Abstract
Objective
To assess relationships between adverse childhood experiences and self-reported disabilities in adult life.
Design
Cross-sectional random-digit-dialed state-population-based survey (Behavioral Risk Factor Surveillance System (BRFSS))
Setting
14 States and the District of Columbia
Participants
Non-institutionalized adults aged ≥ 18 years surveyed in 2009 and/or in 2010 (n = 81,184).
Methods
The BRFSS Adverse Childhood Experience (ACE) Module asks about abuse (physical, sexual, emotional), family dysfunction (exposures to domestic violence, living with mentally ill, substance abusing, or incarcerated family member(s), and/or parental separation/divorce) occurring before age 18. The ACE Score sums affirmed ACE categories (range 0-8). We controlled for demographic characteristics (age, race, education, income, and marital status) and self-reported physical health conditions (stroke, myocardial infarction, diabetes, coronary heart disease, asthma). Five states asked participants about mental health conditions (anxiety and depression). A subset analysis of participants in these states evaluated the effect of adjusting for these conditions.
Main Outcome Measures
The primary outcome was disability (self-reported activity limitation and/or assistive device use.)
Results
Over half (57%) of participants reported at least one adverse childhood experience category and 23.2% reported disability. The odds ratio (OR [95% confidence interval]) of disability increased in a graded fashion from 1.3 [1.2-1.4] among those experiencing 1 adverse experience to 5.8 [4.6-7.5] among those with 7 to 8 adverse experiences compared to those with no such experiences, adjusting for demographic factors. The relationship between adverse experiences and disability remained strong after adjusting for physical and mental health conditions.
Conclusions
There is a strong graded relationship between childhood exposure to abuse and household dysfunction and self-reported disability in adulthood, even after adjusting for potentially mediating health conditions. Greater clinician, researcher and policymaker awareness of the impact of childhood adversity on disability is crucial to help those affected by childhood adversity lead more functional lives.
INTRODUCTION
Adverse childhood experiences (ACEs), including abuse and family dysfunction, impact over 50% of the US population1-3 and are increasingly recognized to have powerful adverse effects on health at all life stages. ACE exposure can increase the prevalence of childhood somatic symptoms.4 There is also a dose-response effect of the number of ACE categories on the prevalence of adolescent and adult health risk behaviors.5-11 Effects of ACEs last well into adulthood1,12,13 increasing the prevalence of somatic symptoms,14 chronic health conditions,1-3,15 and premature mortality.16 Less is known about their effects on disability or how they affect functional recovery from potentially disabling conditions.
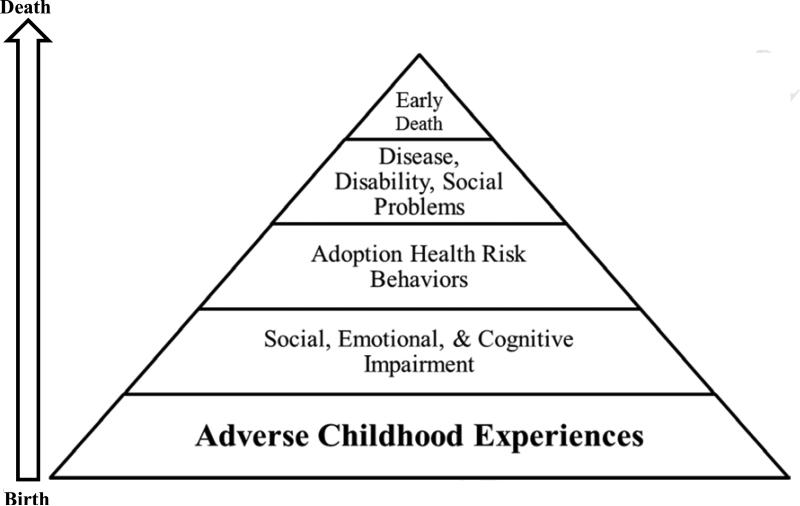
The paucity of research focusing on disability and disparities in health outcomes has been recently recognized by several national health organizations which have called for more research on disability and health disparities. 17-19 Recognizing the need for a common conceptual framework of disability, the Institute of Medicine advocated adapting concepts from the International Classification of Functioning, Disability and Health (ICF),20 which distinguishes between health conditions, negative changes in body structure and function (impairments), activity limitations and participation restrictions.21,22 The original ACE conceptual model was a pyramid illustrating the life course with ACEs at the foundation adversely affecting later stages of life. Disease, disability (and social problems) are combined in the same higher layer just below premature death (Fig 1).1 Yet not all disease leads to disability and therefore understanding how ACEs influence the development and/or effects of disability is vital for designing effective clinical interventions to improve function in those affected by childhood adversity. Thus, we wished to expand this ACE model by recognizing distinctions between health conditions and subsequent disabilities, allowing evaluation of the relationship between childhood adversity and later onset of disability.
Figure 1. Centers for Disease Control and Prevention (CDC) - Kaiser Adverse Childhood Experience (ACE) Study conceptual model70.
CDC ACE pyramid70 illustrating potential effects of ACEs throughout the life course
Mounting evidence suggests that ACEs can affect neurodevelopment through epigenetic mechanisms. Thus an early adverse environment can lead to changes in gene expression causing functional and structural changes to brain, neuroendocrine, autonomic and immune functions that may affect the way individuals respond to stress later in life.12,23-28 Although disease and health conditions are often analyzed as outcomes, they can also be stressors. Beyond affecting the biological response to adult stressors, childhood adversity increases the likelihood of engaging in health-risk behaviors in adolescence and adulthood,1,8,9,29 and may adversely affect adult-life social resources,30 coping skills and emotional functioning/distress.31 All such factors may affect the disablement process. We hypothesized that ACEs would be associated with increased rates of disability even after controlling for health conditions and that as the number of ACE categories experienced increased, rates of disability would increase. We further anticipated that different types of abuse may have differential effects on disability
METHODS
Study Design and Sample
We analyzed data from the Behavioral Risk Factor Surveillance System (BRFSS), a population-based cross-sectional survey. The BRFSS uses a disproportionate stratified sampling technique to obtain state-specific probability samples of households with telephones. Since it is not practical to survey every resident of a state, the goal of probability sampling to is to obtain a sample that is representative of that state. The BRFSS also uses survey weights to ensure that the weighted sample represents the known proportions of age, sex, race/ethnicity within a state or geographic region.32 Fourteen states and the District of Columbia administered the ACE module in 2009 and/or 2010.33 (Table 1) The state-specific cooperation rates (proportion of completed interviews of those contacted) ranged from 68.9 to 82.4. Council of American Survey Research Organizations response rates (proportion of completed interviews of the estimated eligible) ranged from 47.0 to 68.7.34,35 Of 89,810 participants, we excluded 7,278 (8.1%) because of missing ACE data and 1,348 (1.5%) because of missing disability, demographic, or health condition data, resulting in a final sample size of 81,184 (90.4% of the total original sample).
Table 1.
Estimated Prevalence of Adverse Childhood Experiences (ACE) and Disability by Demographic and Health Characteristics
| Characteristic | Weighted % of total sample1 | ACE ≥ 1 wt.2 % (95% CI2) | ACE ≥ 5 wt. % (95% CI) | Disability wt. % (95% CI) |
|---|---|---|---|---|
| Overall | 100 | 56.8 (56.0-57.5) | 8.4 (8.0-8.9) | 23.1 (22.5-23.7) |
| Age | ||||
| 18-29 | 14.1 | 63.8 (61.3-66.4) | 12.8 (11.1-14.6) | 13.2 (11.4-15.0) |
| 30-44 | 33.3 | 61.6 (60.0-63.2) | 10.8 (9.8-11.8) | 15.4 (14.2-16.5) |
| 45-54 | 19.4 | 59.2 (57.7-60.7) | 8.8 (8.0-9.6) | 24.6 (23.3-25.9) |
| 55-65 | 15.5 | 53.8 (52.4-55.2) | 5.8 (5.2-6.4) | 31.1 (29.9-32.4) |
| 65-74 | 9.6 | 47.3 (45.7-48.9) | 3.3 (2.7-3.8) | 32.1 (30.6-33.6) |
| 75+ | 8.1 | 35.5 (33.9-37.2) | 1.1 (0.8-1.4) | 43.0 (41.3-44.7) |
| Sex | ||||
| Male | 48.6 | 55.7 (54.5-57.0) | 6.9 (6.2-7.6) | 22.1 (21.1-23.0) |
| Female | 51.4 | 57.7 (56.8-58.6) | 9.9 (9.3-10.5) | 24.1 (23.4-24.9) |
| Race | ||||
| Non-Hispanic White | 82.3 | 55.6 (54.7-56.4) | 8.3 (7.7-8.8) | 23.5 (22.8-24.2) |
| Non-Hispanic Black | 7.2 | 65.6 (62.9-68.3) | 7.4 (6.0-8.8) | 24.5 (22.3-26.7) |
| Hispanic | 4.6 | 65.1 (62.1-68.0) | 9.8 (7.9-11.6) | 16.9 (14.9-18.9) |
| Asian/Nat Haw/PI2 | 2.6 | 38.3 (34.0-42.6) | 2.4 (1.6-3.3) | 11.5 (9.4-13.5) |
| Other3 | 3.3 | 70.4 (67.0-73.8) | 17.2 (14.3-20.1) | 28.6 (25.4-31.9) |
| Marital Status | ||||
| Couple | 67.1 | 55.3 (54.3-56.2) | 7.6 (7.0-8.1) | 20.5 (19.7-21.2) |
| Divorced/Separated | 10.6 | 67.0 (65.1-68.9) | 13.5 (12.2-14.9) | 34.7 (32.8-36.5) |
| Widowed | 6.3 | 43.6 (41.8-45.4) | 3.7 (3.0-4.4) | 40.7 (38.9-42.5) |
| Never Married | 16.0 | 61.5 (59.2-63.8) | 10.4 (9.1-11.8) | 19.7 (18.1-21.4) |
| Annual Household Income | ||||
| Less than 15k | 7.0 | 67.0 (64.4-69.6) | 15.8 (13.9-17.8) | 46.7 (43.9-49.5) |
| 15k to less than 25k | 14.2 | 60.8 (58.8-62.8) | 12.2 (10.7-13.8) | 33.7 (31.8-35.5) |
| 25k to less than 50k | 23.3 | 56.8 (55.3-58.3) | 7.9 (7.1-8.7) | 23.7 (22.5-24.8) |
| greater than 50k | 43.5 | 55.5 (54.3-56.7) | 6.7 (6.1-7.4) | 14.8 (14.0-15.6) |
| Don't Know | 6.3 | 54.7 (51.4-58.1) | 8.9 (6.6-11.3) | 30.3 (27.3-33.4) |
| Refused to Answer | 5.7 | 45.7 (42.6-48.8) | 4.4 (3.1-5.8) | 21.7 (19.3-24.0) |
| High School Graduate | ||||
| No | 6.9 | 56.1 (55.3-56.9) | 8.0 (7.5-8.5) | 22.1 (21.5-22.7) |
| Yes | 93.1 | 65.5 (63.0-68.1) | 13.8 (11.7-15.9) | 36.6 (33.9-39.4) |
| Health Conditions4 | ||||
| Asthma (ever) | 12.9 | 66.8 (64.8-68.9) | 14.8 (13.1-16.4) | 37.1 (35.1-39.1) |
| No Asthma | 87.1 | 55.9 (55.0-56.8) | 7.9 (7.3-8.4) | 19.9 (19.3-20.6) |
| Coronary Heart | 4.3 | 63.7 (55.4-72.1) | 21.9 (12.0-31.7) | 59.6 (51.3-67.9) |
| No Coronary Heart | 95.7 | 57.1 (56.3-57.9) | 8.7 (8.2-9.2) | 21.2 (20.5-21.8) |
| Myocardial Infarction | 4.0 | 69.2 (62.4-75.9) | 14.2 (8.8-19.6) | 49.6 (39.5-59.7) |
| No Myocardial Infarction | 96.0 | 57.0 (56.2-57.9) | 8.7 (8.1-9.2) | 21.3 (20.7-21.9) |
| Stroke | 2.8 | 70.6 (65.1-76.1) | 16.7 (10.6-22.7) | 63.5 (56.2-70.7) |
| No Stroke | 97.2 | 57.1 (56.3-57.9) | 8.7 (8.2-9.2) | 21.2 (20.6-21.9) |
| Diabetes | 9.0 | 64.8 (60.3-69.2) | 14.3 (10.4-18.3) | 39.8 (35.3-44.4) |
| No Diabetes | 91.0 | 56.8 (55.9-57.7) | 8.6 (8.1-9.1) | 20.6 (20.0-21.2) |
| Subset Analysis: Psychological Health Conditions4, 5 | ||||
| Anxiety | 13.5 | 78.3 (74.4-82.1) | 23.5 (19.2-27.9) | 43.6 (39.3-47.9) |
| No Anxiety | 86.5 | 54.5 (52.6-56.3) | 7.0 (6.0-8.0) | 18.0 (16.7-19.2) |
| Depression | 17.0 | 77.1 (73.6-80.6) | 24.5 (20.4-28.5) | 45.0 (40.9-49.0) |
| No Depression4 | 83.0 | 53.7 (51.8-55.6) | 6.3 (5.3-7.2) | 16.7 (15.5-18.0) |
The full sample included data from the following states: BRFSS 2009: Arkansas, Louisiana, New Mexico, Tennessee, Washington; BRFSS 2010: District of Columbia, Hawaii, Maine, Nebraska, Nevada, Ohio, Pennsylvania, Utah, Vermont, Washington, Wisconsin. (n = 81,184)
Abbreviations: wt. = weighted; CI = confidence interval; Nat Haw = Native Hawaiian; PI = Pacific Islander
Native American, Multiracial, Other
Health conditions were age standardized using the direct standardization method and the 2000 US standard population37
Psychological Health Condition Variables were only available for states: Ohio, Vermont, Maine, Hawaii, Nevada (Total n = 22,739)
Study Variables
The ACE Module adapted questions from the Kaiser-CDC ACE Study to assess childhood (occurring before age 18) abuse (sexual, physical, emotional) and family dysfunction (experiencing parental domestic violence, parental divorce/separation, family member incarceration, substance abuse36 and mental illness).1,10 The adapted questions were tested using focus groups and cognitive testing.10,37 The individual abuse and domestic violence questions contain a measure of self-reported frequency (once, more than once). The three sexual abuse questions ask about different kinds of sexual contact (being touched, forced to touch, and forced to have sex). We followed the CDC's reported method to group the 11 ACE questions into 8 ACE categories (Table 2). In addition, we used the same criteria for inclusion in each of the ACE categories (Table 2), and the same approach of coding answers of don't know as a negative response. 10 An ACE Score (range 0-8) was calculated by summing the ACEs categories. We grouped scores 7-8 because of low numbers. While count variables capture severity well, qualitative information is lost. Since there may be different effects of abuse by a caretaker and family dysfunction on both the individual child and on family resources, we also analyzed ACEs by type, using the following categories: abuse and family dysfunction, abuse only, and family dysfunction only. Since the broad ACE categories do not differentiate among frequency of experience or severity of experience we also analyzed the individual abuse and domestic violence questions to evaluate the effect of frequency and in the case of sexual abuse, severity of experience.
Table 2.
Adverse Childhood Experiences Questions, Categories and Summary Measures and Prevalence of Disability1
| ACE Categories | Population % (n = 81, 484) | % reporting disability | Adjusted OR2 (95% CI) Disability | |
|---|---|---|---|---|
| Abuse ACE Categories | ||||
| I. Sexual Abuse Category (criterion: once or more than once to any of following 3 questions) | 11.5 | 37.9 | 2.4 (2.1-2.6) | |
| How often did anyone at least 5 years older than you or an adult... | ||||
| 1) Ever touch you Sexually? (missing = 11) | Never | 90.0 | 21.4 | reference |
| Once | 3.9 | 31.4 | 1.8 (1.5-2.2) | |
| More than Once | 6.1 | 43.6 | 3.0 (2.6-3.5) | |
| 2) Try to make you touch them ? (missing = 37) | Never | 92.6 | 21.9 | reference |
| Once | 2.8 | 31.1 | 1.7 (1.4-2.1) | |
| More than Once | 4.6 | 43.3 | 2.9 (2.5-3.4) | |
| 3) Force you to have sex? (missing = 84) | Never | 96.0 | 22.1 | reference |
| Once | 1.5 | 43.8 | 2.9 (2.2-3.8) | |
| More than Once | 2.5 | 49.5 | 3.3 (2.7-4.0) | |
| II. Emotional Abuse Category (criterion: more than once) | 26.7 | 30.7 | 2.1 (1.9-2.3) | |
| 4) How often did a parent or adult in your home ever swear at you, insult you, or put you down? | Never | 66.1 | 20.4 | Reference |
| Once | 7.2 | 20.1 | 1.3 (1.1-1.5) | |
| More than Once | 26.7 | 30.7 | 2.2 (2.0-2.4) | |
| III. Physical Abuse Category (criterion: once or more than once) | 15.6 | 34.9 | 2.2 (2.1-2.3) | |
| 5) Before age 18, how often did a parent or adult in your home ever hit, beat, kick or physically hurt you in any way? Do not include spanking. | Never | 84.4 | 21.0 | Reference |
| Once | 4.1 | 27.4 | 1.6 (1.3-1.9) | |
| More than Once | 11.5 | 37.6 | 2.4 (2.2-2.7) | |
| Family Dysfunction ACE Categories | ||||
| IV. Domestic Violence Category (criterion: once or more than once) | 15.4 | 31.8 | 1.8 (1.6-2.0) | |
| 6) How often did your parents or adults in your home ever slap, hit, kick, punch or beat each other up? | Never | 84.6 | 21.6 | reference |
| Once | 4.1 | 26.4 | 1.4 (1.2-1.7) | |
| More than Once | 11.3 | 33.8 | 1.9 (1.7-2.1) | |
| V. Incarcerated Household Member (criterion: yes) | 6.4 | 31.3 | 1.9 (1.6-2.2) | |
| 7) Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | Yes | 6.4 | 31.3 | 1.9 (1.6-2.2) |
| No | 93.6 | 22.6 | Reference | |
| VI. Substance Abuse Category: (criterion yes to 1 or both) | 26.4 | 29.1 | 1.7 (1.6-1.8) | |
| 8) Did you live with anyone who was a problem drinker or alcoholic? | Yes | 22.8 | 30.1 | 1.7 (1.6-1.8) |
| No | 77.2 | 21.1 | reference | |
| 9) Did you live with anyone who used illegal street drugs or who abused prescription medication?3 | Yes | 10.0 | 29.2 | 1.9 (1.7-2.2) |
| No | 90.0 | 22.5 | reference | |
| VII. Mental Illness Category (criterion: yes) | 17.1 | 31.3 | 2.1 (1.9-2.3) | |
| 10) Did you live with anyone who was depressed, mentally ill or suicidal? | Yes | 17.1 | 31.3 | 2.1 (1.9-2.3) |
| No | 82.9 | 21.5 | reference | |
| VIII. Divorce Category (criterion: yes) | 23.9 | 25.4 | 1.4 (1.3-1.5) | |
| 11) Were your parents separated or divorced? | Yes | 24.2 | 25.6 | 1.4 (1.3-1.5) |
| No | 75.0 | 22.3 | reference | |
| Not Married | 0.8 | 29.1 | 1.7 (1.1-2.8) | |
| Summary ACE Measures | ||||
| ACE Score | ||||
| 0 | 43.2 | 18.7 | reference | |
| 1 | 22.1 | 20.5 | 1.3 (1.2-1.4) | |
| 2 | 12.4 | 25.9 | 1.9 (1.6-2.1) | |
| 3 | 7.9 | 29.0 | 2.3 (2.0-2.6) | |
| 4 | 5.9 | 30.6 | 2.6 (2.2-3.0) | |
| 5 | 4.1 | 34.9 | 3.2 (2.7-3.8) | |
| 6 | 2.6 | 36.3 | 3.6 (2.8-4.6) | |
| 7-8 | 1.7 | 49.0 | 6.1 (4.6-8.0) | |
| ACE Type | ref = no ACE | |||
| Abuse & Family Dysfunction | 25.3 | 31.6 | 2.6 (2.4-2.7) | |
| Abuse Only | 9.3 | 27.2 | 1.9 (1.7-2.0) | |
| Family Dysfunction Only | 22.1 | 20.5 | 1.3 (1.2-1.4) | |
All percentages are weighted to account for survey design and weights and include the full sample.
Adjusted for sex, age, race/ethnicity, education, income. Each Question and Category (reference is not meeting category criterion) and summary measure modeled separately.
missing = 4
Disability was defined as a positive answer to either (or both) of the BRFSS disability questions: “Are you limited in any way in any activities because of physical, mental, or emotional problems?” and “Do you now have any health problem that requires you to use special equipment, such as a cane, a wheelchair, a special bed, or a special telephone?” The first question directly measures activity limitation; a positive answer to the second question suggests the presence of one.
Demographics included age, sex, race/ethnicity, marital status, and education dichotomized (high school graduate/non graduate). Self-reported health conditions were defined by positive answers to the questions about diagnoses of asthma, coronary heart disease, myocardial infarction, stroke, diabetes (did not include gestational and pre-diabetes). Answers of “do not know” were coded as negative.
Statistical Analysis
We performed descriptive analyses and logistic regression38 using SAS® 9.3 (SAS Institute, Inc., Cary, NC, 2011) survey analysis procedures to account for the complex survey design. Model covariates were chosen by a priori reasoning rather than by model selection. After our descriptive analyses confirmed that age was a strong confounder, prevalence rates of ACE and disability by health condition were age adjusted using the direct standardization method and the US Census 2000 standard population.39 Prevalence rates were presented along with odds ratios to aid in interpretation of the data, especially since odds ratios cannot be interpreted as equivalent to increases in risk when the prevalence is high. Since health conditions may be considered intermediate in the disability causal pathway, two sets of models were analyzed: one including only demographic covariates and one including both demographic and health condition covariates.
The BRFSS did not ask about mental health diagnoses in the core questionnaire, but five states implemented an anxiety/depression module along with the ACE module in 2010. Because childhood adversity is strongly associated with these mental health diagnoses, both of which are associated with disability and decreases in role functioning,2,3,40-43 we performed a subset analysis examining whether the addition of these diagnoses to the model would attenuate the ACE-disability relationship. Because of the smaller sample size, we aggregated ACE Scores ≥ 4.
RESULTS
The study sample consisted of 31,172 (48.6 weighted %) men and 50,012 (51.4%) women (Table1). The mean age was 47.9 (standard deviation 15.9). Non-Hispanic whites comprised 82.3% of the sample and 93.1% were high school graduates. Fifty-seven percent of the sample reported one or more ACEs, 8.4% reported five or more ACEs, and 23.1% reported disability. The prevalence of any ACE was similar in men and women, but women had a higher prevalence of five or more ACEs. The prevalence of any ACE decreased by age group, from 63.8% (19-29 years) to 35.5% (75+ years) with sharper declines starting at age 55. The decreases between age groups were more distinct for those reporting 5 or more ACEs, with the prevalence decreasing from 13.2% in the youngest to 1.1% in the oldest group. In contrast, disability rates increased from 13.2 in the youngest to 43.0% in the eldest group. Asians/Pacific Islanders had a considerably lower prevalence of ACE (38.3%) than other racial/ethnic groups as well as the lowest prevalence of disability (11.5%). ACE exposure was more common in those with lower income, those without a high school education and those who were divorced/separated. Those with health conditions had higher age-adjusted rates of ACE exposure and disability than those without these conditions.
The most common ACEs were having lived with a substance abuser (26.4%), verbal abuse (26.7%) and parental separation/divorce (23.9%); the least common ACEs were having an incarcerated family member (6.4%), followed by sexual abuse (11.5%). (Table 2) Experiencing both abuse and family dysfunction was slightly more common (25.3%) than experiencing only family dysfunction (22.1%); experiencing abuse only (9.3%) was less frequently reported.
For each of the individual ACE questions asking about abuse and domestic violence, those reporting experiencing abuse or parental domestic violence more than once had a higher disability prevalence than those who reported it only occurred once. (Table 2) Among the sexual abuse questions, those reporting having been forced to have sex more than once had the highest disability prevalence (49.5%). For every individual ACE category, those who experienced it had higher disability prevalence than those who did not. Sexual abuse had the highest disability prevalence (37.9%) and parental separation/divorce had the lowest (25.4%). As the ACE Score increased from 1 to 7+, disability prevalence increased in a stepwise fashion. The self-reported disability prevalence for those who had not experienced any of those ACE categories was 18.7%. Those experiencing only abuse had a higher disability prevalence (27.2%) than those experiencing only family dysfunction (20.5%); the highest disability prevalence was reported by those who experienced both (31.6%).
After adjusting for demographic factors (age, sex, race/ethnicity, education, marital status, income), the odds of reporting disability was higher for each ACE category compared to those without that specific experience (Table 2). The odds of disability increased in a graded fashion with ACE count. Compared to those with no ACEs, the odds of disability was highest in those experiencing both abuse and family dysfunction (2.6), followed by those experiencing abuse only (1.9) and then family dysfunction only (1.3).
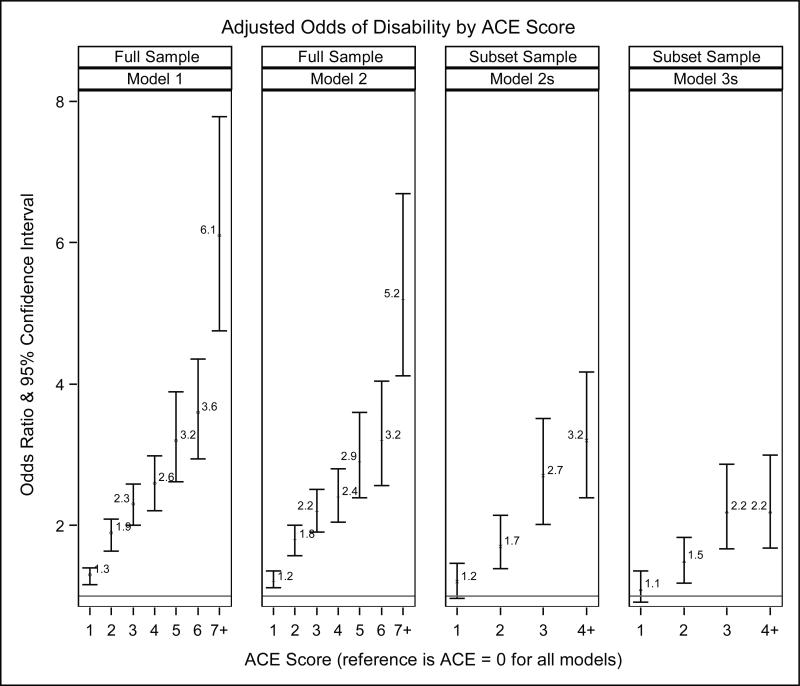
After adding chronic physical conditions to the model, there was still a graded increase in the odds of disability as ACE count increased (Fig. 2), however, there was slight attenuation of the odds ratios, particularly for higher ACE scores. For the subset analysis, in the model controlling for demographics and physical health conditions, the odds of disability also increased in a step-wise fashion. After adding anxiety and depression to the model, the odd ratios of disability were attenuated, particularly for ACE Score 3 and above where there appeared to be a leveling off. However, ACEs still had a significant effect on disability even after controlling for mental health conditions. The Wald Chi-Square test for trend had a p-value < 0.001 for all models.
Figure 2. Odds of Disability by ACE Score (Counted number of ACE categories).
Model 1 is adjusted for demographics (age, sex, race/ethnicity, marital status, education, income) Model 2 is adjusted for demographics and physical health conditions (asthma, stroke, myocardial infarction, coronary heart disease, diabetes)
Model 2s is the same as model 2, but performed in the sample subset (n = 22,739) which answered the Anxiety/Depression module. It is needed as a baseline comparison to Model 3s in order to be able to understand how the addition of anxiety and depression changes the association between ACE and disability.
Model 3s adds anxiety and depression to the covariates adjusted for in Model 2s, allowing one to see how the association between ACE Score and disability changes with the inclusion of these covariates.
DISCUSSION
As hypothesized, adverse childhood experiences had a strong graded effect on self-reported disability in adult life after controlling for demographic factors and chronic conditions in this large multi-state population-level study. Since health conditions may be considered intermediaries on the pathway between ACE and disability, it is notable that ACEs affected disability strongly even after controlling for these conditions. This is particularly noteworthy for our subset analysis, since prior studies have shown that serious psychological distress has a large effect on activity limitations in those with and without chronic health conditions.44 As we anticipated, there were differing effects of ACEs by category and type. While sexual abuse was the least common form of abuse, it appeared to be the most toxic, resulting in the highest prevalence of later life disability.
Our study is consistent with other reports that examined relationships between ACEs and various aspects of disability. Prior work in those with past-year psychiatric disorders found a graded relationship between role impairment and ACEs, even after controlling for comorbid psychiatric illnesses, but did not examine physical illnesses.41 Two Canadian community-based studies which separately examined disability related to mental45 and physical illness in community-dwelling women,46 also found that sexual abuse, physical abuse, and living with a mentally ill parent(s) had the strongest associations with disability. These reports did not examine physical and mental illness together or test for a graded relationship.45,46 On the population level, a study from the Netherlands used econometric modeling to estimate the years lived with disability per 1000 people attributable to individual adverse childhood exposures and found an independent effect of childhood adversity after accounting for mental and medical diagnoses. However, they did not test for a graded relationship or evaluate different types of disability.47
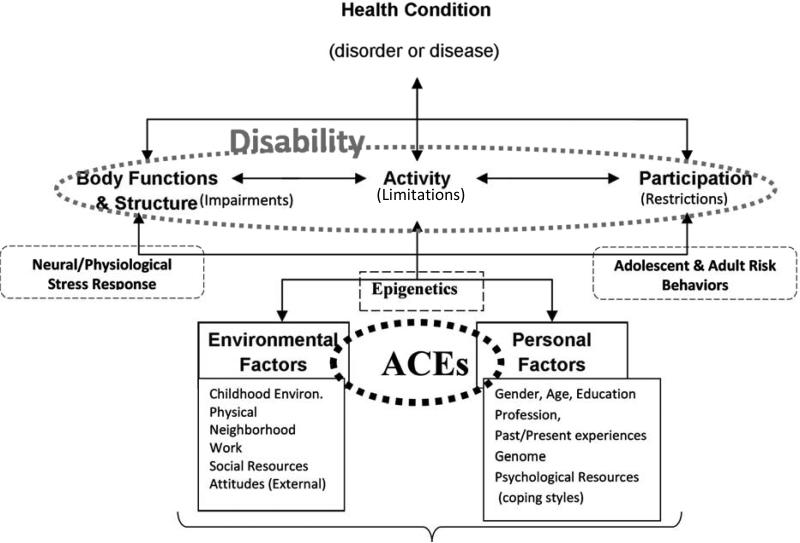
In order to understand and illustrate potential mechanisms that might explain the association we found between ACE burden and increased rates of disability, we used the ICF framework. (Fig. 3) The complexity of interactions and multiple potential mechanisms through which ACEs may affect disability are more easily illustrated using this framework than the ACE pyramid. There is growing evidence that childhood adversity can cause persistent alterations in the biological stress response, which may affect how individuals react to disabling impairments in adulthood. Studies examining stress sensitization have found that those with childhood adversity are more likely to develop psychiatric conditions when exposed to later-life stressors.31,48 In addition, childhood maltreatment may increase the sensitivity to stressful social contexts, which can increase the incidence of health-risk behaviors.49 An increase in these behaviors in response to stressors is yet another mechanism by which ACE exposure might increase disability, independent of chronic disease. Physical environment also contributes to disability50,51 and the interaction between environment, ACE exposure and disability requires further study. Furthermore, children who experience abuse are more likely to experience adult interpersonal violence.52-54 Prior studies have found that men and women with disabilities are more likely to report lifetime and past-year sexual abuse and intimate-partner physical abuse than those without disabilities.55,56 Given that cumulative stress load is important in the current conceptual models of stress and disease, future studies will need to explore how the full life span adversity exposure affects disability.57
Figure 3. Potential Mechanisms by which Adverse Childhood Experiences (ACEs) may affect disability using the International Classification of Functioning, Disease and Health (ICF) Framework.
Adverse Childhood Experiences and childhood environment are environmental factors in childhood, but may be considered personal factors in adulthood where they are past experiences. The interaction of ACEs with other childhood environmental factors and personal factors may through epigenetic mechanisms lead to persistent changes in the neural/physiological stress response. They may adversely affect adult environmental factors such as social resources, as well as personal factors such as educational attainment and psychological resources. ACEs are highly associated with adult risk behaviors which can cause alterations in body functions and structure, and also adversely affect participation and activity.
Limitations
The BRFSS is limited to those in the community with telephones. Excluding those without or who are unable to use a telephone may underestimate the prevalence of abuse and disability, but this may not be the case since a Washington state study found higher disability rates in telephone surveys than in the Census 2000 Supplementary survey, which uses multimode data collection58 The BRFSS has started surveying cell phone users, but their data is not yet released with the main sample.32 Thus younger people are currently underrepresented.34,35 There is also the potential for non-response bias. Post stratification weighting may not completely address these biases if either cell phone only users or non-respondents differ from the rest of the population.59 Because not all 50 states administered the ACE module, the results may not be generalizable to the entire community-dwelling US population. On the other hand, our findings are based on a rich population-level source of data which are generalizable to the combined population of the states that used the module. Furthermore, the states that administered the ACE Module represent a broad range of different US regions and there is no reason to think that the results would differ significantly in the general US community-dwelling population.
The BRFSS is based on self-reported data which may result in underestimates of ACE prevalence since the primary problem with self-reports are false negative reports.60 Under reporting may occur because of reluctance to discuss sensitive information61, trauma-related autobiographical memory disturbances,62 and memory attenuation with aging. Underreporting in general would tend to bias towards the null unless healthy adults were more likely to underreport than those with disabilities. One early non-population based prospective study raised the concern that retrospective associations of childhood abuse and poor health are stronger than those determined prospectively.63-65 A more recent population-based study, however, found no difference in the strength of association between childhood abuse and adult depression, anxiety, or substance abuse between those with prospectively determined abuse versus retrospectively self-reported abuse. The only exception was that those with prospectively determined abuse had worse depression treatment outcomes. Another prospective study found that frequency and chronicity of abuse is associated with poorer child and adult health outcomes which is also consistent with our findings.66
Ultimately there is no perfect method to determine childhood abuse. Much childhood abuse goes undetected; those with documented abuse in childhood are unlikely to be representative of those whose abuse was never documented. Furthermore, those who do not disclose abuse do not have the opportunity to receive social support which can mitigate later symptomatology. In addition, prospective studies tend to be small and non-population based. Thus, given the limitations of both prospective and retrospective studies, large population-based studies such as ours provide valuable information that needs to be combined with other research to gain a full picture of the impact of childhood adversity throughout the life course.
In addition, to underreporting, ACEs may be undercounted in the oldest age groups because of premature mortality in those most affected by ACEs. The Kaiser-CDC study found that those reporting 6 or more ACE categories were 2.7 times more likely to die before age 65 and 1.7 times more likely to die before age 75, than those reporting no ACEs.16 Premature mortality in the oldest age groups may attenuate the strength of our findings and is a likely contributor to the decrease in reported ACE prevalence noted in this age group.
BRFSS measures are broad and do not include developmental timing of childhood adversity, severity of health conditions or specific details about disability, which may attenuate the strength of the association. To evaluate whether we would have different results with a more narrow definition of disability, we repeated our analysis using an affirmative answer to the question about use of an assistive device as the definition of disability and found that the patterns of findings were similar. Since the study is cross-sectional and the timing of disability in relationship to the childhood adverse experiences is unknown, we could not exclude those with developmental disabilities. We do not expect this to greatly affect our results, since prevalence of developmental disabilities in the non-institutionalized adult population is very small (0.79%)67 compared to the large increases in disability prevalence associated with increased age shown by our findings.
The core questionnaire only asks about a few health conditions, and other conditions, such as musculoskeletal disorders, may also mediate the relationship between ACE and disability. Recognizing the importance of mental health diagnoses, we were able to analyze a subset of the sample that belonged to the 5 states which administered the anxiety/depression and ACE modules together. This subset analysis suggests that while mental health disorders are important, they are not the sole mediators of increased disability. However, the more limited sample may affect the generalizability of these results. We could not fully assess other health, personal, social, and environmental factors that can affect disability since the information was not available. In addition many of the measures that were available lacked sophistication, thus it is likely that our control for confounding was insufficient. Incompletely controlling for these factors, however, does not negate the importance of our findings, but rather points to the need for further research to identify mediating factors, or groups at particular risk important for designing interventions. Attention must be paid to other factors, including social and environmental ones, with the potential to increase rates of disability in those exposed to childhood adversity.
CONCLUSIONS
In contrast to previous studies, we incorporate a broader measure of disability, include both physical and mental health conditions and more comprehensively examine childhood adversity. In addition, prior studies have focused more on health risk behaviors and disease outcomes. Our paper focuses on disability, emphasizing that disabilities are distinct from health conditions and that ACEs influence the development of disability beyond what would be expected solely from the increased rates of chronic disease associated with ACE exposure.
Within the past year, there has been a call by the CDC and other national health organizations for more research on health disparities in those with disability17 and a call by the American Academy of Pediatrics for all health care professionals to incorporate an ecobiodevelopmental framework68 as “a means of understanding social, behavioral and economic determinants of lifelong disparities in physical and mental health.”69 Our study integrates these two vital public health concerns and supports the use of such a framework in understanding disparities related to disability in a way that is relevant to inter-disciplinary rehabilitative principles. Although primary prevention of child abuse and other childhood adversities has been the focus of public health discussions, an improved understanding of how ACEs affect the development of disability is important for clinicians, particularly rehabilitation clinicians. Such knowledge may lead to rehabilitation interventions to address the impact of ACEs on functional recovery.
By addressing the impact of ACEs which have been shown to influence responses to later stressors, rehabilitation clinicians may improve the functional recovery of patients affected by ACEs. It may be necessary to include psychologists with expertise in traumatic stress on the rehabilitation team. Future research is needed to determine the best way to address ACEs to improve coping and functional recovery from stresses related to patients’ emerging or existing disabilities. While it is too late to prevent ACEs and/or prevent disease in these adults, it may still be possible to ameliorate the effects of impairments and help those affected by childhood adversity lead more functional lives.
Acknowledgments
Support: The research for this manuscript was supported by Post-Doctoral Fellowship for Dr. Sophia Miryam Schüssler-Fiorenza Rose (5-T32-HD-007425) awarded to the University of Pennsylvania from the National Institute of Child Health and Human Development (NICHD) National Center for Medical Rehabilitation Research (NCMRR).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Early results were presented as a Poster Presentation at the 23rd International Trauma Conference in Boston, MA, June 2012. Related abstracts were presented as Poster Presentations at the 2012 AAPMR Annual Assembly, Atlanta, GA, Nov. 2012.
Author Contributions: Sophia Miryam Schüssler-Fiorenza Rose: Conceptualized the study and its design, obtained and analyzed the data and wrote the manuscript. Dawie Xie: Contributed to study design, statistical analysis and interpretation of the data. Margaret Stineman: Contributed to study concept and design, statistical analysis and interpretation of the data. All authors contributed to the revision of the manuscript and approved the final version.
REFERENCES
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27(5):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- 3.Green JG, Mclaughlin KA, Berglund PA, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Tilburg MA, Runyan DK, Zolotor AJ, et al. Unexplained gastrointestinal symptoms after abuse in a prospective study of children at risk for abuse and neglect. Ann Fam Med. 2010;8(2):134–140. doi: 10.1370/afm.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anda RF, Chapman DP, Felitti VJ, et al. Adverse childhood experiences and risk of paternity in teen pregnancy. Obstet Gynecol. 2002;100(1):37–45. doi: 10.1016/s0029-7844(02)02063-x. [DOI] [PubMed] [Google Scholar]
- 6.Brown DW, Riley L, Butchart A, Meddings DR, Kann L, Harvey AP. Exposure to physical and sexual violence and adverse health behaviours in African children: results from the Global School-based Student Health Survey. Bull World Health Organ. 2009;87(6):447–455. doi: 10.2471/BLT.07.047423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004;113(2):320–327. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- 8.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27(5):713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 9.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 10.Ford ES, Anda RF, Edwards VJ, et al. Adverse childhood experiences and smoking status in five states. Prev Med. 2011;53(3):188–193. doi: 10.1016/j.ypmed.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 12.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shonkoff JP, Boyce WT, Mcewen BS. Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities. JAMA. 2009;301(21):2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 14.Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache. 2010;50(9):1473–1481. doi: 10.1111/j.1526-4610.2010.01756.x. [DOI] [PubMed] [Google Scholar]
- 15.Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71(2):243–250. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5):389–396. doi: 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention CDC Health Disparities and Inequalities Report, United States 2011. MMWR Morb Mortal Wkly Rep. 2011;60(Supplement):7–8. Available at http://www.cdc.gov/mmwr/pdf/other/su6001.pdf. Accessed Jan 13, 2014. [Google Scholar]
- 18.Healthy People 2020 Objectives. Disability and Health. 2009 at http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=9. Accessed Jan 13, 2014.
- 19.Agency for Healthcare Research and Quality Closing the Quality Gap Series: Measuring Outcomes of Care for Persons With Disabilities. 2011 Available at http://www.effectivehealthcare.ahrq.gov/ehc/products/336/739/CQG-Disability-Outcomes_Protocol_20110803.pdf. Accessed Jan 13, 2014.
- 20.World Health Organization . International Classification of Functioning, Disability and Health: ICF. World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- 21.World Health Organization Towards a Common Language for Functioning, Disability and Health ICF. 2002 Available at http://www.who.int/entity/classifications/icf/training/icfbeginnersguide.pdf. Accessed Jan 13, 2014.
- 22.Committee on Disability in America . The Future of Disability in America. The National Academies Press; 2007. [PubMed] [Google Scholar]
- 23.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 24.Taylor SE, Way BM, Seeman TE. Early adversity and adult health outcomes. Dev Psychopathol. 2011;23(3):939–954. doi: 10.1017/S0954579411000411. [DOI] [PubMed] [Google Scholar]
- 25.McEwen BS, Eiland L, Hunter RG, Miller MM. Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress. Neuropharmacology. 2012;62(1):3–12. doi: 10.1016/j.neuropharm.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toyokawa S, Uddin M, Koenen KC, Galea S. How does the social environment ‘get into the mind’? Epigenetics at the intersection of social and psychiatric epidemiology. Soc Sci Med. 2012;74(1):67–74. doi: 10.1016/j.socscimed.2011.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mcgowan PO, Sasaki A, D'alessio AC, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. 2009;12(3):342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szyf M. The early life social environment and DNA methylation: DNA methylation mediating the long-term impact of social environments early in life. Epigenetics. 2011;6(8):971–978. doi: 10.4161/epi.6.8.16793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 30.Ford E, Clark C, Stansfeld SA. The influence of childhood adversity on social relations and mental health at mid-life. J Affect Disord. 2011;133(1-2):320–327. doi: 10.1016/j.jad.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 31.Mclaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Overview: BRFSS. 2010 Available at http://www.cdc.gov/brfss/technical_infodata/surveydata/2010/overview_10.rtf. Accessed Jan 13, 2014.
- 33.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Data 2009-2010. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: [Google Scholar]
- 34.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System 2010 Summary Data Quality Report. 2010 Available at ftp://ftp.cdc.gov/pub/Data/Brfss/2010_Summary_Data_Quality_Report.pdf. Accessed Jan 13, 2014.
- 35.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System 2009 Summary Data Quality Report. 2009 Available at ftp://ftp.cdc.gov/pub/Data/Brfss/2009_Summary_Data_Quality_Report.pdf.
- 36.Schoenborn CA. Exposure to alcoholism in the family: United States, 1988. Adv Data. 1991;(205):1–13. [PubMed] [Google Scholar]
- 37.Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1609–1613. [PubMed] [Google Scholar]
- 38.Cook TD. Advanced Statistics: Up with Odds Ratios! A Case for Odds Ratios When Outcomes Are Common. Acad Emerg Med. 2002;9(12):1430–1434. doi: 10.1111/j.1553-2712.2002.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 39.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes. 2001;(20):1–10. [PubMed] [Google Scholar]
- 40.Kessler RC, Ormel J, Demler O, Stang PE. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. J Occup Environ Med. 2003;45(12):1257–1266. doi: 10.1097/01.jom.0000100000.70011.bb. [DOI] [PubMed] [Google Scholar]
- 41.Mclaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) III: associations with functional impairment related to DSM-IV disorders. Psychol Med. 2010;40(5):847–859. doi: 10.1017/S0033291709991115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Druss BG, Hwang I, Petukhova M, Sampson NA, Wang PS, Kessler RC. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2009;14(7):728–737. doi: 10.1038/mp.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chartier MJ, Walker JR, Naimark B. Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. Am J Public Health. 2009;99(5):847–854. doi: 10.2105/AJPH.2007.122408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mcknight-Eily LR, Elam-Evans LD, Strine TW, et al. Activity limitation, chronic disease, and comorbid serious psychological distress in U.S. adults--BRFSS 2007. Int J Public Health. 2009;54(Suppl 1):111–119. doi: 10.1007/s00038-009-0015-0. [DOI] [PubMed] [Google Scholar]
- 45.Tonmyr L, Jamieson E, Mery LS, Macmillan HL. The relation between childhood adverse experiences and disability due to mental health problems in a community sample of women. Can J Psychiatry. 2005;50(12):778–783. doi: 10.1177/070674370505001207. [DOI] [PubMed] [Google Scholar]
- 46.Tonmyr L, Jamieson E, Mery LS, Macmillan HL. The relationship between childhood adverse experiences and disability due to physical health problems in a community sample of women. Women Health. 2005;41(4):23–35. doi: 10.1300/J013v41n04_02. [DOI] [PubMed] [Google Scholar]
- 47.Cuijpers P, Smit F, Unger F, Stikkelbroek Y, Ten Have M, De Graaf R. The disease burden of childhood adversities in adults: a population-based study. Child Abuse Negl. 2011;35(11):937–945. doi: 10.1016/j.chiabu.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 48.Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. J Consult Clin Psychol. 2000;68(5):782–787. [PubMed] [Google Scholar]
- 49.Keyes KM, Mclaughlin KA, Koenen KC, Goldmann E, Uddin M, Galea S. Child maltreatment increases sensitivity to adverse social contexts: Neighborhood physical disorder and incident binge drinking in Detroit. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2011.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stineman MG, Ross RN, Maislin G, Gray D. Population-based study of home accessibility features and the activities of daily living: clinical and policy implications. Disabil Rehabil. 2007;29(15):1165–1175. doi: 10.1080/09638280600976145. [DOI] [PubMed] [Google Scholar]
- 51.Liu SY, Lapane KL. Residential modifications and decline in physical function among community-dwelling older adults. Gerontologist. 2009;49(3):344–354. doi: 10.1093/geront/gnp033. [DOI] [PubMed] [Google Scholar]
- 52.Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: a review of the empirical literature. Trauma Violence Abuse. 2005;6(2):103–129. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- 53.Widom CS, Czaja SJ, Dutton MA. Childhood victimization and lifetime revictimization. Child Abuse Negl. 2008;32(8):785–796. doi: 10.1016/j.chiabu.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Desai S, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent adult revictimization assessed in a nationally representative sample of women and men. Violence Vict. 2002;17(6):639–653. doi: 10.1891/vivi.17.6.639.33725. [DOI] [PubMed] [Google Scholar]
- 55.Mitra M, Mouradian VE, Diamond M. Sexual violence victimization against men with disabilities. Am J Prev Med. 2011;41(5):494–497. doi: 10.1016/j.amepre.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 56.Smith DL. Disability, Gender and Intimate Partner Violence: Relationships from the Behavioral Risk Factor Surveillance System. Sex Disabil. 2007;26(1):15–28. [Google Scholar]
- 57.Scott-Storey K. Cumulative Abuse: Do Things Add Up? An Evaluation of the Conceptualization, Operationalization, and Methodological Approaches in the Study of the Phenomenon of Cumulative Abuse. Trauma Violence & Abuse. 2011;12(3):135–150. doi: 10.1177/1524838011404253. [DOI] [PubMed] [Google Scholar]
- 58.Kinne S, Topolski TD. Inclusion of people with disabilities in telephone health surveillance surveys. Am J Public Health. 2005;95(3):512–517. doi: 10.2105/AJPH.2004.040881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee S, Brick JM, Brown ER, Grant D. Growing cell-phone population and noncoverage bias in traditional random digit dial telephone health surveys. Health Serv Res. 2010;45(4):1121–1139. doi: 10.1111/j.1475-6773.2010.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 61.Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 62.Brown DW, Anda RF, Edwards VJ, Felitti VJ, Dube SR, Giles WH. Adverse childhood experiences and childhood autobiographical memory disturbance. Child Abuse Negl. 2007;31(9):961–969. doi: 10.1016/j.chiabu.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 63.Widom CS, Dumont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64(1):49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- 64.Widom CS, Weiler BL, Cottler LB. Childhood victimization and drug abuse: A comparison of prospective and retrospective findings. J Consult Clin Psychol. 1999;67(6):867–880. doi: 10.1037//0022-006x.67.6.867. [DOI] [PubMed] [Google Scholar]
- 65.Widom CS, Raphael KG, Dumont KA. The case for prospective longitudinal studies in child maltreatment research: commentary on Dube, Williamson, Thompson, Felitti, and Anda (2004). Child Abuse Negl. 2004;28(7):715–722. doi: 10.1016/j.chiabu.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 66.Jonson-Reid M, Kohl PL, Drake B. Child and adult outcomes of chronic child maltreatment. Pediatrics. 2012;129(5):839–845. doi: 10.1542/peds.2011-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Larson SA, Lakin KC, Anderson L, Kwak N, Lee JH, Anderson D. Prevalence of mental retardation and developmental disabilities: estimates from the 1994/1995 National Health Interview Survey Disability Supplements. Am J Ment Retard. 2001;106(3):231–252. [PubMed] [Google Scholar]
- 68.Shonkoff JP, Garner AS, Siegel BS, et al. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 69.American Academy of Pediatrics Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science Into Lifelong Health. Pediatrics. 2012;129(1):e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention Adverse Childhood Experiences (ACE) study. [February 23, 2013]; Available at http://www.cdc.gov/ace/pyramid.htm. [Google Scholar]