Abstract
Early-career academic cardiologists currently face unprecedented challenges that threaten a highly valued career path. A team consisting of early career professionals and senior leadership members of American College of Cardiology (ACC) completed this white paper to inform the cardiovascular medicine profession regarding the plight of early career cardiologists and to suggest possible solutions. This paper includes: (1) definition of categories of early career academic cardiologists, (2) general challenges to all categories and specific challenges to each category, (3) obstacles as identified by a survey of current early career members of the ACC, (4) major reasons for the failure of physician-scientists to receive funding from National Institute of Health/National Heart Lung and Blood Institute (NIH/NHLBI) career development grants, (5) potential solutions, and (6) a call to action with specific recommendations.
Keywords: Early Career Academic Cardiologist, Physician-Scientist, Clinician-Educator, Academic Medical Center
INTRODUCTION
The majority of advances in cardiovascular care emerge from academic medical centers (AMCs) through research, publication, and development of clinical protocols by physicians and scientists(1).Our ability to advance knowledge, to develop novel technologies/therapeutics, to educate trainees, and to provide quality care is currently in jeopardy due to increasingly challenging conditions placed on AMCs and early-career academic cardiologists. As heart disease remains the number one cause of death in the United States (2) and 40% of Americans will develop some form of cardiovascular disease by 2030 (3), academic cardiologists in conjunction with AMCs strive to continually improve cardiovascular care through discovery and teaching.
Early-career academic cardiologists, defined as those who are within 10 years of completion of a cardiology fellowship training program, often find themselves challenged to remain in academics and thus must consider a transition to non-academic practice. Many early-career cardiologists view a career in academics as an opportunity to make discoveries that may lead to new therapies or influence clinical practice in substantive ways. Others view it as an opportunity to educate and train the next generation of providers. Sadly, current uncertainties regarding the viability of an academic career are driving many early-career academic cardiologists away.
In light of these developments, the early-career professional section of the American College of Cardiology (ACC), along with senior leadership, initiated this manuscript to summarize challenges faced by early-career academic cardiologists, to present data on perceived obstacles, and to discuss potential solutions to these challenges and obstacles.
DEFINING THE ACADEMIC CARDIOLOGIST
Physician-Scientist
Physician-scientists provide direct patient care and conduct research as principal investigators (PIs). They formulate research hypotheses based on existing data and their experience in treating patients. They then test their hypotheses by means of basic, translational, or clinical research, culminating sometimes in intellectual property development. Responsibilities of these individuals include overseeing research, publishing results, and writing grants to obtain external funding. Physician-scientists are often expected to provide didactic lectures to medical students and to serve as the teaching attending for medical students and residents on hospital services. By participating in both clinical and research domains, physician-scientists provide a critical bridge to translate clinical observations into the realm of scientific discovery and to return new-found knowledge to direct patient care.
Scientist-Researcher
Scientist-researchers dedicate nearly 100% effort to research. While their investigative responsibilities are similar to those of a physician-scientist, scientist-researchers do not have clinical duties.
Clinician-Educator
Clinician-educators dedicate a significant amount of time to educational activities: participating in preceptorships, presenting didactic lectures to housestaff and students, and participating as instructors in formal coursework offered through an associated medical school and/or graduate medical education program. The relative distribution of effort among these activities for clinician-educators is predominantly clinical. More recently, preceptor and mentor roles have extended beyond the traditional medical trainee to include allied health professionals, such as physician assistants, nurse practitioners, and pharmacy students.
Clinician-Educator-Administrator
Clinician-Educator-Administrators have responsibilities in course administration, rotation administration, and clinical operations added to the role of clinician-educator. Administrative roles include program director, director of clinical cardiology, or medical school course director. Some may chair or co-chair institutional, regional, national, or international continuing medical education courses.
Pure Clinician
Pure clinicians have the primary role of providing direct patient care. Unlike the other types of academic cardiologist, pure clinicians are contracted to dedicate essentially 100% of their allotted effort to direct patient care. Pure clinicians who wish to maintain academic interests must do so outside of their allotted and expected clinical time, whereas other categories of academic cardiologist usually have defined protected time for academic pursuits.
CHALLENGES
Common challenges are summarized in Table-1 and specific challenges facing each category of early-career academic cardiologists are summarized in Table-2.
Table 1.
Common Challenges
| Traditional sources of funding have declined | |
|---|---|
| Federal | National Institutes of Health/National Heart and Lung and Blood Institute (NIH/NHLBI) |
| General Medical Education (GME) | |
| Industry | |
| Increasing number of PhDs competing for smaller available funding pool | |
Over-reliance on relative value units (RVU) discourages academic pursuits
| |
Trends in medicine and academia reduce available time for investigator-initiated academic pursuits
| |
Table 2.
Category Specific Challenges
| Physician-Scientist and Scientist-Researcher |
|
| Clinician-Educator and Clinician-Educator-Administrator |
|
| Pure-Clinicians |
|
Challenges Felt by Current Academic Leadership of ACC
Cuts in research support, pending cuts in graduate medical education (GME), and the decline in reimbursements for clinical activities have come together to create a “perfect storm” that threatens the future health and health care of our nation. These events also threaten early career investigators during this particularly vulnerable career phase. Academic medical centers are challenged by these cuts as well. Left unchecked, this present course will render our nation ill-equipped to meet our rapidly expanding healthcare needs. Further, it is already jeopardizing our nation’s longstanding predominance in health care research and innovation.
A career in biomedical discovery coupled with the practice of clinical medicine requires many years of preparation, often involving earning both MD and PhD degrees. As such, it is not uncommon for an academic cardiologist to assume a first faculty position in his/her late 30’s. New faculty often faces extended “dry spells,” while the numerous skills required for success in academia are still in development. Bright, ambitious, well-trained physicians – who seek to discover and advance the field – are sometimes unable to navigate this difficult phase of the academic career path. There is a lack of societal awareness and interest in fostering this career track, failing to recognize its importance to the future healthcare needs of our world. Future benefits to society through enhanced longevity, improved quality of life, economic growth, and tax revenues are at risk.
VIEW FROM THE GROUND
Survey Design
The ACC conducted an online survey of its early-career membership between September and October, 2013. Email survey invitations and three follow-up reminders were sent to 2,957 randomly selected individuals within this member group. Inclusion criteria included being within 10 years of fellowship completion and self-identification as an academic cardiologist. 218 out of the 324 responses met the inclusion criteria. The majority (87%) resided in the US, were male (71%), and completed training within the last five years (58%). Self-identified distribution of categories were as follows: scientist-researcher (1%); physician-scientist (8% at >75% research, 13% at 40–75% research, and 38% at < 40% research); clinician-educator (25%); and clinician-educator-administrator (15%). Whereas this survey resulted in a modest response rate, the ACC market survey team estimates that 7%-10% of the 8651 early career cardiologists within the ACC are academic cardiologists.
Results
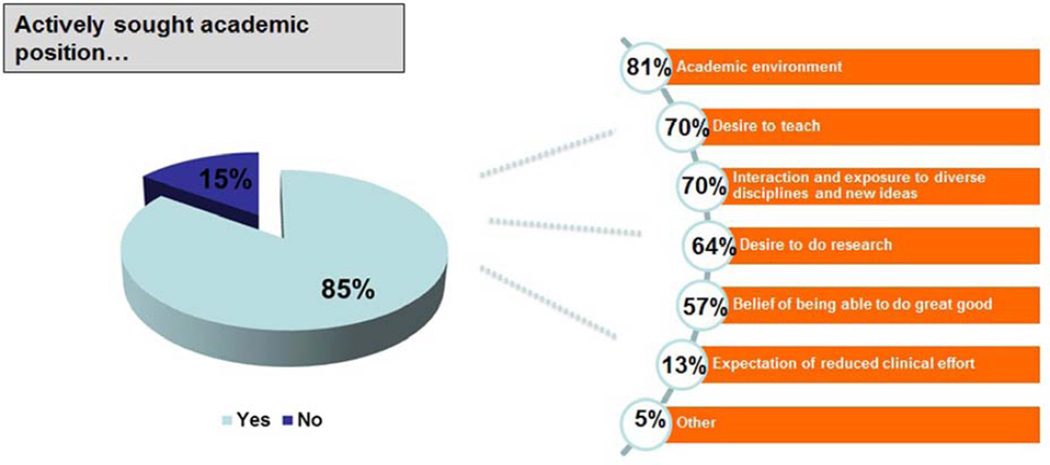
The majority (85%) of early career academic professionals actively sought an academic position (Figure 2). Top reasons included academic environment (81%), desire to teach (70%), and interaction/exposure to diverse disciplines and new ideas (70%). Approximately two-thirds (64%) indicated a desire to conduct research as a motivation to seek out an academic position. Furthermore, 57% of respondents stated the ability to do greater good as a reason for their choice. A smaller fraction of respondents (13%) indicated reduced clinical responsibility as a reason.
Figure 2. Reasons for Choosing Academic Cardiology.
A majority of the early academic cardiologists actively sought academic positions for altruistic reasons.
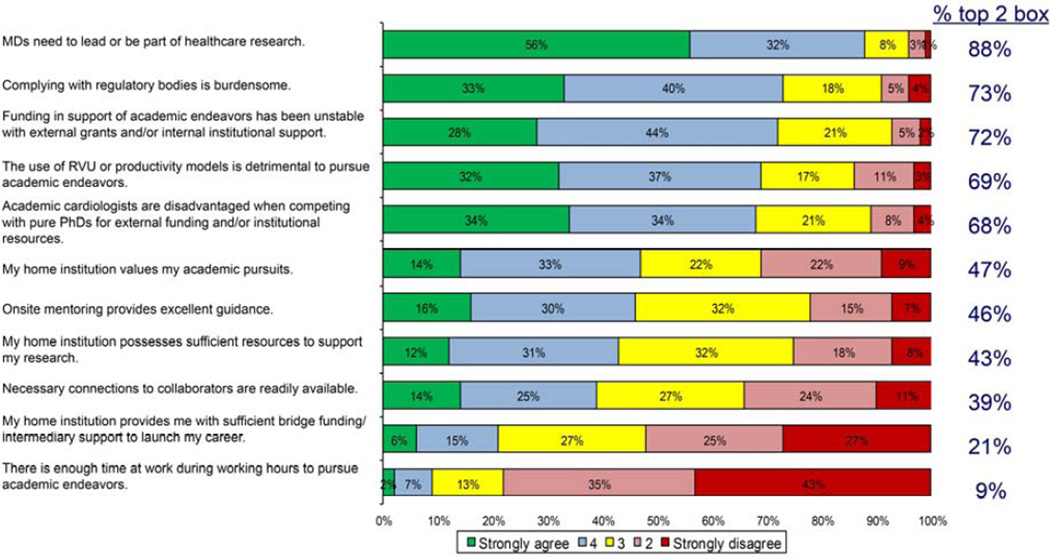
The vast majority of respondents (88%) strongly believed that physicians need to lead or be part of healthcare research. However, respondents identified multiple obstacles (Figure 3). A majority pointed to lack of time (78%), unstable funding (73%), burdensome regulatory compliance (72%), the disadvantage of competing against pure PhDs (69%), over-emphasis on relative value unit (RVU)-based metrics of performance which can discourage academic pursuits (62%), and insufficient support from the home institution (52%).
Figure 3. Perceived Obstacles to Academic Pursuits.
Survey identified complying with regulatory burden, unstable funding, detrimental use of RVUs, being disadvantaged when competing with PhDs, lack of good onsite mentoring, home institution lacking resources, lacking collaborators, lacking bridge funding, and insufficient time during work hours as major obstacles.
The vast majority (91%) reported insufficient external funding (defined as equivalent to NIH/NHLBI K08/K23 direct funding of $500,000), which is a major challenge for progression into a stable academic career. The distribution of external grant funding resembled a negative exponential curve: 80% (no funding), 11% ($5K-499K), 5% ($500K-999K), and 4% (>$1M). NIH grants accounted for approximately 43% of external funding for academic pursuits of early-career academic cardiologists (median: $117,500). Non-NIH grants accounted for a larger percentage of the external funding (median: $126,000).
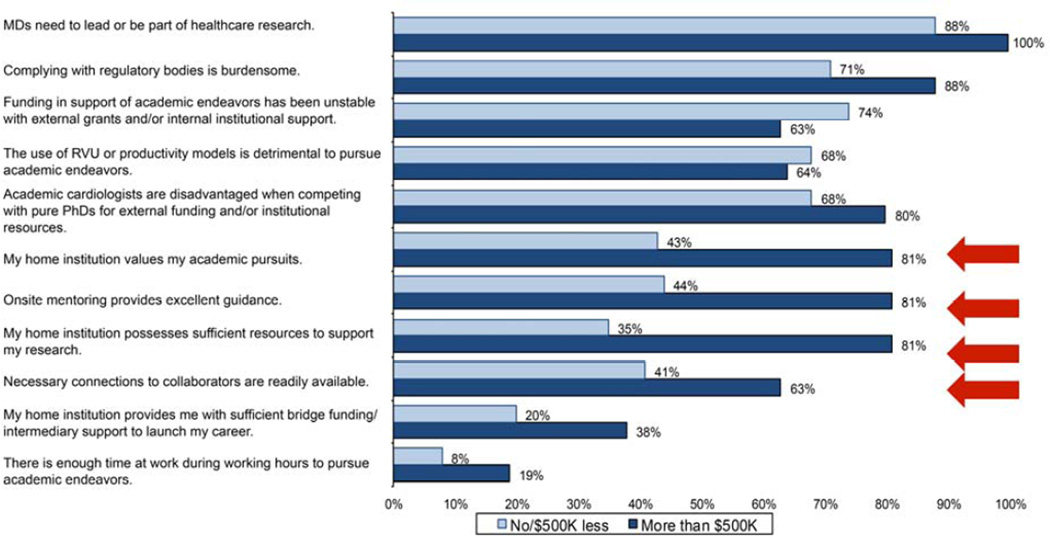
Correlation analyses revealed the following factors as associated with a greater ability to obtain >$500K of external funding (Figure 4): onsite mentoring, sufficient institutional resources, collaborative connections, and the perception that one’s institution values academic pursuits.
Figure 4. Factors Leading to Obtaining >$500K of External Grants (red arrows.
Spearman’s Rho analyses identified factors that correlated with success in obtaining >$500K of external grant funding. These factors include home institution placing value on academic pursuits, excellent onsite mentoring, home institution possessing sufficient resources, and readily available collaborators.
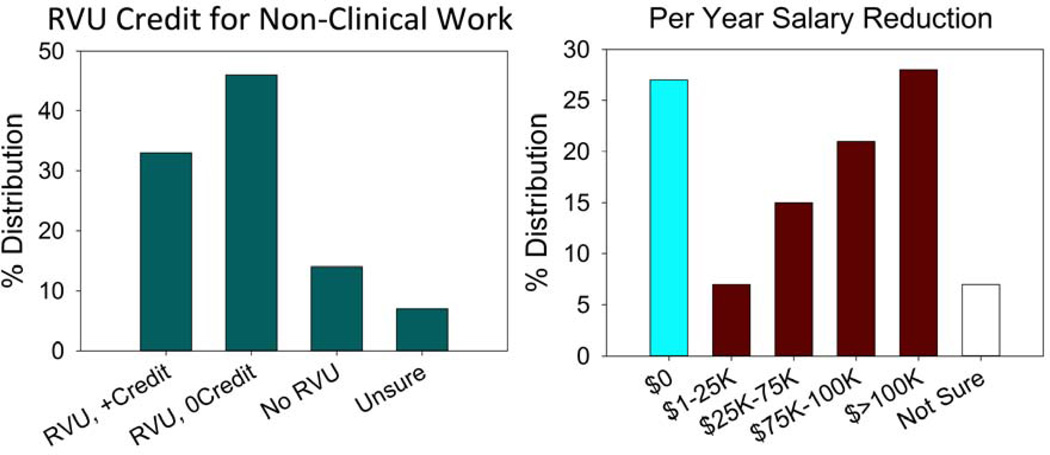
Economic difficulties experienced by the academic cardiologist included financial disincentives and RVU tracking (Figure 5). Most practitioners (71%) reported the reduction in pay required to pursue academic endeavors as a significant disincentive. Nearly half of respondents (49%) reported a reduction of ≥ $75,000 per year. The majority of academic practitioners (79%) reported that RVUs are tracked and nearly half (46%) did not receive RVU-like credit for academic endeavors. Clearly, this focus on clinical productivity leaves less time for two important motivators of the academic professional: research and teaching.
Figure 5. Financial Disincentives for Early-Career Academic Cardiologists.
(A) Early career members generally did not receive RVU credits for academic pursuits, and (B) took reductions in pay for pursuing academic cardiology.
Survey Conclusions
Tangible factors such as onsite mentoring, institutional commitment, and the availability of collaborators directly contribute to the success of early-career cardiologists. Thus, development of these resources where they do not exist, and preservation of them where they do, are essential. Interestingly, institutional value placed on academic pursuits also contributes to successful grant applications, demonstrating the need for recognition of non-RVU generating activities of early career academic cardiologists.
Our survey lends objective credence to the concern that the career path of academic cardiology is in peril and that early-stage faculty are particularly challenged. The NIH/NHLBI K-grants funding level of $500K is critical to providing dedicated research time, but does not cover research-related costs (e.g., equipment, personnel, reagents, animals, and clinical database access). Thus, we believe that the 91% of survey respondents who have not achieved this level of funding are challenged to emerge with success in the research arena. Moreover, the lack of institutional recognition of academic endeavors (e.g. RVU credit) and pay reductions further discourage early career members from continue to pursuit academic cardiology.
NIH/NHLBI CRITIQUE
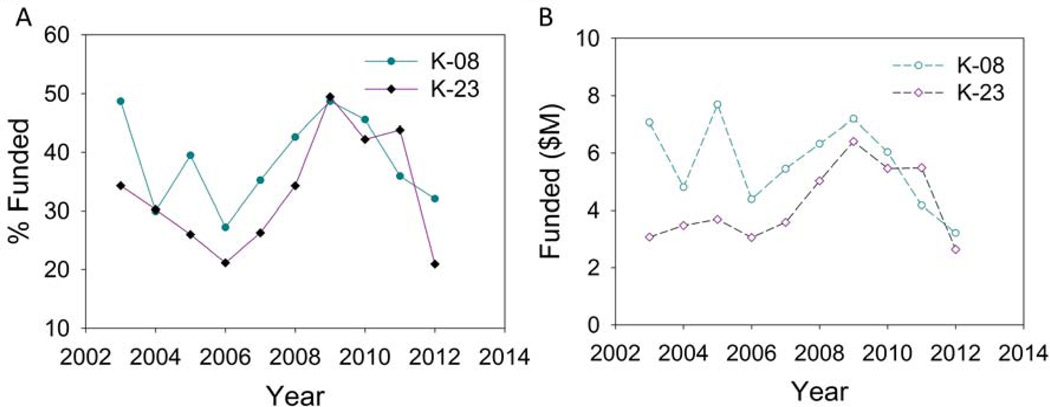
Despite decreases in total funding amount and award success percentage (Figure 6), NIH/NHLBI career development K08 (basic research) and K23 (clinical research) grants remain relatively obtainable. In 2012, the funding success rates were 32.1% and 20.9% for K08 and K23 respectively (4). Between 2007–2010, 49% of K08 grants were awarded to adult cardiology(5). Thus, NIH/NHLBI career development grants remain viable sources of grant support for early-career academic cardiologists. However, all K-grants are grouped together and awarded by their priority score without regard to sub-categories (i.e., K01, K02, K08, K12, K23, K24, K25, K99/R00); consequently, early-career academic cardiologists compete with more established applicants (e.g. mid-career K02). In this light, we have worked with NHLBI program officers and a past chairman of K-grants review study section to compile a list of major reasons for the failure of physician-scientists to receive funding (see Table 3).
Figure 6. NIH/NHLBI Funding of Career Development Grants by Year.
NHLBI funding of K08 (basic research) and K23 (clinical research) career development grants fluctuated from 2003–2012 in proposal success rate (A) and amount (B). Data were extracted from reference (4).
Table 3.
Top Reasons from NIH Official for K-Grant Failure
| Applicant appears to be inadequately prepared nor committed to research. The applicant did not demonstrate sufficient skill in the area of proposed research as seen by lack of prior first author publication and lack of valid preliminary data in the proposal. The applicant did not demonstrate commitment to research by lack of prior dedicated research time. Furthermore, the applicant seems to suddenly jump into the proposed research without indication of prior experience, preparation, or believable motivation. |
| Career development plan appears to be poorly designed. Being career development grant, reviewers expect to see career development plan that integrates well with research plan. Often, applicants fail to demonstrate how the proposed research can directly contribute to their career development. |
| Research proposal is poorly developed. Being early career, applicants have the tendency to propose projects that cannot plausibly be completed. Furthermore, research plans lack focus; therefore, reviewers doubt that meaningful results can be accomplished for both advancement of science and career development. |
| Mentor does not appear to have the ability to help the mentee. Mentor not having NIH R01 level type of funding raises doubts about his/her ability to financially help the mentee if the research encounters difficulties or needing new methods. Mentor’s letter may not match applicant’s career development plans; consequently, reviewers interpret this mismatch as mentor being unwilling or unable to commit the necessary effort to help the mentee. Sometimes, the mentor does not demonstrate having expertise in the area of proposed research; thus, mentor will not be able to help. Since mentoring is an extraordinary crucial part of career development, perception of an inadequate mentor will doom the proposal even all other sections are excellent. |
Successful K-grants provide robustly positive impact on the development of early career cardiologists. These grants require institutions to allocate 75% dedicated research effort. This dedicated research time provides the early-career professional with time to develop critical skills and to acquire preliminary observations and reagents. In other words, these career development awards are a pivotal juncture in the emergence of a cardiologist-scientist.
POTENTIAL SOLUTIONS
Improving Fellowship Training
We must better prepare fellows to succeed early in their careers. However, changes in fellowship training needed to meet this goal must occur without extending the current fellowship duration of 3–5 years.
Allocating dedicated research time during fellowship training correlates with the decision of fellows to pursue an academic career (6–10) and allows for the completion of research resulting in publication during fellowship (6–10). The NIH/NHLBI’s top reasons for failure to obtain grants (Table-3) emphasize the need for fellows to be better prepared. This preparation includes proposal writing, proficiency in specialized research skills (e.g., basic, clinical, and translational research techniques), and completion of transferable products (e.g. novel reagents). Inherent in the ability to train competitive fellows is dedicated research time.
Mentorship is a critical part of all training programs (7, 8, 10, 11), and outstanding mentors should be acknowledged and rewarded by institutional leadership. The NIH/NHLBI critique illustrates that the quality of mentorship needs to improve. Protected time for the mentor and credit for successful mentoring will help create a strong group of future mentors.
Opportunities for education on the broader range of skills pertinent to the academic practice should be expanded. Fellows must be adept at delivering cost-effective care with attention to error prevention(12). Furthermore, department chairs, program directors, and other clinical leaders should educate fellows on the details of their specific supervisory functions (e.g. department, lab). As time constraints of fellowship training will not allow education of all fellows in all of these areas, programs must provide flexibility in aspects of their training program to allow for acquisition of specific skills needed for given career paths.
Fellows choosing a clinician-educator track need formal training in education to navigate the complexities of curriculum development, educational assessment, and accreditation regulations. Training in educational methodology and mentorship are critical for those striving for excellence as an educator. Training in educational research will help clinician educators produce scholarly work related to their teaching effort and contribute to their understanding of best practices in medical education.
Developing Novel Partnerships and Alternative Funding Sources
Partnership between university systems and clinical entities can provide stability during early career years. Under this type of partnership, a university system supports a portion of salary dedicated to academic pursuits while the clinical entity provides support for effort dedicated to patient care. Any salary support for the academic cardiologist derived from external grants is counted as salary savings to the university system and then re-applied toward the academic cardiologist’s research. This partnership provides stability and amplifies the effect of external grants. This type of partnership, successfully implemented at Texas A&M University partnering with Baylor Scott & White Healthcare, provides upfront stability for roughly five years.
Creating partnerships with institutions hosting a Clinical and Translational Science Award (CTSA) from the NIH can be helpful. A portion of CTSA funds is used to support the training of early stage investigators, including KL2 Career Development Awards. Similar to NIH-K awards, these awards mandate 75% protected time for research and related career development activities and typically provide approximately $25,000/year in research support. These awards often include a didactic component and provide for coursework towards a master’s degree in clinical investigation.
Another alternative source for funding are investigator initiated trials (IIT), through which uses for newer drugs or new uses for established agents (13) are investigated. Establishing training and research partnerships with pharmaceutical companies outside of IITs is also possible. For example, Rutgers Pharmaceutical Industry Fellowship Program involves participation of 17 pharmaceutical companies to fund 1–2 years of training in research and advocacy for those who hold doctorates in pharmacology(14). However, pharmaceutical partnerships require special focus to ensure that conflicts of interest, or the appearance thereof, do not emerge.
Access to key personnel, information regarding funding opportunities, and knowledge of resources are crucial to obtaining external grants. Thus, creation of regional network of collaborators, mentors, and networks of sharable resources can enhance access to early-career professionals. Electronic media allows for remote mentoring. Regional sharing of resources allows for experiments to occur when the home institution lacks the capability of conducting experiments locally. The ACC is well positioned to facilitate these efforts.
The Early Career Professional section of the ACC has initiated a College-wide mentorship program. Additionally, a new partnership between the ACC and infoEd (https://acc.spin.infoedglobal.com/Home/GridResults) has established a searchable database of funding resources, providing members access to information that would otherwise be difficult to locate.
Seeking Policy Changes
We must better educate the public, elected representatives, and regulatory officials regarding the critical importance of medical education and research(15). The reduction in deaths due to coronary artery disease from ~470/100,000 per year in the 1960s to ~150/100,000 per year in 2010 (1) is an excellent example of the benefit achieved by cardiovascular innovation. Despite this, cardiovascular disease remains the leading cause of death in the US (2) and heart failure is a progressive disease with 5-year mortality greater than most cancers(16–18). Clearly, more research is needed. Increased awareness is critical in enhancing societal investment in research to tackle the grave issues.
A major reason for declining societal investment in medical education (GME) has been our failure to demonstrate the value that AMCs provide to society. We must reinforce to the public that AMCs perform critical functions: training the next generation of physicians, hosting the majority of medical advances, treating the most vulnerable and challenging populations (e.g. those who require multi-disciplinary care, those with advanced diseases not treatable elsewhere, and those who are indigent). Furthermore, increased GME funding is critical to ensure that AMCs are prepared for the increases in patients accessing our healthcare system as a result of the Affordable Care Act.
Advocacy requires direct involvement. Our role as academic cardiologists must be explained and justified to the public. We must do a better job of determining the return on societal investment and communicating that information. This public education needs to begin at the regional and state level. Ultimately though, to best effect policy change, these efforts must be coordinated at the national level.
The cost for caring of cardiovascular disease patients has risen significantly (19, 20). We must contain this growth in costs and demonstrate to the public that we are consciously working to trim expenditures. Finding efficient ways to treat patients and reduce expenditures can bend the cost growth curve. Actual savings may translate into broader overall support for development of physician-investigators dedicated to enhancing our future.
CALL TO ACTION
We are witnessing a convergence of events that threaten the existence of the academic cardiologist career path. Traditional mechanisms of research support and investment in education are declining. Competition for funding continues to increase. In response, some institutions are devaluing the academic enterprise. Our survey and NIH/NLHBI critique suggest strongly that early-career academic cardiologists are facing career-threatening challenges, arguably more so than ever. Failure to renew the pipeline of academic cardiologists threatens our ability to meet the healthcare needs of the future. Thus, we call on the ACC and our colleague-members to act on the following specifics (Table-4) for the good of society and the preservation of our profession.
Table 4.
Call to Action Specifics
ACC Leadership:
|
ACC Advocacy:
|
Division Chiefs and Academic Leadership:
|
Program Directors:
|
Established Investigators:
|
Trainees:
|
All Cardiologists:
|
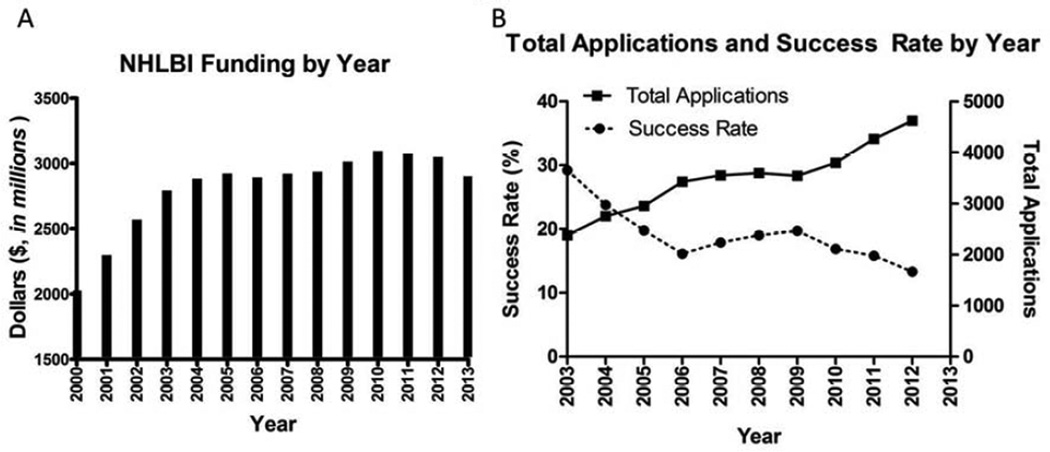
Figure 1. NIH/NHLBI Funding and Proposal Success Rate by Year.
(A) NHLBI funding grew rapidly from 2000 to 2005, grew again by smaller increments from 2008 to 2010, and declined steadily since 2010. (B) NHLBI proposal success rates have declined from 29.2% in 2003 to 13.3% in 2012. Data were extracted from references (21, 22).
ACKNOWLEDGEMENTS
This effort was supported in part by ACC, NIH/K23HL11660 to BRL, and NIH/K08HL114877 to CWT.
Abbreviations
- ACC
American College of Cardiology
- AHA
American Heart Association
- AMC
Academic Medical Center
- CTSA
Clinical and Translational Science Awards
- GME
General Medical Education
- IIT
Investigator Initiated Trials
- NHLBI
National Heart Lung and Blood Institute
- NIH
National Institutes of Health
- PI
Principal Investigator
- RVU
Relative Value Unit
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There is no industry relationship to disclose for the work in this manuscript.
References
- 1.Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366:54–63. doi: 10.1056/NEJMra1112570. [DOI] [PubMed] [Google Scholar]
- 2.Sherry L, Murphy JX, Kenneth D, Kochanek MA. Deaths: Final Data for 2010. National Vital Statistics Reports: U.S. Department of Health and Human Services. 2013:1–118. [PubMed] [Google Scholar]
- 3.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 4.(OSAR) OoSAaR, editor. NIH. Table #204, NIH Career Development (K) Grants: Competing Applications, Awards, Success Rates and Total Funding by NIH Institutes. NIH; 2013. [Google Scholar]
- 5.Scott JD, Carlson DE. K08 and K99 cardiovascular training: comparisons and trends among current awardees. Circ Res. 2012;110:910–914. doi: 10.1161/RES.0b013e3182533291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhattacharya SD, Williams JB, de la Fuente SG, Kuo PC, Seigler HF. Does protected research time during general surgery training contribute to graduates' career choice? Am Surg. 2011;77:907–910. [PMC free article] [PubMed] [Google Scholar]
- 7.Borges NJ, Navarro AM, Grover A, Hoban JD. How, when, and why do physicians choose careers in academic medicine? A literature review. Acad Med. 2010;85:680–686. doi: 10.1097/ACM.0b013e3181d29cb9. [DOI] [PubMed] [Google Scholar]
- 8.Horn L, Koehler E, Gilbert J, Johnson DH. Factors associated with the career choices of hematology and medical oncology fellows trained at academic institutions in the United States. J Clin Oncol. 2011;29:3932–3938. doi: 10.1200/JCO.2011.35.8663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lyle JL, Vandergrift JL, Hinkel JM, Lepisto EM, Cortazzo KA, Sherman S, et al. Influential factors for post-fellowship career decision-making: an NCCN survey. J Natl Compr Canc Netw. 2012;10:969–974. doi: 10.6004/jnccn.2012.0101. [DOI] [PubMed] [Google Scholar]
- 10.Straus SE, Straus C, Tzanetos K. Career choice in academic medicine: systematic review. J Gen Intern Med. 2006;21:1222–1229. doi: 10.1111/j.1525-1497.2006.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuster V, van der Zee S, Elmariah S, Bonow RO. Academic careers in cardiovascular medicine. Circulation. 2009;119:754–760. doi: 10.1161/CIRCULATIONAHA.108.792564. [DOI] [PubMed] [Google Scholar]
- 12.Crosson FJ, Leu J, Roemer BM, Ross MN. Gaps in residency training should be addressed to better prepare doctors for a twenty-first-century delivery system. Health Aff (Millwood) 2011;30:2142–2148. doi: 10.1377/hlthaff.2011.0184. [DOI] [PubMed] [Google Scholar]
- 13.Gupta SK, Nayak RP. An insight into the emerging role of regional medical advisor in the pharmaceutical industry. Perspect Clin Res. 2013;4:186–190. doi: 10.4103/2229-3485.115386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutgers IfPIF. Rutgers Institute for Pharmaceutical Industry Fellowships. Rutgers Institute for Pharmaceutical Industry Fellowships; 2013. [Google Scholar]
- 15.Laslett LJ, Alagona P, Jr, Clark BA, 3rd, Drozda JP, Jr, Saldivar F, Wilson SR, et al. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J Am Coll Cardiol. 2012;60:S1–S49. doi: 10.1016/j.jacc.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Askoxylakis V, Thieke C, Pleger ST, Most P, Tanner J, Lindel K, et al. Long-term survival of cancer patients compared to heart failure and stroke: a systematic review. BMC Cancer. 2010;10:105. doi: 10.1186/1471-2407-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart S, Ekman I, Ekman T, Oden A, Rosengren A. Population impact of heart failure and the most common forms of cancer: a study of 1 162 309 hospital cases in Sweden (1988 to 2004) Circ Cardiovasc Qual Outcomes. 2010;3:573–580. doi: 10.1161/CIRCOUTCOMES.110.957571. [DOI] [PubMed] [Google Scholar]
- 18.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More 'malignant' than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001;3:315–322. doi: 10.1016/s1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 19.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circ Cardiovasc Qual Outcomes. 2012;5:31–36. doi: 10.1161/CIRCOUTCOMES.111.961813. [DOI] [PubMed] [Google Scholar]
- 20.Miller G, Hughes-Cromwick P, Roehrig C. National spending on cardiovascular disease, 1996–2008. J Am Coll Cardiol. 2011;58:2017–2019. doi: 10.1016/j.jacc.2011.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NIH. Table #206, Competing Applications, Awards, Success Rate and Total Funding by Application Type, NIH Institutes/Centers and Activity Code Fiscal Years* 2003–2012. Office of Statistical Analysis and Reporting. 2013 [Google Scholar]
- 22.NIH_Office_of_Budget, editor. NIH-Office_of_Budget. Actual Obligations By IC, FY 2000 - FY2012. Spending History by Institute: National Institutes of Health; 2013. [Google Scholar]
- 23.NIH. National Institutes of Health (NIH) Sequestration Operating Plan for FY2013. National Institutes of Health (NIH); 2013. [Google Scholar]
- 24.FASEB. BUDGET CUTS REDUCE BIOMEDICAL RESEARCH. Federation of American Societies for Experimental Biology. 2013 [Google Scholar]
- 25.Dower C. Health Policy Brief: Graduate Medical Education. Health Affairs: Robert Wood Johnson Foundation. 2012 [Google Scholar]
- 26.Association AH. FactSheet - Graduate Medical Education. American Hospital Assocation Fact Sheet: American Hospital Association. 2013 [Google Scholar]
- 27.Dower C. Graduate Medical Education. A debate continues over the size and scope of federal subsidies to support residency training of the nation’s physicians. Health Affairs: Robert Wood Johnson Foundation. 2012 [Google Scholar]
- 28.Campbell EG. The future of research funding in academic medicine. N Engl J Med. 2009;360:1482–1483. doi: 10.1056/NEJMp0900132. [DOI] [PubMed] [Google Scholar]
- 29.Dorsey ER, de Roulet J, Thompson JP, Reminick JI, Thai A, White-Stellato Z, et al. Funding of US biomedical research, 2003–2008. JAMA. 2010;303:137–143. doi: 10.1001/jama.2009.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pammolli F, Magazzini L, Riccaboni M. The productivity crisis in pharmaceutical R&D. Nat Rev Drug Discov. 2011;10:428–438. doi: 10.1038/nrd3405. [DOI] [PubMed] [Google Scholar]
- 31.Cyranoski D, Gilbert N, Ledford H, Nayar A, Yahia M. Education: The PhD factory. Nature. 2011;472:276–279. doi: 10.1038/472276a. [DOI] [PubMed] [Google Scholar]
- 32.Fiegener MK. In: Science and Engineering Doctorate Awards: 2009–2010. Statistics NCfSaE, editor. National Science Foundation; 2013. [Google Scholar]
- 33.Harold JG, Bass TA, Bashore TM, Brindis RG, Brush JE, Jr, Burke JA, et al. ACCF/AHA/SCAI 2013 update of the clinical competence statement on coronary artery interventional procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training (Writing Committee to Revise the 2007 Clinical Competence Statement on Cardiac Interventional Procedures) J Am Coll Cardiol. 2013;62:357–396. doi: 10.1016/j.jacc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Bonow RO, Smith SC., Jr Cardiovascular manpower: the looming crisis. Circulation. 2004;109:817–820. doi: 10.1161/01.CIR.0000119801.38445.8F. [DOI] [PubMed] [Google Scholar]
- 35.Fye WB. Introduction: The origins and implications of a growing shortage of cardiologists. J Am Coll Cardiol. 2004;44:221–232. [PubMed] [Google Scholar]