board approved this protocol.
Study Setting
California is a large and diverse state, home to 1/8 of the pediatric population of the US.5 It does not have a statewide trauma system; instead, approximately 20 local emergency medical services associations (LEMSAs) operate with guidance from the California EMS authority. TCs are “designated” by the LEMSAs which are able, but not required, to use the American College of Surgeons to verify the hospital’s qualifications as a TC. In 2008, California had 36 level I and II TCs, and 10 pTCs.6 Trauma centers are classified as aTC level I and II, III and IV and pediatric level I and II. Level III and IV TCs are generally smaller facilities that can provide advanced trauma support but cannot provide all the resources of a level I or II TC, so they must transfer seriously injured patients.
Study population
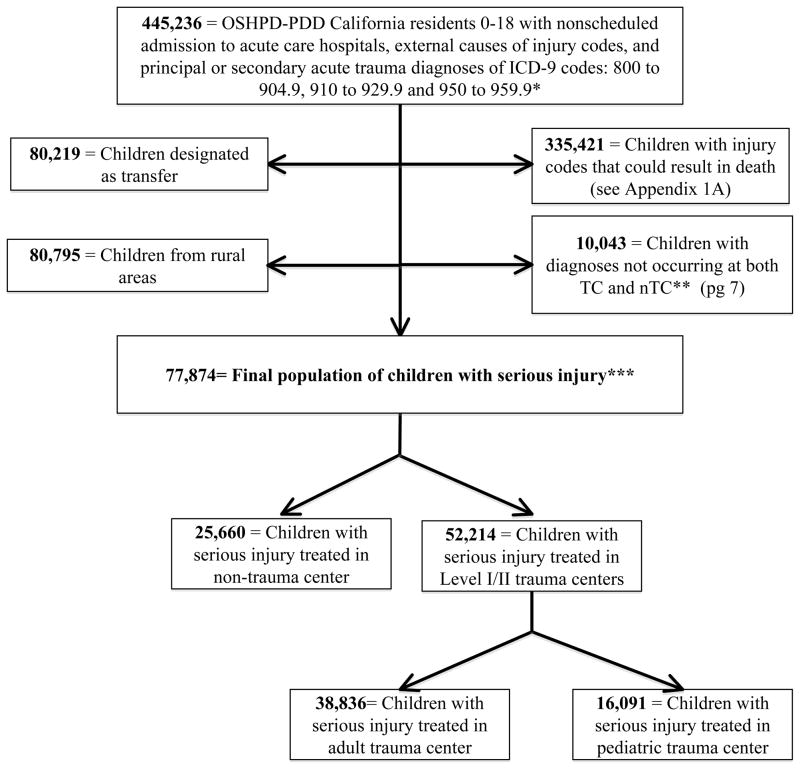
Using previously published methods, 7 we queried the OSHPD-PDD for California residents 0 through 18 years of age, with nonscheduled admission to California acute care hospitals, with acute trauma diagnoses in the principal or any of the secondary ICD-9 diagnosis codes (800 to 904.9, 910 to 929.9 and 950 to 959.9) during the study period. We excluded children with sole ICD-9 codes indicating minor injuries such as sprains and strains (840–848.9), open wounds (871.9–894.1), superficial abrasions (910.0–919.8), contusion with intact skin surface (920–924.9), foreign bodies (930–939), late effects of injury (905–909) and those with trauma ICD-9 codes associated with pregnancy and perinatal conditions. We also excluded children with the sole diagnosis of burns (940–949), because in California burns are cared for at regional burn centers, which can be separate from trauma centers. Finally, to ensure that patients were hospitalized for acute trauma, we excluded patients with no E-codes.8 Because these exclusions were not mutually exclusive, our preliminary study sample included 445,236 children with an overall mortality rate of 1.2%.
While rural areas stand to benefit the most from regionalization of trauma expertise and resources, the trauma response is most varied in these areas. We thus initially excluded patients who lived in rural areas and who lived >50 miles from a TC. 9 Similarly, although patients receiving appropriate transfer to a higher level of care can illustrate the degree of pediatric regionalization achieved, these patients experience variable care within variable time frames and thus were also excluded from our major analyses. (As part of our sensitivity analyses, we re-incorporated these patients into the study population with no major change in outcome. See Appendix 4 for further information.)
Because the majority of injuries in children do not result in death, we further refined our study population to include only conditions that carried a risk of death in order to best evaluate both centers with the outcome variable of mortality. We identified ICD-9 code groupings accepted in the literature as indicative of serious injury with an increased likelihood of fatality including: fractures (of the skull, neck and trunk) intracranial injury and spinal cord injuries (800–809,850–854, and 952); internal injury of the thorax, abdomen or pelvis (860–869); and injury of blood vessels (900–904).10 The emergency physician author (NEW), further identified and removed any injury codes which could be associated with, but not cause, death. If an injury’s level of association with death was unclear, the author consulted with trauma colleagues. (See Appendix 1 for more detail)
Greater overall acuity coupled with disproportionate representation of complicated injuries in a TC can confound comparisons of mortality between TC and nTC. Trauma designated hospitals have more experience coding injuries in an administrative database resulting in more refined or rare diagnoses coded uniquely in a TC. Thus we further restricted our population to include only diagnoses that occurred in both TC and nTC populations. Our final sample included 77,874 seriously injured children, who were all seen at either nTCs or Level I/II TCs.
Variables
Outcome variable
In-hospital mortality
Treatment variable
TC designation
Independent variables
Demographic variables included: sex, age, race/ethnicity, and insurance status. We derived zip-code level median household income categories for patient resident zip-code 11 which we then correlated with the 2004 federal poverty designation level of $18,850 for a family of 4.12 Distance from the patient residence to the hospital was calculated by the method of Phibbs and Luft13 as the shortest distance between the centroids of the patient’s residence and the hospital’s zip-codes.14
We included external cause of injury codes (E-codes), since injury outcome is associated with the injury mechanism and intent. We calculated injury severity from ICD-9 diagnostic codes using validated injury severity scoring systems (ICDPIC Stata v. 11, StataCorp, College Station, TX). 15–18 Although the Injury Severity Score (ISS) is the most commonly used scoring system, it is expert consensus based, and uses a non-linear, discontinuous scale. The Trauma Mortality Prediction Model (TMPM) is a newer mortality prediction model. It uses ICD-9 CM injury codes to generate empirically derived survival risk ratios and develops a measure of injury severity based on regression modeling. 19 We used TMPM as the primary injury severity scoring system for our primary analyses but performed sensitivity analyses with ISS (Appendix 3). Trauma centers were identified from the California EMSA website.6
Data analysis
Our analyses tested the association between mortality and TC designation. In our primary analyses, we compared outcomes from nTCs with level I and II TCs, regardless of pediatric designation. In our secondary analysis, we compared outcomes from adult level I and II TCs with pTCs. TCs classified as both adult and pediatric were identified as TCs in the primary analyses and as pTCs in the secondary analyses.
Regression analysis is a method classically used to estimate the relative contribution of different variables to an outcome of interest. In many cases, this method is sufficient to adjust for observable differences in patient populations. However, differences in patients may be un-observable and the effect of the treatment will be confounded. In the case of trauma, clinicians are well aware that patients cared for in TCs are different in many characteristics from those cared for in nTCs. These differences are not fully reflected by available variables including diagnoses or injury severity scores derived from administrative data.
Randomized control trials (RCT) are the ideal method to evaluate outcomes when unobservable variables are possible confounders. They insure that patients receiving a treatment are similar to those that are not. However in many cases, such as in the case of TC care, an RCT is not possible and in these cases an Instrumental Variable method can be utilized to achieve a “pseudorandomization” of observational data. The instrumental variable approach identifies a variable, the “instrumental variable,” which correlates with the treatment variable but does not have an effect on the outcome. The instrumental variable provides a way of randomly assigning people to a treatment or control group (analogous to a coin toss) based on a factor that is associated with the patient’s treatment but is not directly associated with the outcome. 20 Distance has been used as an instrumental variable in classic studies assessing outcome of specialty hospitals for acute myocardial infarction,20 as well as trauma. 10,21
In this study, our IV is the differential distance (DD) between the nearest acute care hospital and the nearest TC. DD meets the two key criteria of an instrumental variable: it is highly correlated with the treatment received but does not directly affect outcomes. (See Appendix 2 for instrumental variable analysis details and diagnostics.)
Our model estimated instrumental variable adjusted mortality differences using DD from a trauma center as the IV. In all models, we adjusted for all covariates including: age categories, gender, race/ethnicity, median household income of zipcode (in terciles), insurance status, injury severity (TMPM grouped in quartiles), E-code, injury category and year. (In sensitivity analyses we included two important populations which were initially excluded: rural and transfer patients. See Appendix 4 for more detail.)
All variables were checked to confirm a normal distribution (parametric), linearity of continuous variables and additivity of effects, as required by the assumptions of the regression model. In addition, model assumptions were verified, including functional form, random distribution of residuals, and for outliers or influential points. P values less than. 05 were apriori designated as statistically significant. Statistical analysis was performed using SAS 9.3 (SAS Institute Inc, Cary, NC) and STATA 10.1 for Windows (StataCorp LP, College Station, TX).
Results
Our final study population contained 77,874 seriously children: 52,214 (67.1%) were cared for in a TC (Table 1). Approximately half of the children were older adolescents (39,263); almost three quarters were male (56,664). The majority of injuries were unintentional. The top two injury mechanisms were motor vehicle crash (29,986), and falls (12,999). A total of 4,146 (5.3%) of the children in our sample died. TCs cared for more than double the volume of trauma patients of nTCs (n=52,214 vs. 25,660 respectively). Race/ethnicity and socio-economic profiles were different between TCs and nTCs. In general, an increased proportion of injured children cared for in a TC were Black or Hispanic and from poorer households than those in nTCs. It is notable that Blacks comprised 13.5% of the TC population, but 6.7% of the California population. Asians comprised approximately 5–6% of the TC and nTC population although they make up 10.9% of the California population.22 TCs cared for a larger proportion of children with public insurance than nTCs (53.1 vs. 34.1%). Fewer mild injuries were cared for in TCs compared to nTCs (31.0 vs. 41.3%); in contrast TCs cared for proportionally more severely injured patients (31.2 vs. 23.8%). A little less than double the proportion of children died in a TC vs. nTC (6.1 vs 3.8%). Of children cared for within a TC (52,214), approximately three quarters (38,836) were cared for in an aTC and one quarter were cared for in pediatric-specific trauma centers. Children cared for in an aTC vs. pTC were older (61.9 vs. 27.2% were 15–19 years of age) and a smaller proportion had public insurance (49.7 vs. 58.9%, respectively). Of children cared in an aTC and pTC, 6.3 vs. 5.8% respectively, died. (Table 1).
Table 1.
Demographics of population of seriously injured pediatric trauma patients after exclusions and adjustment for difference in TC and nTC hospital case mix.
| Total | Non-Trauma Center | % | Trauma Center (TC) | % | Adult TC | % | Pediatric TC | % | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | 77,874 | 25,660 | 32.95% | 52,214 | 67.05% | 38,836 | 49.87% | 16,091 | 20.66% |
| Total TC | |||||||||
|
| |||||||||
| Age (yr) | |||||||||
| 0–364 days | 3,877 | 1,455 | 5.67% | 2,422 | 4.64% | 1,162 | 2.99% | 1,246 | 7.74% |
| 1–4 | 9,410 | 2,765 | 10.78% | 6,645 | 12.73% | 3,792 | 9.76% | 3,050 | 18.95% |
| 5–9 | 10,373 | 3,492 | 13.61% | 6,881 | 13.18% | 3,933 | 10.13% | 3,266 | 20.30% |
| 10–14 | 14,951 | 5,521 | 21.52% | 9,430 | 18.06% | 5,911 | 15.22% | 4,155 | 25.82% |
| 15–19 | 39,263 | 12,427 | 48.43% | 26,836 | 51.40% | 24,038 | 61.90% | 4,374 | 27.18% |
| Gender | |||||||||
| Male | 56,664 | 18,898 | 73.65% | 37,766 | 72.33% | 28,716 | 73.94% | 10,870 | 67.55% |
| Female | 21,203 | 6,760 | 26.34% | 14,443 | 27.66% | 10,117 | 26.05% | 5,219 | 32.43% |
| Unknown | 7 | 2 | 0.01% | 5 | 0.01% | 3 | 0.01% | 2 | 0.01% |
| Race/Ethnicity | |||||||||
| White-non Hispanic | 28,765 | 12,047 | 46.95% | 16,718 | 32.02% | 13,551 | 34.89% | 5,131 | 31.89% |
| Black-non Hispanic | 8,936 | 1,906 | 7.43% | 7,030 | 13.46% | 4,947 | 12.74% | 2,053 | 12.76% |
| Hispanic | 32,125 | 9,429 | 36.75% | 22,696 | 43.47% | 16,811 | 43.29% | 6,330 | 39.34% |
| Asian | 4,474 | 1,372 | 5.35% | 3,102 | 5.94% | 2,269 | 5.84% | 878 | 5.46% |
| Native American | 184 | 69 | 0.27% | 115 | 0.22% | 95 | 0.24% | 40 | 0.25% |
| Other/unknown | 3,390 | 837 | 3.26% | 2,553 | 4.89% | 1,163 | 2.99% | 1,659 | 10.31% |
| Payer | |||||||||
| Public | 36,441 | 8,736 | 34.05% | 27,705 | 53.06% | 19,283 | 49.65% | 9,476 | 58.89% |
| HMO | 11,738 | 6,179 | 24.08% | 5,559 | 10.65% | 3,939 | 10.14% | 1,778 | 11.05% |
| Private | 22,207 | 8,233 | 32.08% | 13,974 | 26.76% | 11,127 | 28.65% | 4,117 | 25.59% |
| Self pay | 6,053 | 2,227 | 8.68% | 3,826 | 7.33% | 3,408 | 8.78% | 608 | 3.78% |
| Other/unknown | 1,435 | 285 | 1.11% | 1,150 | 2.20% | 1,079 | 2.78% | 112 | 0.70% |
| Income* | |||||||||
| <=2* FPL | 24,060 | 6,538 | 25.48% | 17,522 | 33.56% | 13,405 | 34.52% | 5,192 | 32.27% |
| 2* FPL – 3* FPL | 29,567 | 10,069 | 39.24% | 19,498 | 37.34% | 14,203 | 36.57% | 6,411 | 39.84% |
| >3* FPL | 22,153 | 8,289 | 32.30% | 13,864 | 26.55% | 10,095 | 25.99% | 4,183 | 26.00% |
| Unknown | 2,094 | 764 | 2.98% | 1,330 | 2.55% | 1,133 | 2.92% | 305 | 1.90% |
| Disposition | |||||||||
| Died | 4,146 | 972 | 3.79% | 3,174 | 6.08% | 2,431 | 6.26% | 939 | 5.84% |
| Discharge | 73,726 | 24,687 | 96.21% | 49,039 | 93.92% | 36,405 | 93.74% | 15,151 | 94.16% |
| Unknown | 2 | 1 | 0.00% | 1 | 0.00% | 0 | 0.00% | 1 | 0.01% |
| Injury Mechanism** | |||||||||
| Fall | 12,999 | 5,601 | 21.83% | 7,398 | 14.17% | 4,777 | 12.30% | 2,816 | 17.50% |
| Firearm | 9,543 | 2,077 | 8.09% | 7,466 | 14.30% | 6,285 | 16.18% | 1,254 | 7.79% |
| MVA | 29,986 | 7,344 | 28.62% | 22,642 | 43.36% | 17,138 | 44.13% | 7,124 | 44.27% |
| Injury Type*** | |||||||||
| Central nervous system | 30,387 | 8,591 | 33.48% | 21,796 | 41.74% | 15,175 | 39.07% | 6,775 | 42.10% |
| Abd thorax | 39,419 | 13,449 | 52.41% | 25,970 | 49.74% | 19,553 | 50.35% | 8,012 | 49.79% |
| Blood vessels | 2,410 | 470 | 1.83% | 1,940 | 3.72% | 1,600 | 4.12% | 426 | 2.65% |
| Other | 18,005 | 5,144 | 20.05% | 12,861 | 24.63% | 8,978 | 23.12% | 4,717 | 29.31% |
| Injury Severity | |||||||||
| Mild (iss<9)**** | 26,765 | 10,601 | 41.31% | 16,164 | 30.96% | 12,227 | 31.48% | 4,665 | 28.99% |
| Moderate(9<=iss<=15) | 28,623 | 8,905 | 34.70% | 19,718 | 37.76% | 14,981 | 38.58% | 5,775 | 35.89% |
| Severe (iss>15) | 22,373 | 6,099 | 23.77% | 16,274 | 31.17% | 11,608 | 29.89% | 5,613 | 34.88% |
| ISS not listed | 113 | 55 | 0.21% | 58 | 0.11% | 20 | 0.05% | 38 | 0.24% |
Missing data was minimal. There was no differential missing data rate by outcomes.
Income is median household income per zipcode and is based on federal poverty level (FPL) from 2004 ($18,850 household income)
Injury Mechanism is based on E-code; Patients can have 0 to 5 E-codes thus the column sum can be greater than 100%. We list only the top three mechanisms of injury.
Injury type: Injury type is categorized according to ICD-9 groupings. We list only the most serious categories. These are not mutually exclusive.
ISS=Injury Severity Score
Our model demonstrates the effect of TC vs. nTC care on the population of children with serious injury who could benefit from trauma center care (n=77,874 with an unadjusted mortality of 5.3%) (Table 2). Using IV techniques to adjust for unobservable differences in the populations cared for in TC vs. nTC, we demonstrate a −0.79 (95% CI −0.80 to −0.30; p=0.044) percentage point impact on mortality for children cared for in TC vs. nTC.
Table 2.
IV regression model demonstrating estimates of treatment effect (decreased mortality) of trauma center care vs. non-trauma center care. All models have been adjusted for demographic and clinical variables as delineated in the text including: age, sex, race/ethnicity, median household income, payer status, injury severity (TMPM) and mechanism, and year.
| Variable | Estimate* | (p) | CI |
|---|---|---|---|
|
| |||
| TC mortality affect | −0.79 | 0.044 | −0.80 to −0.30 |
|
| |||
| 0–1 | ref | ||
| 1–4 | 1.26 | 0.001 | 0.50 to 2.02 |
| 5–9 | 0.84 | 0.03 | 0.07 to 1.62 |
| 10–14 | 0.29 | 0.46 | −0.47 to 1.04 |
| 15–19 | 0.37 | 0.32 | −3.59 to 1.10 |
| Gender | |||
| Male | ref | ||
| Female | −0.11 | 0.49 | −0.42 to 0.20 |
| Race/Ethnicity | |||
| White non hispanic | ref | ||
| Black non hispanic | 0.36 | 0.15 | −0.13 to 0.85 |
| Hispanic | 0.06 | 0.72 | −0.28 to 0.40 |
| Asian | 0.87 | 0.01 | 0.27 to 1.47 |
| Native | 0.08 | 0.95 | −2.67 to 2.83 |
| Other | 0.85 | 0.03 | 0.07 to 1.63 |
| Payer | |||
| Public | ref | ||
| HMO | 1.17 | <0.0001 | 0.72 to 1.62 |
| Private | 1.03 | <0.0001 | 0.67 to 1.39 |
| Self pay | 3.35 | <0.0001 | 2.82 to 3.88 |
| Other | 2.18 | <0.0001 | 1.18 to 3.19 |
| Income | |||
| <=2* FPL | ref | ||
| 2*FPL - 3*FPL | −0.35 | 0.03 | −0.68 to −0.03 |
| >3* FPL | −0.29 | 0.13 | −0.67 to 0.09 |
| Mechanism | |||
| Fall | ref | ||
| Firearm | 8.62 | <0.0001 | 7.85 to 9.39 |
| MVA | 1.51 | <0.0001 | 1.07 to 1.95 |
| Intent | |||
| Unintentional | ref | ||
| Intentional (suicide) | 13.15 | <0.0001 | 11.57 to 14.73 |
| Assault | −1.47 | <0.0001 | −2.08 to −0.85 |
Regression diagnostics: The partial F of 210.52 falls well above the recommended value of 30 for a superior instrument.40
Estimates are in percentage points
bold indicates significance
Sensitivity analyses which included the a) rural, b) transfer and c) rural and transfer populations combined into our analyses demonstrate: a −0.71 (95% CI −1.22 to 0.03; p=0.53); a −0.98 (95% CI −1.78 to −0.22; p=0.012); and a −0.95 (95% CI −1.70 to −0.21; p=0.012) percentage point impact on mortality in TC vs. nTC (see Appendix 4 table A-4b for details).
Our model demonstrates that of children with serious injury, payer status had a significant impact on mortality in both models. The categories of “self-pay” and “other payer” are associated with a 3.13 (95% CI 2.64 to 3.64; p<0.0001) and 2.05 (95% CI 1.16 to 2.95; p<0.0001) percentage point increase in mortality, respectively. Higher household income categories are associated with a statistically significant decrease in mortality. Households with income between 2–3 times and greater than 3 times the federal poverty level had −0.39 (95% CI −0.69 to −0.09; p=0.009) and −0.44 (95% CI −0.78 to −0.10; p=0.01) percentage point decrease in mortality, respectively. Race/ethnicity categories were not associated with a clear pattern of mortality benefit. Mechanisms of intentional injury had no mortality benefit from TC care and in fact there was a 12.53 (95% CI 11.06 to 14.00; p<0.0001) percentage point increase in mortality. However, assault injuries had a significant mortality benefit of a −1.14 (95% CI −1.70 to −0.59; p<0.0001) percentage point decrease in mortality from TC care. (Table 2)
Our second model analyzed the effect of aTC vs. pTC care on the population of children with serious injury who could benefit from trauma center care (n=52,214 with an unadjusted mortality of 6.5%). We found a 0.64 (95% CI −0.26 to 1.54; p=0.16) percentage point increase in mortality for children treated in an pTC vs. aTC, which was not statistically significant. (Table 3)
Table 3.
Regression models demonstrating treatment estimates of effect (decreased mortality) of pediatric trauma center care vs. adult trauma center care.
All models have been adjusted for demographic and clinical variables as delineated in the text including: age, sex, race/ethnicity, median household income, payer status, injury severity (TMPM) and mechanism, and year.
| Population (n=52,214; unadjusted mortality: 6.5%) | Estimate* | (p) | CI |
|---|---|---|---|
| Pediatric Trauma Center vs. Adult Trauma Center Care | 0.64 | 0.16 | −0.26 to 1.54 |
| Trauma center mortality effect |
Regression diagnostics: The partial F of 219.7 is well above the recommended value of 30 for a superior instrument.40
Estimates are in percentage points
Discussion
Seriously injured children have unique resource and expertise needs, which are not uniformly available. There has been, to date, insufficient evidence to determine the optimal location of care for children with trauma. 23 Most outcome studies are from single institutions and are unable to account for regionalization of trauma services. To our knowledge, there are very few population-wide studies measuring the benefit of TC compared with nTC care for children. 24 While Rutledge did not find decreased mortality for children with a trauma center within the county of injury in North Carolina, 25 Hulka demonstrated decreased pediatric mortality from trauma in the Oregon statewide trauma system. 26 More recently, Pracht demonstrated decreased mortality in children (0–19 years) receiving TC care in Florida. 10 We demonstrate that, in California, seriously injured children cared for in TCs have decreased mortality compared to children cared for in non-trauma hospital settings. Our sensitivity analyses support the strength of our models, demonstrating that the TC mortality benefit extends to rural and transfer patients although the magnitude and overall significance of the effect varies.
Although not our primary outcome, we note with concern that after controlling for clinical and socio-demographic variables including median household income and race/ethnicity, children with “self pay” and “other payer” status had up to a 3 percentage point increase in death after trauma. This finding of increased rates of trauma death for children from poor households27 and who are uninsured 28,29 has been noted in the literature. Our previous work has also demonstrated that uninsured injured children have an increased likelihood of dying in the ED as compared to privately insured children.30 Reasons for this disparity in outcomes have been postulated as possibly due to decreased utilization of medical care and preventative services, resulting in poorer baseline health and increased preexisting conditions, as well as decreased access to quality care after an injury.27,29,31
Our sensitivity analyses, which included children living in rural areas and transfer patients, continue to demonstrate a mortality benefit for children cared for in a TC. Although these results must be interpreted with caution, they may provide evidence that current local EMS system practices are operating effectively for these challenging populations most in need of systematic trauma care.
Much of the discourse regarding whether trauma care improves outcomes for children has focused on whether pediatric specific trauma care has better outcomes than aTCs, with controversial results.32–34 In Florida, Pracht et al used a population-wide analysis similar to ours, and found no significant mortality benefit for pediatric specific trauma center care in younger children aged 0–15, but did find benefit when all children (0–19) were included in the model. We were unable to replicate those results. However, given the relatively low overall mortality rate of pediatric trauma, the fact that pTCs are scarce and non-uniformly distributed, in conjunction with other confounders including differences in demographic, geographic and trauma system characteristics between Florida and California, we were not surprised that we were unable to demonstrate that subspecialty pTC care has any mortality benefit over aTC care in California.
Regardless of our ability to demonstrate a mortality difference in pTC vs. aTC outcomes for children with serious injury; we believe that pediatric subspecialty care has many benefits, including possible mortality benefits not demonstrable with our analytic methods. However, ultimately a minority of injured children in the US are cared for in pTCs 35 or children’s hospitals.36 We believe that the discourse regarding whether trauma care improves outcomes for children must focus on our finding that trauma specific care, be it adult or pediatric, improves patient outcomes. Our research and previously published literature clearly mandate that we must act now to ensure every child has access to specialized trauma care, with further access to subspecialty care an important future step.3,10,32,33
This is one of the largest population-based analyses of which we are aware, which demonstrates that TC care saves lives for seriously injured children. Given that pediatric trauma care outcomes are dependent on regionalization of services, of which TC care is only one component, and because we use administrative data, we suspect our results are actually an underestimation of the benefits of TC and trauma system care. However, we believe our findings and methodology are significant initial steps to enable academicians, physicians, EMS administrators and policymakers to take evidence-based steps to decrease disparities in access to and outcomes of trauma care for children. 37 For example, based on our results, as well as suggested by others, EMS and community should be educated to initially bring seriously injured children to a TC regardless of pediatric subspecialty status. 32 Although further research is necessary to discover how these findings might be applied to rural and transfer populations, these data might support systematic development of formal transfer agreements between nTC and TC. Our methods can be used to further understand if outcomes are improved if subpopulations of critical trauma patients are transported directly to a trauma center (bypassing closer, local facilities), as has been demonstrated for closed head injury in adults. 38
Our work has limitations. While California is a large and diverse state, our analyses represent only one state. Although it is a common belief among trauma researchers that physiologic data is needed to demonstrate trauma care outcome benefits, we use administrative hospital discharge data, as it was the only way to conduct a total population analysis without a statewide trauma system. We also stringently defined our population of seriously injured children as children with injuries that could result in death. Using physiologic data as well as data linked across different arenas of care (out-of-hospital, ED, and in-hospital) are the next steps in understanding the full scope of trauma center outcomes. Additionally, mortality may be too crude of an outcome measurement and alternative outcomes to survival such as processes of care, 39 measures of functional outcomes, and quality of care are needed to fully demonstrate improved trauma center outcomes.
Conclusion
Our trauma center outcome models use improved injury severity and case mix adjustment, as well as unique statistical methods to demonstrate decreased mortality for seriously injured children treated in major trauma centers.
Figure 1. Derivation of patient study sample from the California Office of Statewide Health Planning and Development Patient Discharge Database (1999–2011).
*=Excludes children with sole codes indicating minor injuries, perinatal or pregnancy associated conditions, burn injuries.
**=Children cared for in level III and IV TCs were eliminated when matching TC and ntC diagnoses
***=Categories are not mutually exclusive
Appendix 1
Method used to limit the study population to children with serious injury potentially associated with death.
We identified ICD-9 code groupings accepted in the literature as indicative of serious injury with a high likelihood of fatality including: fractures (of the skull, neck and trunk) intracranial injury and spinal cord injuries (800–809,850–854, and 952); internal injury of the thorax, abdomen or pelvis (860–869); and injury of blood vessels (900–904).10
To further refine our population, the emergency physician author (NEW) identified and removed any injury codes which could be associated with, but not cause, death. If an injury’s level of association with death was unclear, the author consulted with trauma colleagues.
Our study population thus included patients that had the following ICD-9 diagnostic codes included anywhere in the primary and up to additional 24 ICD-9 diagnostic codes possible.
Table A-1.
ICD-9 codes indicative of serious, potentially fatal, injury
| Injury Category | ICD-9 codes (Specific) |
|---|---|
| Fracture of Skull (800–804) | 800.05, 800.06, 801.05, 801.06, 801.15, 801.16, 801.2x, 801.3x, 801.45, 801.46, 801.55, 801.56, 801.65, 801.66, 801.7x, 801.8x, 801.9x, 803.05, 803.06, 803.15, 803.16, 803.2x, 803.3x, 803.45, 803.46, 803.55, 803.56, 803.65, 803.66, 803.7x, 803.8x, 803.9x, 804.05, 804.06, 804.15, 804.16, 804.2x, 804.3x, 804.4x, 804.55, 804.56, 804.65, 804.66, 804.7x |
| Fracture of Spine and Trunk (805–809) | 805.0x, 805.1x, 807.03, 807.04, 807.05, 807.06, 807.07, 807.08, 807.09, 807.1x, 807.4, 807.5x, 807.6x, 808.x |
| Dislocation-multiple locations (839) | 839.0x, 839.1x |
| Intracranial Injury, Excluding those with skull fracture (850–854) | 850.4, 851.05, 851.06, 851.1x, 851.2x, 851.3x, 851.4x, 851.5x, 851.6x, 851.7x, 851.8x, 851.9x, 852.x, 853.x, 854.x |
| Internal injury of chest, abdomen and pelvis (860–869) | All |
| Open wound of neck and chest (874, 875) | 874.0x, 874.0x, 874.1x, 874.4x, 874.5x, 875.x |
| Injury to blood vessels (900–904) | 900.x, 901.x, 902.x, 904.0, 904.2, |
| Crushing injury of face, scalp, neck and trunk (925, 926) | 925.2, 926 |
| Injury to nerves and spinal cord | 952.0x, 952.1x, 958.0, 958.1, 958.2, 958.4, 958.5 |
Appendix 2
Details of Instrumental Variables analysis
Distance has been used as an IV in classic studies assessing outcome of specialty hospitals for acute myocardial infarction,20 as well as trauma. 10,21 Thus, we used the differential distance (DD) between the nearest acute care hospital and the nearest TC as our IV. DD meets the two key criteria of an IV; it is highly correlated with the treatment received; however, DD does not directly affect outcomes.
A DD of <=4 miles and >4 miles broke our population into two approximately equally sized groups. Gender, age groupings and injury severity were proportionally similar in both groups; race/ethnicity, insurance, household income and some injury characteristics varied (Table A-2).
Classic econometric studies have used a two step linear model with their IV analyses,20,41 although the majority of trauma outcome studies use a bivariable probit model.10,21,38 We estimated both types of models with similar trends but present the linear models because the results were much easier to interpret.
The partial F of the instrument is the definitive regression diagnostic for instrumental variables analyses. It is a test of the explanatory power of the instrument. The partial Fs of our instrument (stated at the bottom of each model) are well above the recommended value of 30 for a superior instrument.40
Table A-2.
Comparison of the populations with a DD of <=4 miles and >4 miles.
| Total | Non-Trauma Center | % | Trauma Center (TC) | % | DD<=4mi | % | DD>4mi | % | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | 77,874 | 25,660 | 32.95% | 52,214 | 67.05% | 37,936 | 52.60% | 37,019 | 46.80% |
| Total TC | |||||||||
|
| |||||||||
| Age (yr) | |||||||||
| 0–364 days | 3,877 | 1,455 | 5.67% | 2,422 | 4.64% | 1,997 | 5.26% | 1,693 | 4.57% |
| 1–4 | 9,410 | 2,765 | 10.78% | 6,645 | 12.73% | 4,947 | 13.04% | 4,126 | 11.15% |
| 5–9 | 10,373 | 3,492 | 13.61% | 6,881 | 13.18% | 5,074 | 13.38% | 5,012 | 13.54% |
| 10–14 | 14,951 | 5,521 | 21.52% | 9,430 | 18.06% | 6,898 | 18.18% | 7,530 | 20.34% |
| 15–19 | 39,263 | 12,427 | 48.43% | 26,836 | 51.40% | 19,020 | 50.14% | 18,658 | 50.40% |
| Gender | |||||||||
| Male | 56,664 | 18,898 | 73.65% | 37,766 | 72.33% | 27,842 | 73.39% | 26,663 | 72.03% |
| Female | 21,203 | 6,760 | 26.34% | 14,443 | 27.66% | 10,092 | 26.60% | 10,352 | 27.96% |
| Unknown | 7 | 2 | 0.01% | 5 | 0.01% | 2 | 0.01% | 4 | 0.01% |
| Race/Ethnicity | |||||||||
| White-non Hispanic | 28,765 | 12,047 | 46.95% | 16,718 | 32.02% | 10,865 | 28.64% | 16,946 | 45.78% |
| Black-non Hispanic | 8,936 | 1,906 | 7.43% | 7,030 | 13.46% | 6,055 | 15.96% | 2,575 | 6.96% |
| Hispanic | 32,125 | 9,429 | 36.75% | 22,696 | 43.47% | 16,734 | 44.11% | 14,063 | 37.99% |
| Asian | 4,474 | 1,372 | 5.35% | 3,102 | 5.94% | 2,565 | 6.76% | 1,754 | 4.74% |
| Native American | 184 | 69 | 0.27% | 115 | 0.22% | 66 | 0.17% | 118 | 0.32% |
| Other/unknown | 3,390 | 837 | 3.26% | 2,553 | 4.89% | 1,651 | 4.35% | 1,563 | 4.22% |
| Payer | |||||||||
| Public | 36,441 | 8,736 | 34.05% | 27,705 | 53.06% | 19,714 | 51.97% | 15,117 | 40.84% |
| Hmo | 11,738 | 6,179 | 24.08% | 5,559 | 10.65% | 5,396 | 14.22% | 6,066 | 16.39% |
| Private | 22,207 | 8,233 | 32.08% | 13,974 | 26.76% | 9,077 | 23.93% | 12,318 | 33.27% |
| Self pay | 6,053 | 2,227 | 8.68% | 3,826 | 7.33% | 2,957 | 7.79% | 2,914 | 7.87% |
| Other/unknown | 1,435 | 285 | 1.11% | 1,150 | 2.20% | 792 | 2.09% | 604 | 1.63% |
| Income | |||||||||
| <=2* FPL | 24,060 | 6,538 | 25.48% | 17,522 | 33.56% | 15,737 | 41.48% | 7,568 | 20.44% |
| 2* FPL - 3* FPL | 29,567 | 10,069 | 39.24% | 19,498 | 37.34% | 11,818 | 31.15% | 16,467 | 44.48% |
| >3* FPL | 22,153 | 8,289 | 32.30% | 13,864 | 26.55% | 9,590 | 25.28% | 11,764 | 31.78% |
| NA | 2,094 | 764 | 2.98% | 1,330 | 2.55% | 791 | 2.09% | 1,220 | 3.30% |
| Disposition | |||||||||
| Died | 4,146 | 972 | 3.79% | 3,174 | 6.08% | 2,124 | 5.60% | 1,879 | 5.08% |
| Discharge | 73,726 | 24,687 | 96.21% | 49,039 | 93.92% | 35,812 | 94.40% | 35,138 | 94.92% |
| Unknown | 2 | 1 | 0.00% | 1 | 0.00% | 0 | 0.00% | 2 | 0.01% |
| Injury Mechanism | |||||||||
| Fall | 12,999 | 5,601 | 21.83% | 7,398 | 14.17% | 6,526 | 17.20% | 5,962 | 16.11% |
| Firearm | 9,543 | 2,077 | 8.09% | 7,466 | 14.30% | 6,107 | 16.10% | 3,141 | 8.48% |
| MVA | 29,986 | 7,344 | 28.62% | 22,642 | 43.36% | 13,871 | 36.56% | 15,106 | 40.81% |
| Injury Type | |||||||||
| CNS | 30,387 | 8,591 | 33.48% | 21,796 | 41.74% | 15,041 | 39.65% | 14,230 | 38.44% |
| Abd thorax | 39,419 | 13,449 | 52.41% | 25,970 | 49.74% | 18,503 | 48.77% | 19,293 | 52.12% |
| blood vessels | 2,410 | 470 | 1.83% | 1,940 | 3.72% | 1,411 | 3.72% | 894 | 2.41% |
| Other | 18,005 | 5,144 | 20.05% | 12,861 | 24.63% | 8,282 | 21.83% | 8,898 | 24.04% |
| Injury Severity | |||||||||
| Iss n/a | 26,765 | 10,601 | 41.31% | 16,164 | 30.96% | 13,412 | 35.35% | 12,669 | 34.22% |
| Mild (iss<9)* | 28,623 | 8,905 | 34.70% | 19,718 | 37.76% | 13,997 | 36.90% | 13,463 | 36.37% |
| Moderate (9<=iss<=15) | 22,373 | 6,099 | 23.77% | 16,274 | 31.17% | 10,484 | 27.64% | 10,829 | 29.25% |
| Severe (iss>15) | 113 | 55 | 0.21% | 58 | 0.11% | 43 | 0.11% | 58 | 0.16% |
ISS=Injury Severity Score
Appendix 3
Sensitivity analysis of regression analyses between nTC and TC using ISS as the injury severity score.
Table A-3.
Regression model demonstrating treatment estimates of effect (decreased mortality) of pediatric trauma center care vs. adult trauma center care using ISS as the injury severity score.
All models have been adjusted for demographic and clinical variables as delineated in the text including: age, sex, race/ethnicity, median household income, payer status, injury severity (ISS) and mechanism, and year.
| Population (n=52,214; unadjusted mortality: 6.5%) | Estimate* | (p) | CI |
|---|---|---|---|
| Pediatric Trauma Center vs. Adult Trauma Center Care | 0.33 | 0.47 | −0.56 to 1.21 |
| Trauma center mortality effect |
Regression diagnostics: The partial F of 219.7 is well above the recommended value of 30 for a superior instrument.40
Estimates are in percentage points
Appendix 4
Sensitivity analysis of analyses including rural and transfer populations. We initially excluded rural and transfer populations from our analyses. After putting these patients back into the study population, we demonstrate the demographics of the entire population of seriously injured pediatric trauma patients after exclusions and adjustment for difference in TC and nTC hospital case mix. (Table A-4a).
We created models demonstrating estimates of treatment effect (decreased mortality) of trauma center care vs. non-trauma center care including the rural population (Table A-4b).
All models have been adjusted for demographic and clinical variables as delineated in the text including: age, sex, race/ethnicity, median household income, payer status, injury severity (TMPM) and mechanism, and year.
Table A-4a.
Demographics of population of seriously injured pediatric trauma patients including rural and transfer populations, after exclusions and adjustment for difference in TC and nTC hospital case mix.
| Total | Non-Trauma Center | % | Trauma Center (TC) | % | Adult TC | % | Pediatric TC | % | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | 90,800 | 31,481 | 34.67% | 59,319 | 65.33% | 40,364 | 44.45% | 18,258 | 20.11% |
| Total TC | |||||||||
|
| |||||||||
| Age (yr) | |||||||||
| 0–364 days | 4,848 | 1,809 | 5.75% | 3,039 | 5.12% | 1,327 | 3.29% | 1,552 | 8.50% |
| 1–4 | 11,178 | 3,414 | 10.84% | 7,764 | 13.09% | 4,034 | 9.99% | 3,605 | 19.74% |
| 5–9 | 12,294 | 4,274 | 13.58% | 8,020 | 13.52% | 4,145 | 10.27% | 3,757 | 20.58% |
| 10–14 | 17,645 | 6,745 | 21.43% | 10,900 | 18.38% | 6,136 | 15.20% | 4,675 | 25.61% |
| 15–19 | 44,835 | 15,239 | 48.41% | 29,596 | 49.89% | 24,722 | 61.25% | 4,669 | 25.57% |
| Gender | |||||||||
| Male | 65,578 | 22,973 | 72.97% | 42,605 | 71.82% | 29,799 | 73.83% | 12,271 | 67.21% |
| Female | 25,215 | 8,506 | 27.02% | 16,709 | 28.17% | 10,562 | 26.17% | 5,985 | 32.78% |
| Unknown | 7 | 2 | 0.01% | 5 | 0.01% | 3 | 0.01% | 2 | 0.01% |
| Race/Ethnicity | |||||||||
| White-non Hispanic | 35,896 | 15,402 | 48.92% | 20,494 | 34.55% | 14,250 | 35.30% | 6,002 | 32.87% |
| Black-non Hispanic | 9,713 | 2,294 | 7.29% | 7,419 | 12.51% | 5,066 | 12.55% | 2,254 | 12.35% |
| Hispanic | 35,819 | 11,024 | 35.02% | 24,795 | 41.80% | 17,428 | 43.18% | 7,087 | 38.82% |
| Asian | 4,937 | 1,615 | 5.13% | 3,322 | 5.60% | 2,315 | 5.74% | 963 | 5.27% |
| Native American | 250 | 98 | 0.31% | 152 | 0.26% | 99 | 0.25% | 53 | 0.29% |
| Other/unknown | 4,185 | 1,048 | 3.33% | 3,137 | 5.29% | 1,206 | 2.99% | 1,899 | 10.40% |
| Payer | |||||||||
| Public | 41,584 | 10,529 | 33.45% | 31,055 | 52.35% | 20,027 | 49.62% | 10,712 | 58.67% |
| HMO | 14,325 | 8,020 | 25.48% | 6,305 | 10.63% | 4,137 | 10.25% | 2,080 | 11.39% |
| Private | 26,494 | 9,974 | 31.68% | 16,520 | 27.85% | 11,601 | 28.74% | 4,680 | 25.63% |
| Self pay | 6,799 | 2,604 | 8.27% | 4,195 | 7.07% | 3,493 | 8.65% | 658 | 3.60% |
| Other/unknown | 1,598 | 354 | 1.12% | 1,244 | 2.10% | 1,106 | 2.74% | 128 | 0.70% |
| Income* | |||||||||
| <=2* FPL | 27,983 | 8,198 | 26.04% | 19,785 | 33.35% | 13,877 | 34.38% | 5,750 | 31.49% |
| 2* FPL - 3* FPL | 35,025 | 12,659 | 40.21% | 22,366 | 37.70% | 14,822 | 36.72% | 7,280 | 39.87% |
| >3* FPL | 25,156 | 9,577 | 30.42% | 15,579 | 26.26% | 10,459 | 25.91% | 4,865 | 26.65% |
| Unknown | 2,636 | 1,047 | 3.33% | 1,589 | 2.68% | 1,206 | 2.99% | 363 | 1.99% |
| Disposition | |||||||||
| Died | 4,836 | 1,201 | 3.81% | 3,635 | 6.13% | 2,528 | 6.26% | 1,100 | 6.02% |
| Discharge | 85,961 | 30,278 | 96.18% | 55,683 | 93.87% | 37,836 | 93.74% | 17,157 | 93.97% |
| Unknown | 3 | 2 | 0.01% | 1 | 0.00% | 0 | 0.00% | 1 | 0.01% |
| Injury Mechanism** | |||||||||
| Fall | 15,281 | 6,649 | 21.12% | 8,632 | 14.55% | 5,074 | 12.57% | 3,240 | 17.75% |
| Firearm | 10,251 | 2,419 | 7.68% | 7,832 | 13.20% | 6,453 | 15.99% | 1,321 | 7.24% |
| MVA | 35,282 | 9,536 | 30.29% | 25,746 | 43.40% | 17,647 | 43.72% | 7,979 | 43.70% |
| Injury Type*** | |||||||||
| Central nervous system | 35,481 | 10,601 | 33.67% | 24,880 | 41.94% | 15,836 | 39.23% | 7,760 | 42.50% |
| Abd thorax | 45,583 | 16,314 | 51.82% | 29,269 | 49.34% | 20,177 | 49.99% | 8,989 | 49.23% |
| Blood vessels | 2,676 | 559 | 1.78% | 2,117 | 3.57% | 1,638 | 4.06% | 476 | 2.61% |
| Other | 21,632 | 6,659 | 21.15% | 14,973 | 25.24% | 9,383 | 23.25% | 5,379 | 29.46% |
| Injury Severity | |||||||||
| Mild (iss<9)**** | 30,652 | 12,587 | 39.98% | 18,065 | 30.45% | 12,708 | 31.48% | 5,276 | 28.90% |
| Moderate(9<=iss<=15) | 33,022 | 10,902 | 34.63% | 22,120 | 37.29% | 15,503 | 38.41% | 6,516 | 35.69% |
| Severe (iss>15) | 26,982 | 7,922 | 25.16% | 19,060 | 32.13% | 12,128 | 30.05% | 6,420 | 35.16% |
| Iss not listed | 144 | 70 | 0.22% | 74 | 0.12% | 25 | 0.06% | 46 | 0.25% |
| MSA status# | |||||||||
| Rural | 6,714 | 3,065 | 9.74% | 3,649 | 6.15% | 2,308 | 5.72% | 1,341 | 7.34% |
| Urban | 84,086 | 28,416 | 90.26% | 55,670 | 93.85% | 38,056 | 94.28% | 16,917 | 92.66% |
| Transfer status | |||||||||
| Transferred -in | 6,246 | 2,692 | 8.55% | 3,554 | 5.99% | 1,393 | 3.45% | 2,113 | 11.57% |
Missing data was minimal. There was no differential missing data rate by outcomes
Income is median household income per zipcode and is based on federal poverty level (FPL) from 2004 ($18,850 household income)
Injury Mechanism is based on E-code; Patients can have 0 to 5 E-codes thus the column sum can be greater than 100%. We list only the top three mechanisms of injury.
Injury type: Injury type is categorized according to ICD-9 groupings. We list only the most serious categories. These are not mutually exclusive.
ISS=Injury Severity Score
MSA=metropolitan statistical area as designated by U.S. Census Bureau
Table A-4b.
IV Regression models demonstrating estimates of treatment effect (decreased mortality) of trauma center care vs. non-trauma center care including rural, transfer and both populations. We include also the estimates of age and payer status on treatment effect.
All models have been adjusted for demographic and clinical variables as delineated in the text including: age, sex, race/ethnicity, median household income, payer status, injury severity (TMPM) and mechanism, and year.
| Population of seriously injured children including rural population (n=80,795) | Population of seriously injured children including transfer population (n=80,219) | Population of seriously injured children including rural and transfer population (n=86,934) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Est.* | (p) | CI | Est. | (p) | CI | Est. | (p) | CI | |
|
| |||||||||
| TC mortality effect | −0.71 | 0.053 | −1.22 to 0.03 | −0.98 | 0.012 | −1.78 to −0.22 | −0.95 | 0.012 | −1.70 to −.21 |
|
| |||||||||
| Age | |||||||||
| 0–1 | ref | ref | ref | ||||||
| 1–4 | 1.28 | 0.001 | 0.54 to 2.02 | 1.13 | 0.002 | 0.41 to 1.84 | 1.12 | 0.002 | 0.43 to 1.81 |
| 5–9 | 0.84 | 0.03 | 0.08 to 1.59 | 0.56 | 0.13 | −0.17 to 1.30 | 0.51 | 0.16 | −0.20 to 1.22 |
| 10–14 | 0.29 | 0.44 | −0.44 to 1.02 | −0.04 | 0.91 | −0.76 to 0.68 | −0.05 | 0.88 | −0.75 to 0.64 |
| 15–19 | 0.27 | 0.45 | −0.44 to 0.98 | 0.01 | 0.98 | −0.70 to 0.68 | −0.1 | 0.77 | −0.77 to 0.57 |
| Gender | |||||||||
| Male | ref | ref | ref | ||||||
| Female | −0.09 | 0.55 | −0.39 to 0.21 | −0.06 | 0.69 | −0.36 to 0.24 | −0.08 | 0.58 | −0.37 to 0.21 |
| Race/Ethnicity | |||||||||
| White non Hispanic | ref | ref | ref | ||||||
| Black non Hispanic | 0.36 | 0.14 | −0.11 to 0.84 | 0.39 | 0.11 | 0.22 to 1.39 | 0.35 | 0.14 | −0.11 to 0.81 |
| Hispanic | 0.07 | 0.69 | −0.26 to 0.39 | 0.08 | 0.62 | −0.24 to 0.41 | 0.06 | 0.60 | −0.26 to 0.37 |
| Asian | 0.94 | 0.002 | 0.35 to 1.52 | 0.81 | 0.01 | 0.24 to 1.26 | 0.86 | 0.001 | 0.29 to 1.43 |
| Native | −0.01 | 0.99 | −2.50 to 2.48 | 0.46 | 0.73 | −2.18 to 3.11 | 0.21 | 0.94 | −2.18 to 2.60 |
| Other | 0.61 | 0.11 | −0.13 to 1.35 | 1.02 | 0 | 0.26 to 1.77 | 0.65 | 0.02 | −0.06 to 1.37 |
| Payer | |||||||||
| Public | ref | ref | ref | ||||||
| HMO | 1.15 | <0.0001 | 0.71 to 1.58 | 0.822 | 0.02 | 0.38 to 1.26 | 0.78 | <0.0001 | 0.36 to 1.21 |
| Private | 0.93 | <0.0001 | 0.59 to 1.27 | 1 | <0.0001 | 0.65 to 1.35 | 0.88 | <0.0001 | 0.55 to 1.22 |
| Self pay | 3.33 | <0.0001 | 2.82 to 3.84 | 3.29 | <0.0001 | 2.77 to 3.82 | 3.26 | <0.0001 | 2.76 to 3.77 |
| Other | 2.27 | <0.0001 | 1.29 to 3.24 | 2.14 | <0.0001 | 1.14 to 3.27 | 2.16 | <0.0001 | 1.20 to 3.12 |
| Income | |||||||||
| <=2* FPL | ref | ref | ref | ||||||
| 2*FPL - 3*FPL | −0.35 | 0.03 | −0.66 to −0.04 | −0.25 | 0.12 | −0.57 to 0.06 | −0.30 | 0.05 | −0.60 to 0.00 |
| >3* FPL | −0.28 | 0.13 | −0.64 to 0.08 | −0.21 | 0.26 | −0.58 to 0.16 | −0.24 | 0.18 | −0.59 to 0.11 |
| Mechanism** | |||||||||
| Fall | ref | ref | ref | ||||||
| Firearm | 8.66 | <0.0001 | 7.92 to 9.40 | 8.29 | <0.0001 | 7.55 to 9.03 | 8.39 | <0.0001 | 7.67 to 9.10 |
| MVA Intent | 1.51 | <0.0001 | 1.09 to 1.94 | 1.48 | <0.0001 | 1.05 to 1.90 | 1.51 | <0.0001 | 1.10 to 1.92 |
| Unintentional | ref | ref | ref | ||||||
| Intentional (suicide) | 13.06 | <0.0001 | 11.54 to 14.57 | 13.20 | <0.0001 | 11.67 to 14.73 | 13.47 | <0.0001 | 12.00 to 14.94 |
| Assault | −1.49 | <0.0001 | −2.08 to −0.89 | −1.17 | <0.0001 | −1.76 to −0.57 | 1.22 | <0.0001 | −1.79 to −0.64 |
estimates are in percentage points
bold indicates significance
Footnotes
Conflict of Interest: No conflicts of interest have been declared by any author.
Author Contribution:
NE Wang:
Contributed to all portions of the study: Literature search, study design, data analysis and interpretation, writing and critical revision.
Olga Saynina
Contributed to: literature search, study design, data analysis and interpretation and critical revision.
Lara Vogel
Contributed to: literature search, data interpretation, and critical revision.
Craig D. Newgard
Contributed to: literature search, data interpretation, and critical revision.
Jayanta Bhattacharya:
Contributed to: study design, data analysis and interpretation, and critical revision.
Ciaran S. Phibbs
Contributed to: study design, data analysis and interpretation, and critical revision.
Funding Disclosure: Work funded by National Institute of Health Grant NICH K23 HD051595
Contributor Information
NE Wang, Email: ewen@stanford.edu, Associate Professor Surgery and by courtesy Pediatrics, Stanford University School of Medicine, Stanford, California, 94305, (650) 723-0757.
Olga Saynina, Email: Olga0@stanford.edu, Center for Primary Care and Outcomes Research, Center for Policy, Outcomes and Prevention, Stanford University School of Medicine.
Lara Vogel, Email: lvogel@stanford.edu, Stanford Medical School.
Craig D. Newgard, Email: newgardc@ohsu.edu, Associate Professor Emergency Medicine, Director, Center for Policy and Research in Emergency Medicine, Oregon Health & Science University.
Jayanta Bhattacharya, Email: jay@stanford.edu, Associate Professor of Medicine (Center for Primary Care and Outcomes Research) and by courtesy in Health Research and Policy and Economics, Stanford University School of Medicine.
Ciaran S. Phibbs, Email: Ciaran.phibbs@va.gov, Health Economics Resource Center, Palo Alto VA Health Care System.
Bibliography
- 1.Web-Based Injury Statistics Query and Reporting System. Centers for Disease Control and Prevention National Center for Injury Prevention and Control; 2010. [Accessed December 21, 2012.]. http://www.cdc.gov/ncipc/wisqars. [Google Scholar]
- 2.Lorch SA, Myers S, Carr B. The regionalization of pediatric health care. Pediatrics. 2010 Dec;126(6):1182–1190. doi: 10.1542/peds.2010-1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 4.California Office of Statewide Health Planning and Development. [Accessed December 22, 2012.];Patient discharge data file documentation. 2010 http://www.oshpd.ca.gov/HID/Products/PatDischargeData/PublicDataSet/Doc/PD10docwapp.pdf.
- 5.US Bureau of the Census. State and County Quick Facts – California. 2011 http://quickfacts.census.gov/qfd/states/06000.html.
- 6.California Emergency Medical Services Authority. [Accessed November 1, 2012.];Trauma centers in California. 2008 http://www.emsa.ca.gov/systems/files/trauma/trma_ctr.pdf.
- 7.Wang NE, Saynina O, Kuntz-Duriseti K, Mahlow P, Wise PH. Variability in pediatric utilization of trauma facilities in California: 1999 to 2005. Ann Emerg Med. 2008 Dec;52(6):607–615. doi: 10.1016/j.annemergmed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. [Accessed November 1, 2012.];Recommended framework of E-code groupings for presenting injury mortality and morbidity data. 2011 Aug 10; http://www.cdc.gov/injury/wisqars/ecode_matrix.html.
- 9.United States Census Bureau. [Accessed March 28, 2013.];Metropolitan and Micropolitan Delineation Files. 2013 http://www.census.gov/population/metro/data/def.html.
- 10.Pracht EE, Tepas JJ, 3rd, Langland-Orban B, Simpson L, Pieper P, Flint LM. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg. 2008 Jan;43(1):212–221. doi: 10.1016/j.jpedsurg.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 11.POP-FACTS Database (Zip(Area)Level) 2010.
- 12.U.S. Department of Health and Human Services. [Accessed March 28, 2013.];The 2004 Health & Human Services Poverty Guidelines. 2004 http://aspe.hhs.gov/poverty/04poverty.shtml.
- 13.Phibbs CS, Luft HS. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995 Nov;52(4):532–542. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 14.SAS Institute. [Accessed December 19, 2012.];Zipcode Dataset. http://support.sas.com/rnd/datavisualization/mapsonline/html/misc.html.
- 15.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Boston: Boston College, Department of Economics; 2009. [Google Scholar]
- 16.Fleischman RJ, Mann NC, Wang NE, et al. The Use of ICD-9 Codes to Generate Injury Severity Score: The ICDPIC Mapping Procedure. Academic Emergency Medicine; 2012. In Press. [Google Scholar]
- 17.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989 Apr;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 18.MacKenzie EJ, Steinwachs DM, Shankar BS, Turney SZ. An ICD-9CM to AIS conversion table: development and application. Proc AAAM. 1986;30:135–151. [Google Scholar]
- 19.Glance LG, Osler TM, Mukamel DB, Meredith W, Wagner J, Dick AW. TMPM-ICD9: a trauma mortality prediction model based on ICD-9-CM codes. Ann Surg. 2009 Jun;249(6):1032–1039. doi: 10.1097/SLA.0b013e3181a38f28. [DOI] [PubMed] [Google Scholar]
- 20.Newhouse JP, McClellan M. Econometrics in outcomes research: the use of instrumental variables. Annu Rev Public Health. 1998;19:17–34. doi: 10.1146/annurev.publhealth.19.1.17. [DOI] [PubMed] [Google Scholar]
- 21.Newgard CD, Schmicker RH, Hedges JR, et al. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010 Mar;55(3):235–2463. e234. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Bureau of the Census. [Accessed December 21, 2012.];Profile of General Demographic Characteristics: 2000 - California. 2000 http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 23.Ochoa C, Chokshi N, Upperman JS, Jurkovich GJ, Ford HR. Prior studies comparing outcomes from trauma care at children’s hospitals versus adult hospitals. J Trauma. 2007 Dec;63(6 Suppl):S87–91. doi: 10.1097/TA.0b013e31815acc0f. discussion S92–85. [DOI] [PubMed] [Google Scholar]
- 24.Hulka F. Pediatric trauma systems: critical distinctions. J Trauma. 1999 Sep;47(3 Suppl):S85–89. doi: 10.1097/00005373-199909001-00019. [DOI] [PubMed] [Google Scholar]
- 25.Rutledge R, Smith CY, Azizkhank RG. A population-based multivariate analysis of the associat ion of county demographic and medical system factors with per capita pediatric trauma death rates in North Carolina. Ann Surg. 1994 Feb;219(2):205–210. doi: 10.1097/00000658-199402000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997 Mar;42(3):514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 27.Marcin JP, Schembri MS, He J, Romano PS. A population-based analysis of socioeconomic status and insurance status and their relationship with pediatric trauma hospitalization and mortality rates. Am J Public Health. 2003 Mar;93(3):461–466. doi: 10.2105/ajph.93.3.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010 Aug;17(8):809–812. doi: 10.1111/j.1553-2712.2010.00819.x. [DOI] [PubMed] [Google Scholar]
- 29.Rosen H, Saleh F, Lipsitz SR, Meara JG, Rogers SO., Jr Lack of insurance negatively affects trauma mortality in US children. J Pediatr Surg. 2009 Oct;44(10):1952–1957. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 30.Arroyo A, Wang N, Saynina O, JB, Wise P. The Association Between Insurance Status and Emergency Department Disposition of Injured California Children. Acad Emerg Med. 2012;19(5):541–551. doi: 10.1111/j.1553-2712.2012.01356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson W, Rimsza M. The effects of acces to pediatric care and insurance coverage on emergency department utilization. Pediatrics. 2004;(11):483–487. doi: 10.1542/peds.113.3.483. [DOI] [PubMed] [Google Scholar]
- 32.Osler TM, Vane DW, Tepas JJ, Rogers FB, Shackford SR, Badger GJ. Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J Trauma. 2001 Jan;50(1):96–101. doi: 10.1097/00005373-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Potoka DA, Schall LC, Ford HR. Improved functional outcome for severely injured children treated at pediatric trauma centers. J Trauma. 2001 Nov;51(5):824–832. doi: 10.1097/00005373-200111000-00002. discussion 832–824. [DOI] [PubMed] [Google Scholar]
- 34.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma. 2000 Aug;49(2):237–245. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Segui-Gomez M, Chang DC, Paidas CN, Jurkovich GJ, Mackenzie EJ, Rivara FP. Pediatric trauma care: an overview of pediatric trauma systems and their practices in 18 US states. J Pediatr Surg. 2003 Aug;38(8):1162–1169. doi: 10.1016/s0022-3468(03)00262-8. [DOI] [PubMed] [Google Scholar]
- 36.Densmore JC, Lim HJ, Oldham KT, Guice KS. Outcomes and delivery of care in pediatric injury. J Pediatr Surg. 2006 Jan;41(1):92–98. doi: 10.1016/j.jpedsurg.2005.10.013. discussion 92–98. [DOI] [PubMed] [Google Scholar]
- 37.Ciesla DJ, Pracht EE, Cha JY, Langland-Orban B. Geographic distribution of severely injured patients: Implications for trauma system development. J Trauma Acute Care Surg. 2012 May 2; doi: 10.1097/TA.0b013e3182509132. [DOI] [PubMed] [Google Scholar]
- 38.McConnell KJ, Newgard CD, Mullins RJ, Arthur M, Hedges JR. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005 Apr;40(2):435–457. doi: 10.1111/j.1475-6773.2005.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stylianos S, Ford HR. Outcomes in pediatric trauma care. Semin Pediatr Surg. 2008 May;17(2):110–115. doi: 10.1053/j.sempedsurg.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 40.Staiger DSJ. Instrumental Variables Regression with Weak Instruments. Econometrica. 1997;65:557–586. [Google Scholar]
- 41.Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007 Jan 17;297(3):278–285. doi: 10.1001/jama.297.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]