Abstract
Healthcare-associated pneumonia (HCAP) is a new concept of pneumonia proposed by the American Thoracic Society/Infectious Diseases Society of America in 2005. This category is located between community-acquired pneumonia and hospital-acquired pneumonia with respect to the characteristics of the causative pathogens and mortality, and primarily targets elderly patients in healthcare facilities. Aspiration among such patients is recognized to be a primary mechanism for the development of pneumonia, particularly since the HCAP guidelines were published. However, it is difficult to manage patients with aspiration pneumonia because the definition of the condition is unclear, and the treatment is associated with ethical aspects. This review focused on the definition, prevalence and role of aspiration pneumonia as a prognostic factor in published studies of HCAP and attempted to identify problems associated with the concept of aspiration pneumonia.
Keywords: healthcare-associated pneumonia, aspiration pneumonia, elderly, diagnosis
A new classification of pneumonia, healthcare-associated pneumonia (HCAP), was introduced by the American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) in 2005 [1]. The definition of HCAP includes hospitalization for two days or more within the preceding 90 days, residence in a nursing home or extended care facility, the use of home infusion therapy (including antibiotics), receipt of chronic dialysis within 30 days, home wound care and a history of infection with a multidrug-resistant pathogen in a family member. Patients with HCAP are characterized by an older age, increased risk factors for infection with drug-resistant pathogens and poorer prognosis compared to those with community-acquired pneumonia (CAP) [2]. Consequently, guidelines recommend the use of empiric broad-spectrum antibiotic therapy in these patients. However, most clinicians do not actually choose broad-spectrum antibiotics in cases of HCAP [3]. In fact, the use of guideline-concordant therapy does not improve the prognosis, and host factors, rather than the presence of drug-resistant pathogens, appear to influence the prognosis [4–7]. Previous studies have demonstrated aspiration pneumonia to be a host factor associated with mortality in patients with HCAP [8–11]. Aspiration pneumonia is defined as the misdirection of oropharyngeal or gastric contents into the larynx and lower respiratory tract [12,13]. Although initial clinical reports focused on aspiration pneumonia resulting from accidental exogenous factors, such as the ingestion of oil [14–16], the number of studies regarding aspiration pneumonia due to the aspiration of oropharyngeal secretions in the elderly has increased as the population ages, especially in developed countries [13, 17–22]. However, the definition of aspiration pneumonia remains vague and unclear, which is likely to complicate clinical research regarding the prognosis of pneumonia. We therefore reviewed previously published papers focusing on aspiration pneumonia among patients with HCAP in order to clarify the variability in the definition of aspiration pneumonia, as well as the prevalence of the condition and its impact on the prognosis. In addition, we discuss the meaning and purpose of a diagnosis of aspiration pneumonia according to guidelines for pneumonia.
METHODS and RESULTS
Search Procedure
A search of the English-language literature published from January 2005 to September 2013 was made using PubMed with the phrase ‘healthcare-associated pneumonia’ (accessed on September 20, 2013). Of the 285 articles identified during the search, 31 manuscripts focusing on HCAP or nursing and healthcare-associated pneumonia (NHCAP) contained information about aspiration pneumonia (five prospective observational studies [10, 23–26], 12 retrospective observational studies [4, 8, 27–36] and 14 reviews [37–50]). Furthermore, the 14 reviews included two studies of aspiration pneumonia among patients with HCAP (one prospective observational study [51], one retrospective observational study [52]) that did not overlap with the above prospective or retrospective observational studies. Consequently, 19 studies, including six prospective studies [10, 23–26, 51] and 13 retrospective studies [4, 8, 27–36, 52], referring to aspiration pneumonia in the manuscript were found. Of these 19 studies, 13 (six prospective observational studies [10, 23–26, 51] and seven retrospective observational studies [8, 27–30, 33, 52]) defined aspiration pneumonia; thus, 13 studies were ultimately included in this review. The remaining six studies [4, 31, 32, 34–36] did not define aspiration pneumonia, although they described the term ‘aspiration pneumonia’ in the patient characteristics section in the manuscript. The term NHCAP was proposed by the Japanese Respiratory Society in 2011 in order to adjust the concept of HCAP to the Japanese medical and nursing care insurance system [53]. In this study, we regarded NHCAP to be the same classification as HCAP because the subject characteristics were almost identical between the two categories.
Definition of aspiration pneumonia
The definition of aspiration pneumonia in the enrolled studies varied depending on the author, except for some studies that cited a previously published definition (Table 1). No studies prospectively screened risks for aspiration or performed instrumental swallowing evaluations, such as videoendoscopic or videofluorographic swallowing tests, in all patients, although most of the studies included swallowing dysfunction or dysphagia as a primary component of the definition of aspiration. The definition in three studies included radiological evidence of involvement in a dependent pulmonary segment [25, 26, 51], while one study required evidence of gravity-dependent opacity on chest CT [8]. The remaining studies did not include specific radiological features in the definition of aspiration pneumonia. Falcon and colleagues focused on the bacteriological findings in addition to the clinical characteristics [38].
Table 1.
Definition of aspiration pneumonia among studies of healthcare-associated pneumonia
| Study | Country | Design | Patients | Definition of aspiration pneumonia or risk factors for aspiration pneumonia |
|---|---|---|---|---|
| Carratalà J, et al. 200748 | Spain | prospective | CAP/HCAP | Patients with risk factors such as compromised consciousness, altered gag reflex, dysphagia, severe periodontal disease, putrid sputum and radiographic evidence of involvement of a dependent pulmonary segment or necrotizing pneumonia. |
| Garcia-Vidal C, et al. 201123 | Spain | prospective | CAP/HCAP | Same as Carratalà J, et al. 2007. |
| Simonetti A, et al. 201222 | Spain | prospective | CAP/HCAP | Same as Garcia-Vidal C, et al. 2011. |
| Giannella M, et al. 201221 | Spain | prospective | CAP/HCAP/HAP | Altered consciousness, altered gag reflex, dysphagia, severe periodontal disease or putrid sputum. |
| Falcone M, et al. 201210 | Italy | prospective | HCAP | Patients with risk factors such as compromised consciousness, altered gag reflex, dysphagia, severe periodontal disease, putrid sputum or necrotizing pneumonia in absence of positive respiratory specimen cultures. |
| Fukuyama H, et al. 201320 | Japan | prospective | CAP/NHCAP | Patients with apparent aspiration, a condition in which aspiration is strongly expected or the existence of an abnormal swallowing function or dysphagia. Suspected patients were assessed using water swallowing tests or VE for the purpose of evaluating the swallowing function. |
| Shindo Y, et al. 200949 | Japan | retrospective | CAP/HCAP | Probable aspiration was defined as any witnessed aspiration before hospital admission or aspiration confirmed by fluid-drinking test on hospital admission. |
| Miyashita N, et al. 201230 | Japan | retrospective | CAP/NHCAP | Pneumonia in a patient with a predisposition to aspiration because of dysphagia or a swallowing disorder. The swallowing function was assessed using the water-swallowing test, repetitive saliva-swallowing test, simple swallowing provocation test and VF. When the swallowing function was not assessed using these examinations, the presence of overt symptoms of dysphagia or a medical history of aspiration was determined to a swallowing disorder in the patient. |
| Ishida T, et al. 201227 | Japan | retrospective | CAP/NHCAP | Trained nurses checked the following factors three times: a past history of aspiration, the occurrence of a choking sensation with a wet cough during meals and the presence of massive fur on the tongue. If at least one factor was identified, the patient was judged to have a risk of aspiration and the swallowing function was assessed using the water swallowing test, repetitive saliva swallowing test, VE and VF. |
| Miyashita N, et al. 201326 | Japan | retrospective | NHCAP | Same as Miyashita N, et al. 2012. |
| Oshitani Y, et al. 201325 | Japan | retrospective | CAP/NHCAP | Involvement of aspiration was defined as dysphagia or aspiration confirmed or strongly suspected. |
| Komiya K, et al. 20138 | Japan | retrospective | CAP/HCAP | Patients with both risk factors for aspiration and evidence of gravity-dependent opacity on chest CT. |
| Nakagawa N, et al. 201324 | Japan | retrospective | CAP/NHCAP | Aspiration was recorded when witnessed by a patient’s family member or care staff member before the onset of pneumonia and confirmed by a water swallowing test or swallowing test using a laryngoscope. |
Abbreviations: CAP = community-acquired pneumonia; HCAP = healthcare-associated pneumonia; NHCAP=nursing and healthcare-associated pneumonia; VE = videoendocsopy; VF = videofluorography
Prevalence of aspiration pneumonia
The overall prevalence of aspiration pneumonia exhibited a wide range, from 6.1% [51] to 53.2% [28], among the studies (Table 2). The rate of patients diagnosed with aspiration pneumonia in Japan tended to be higher than that reported in European countries. Although some individual reports included different definitions, HCAP and NHCAP comprehensively had a higher prevalence than CAP in these studies.
Table 2.
Prevalence and role of aspiration pneumonia as a prognostic factor among studies defining aspiration pneumonia in patients with CAP and (N)HCAP
| Study | Ratio in CAP/(N)HCAP | Ratio in CAP | Ratio in (N)HCAP | Crude mortality or adjusted OR or HR |
|---|---|---|---|---|
| Carratalà J, et al. 200748 | 44/727 (6.1%) | 18/601 (18%) | 26/126 (20.6%) | n.a. |
| Garcia-Vidal C, et al. 201123 | 162/2153 (7.5%) | 91/1668 (5.5%) | 71/485 (14.6%) | n.a. |
| Simonetti A, et al. 201222 | 123/1593 (7.7%) | 68/1274 (5.3%) | 55/319 (17.2%) | no significance? |
| Giannella M, et al. 201221 | 262/898 (29.2%) | 108/591 (18.3%) | 154/307 (50.2%) | OR 0.87 (0.48–1.57) p=0.66 for in-hospital mortality |
| Falcone M, et al. 201210 | n.a. | n.a. | 55/217 (25.3%) | OR 4.94 (1.71–14.27) as in-hospital mortality with significance |
| Fukuyama H, et al. 201320 | 129/306 (42.2%) | 7/114 (6.1%) | 122/192 (63.5%) | 14.8% vs 4.3% 30 day-mortality |
| Shindo Y, et al. 200949 | 124/371 (33.4%) | 42/230 (18.3%) | 82/141 (58.2%) | n.a. |
| Miyashita N, et al. 201230 | 492/1385 (35.5%) | 122/786 (15.5%) | 370/599 (61.8%) | no significance? |
| Ishida T, et al. 201227 | 376/893 (42.1%) | 96/451 (21.3%) | 280/442 (63.3%) | n.a. |
| Miyashita N, et al. 201326 | n.a. | n.a. | 370/599 (61%) | n.a. |
| Oshitani Y, et al. 201325 | 382/718 (53.2%) | 24/241 (10%) | 358/477 (75.1%) | no significance in NHCAP |
| Komiya K, et al. 20138 | 116/637 (18.2%) | n.a. | n.a. | HR 5.690 (2.306–14.040) <0.001 at 30 days |
| Nakagawa N, et al. 201324 | 484/960 (50.4%) | 46/373 (12.3%) | 438/587 (74.6%) | 72/484 (14.9%) vs 28/476 (5.9%) during hospitalization |
Abbreviations: CAP = community-acquired pneumonia; HCAP = healthcare-associated pneumonia; HR = hazard ratio; n.a. = not assessed; NHCAP=nursing and healthcare-associated pneumonia; OR = odds ratio
Role of aspiration pneumonia as a prognostic factor
The mortality of patients with aspiration pneumonia was higher than that of those without (Table 2). Aspiration pneumonia was found to be a significant prognostic factor in multivariable analyses by Falcone et al. [38] and Komiya et al. [8] Falcone and colleagues demonstrated that a SOFA score of more than 5 [OR 5.62 (95% CI 1.89–16.65)], residence in a long-term facility [8.69 (1.63–46.42)], hospitalization within the previous six months [15.07 (1.87–121.55)] and the presence of pleural effusion [4.90 (1.66–14.47)] were significantly associated with inhospital mortality, while Komiya and colleagues showed that a high level of C-reactive protein [HR 1.048 (95% CI 1.011–1.086)] and decreased PaO2/FIO2 [1.003 (1.000–1.007)] were significantly associated with the risk of 30-day mortality in the same model [8, 38]. Treatment failure due to the presence of drug-resistant pathogens was not associated with the prognosis in the latter analysis [8], whereas the former study demonstrated that the use of empirical broad-spectrum therapy significantly improved the prognosis [38].
In contrast, studies by Giannella et al. [24] and Ohitani et al. [28] reported that aspiration pneumonia was not associated with mortality in their multivariate analyses. The Charlson comorbidity index [OR 1.13 (95%CI 1.05–1.22)], dyspnea [2.59 (1.26–5.33)], an altered mental status [4.24 (2.55–7.04)] and the presence of multilobar infiltrates [2.96 (1.94–4.52] were primarily associated with in-hospital mortality, while diabetes [2.39 (1.24–4.62)], hypoalbuminemia [2.77 (1.43–5.35)], a high A-DROP score [1.93 (1.10–3.38)] and findings of extensive pneumonia [2.54 (1.42–4.55)] were associated with mortality within 30 days after admission [24, 28].
DISCUSSION
Why is it difficult to define aspiration pneumonia?
Aspiration is a general mechanism underlying the development of pneumonia associated with inhalation [54]. Even young healthy individuals aspirate oral secretions, particularly during sleep [55]. If the volume of aspirated fluid is large or the defense mechanism is immunologically or medicophysically compromised, aspiration pneumonia can occur [56]. It is difficult to objectively estimate the incidence of this phenomenon, and the swallowing function can change before and after admission and during hospitalization. Hirose and colleagues demonstrated that some patients with confirmed severe swallowing dysfunction on admission have the potential to improve their swallowing function during oral intake [57]. This review revealed that patients with CAP or HCAP in Japan have a higher rate of aspiration pneumonia than those in other countries. One of possible reasons for this discrepancy is likely differences in the evaluation and diagnosis of patients with this condition, and the diagnostic tests are easily available in Japan [58].
Risk factors for aspiration pneumonia
Dysphagia commonly occurs as a result of cerebral vascular disease or degenerative diseases of the central nervous system, such as Alzheimer’s or Parkinson’s disease [59,60]. Nakagawa and colleagues investigated the cough reflex and swallowing function in patients suffering from stroke who were followed for one year [59]. While no patients without an impaired cough reflex or swallowing function developed pneumonia, approximately one quarter of the patients with an abnormal cough reflex and swallowing function developed pneumonia. The authors also demonstrated that patients with silent cerebral infarction have a higher risk of developing pneumonia than those with normal head CT findings. In that study, the occurrence of cerebral infarction did not lead to aspiration pneumonia in every case; the incidence of aspiration pneumonia depended on the location and extent or number of infarcts [61]. Additionally, poor oral hygiene [62–64], the overuse of sedative medications [19], impaired immunity [65, 66], reduced mucociliary transport [56] and a depressed lung function due to aging are risk factors for aspiration pneumonia. These factors appear to be associated with each other, suggesting that aspiration pneumonia occurs as a result of multifactorial risk factors (Figure 1).
Figure 1.
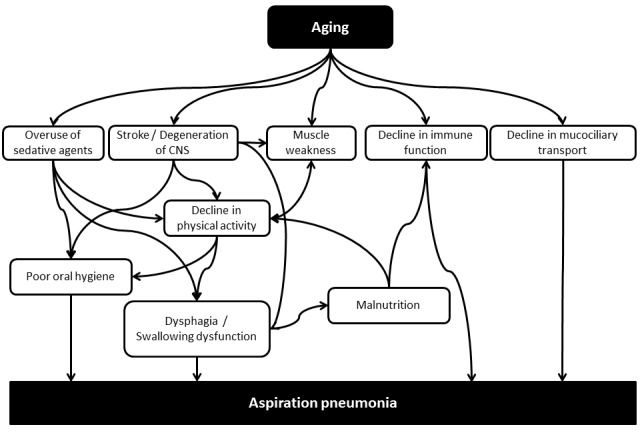
Risk factors associated with aspiration pneumonia.
Abbreviations: CNS= central nervous system
Evaluating the swallowing function has limitations regarding the diagnosis of aspiration pneumonia
Videofluorographic swallowing tests are the most commonly used instrumental assessment tool for evaluating the swallowing function [67,68]. This procedure assesses anatomical structures as well as the following swallowing phases: oral, pharyngeal and esophageal [69]. However, this examination carries a risk of failing to detect small amounts of aspiration that cannot be identified on radiographic images (Figure 2). In fact, Matsuse and colleagues reported that oropharyngeal dysphagia is not observed in approximately half of cases of diffuse aspiration bronchiolitis [70], and Kukichi and colleagues documented that silent aspiration occurs in 71% of patients with CAP [71].
Figure 2.
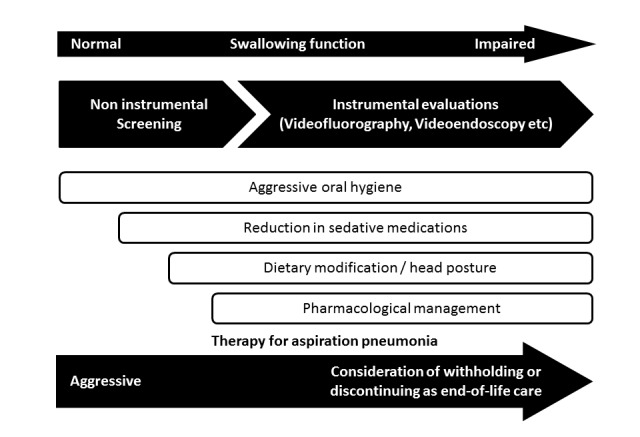
Diagnostic procedures and types of intervention for dysphagia and aspiration pneumonia.
Are radiographic features useful for diagnosing aspiration pneumonia?
Esayag and colleagues reported that normal chest radiography findings do not rule out a diagnosis of pneumonia in bedridden patients with suspected pneumonia and that chest CT provides valuable diagnostic information [72]. We investigated chest CT scans in 53 patients admitted for the treatment of pneumonia who were subsequently confirmed to have dysphagia on videofluorographic examinations [73]. A bronchopneumonia pattern was most commonly observed, with a distribution characterized by gravity dependence. When we defined aspiration pneumonia as involving both risk factors for aspiration and evidence of gravity-dependent opacity on chest CT, the prevalence of the disease was lower than that observed in other Japanese studies, although the characteristics of the study population were slightly different [8, 23, 27, 28, 33, 52]. Similarly, the prevalence of aspiration pneumonia in the studies from Spain [25, 26, 51], which required radiographic evidence for a diagnosis, was lower than that observed in the study by Giannella et al. [24], which did not require radiographic evidence. Including radiographic evidence in a dependent pulmonary segment as an essential requirement in the definition of aspiration pneumonia may result in underestimation of the prevalence of the condition. Although a gravity-dependent distribution is consistent with the features of aspiration pneumonia in the elderly, it remains controversial whether radiographic findings influence the prognosis.
What is the purpose of diagnosing aspiration pneumonia?
Physicians consider the benefits when diagnosing patients with aspiration pneumonia. An accurate diagnosis can result in correct prognostic expectations and the administration of effective therapy. Which factors primarily affect the prognosis among patients with CAP or HCAP remains debated [5, 74–76]. Many studies have shown that host factors contribute to the prognosis rather than the presence of drug-resistant pathogens or treatment failure [5, 77]. Relevant host factors reported to date include underlying disease [28, 77], the patient’s activity level [7] and nutrition status [28, 78] and the presence of aspiration pneumonia [8, 9, 26, 27, 38, 78]. However, these factors are cross-associated and exhibit colinearity with each other. For example, aspiration pneumonia often develops in patients with a bedridden status and malnutrition (Figure 2). Well-designed further studies are needed in order to identify the true host factors associated with the prognosis in accordance with such confounding biases.
Aspiration pneumonia also has the potential to be a risk factor for having drug-resistant pathogens [6]. However, the administration of empiric broad-spectrum antibiotic therapy, in accordance with guidelines for the treatment of HCAP, does not necessarily improve the prognosis [5, 31]. Empiric broad-spectrum antibiotic therapy may have beneficial effects in some patients with HCAP, since HCAP is a heterogeneous concept [7]. In addition, covering anaerobic bacteria is not always required, even if such bacteria are detected [17]. Ampicillin/sulbactam is likely to have sufficient efficacy in cases of aspiration pneumonia, although evidence is limited [79–81], and the results were observed among the whole population.
Taking into consideration the perspective of infection control in the hospital, it is essential to detect drug-resistant pathogens in order to prevent the spread of the bacteria, although not all patients with such pathogens require treatment with broad-spectrum antibiotics [82]. When drug-resistant pathogens are detected, medical professionals may need to consider treatment from the viewpoint of infection control in the hospital separately from the therapeutic needs of the individual patient.
Meanwhile, diagnosing aspiration pneumonia enables the physician to consider preventive approaches. Yoshino and colleagues demonstrated that the use of aggressive oral care reduces the risk of developing pneumonia [62]. In addition, dysphagia rehabilitation may have merit in preventing aspiration [83]. Treatment with angiotensin-converting enzyme inhibitors significantly reduces the incidence of pneumonia [20, 84–87], and cilostazol may have a separate effect from that of preventing cerebral infarction [88]. Patients with aspiration pneumonia require multilateral prevention methods due to the presence of confounding risk factors, as shown in Figure 1. Unless appropriate prevention measures are taken in addition to the administration of antibiotic therapy, clinical physicians may misjudge the inefficacy of treatment due to repeated episodes of aspiration resulting from drug-resistant pathogens.
Other reasons for difficulties in managing patients with aspiration pneumonia based on guidelines for pneumonia
We herein described the difficulties in defining aspiration pneumonia in order to evaluate why guidelines for treating pneumonia are not clearly applicable to cases of aspiration pneumonia. Furthermore, there are additional difficulties concerning ethical issues. Aspiration pneumonia, as an acute disease in elderly patients, is treatable in each occurrence [79–81, 89] and preventable to some extent [13, 46]. However, prevention protocols become less effective as the disorder progresses, at which point physicians consider the condition to be unavoidable, indicating a status near the end of life. Therefore, the occurrence of repeated episodes of aspiration pneumonia despite proper prevention likely reflects a terminal phase of life (Figure 2). Bosch and colleagues reported that long-term prognostic factors in patients with aspiration pneumonia are based on host factors, such as age, declines in physical activity and malnutrition, whereas short-term prognostic factors are consistent with the existing severity index of pneumonia [87, 90, 91]. These studies scientifically documented that repeated episodes of aspiration pneumonia in the elderly are unavoidable. Indeed, over half of clinical physicians treating patients suffering from pneumonia regard death among elderly patients with aspiration pneumonia as ‘death from age-related physical debility [92]. It is appropriate to regard death from unavoidable repeated aspiration pneumonia as natural death rather than death due to disease. There is no evidence that tube feeding reduces the risk of aspiration [93–95]. There are also ethical issues regarding the use of tube feeding in such patients [96–98]. The use of strategies involving withholding or discontinuing intensive therapy, administering antibiotics and providing nutritional support for patients with repeated episodes of aspiration pneumonia requires further discussion.
Because guidelines for pneumonia are formulated based on scientific evidence, it is difficult to incorporate the ethical aspects of the concept of aspiration pneumonia. Carrabba and colleagues excluded patients with aspiration pneumonia in one study in order to evaluate the characteristics of HCAP [76]. When planning clinical studies scientifically, it may be necessary to evaluate patients with HCAP separately from those with unavoidable repeated episodes of aspiration pneumonia.
Conclusions
This review revealed that the definition, prevalence and role of aspiration pneumonia as a prognostic factor varies widely. It is difficult for guidelines to include the concept of aspiration pneumonia, as the definition of the condition is unclear, the swallowing function is easily changeable depending on the patient’s condition and there is no standard procedure for objectively evaluating the swallowing function. Aspiration pneumonia is predominantly occurred in the elderly population caused by multifactorial patient background factors. Further studies are therefore needed to evaluate which host factors are primarily associated with mortality taking into consideration confounding. It is essential to discuss these issues so as to correctly carry out clinical studies of pneumonia associated with unavoidable ethical problems.
References
- [1].American Thoracic Society. Infectious Diseases Society of America Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- [2].Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, et al. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128:3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- [3].Seymann GB, Di Francesco L, Sharpe B, Rohde J, Fedullo P, et al. The HCAP gap: differences between self-reported practice patterns and published guidelines for health care-associated pneumonia. Clin Infect Dis. 2009;49:1868–1874. doi: 10.1086/648429. [DOI] [PubMed] [Google Scholar]
- [4].Grenier C, Pepin J, Nault V, Howson J, Fournier X, et al. Impact of guideline-consistent therapy on outcome of patients with healthcare-associated and community-acquired pneumonia. J Antimicrob Chemother. 2011;66:1617–1624. doi: 10.1093/jac/dkr176. [DOI] [PubMed] [Google Scholar]
- [5].Attridge RT, Frei CR. Health care-associated pneumonia: an evidence-based review. Am J Med. 2011;124:689–697. doi: 10.1016/j.amjmed.2011.01.023. [DOI] [PubMed] [Google Scholar]
- [6].Chalmers JD, Taylor JK, Singanayagam A, Fleming GB, Akram AR, et al. Epidemiology, antibiotic therapy, and clinical outcomes in health care-associated pneumonia: a UK cohort study. Clin Infect Dis. 2011;53:107–113. doi: 10.1093/cid/cir274. [DOI] [PubMed] [Google Scholar]
- [7].Ewig S, Welte T, Chastre J, Torres A. Rethinking the concepts of community-acquired and health-care-associated pneumonia. Lancet Infect Dis. 2010;10:279–287. doi: 10.1016/S1473-3099(10)70032-3. [DOI] [PubMed] [Google Scholar]
- [8].Komiya K, Ishii H, Umeki K, Mizunoe S, Okada F, et al. Impact of aspiration pneumonia in patients with community-acquired pneumonia and healthcare-associated pneumonia: A multicenter retrospective cohort study. Respirology. 2013;18:514–521. doi: 10.1111/resp.12029. [DOI] [PubMed] [Google Scholar]
- [9].Polverino E, Cilloniz C, Dambrava P, Gabarrus A, Ferrer M, et al. Systemic corticosteroids for community-acquired pneumonia: reasons for use and lack of benefit on outcome. Respirology. 2013;18:263–271. doi: 10.1111/resp.12013. [DOI] [PubMed] [Google Scholar]
- [10].Falcone M, Corrao S, Licata G, Serra P, Venditti M. Clinical impact of broad-spectrum empirical antibiotic therapy in patients with healthcare-associated pneumonia: a multicenter interventional study. Intern Emerg Med. 2012;7:523–531. doi: 10.1007/s11739-012-0795-8. [DOI] [PubMed] [Google Scholar]
- [11].Teramoto S, Kawashima M, Komiya K, Shoji S. Health-care-associated pneumonia is primarily due to aspiration pneumonia. Chest. 2009;136:1702–1703. doi: 10.1378/chest.09-1204. [DOI] [PubMed] [Google Scholar]
- [12].Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–671. doi: 10.1056/NEJM200103013440908. [DOI] [PubMed] [Google Scholar]
- [13].Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124:328–336. doi: 10.1378/chest.124.1.328. [DOI] [PubMed] [Google Scholar]
- [14].Spickard A, 3rd, Hirschmann JV. Exogenous lipoid pneumonia. Arch Intern Med. 1994;154:686–692. [PubMed] [Google Scholar]
- [15].Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J. 2002;78:399–403. doi: 10.1136/pmj.78.921.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zissin R, Shapiro-Feinberg M, Rozenman J, Apter S, Smorjik J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol. 2001;11:606–611. doi: 10.1007/s003300000619. [DOI] [PubMed] [Google Scholar]
- [17].El-Solh AA, Pietrantoni C, Bhat A, Aquilina AT, Okada M, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003;167:1650–1654. doi: 10.1164/rccm.200212-1543OC. [DOI] [PubMed] [Google Scholar]
- [18].Fernandez-Sabe N, Carratala J, Roson B, Dorca J, Verdaguer R, et al. Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore) 2003;82:159–169. doi: 10.1097/01.md.0000076005.64510.87. [DOI] [PubMed] [Google Scholar]
- [19].Vergis EN, Brennen C, Wagener M, Muder RR. Pneumonia in long-term care: a prospective case-control study of risk factors and impact on survival. Arch Intern Med. 2001;161:2378–2381. doi: 10.1001/archinte.161.19.2378. [DOI] [PubMed] [Google Scholar]
- [20].Yamaya M, Yanai M, Ohrui T, Arai H, Sasaki H. Interventions to prevent pneumonia among older adults. J Am Geriatr Soc. 2001;49:85–90. doi: 10.1046/j.1532-5415.2001.49015.x. [DOI] [PubMed] [Google Scholar]
- [21].Ohrui T. Preventive strategies for aspiration pneumonia in elderly disabled persons. Tohoku J Exp Med. 2005;207:3–12. doi: 10.1620/tjem.207.3. [DOI] [PubMed] [Google Scholar]
- [22].Sasaki H, Sekizawa K, Yanai M, Arai H, Yamaya M, et al. New strategies for aspiration pneumonia. Intern Med. 1997;36:851–855. doi: 10.2169/internalmedicine.36.851. [DOI] [PubMed] [Google Scholar]
- [23].Fukuyama H, Yamashiro S, Tamaki H, Kishaba T. A prospective comparison of nursing- and healthcare-associated pneumonia (NHCAP) with community-acquired pneumonia (CAP) J Infect Chemother. 2013;19:719–726. doi: 10.1007/s10156-013-0557-1. [DOI] [PubMed] [Google Scholar]
- [24].Giannella M, Pinilla B, Capdevila JA, Martinez Alarcon J, et al. Pneumonia treated in the internal medicine department: focus on healthcare-associated pneumonia. Clin Microbiol Infect. 2012;18:786–794. doi: 10.1111/j.1469-0691.2011.03757.x. [DOI] [PubMed] [Google Scholar]
- [25].Simonetti A, Viasus D, Garcia-Vidal C, Adamuz J, Roset A, et al. Timing of antibiotic administration and outcomes of hospitalized patients with community-acquired and healthcare-associated pneumonia. Clin Microbiol Infect. 2012;18:1149–1155. doi: 10.1111/j.1469-0691.2011.03709.x. [DOI] [PubMed] [Google Scholar]
- [26].Garcia-Vidal C, Viasus D, Roset A, Adamuz J, Verdaguer R, et al. Low incidence of multidrug-resistant organisms in patients with healthcare-associated pneumonia requiring hospitalization. Clin Microbiol Infect. 2011;17:1659–1665. doi: 10.1111/j.1469-0691.2011.03484.x. [DOI] [PubMed] [Google Scholar]
- [27].Nakagawa N, Saito Y, Sasaki M, Tsuda Y, Mochizuki H, et al. Comparison of clinical profile in elderly patients with nursing and healthcare-associated pneumonia, and those with community-acquired pneumonia. Geriatr Gerontol Int. 2013 doi: 10.1111/ggi.12110. in press. [DOI] [PubMed] [Google Scholar]
- [28].Oshitani Y, Nagai H, Matsui H, Aoshima M. Reevaluation of the Japanese guideline for healthcare-associated pneumonia in a medium-sized community hospital in Japan. J Infect Chemother. 2013;19:579–587. doi: 10.1007/s10156-012-0517-1. [DOI] [PubMed] [Google Scholar]
- [29].Miyashita N, Akaike H, Teranishi H, Kawai Y, Ouchi K, et al. Evaluation of serological tests for diagnosis of Chlamydophila pneumoniae pneumonia in patients with nursing and healthcare-associated pneumonia. J Infect Chemother. 2013;19:249–255. doi: 10.1007/s10156-012-0491-7. [DOI] [PubMed] [Google Scholar]
- [30].Ishida T, Tachibana H, Ito A, Yoshioka H, Arita M, et al. Clinical characteristics of nursing and healthcare-associated pneumonia: a Japanese variant of healthcare-associated pneumonia. Intern Med. 2012;51:2537–2544. doi: 10.2169/internalmedicine.51.7987. [DOI] [PubMed] [Google Scholar]
- [31].Webb BJ, Dangerfield BS, Pasha JS, Agrwal N, Vikram HR. Guideline-concordant antibiotic therapy and clinical outcomes in healthcare-associated pneumonia. Respir Med. 2012;106:1606–1612. doi: 10.1016/j.rmed.2012.08.003. [DOI] [PubMed] [Google Scholar]
- [32].Kaku N, Yanagihara K, Morinaga Y, Izumikawa K, Nagashima S, et al. The definition of healthcare-associated pneumonia (HCAP) is insufficient for the medical environment in Japan: a comparison of HCAP and nursing and healthcare-associated pneumonia (NHCAP) J Infect Chemother. 2013;19:70–76. doi: 10.1007/s10156-012-0454-z. [DOI] [PubMed] [Google Scholar]
- [33].Miyashita N, Kawai Y, Akaike H, Ouchi K, Hayashi T, et al. Clinical features and the role of atypical pathogens in nursing and healthcare-associated pneumonia (NHCAP): differences between a teaching university hospital and a community hospital. Intern Med. 2012;51:585–594. doi: 10.2169/internalmedicine.51.6475. [DOI] [PubMed] [Google Scholar]
- [34].Madaras-Kelly KJ, Remington RE, Fan VS, Sloan KL. Predicting antibiotic resistance to community-acquired pneumonia antibiotics in culture-positive patients with healthcare-associated pneumonia. J Hosp Med. 2012;7:195–202. doi: 10.1002/jhm.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hsu JL, Siroka AM, Smith MW, Holodniy M, Meduri GU. One-year outcomes of community-acquired and healthcare-associated pneumonia in the Veterans Affairs Healthcare System. Int J Infect Dis. 2011;15:e382–387. doi: 10.1016/j.ijid.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Madaras-Kelly KJ, Remington RE, Sloan KL, Fan VS. Guideline-based antibiotics and mortality in healthcare-associated pneumonia. J Gen Intern Med. 2012;27:845–852. doi: 10.1007/s11606-012-2011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Dobler CC, Waterer G. Healthcare-associated pneumonia: a US disease or relevant to the Asia Pacific, too? Respirology. 2013;18:923–932. doi: 10.1111/resp.12132. [DOI] [PubMed] [Google Scholar]
- [38].Falcone M, Blasi F, Menichetti F, Pea F, Violi F. Pneumonia in frail older patients: an up to date. Intern Emerg Med. 2012;7:415–424. doi: 10.1007/s11739-012-0796-7. [DOI] [PubMed] [Google Scholar]
- [39].Labelle A, Kollef MH. Healthcare-associated pneumonia: approach to management. Clin Chest Med. 2012;32:507–515. doi: 10.1016/j.ccm.2011.05.003. [DOI] [PubMed] [Google Scholar]
- [40].Falcone M, Venditti M, Shindo Y, Kollef MH. Healthcare-associated pneumonia: diagnostic criteria and distinction from community-acquired pneumonia. Int J Infect Dis. 2011;15:e545–550. doi: 10.1016/j.ijid.2011.04.005. [DOI] [PubMed] [Google Scholar]
- [41].Polverino E, Torres A. Current perspective of the HCAP problem: is it CAP or is it HAP? Semin Respir Crit Care Med. 2009;30:239–248. doi: 10.1055/s-0029-1202940. [DOI] [PubMed] [Google Scholar]
- [42].Morrow LE. Prevention strategies for healthcare-associated pneumonia. Semin Respir Crit Care Med. 2009;30:86–91. doi: 10.1055/s-0028-1119812. [DOI] [PubMed] [Google Scholar]
- [43].Restrepo MI, Anzueto A. The role of gram-negative bacteria in healthcare-associated pneumonia. Semin Respir Crit Care Med. 2009;30:61–66. doi: 10.1055/s-0028-1119810. [DOI] [PubMed] [Google Scholar]
- [44].Polverino E, Torres A. Diagnostic strategies for healthcare-associated pneumonia. Semin Respir Crit Care Med. 2009;30:36–45. doi: 10.1055/s-0028-1119807. [DOI] [PubMed] [Google Scholar]
- [45].Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30:26–35. doi: 10.1055/s-0028-1119806. [DOI] [PubMed] [Google Scholar]
- [46].Carratala J, Garcia-Vidal C. What is healthcare-associated pneumonia and how is it managed? Curr Opin Infect Dis. 2008;21:168–173. doi: 10.1097/QCO.0b013e3282f4f248. [DOI] [PubMed] [Google Scholar]
- [47].Chroneou A, Zias N, Beamis JF, Jr, Craven DE. Healthcare-associated pneumonia: principles and emerging concepts on management. Expert Opin Pharmacother. 2007;8:3117–3131. doi: 10.1517/14656566.8.18.3117. [DOI] [PubMed] [Google Scholar]
- [48].Fujitani S, Yu VL. A new category--healthcare-associated pneumonia: a good idea, but problems with its execution. Eur J Clin Microbiol Infect Dis. 2006;25:627–631. doi: 10.1007/s10096-006-0197-9. [DOI] [PubMed] [Google Scholar]
- [49].Mylotte JM. Nursing home-acquired pneumonia: update on treatment options. Drugs Aging. 2006;23:377–390. doi: 10.2165/00002512-200623050-00002. [DOI] [PubMed] [Google Scholar]
- [50].Craven DE. What is healthcare-associated pneumonia, and how should it be treated? Curr Opin Infect Dis. 2006;19:153–160. doi: 10.1097/01.qco.0000216626.05821.40. [DOI] [PubMed] [Google Scholar]
- [51].Carratala J, Mykietiuk A, Fernandez-Sabe N, Suarez C, Dorca J, et al. Health care-associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med. 2007;167:1393–1399. doi: 10.1001/archinte.167.13.1393. [DOI] [PubMed] [Google Scholar]
- [52].Shindo Y, Sato S, Maruyama E, Ohashi T, Ogawa M, et al. Health-care-associated pneumonia among hospitalized patients in a Japanese community hospital. Chest. 2009;135:633–640. doi: 10.1378/chest.08-1357. [DOI] [PubMed] [Google Scholar]
- [53].Kohno S, Imamura Y, Shindo Y, Seki M, Ishida T, et al. Clinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation] Respir Investig. 2013;51:103–126. doi: 10.1016/j.resinv.2012.11.001. [DOI] [PubMed] [Google Scholar]
- [54].RS Fraser NLM, Colman Neil, Pare PD. Fraser and Pare’s Diagnosis of Diseases of the Chest. II W.B. Saunders; 1999. Features of Pulmonary Infection. [Google Scholar]
- [55].Gleeson K, Eggli DF, Maxwell SL. Quantitative aspiration during sleep in normal subjects. Chest. 1997;111:1266–1272. doi: 10.1378/chest.111.5.1266. [DOI] [PubMed] [Google Scholar]
- [56].Parrilla C, Valenza V, Calo L, Passali GC, Castaldi P, et al. Is it sufficient to quantify aspiration for predicting aspiration pneumonia? Clin Nucl Med. 2008;33:236–239. doi: 10.1097/RLU.0b013e31815969d2. [DOI] [PubMed] [Google Scholar]
- [57].Hirose M, Komiya K, Kadota J. Influence of appetite and continuation of meals on the prognosis of elderly patients who have lost swallowing function. J Palliat Med. 2014 doi: 10.1089/jpm.2013.0584. in press. [DOI] [PubMed] [Google Scholar]
- [58].Teramoto S, Yamamoto H, Yamaguchi Y, Ouchi Y, Matsuse T. A novel diagnostic test for the risk of aspiration pneumonia in the elderly. Chest. 2004;125:801–802. doi: 10.1378/chest.125.2.801. [DOI] [PubMed] [Google Scholar]
- [59].Nakagawa T, Sekizawa K, Nakajoh K, Tanji H, Arai H, et al. Silent cerebral infarction: a potential risk for pneumonia in the elderly. J Intern Med. 2000;247:255–259. doi: 10.1046/j.1365-2796.2000.00599.x. [DOI] [PubMed] [Google Scholar]
- [60].Holas MA, DePippo KL, Reding MJ. Aspiration and relative risk of medical complications following stroke. Arch Neurol. 1994;51:1051–1053. doi: 10.1001/archneur.1994.00540220099020. [DOI] [PubMed] [Google Scholar]
- [61].Galovic M, Leisi N, Muller M, Weber J, Abela E, et al. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013;44:2760–2767. doi: 10.1161/STROKEAHA.113.001690. [DOI] [PubMed] [Google Scholar]
- [62].Yoshino A, Ebihara T, Ebihara S, Fuji H, Sasaki H. Daily oral care and risk factors for pneumonia among elderly nursing home patients. JAMA. 2001;286:2235–2236. doi: 10.1001/jama.286.18.2235. [DOI] [PubMed] [Google Scholar]
- [63].Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, et al. Oral care reduces pneumonia in older patients in nursing homes. J Am Geriatr Soc. 2002;50:430–433. doi: 10.1046/j.1532-5415.2002.50106.x. [DOI] [PubMed] [Google Scholar]
- [64].Quagliarello V, Ginter S, Han L, Van Ness P, Allore H, et al. Modifiable risk factors for nursing home-acquired pneumonia. Clin Infect Dis. 2005;40:1–6. doi: 10.1086/426023. [DOI] [PubMed] [Google Scholar]
- [65].Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging. Aging Dis. 2012;3:91–129. [PMC free article] [PubMed] [Google Scholar]
- [66].Hazeldine J, Lord JM. The impact of ageing on natural killer cell function and potential consequences for health in older adults. Ageing Res Rev. 2013 doi: 10.1016/j.arr.2013.04.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Bulow M. Videofluoroscopic swallow study: techniques, signs and reports. Nestle Nutr Inst Workshop Ser. 2012;72:43–52. doi: 10.1159/000339980. [DOI] [PubMed] [Google Scholar]
- [68].Ott DJ, Pikna LA. Clinical and videofluoroscopic evaluation of swallowing disorders. AJR Am J Roentgenol. 1993;161:507–513. doi: 10.2214/ajr.161.3.8352094. [DOI] [PubMed] [Google Scholar]
- [69].Robbins J. Normal swallowing and aging. Semin Neurol. 1996;16:309–317. doi: 10.1055/s-2008-1040989. [DOI] [PubMed] [Google Scholar]
- [70].Matsuse T, Oka T, Kida K, Fukuchi Y. Importance of diffuse aspiration bronchiolitis caused by chronic occult aspiration in the elderly. Chest. 1996;110:1289–1293. doi: 10.1378/chest.110.5.1289. [DOI] [PubMed] [Google Scholar]
- [71].Kikuchi R, Watabe N, Konno T, Mishina N, Sekizawa K, et al. High incidence of silent aspiration in elderly patients with community-acquired pneumonia. Am J Respir Crit Care Med. 1994;150:251–253. doi: 10.1164/ajrccm.150.1.8025758. [DOI] [PubMed] [Google Scholar]
- [72].Esayag Y, Nikitin I, Bar-Ziv J, Cytter R, Hadas-Halpern I, et al. Diagnostic value of chest radiographs in bedridden patients suspected of having pneumonia. Am J Med. 2010;123:e81–85. doi: 10.1016/j.amjmed.2009.09.012. [DOI] [PubMed] [Google Scholar]
- [73].Komiya K, Ishii H, Umeki K, Kawamura T, Okada F, et al. Computed tomography findings of aspiration pneumonia in 53 patients. Geriatr Gerontol Int. 2013;13:580–585. doi: 10.1111/j.1447-0594.2012.00940.x. [DOI] [PubMed] [Google Scholar]
- [74].Ewig S, Welte T, Torres A. Is healthcare-associated pneumonia a distinct entity needing specific therapy? Curr Opin Infect Dis. 2012;25:166–175. doi: 10.1097/QCO.0b013e32835023fb. [DOI] [PubMed] [Google Scholar]
- [75].Jeong BH, Koh WJ, Yoo H, Um SW, Suh GY, et al. Performances of prognostic scoring systems in patients with healthcare-associated pneumonia. Clin Infect Dis. 2013;56:625–632. doi: 10.1093/cid/cis970. [DOI] [PubMed] [Google Scholar]
- [76].Carrabba M, Zarantonello M, Bonara P, Hu C, Minonzio F, et al. Severity assessment of healthcare-associated pneumonia and pneumonia in immunosuppression. Eur Respir J. 2012;40:1201–1210. doi: 10.1183/09031936.00187811. [DOI] [PubMed] [Google Scholar]
- [77].Lujan M, Gallego M, Rello J. Healthcare-associated infections. A useful concept? Curr Opin Crit Care. 2009;15:419–424. doi: 10.1097/MCC.0b013e32832e9956. [DOI] [PubMed] [Google Scholar]
- [78].Riquelme R, Torres A, El-Ebiary M, de la Bellacasa JP, Estruch R, et al. Community-acquired pneumonia in the elderly: A multivariate analysis of risk and prognostic factors. Am J Respir Crit Care Med. 1996;154:1450–1455. doi: 10.1164/ajrccm.154.5.8912763. [DOI] [PubMed] [Google Scholar]
- [79].Allewelt M, Schuler P, Bolcskei PL, Mauch H, Lode H. Ampicillin + sulbactam vs clindamycin +/− cephalosporin for the treatment of aspiration pneumonia and primary lung abscess. Clin Microbiol Infect. 2004;10:163–170. doi: 10.1111/j.1469-0691.2004.00774.x. [DOI] [PubMed] [Google Scholar]
- [80].Kadowaki M, Demura Y, Mizuno S, Uesaka D, Ameshima S, et al. Reappraisal of clindamycin IV monotherapy for treatment of mild-to-moderate aspiration pneumonia in elderly patients. Chest. 2005;127:1276–1282. doi: 10.1378/chest.127.4.1276. [DOI] [PubMed] [Google Scholar]
- [81].Ott SR, Allewelt M, Lorenz J, Reimnitz P, Lode H, German Lung Abscess Study G Moxifloxacin vs ampicillin/sulbactam in aspiration pneumonia and primary lung abscess. Infection. 2008;36:23–30. doi: 10.1007/s15010-007-7043-6. [DOI] [PubMed] [Google Scholar]
- [82].Galvin S, Dolan A, Cahill O, Daniels S, Humphreys H. Microbial monitoring of the hospital environment: why and how? J Hosp Infect. 2012;82:143–151. doi: 10.1016/j.jhin.2012.06.015. [DOI] [PubMed] [Google Scholar]
- [83].Steele CM. Exercise-based approaches to dysphagia rehabilitation. Nestle Nutr Inst Workshop Ser. 2012;72:109–117. doi: 10.1159/000339999. [DOI] [PubMed] [Google Scholar]
- [84].Van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C. Risk factors for aspiration pneumonia in frail older people: a systematic literature review. J Am Med Dir Assoc. 2011;12:344–354. doi: 10.1016/j.jamda.2010.12.099. [DOI] [PubMed] [Google Scholar]
- [85].Arai T, Yasuda Y, Takaya T, Toshima S, Kashiki Y, et al. ACE inhibitors and symptomless dysphagia. Lancet. 1998;352:115–116. doi: 10.1016/S0140-6736(98)85021-6. [DOI] [PubMed] [Google Scholar]
- [86].Sekizawa K, Matsui T, Nakagawa T, Nakayama K, Sasaki H. ACE inhibitors and pneumonia. Lancet. 1998;352:1069. doi: 10.1016/S0140-6736(05)60114-6. [DOI] [PubMed] [Google Scholar]
- [87].Bosch X, Formiga F, Cuerpo S, Torres B, Roson B, et al. Aspiration pneumonia in old patients with dementia. Prognostic factors of mortality. Eur J Intern Med. 2012;23:720–726. doi: 10.1016/j.ejim.2012.08.006. [DOI] [PubMed] [Google Scholar]
- [88].Teramoto S, Yamamoto H, Yamaguchi Y, Ishii M, Hibi S, et al. Antiplatelet cilostazol, an inhibitor of type III phosphodiesterase, improves swallowing function in patients with a history of stroke. J Am Geriatr Soc. 2008;56:1153–1154. doi: 10.1111/j.1532-5415.2008.01703.x. [DOI] [PubMed] [Google Scholar]
- [89].Talaie H, Jabari HR, Shadnia S, Pajouhmand A, Nava-Ocampo AA, et al. Cefepime/clindamycin vs. ceftriaxone/clindamycin for the empiric treatment of poisoned patients with aspiration pneumonia. Acta Biomed. 2008;79:117–122. [PubMed] [Google Scholar]
- [90].Komiya K, Kadota JI. C-reactive protein as a prognostic factor in elderly patients with aspiration pneumonia. Eur J Intern Med. 2013;24:e88–9. doi: 10.1016/j.ejim.2013.06.009. [DOI] [PubMed] [Google Scholar]
- [91].Falcone M, Corrao S, Venditti M, Serra P, Licata G. Performance of PSI, CURB-65, and SCAP scores in predicting the outcome of patients with community-acquired and healthcare-associated pneumonia. Intern Emerg Med. 2011;6:431–436. doi: 10.1007/s11739-011-0521-y. [DOI] [PubMed] [Google Scholar]
- [92].Komiya K, Ishii H, Kushima H, Sato S, Kimura H, et al. Physicians’ attitudes toward the definition of “death from age-related physical debility” in deceased elderly with aspiration pneumonia. Geriatr Gerontol Int. 2013;13:586–590. doi: 10.1111/j.1447-0594.2012.00941.x. [DOI] [PubMed] [Google Scholar]
- [93].Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: a review of the evidence. JAMA. 1999;282:1365–1370. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- [94].Dharmarajan TS, Unnikrishnan D, Pitchumoni CS. Percutaneous endoscopic gastrostomy and outcome in dementia. Am J Gastroenterol. 2001;96:2556–2563. doi: 10.1111/j.1572-0241.2001.04099.x. [DOI] [PubMed] [Google Scholar]
- [95].Galicia-Castillo M. The PEG dilemma: feeding tubes are not the answer in advanced dementia. Geriatrics. 2006;61:12–13. [PubMed] [Google Scholar]
- [96].Komiya K, Ishii H, Okabe E, Iwashita T, Miyajima H, et al. Risk factors for unexpected death from suffocation in elderly patients hospitalized for pneumonia. Geriatr Gerontol Int. 2013;13:388–392. doi: 10.1111/j.1447-0594.2012.00912.x. [DOI] [PubMed] [Google Scholar]
- [97].Komiya K, Ishii H, Teramoto S, Yasuda T, Sato S, et al. Medical professionals’ attitudes toward tube feeding for themselves or their families: a multicenter survey in Japan. J Palliat Med. 2012;15:561–566. doi: 10.1089/jpm.2011.0496. [DOI] [PubMed] [Google Scholar]
- [98].Solomon MZ, O’Donnell L, Jennings B, Guilfoy V, Wolf SM, et al. Decisions near the end of life: professional views on life-sustaining treatments. Am J Public Health. 1993;83:14–23. doi: 10.2105/ajph.83.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]


