Abstract
Despite growing evidence for the efficacy of Gratz and colleagues’ emotion regulation group therapy (ERGT) for deliberate self-harm (DSH) among women with borderline personality disorder (BPD), the proposed mechanism of change in this treatment (i.e., emotion regulation) remains largely unexamined. This study examined change in emotion dysregulation as a mediator of the effects of this ERGT on DSH and BPD symptoms, as well as the extent to which change in emotion dysregulation during treatment predicts further improvements in DSH during a 9-month follow-up. Participants included 61 female outpatients with BPD and recent DSH who were randomly assigned to receive this ERGT in addition to their ongoing outpatient therapy immediately (n = 31) or after 14 weeks (n = 30). Measures of emotion dysregulation, DSH, and BPD symptoms were administered pre- and post-treatment or -waitlist, and at 9-months post-treatment (for participants in both conditions who received ERGT). Results from a series of mediation analyses provide further support for emotion regulation as a mechanism of change in this treatment. Specifically, results revealed that improvements in emotion dysregulation over the course of treatment mediated the observed reductions in BPD cognitive and affective symptoms during treatment and predicted further improvements in DSH during follow-up.
Keywords: borderline personality, treatment, group therapy, self-injury, mechanisms of change, emotion regulation
Introduction
Deliberate self-harm (DSH; also referred to as nonsuicidal self-injury), defined as the deliberate, direct, self-inflicted destruction of body tissue without suicidal intent and for purposes not socially sanctioned (e.g., cutting, burning, severe scratching; Gratz, 2001; ISSS, 2007), is a clinically-important behavior commonly associated with borderline personality disorder (BPD; Linehan, 1993) and implicated in the high levels of health care utilization among individuals with BPD (Zanarini, 2009). Despite the clinical relevance of this behavior, there are few empirically-supported treatments for DSH within BPD. Short-term treatments for DSH in general have not been found to be effective for patients with BPD, and may lead to an increase in the repetition of DSH among individuals with BPD (Tyrer et al., 2004). Moreover, the two treatments with demonstrated efficacy in the treatment of DSH among patients with BPD, Dialectical Behavior Therapy (DBT; Linehan, 1993) and Mentalization-Based Treatment (Bateman & Fonagy, 2004), are difficult to implement in traditional clinical settings (due to their duration and intensity) and are not readily available in many communities (Zanarini, 2009). Thus, there is a need for shorter, less intensive, and more clinically feasible interventions that directly target DSH among individuals with BPD, particularly adjunctive treatments that may augment the therapies provided by clinicians in the community (Zanarini, 2009).
To address this need, Gratz and colleagues (Gratz & Gunderson, 2006; Gratz & Tull, 2011) developed an adjunctive emotion regulation group therapy (ERGT) for DSH among women with BPD, designed to augment the usual treatments provided in the community by directly targeting both DSH and its underlying mechanism. Specifically, drawing on theoretical and empirical literature highlighting the central role of emotion dysregulation in the development and maintenance of DSH (e.g., Chapman, Gratz, & Brown, 2006; Gratz, 2007; Gratz & Gunderson, 2006; Gratz & Roemer, 2008; Gratz & Tull, 2010b; Heath, Toste, Nedecheva, & Charlebois, 2008; Linehan, 1993; Slee, Spinhoven, Garnefski, & Arensman, 2008), this ERGT was developed with the expectation that teaching self-harming women with BPD more adaptive ways of responding to and regulating their emotions would reduce their DSH.
To date, three studies have provided support for the utility of this ERGT in the treatment of DSH among women with BPD, including an open trial (Gratz & Tull, 2011) and two randomized controlled trials (Gratz & Gunderson, 2006; Gratz, Tull, & Levy, 2014). The most recent of these, a larger randomized controlled trial (RCT) and uncontrolled 9-month follow-up (see Gratz et al., 2014), provided further evidence for the efficacy of this adjunctive ERGT (relative to a treatment as usual [TAU] only waitlist condition), revealing positive effects of this treatment on both the primary treatment targets (i.e., DSH, emotion dysregulation, and BPD symptoms) and other relevant outcomes (i.e., depression and stress symptoms, and overall quality of life) within a conservative intent-to-treat (ITT) sample. Moreover, findings from the 9-month follow-up period provide preliminary support for the durability of treatment gains, as all improvements observed from pre- to post-treatment were maintained or further improved upon at follow-up, including additional significant improvements from post-treatment through 9-month follow-up for DSH, emotion dysregulation, and BPD symptoms (among others; Gratz et al., 2014).
Despite growing evidence for the efficacy of this ERGT for DSH within BPD, the proposed mechanism of change in this treatment remains largely unexamined, with only one study to date examining the mediating role of emotion regulation in improvements in DSH over the course of this treatment (Gratz, Levy, & Tull, 2012). However, such research has the potential to elucidate both the precise role of emotion dysregulation in the course of DSH and the clinical utility of targeting emotion dysregulation in the treatment of DSH among women with BPD (thereby providing important information on how best to optimize therapeutic change for this population; Kazdin, 2007). Thus, this study utilized data from the most recent RCT to examine emotion regulation as the mechanism of change in this treatment. Specifically, this study examined change in emotion dysregulation as a mediator of the effects of this ERGT on DSH and BPD symptoms, as well as the extent to which change in emotion dysregulation during treatment predicted further improvements in DSH from post-treatment through the 9-month follow-up. We hypothesized that change in emotion dysregulation would mediate the reductions in DSH frequency and BPD symptom severity observed over the course of treatment and predict further improvements in DSH during the follow-up period.
Method
Sample and procedures
All methods were approved by the institution’s Institutional Review Board. Participants were obtained through referrals by clinicians and self-referrals in response to advertisements for an “emotion regulation skills group for women with self-harm” posted online and throughout the community. Inclusion criteria included: (a) threshold or subthreshold diagnosis of BPD (given evidence that even subthreshold BPD is clinically-meaningful; Clifton & Pilkonis, 2007); (b) a history of repeated DSH, with at least one episode in the past six months; (c) having an individual therapist, psychiatrist, or case manager; and (d) being a woman aged 18–60. To increase generalizability of the sample, exclusion criteria included only diagnoses of a primary psychotic disorder, bipolar I disorder, and current (past month) substance dependence. Participants meeting inclusion and exclusion criteria were matched on four prognostic variables (emotion dysregulation, number of lifetime incidents of DSH, global assessment of functioning scores, and age) and randomly assigned by the principal investigator (PI) to either the ERGT + TAU (n = 31) or TAU waitlist (n = 30) condition using a stratified randomization procedure. See Table 1 for demographic, clinical, and diagnostic data on participants in each condition.
Table 1.
Pretreatment Demographic, Clinical, and Diagnostic Data for Intent-to-Treat Sample
| ERGT + TAU (n = 31)
|
TAU Waitlist (n = 30)
|
|
|---|---|---|
| Demographic Characteristics | ||
| Age | mean = 33.3 ± 11.0 | mean = 33.0 ± 10.9 |
| Racial/ethnic minority | 16.1% (n = 5) | 26.7% (n = 8) |
| Lesbian/bisexual/questioning | 12.9% (n = 4) | 13.7% (n = 4) |
| Marital status: | ||
| Single | 51.7% (n = 16) | 56.7% (n = 17) |
| Married | 25.8% (n = 8) | 13.3% (n = 4) |
| Separated/Divorced | 22.6% (n = 7) | 30.0% (n = 9) |
| Highest educational attainment | ||
| Less than high school | 6.5% (n = 2) | 6.7% (n = 2) |
| High school graduate | 54.8% (n = 17) | 73.3% (n = 22) |
| College graduate | 25.8% (n = 8) | 16.7% (n = 5) |
| Income | ||
| < $20,000 | 38.7% (n = 12) | 57.1% (n = 16) |
| $20,000 – $59,999 | 32.3% (n = 10) | 32.1% (n = 9) |
| > $60,000 | 29.0% (n = 9) | 10.7% (n = 3) |
| Clinical Characteristics | ||
| Number of BPD criteria (DIPD-IV) | mean = 6.5 (SD = 1.6) | mean = 6.0 (SD = 1.5) |
| % meeting full criteria for BPD | 90.3% (n = 28) | 86.7% (n = 26) |
| Suicide attempt in lifetime | 58.1% (n = 18); range = 0–16 | 66.7% (n = 20); range = 0–5 |
| Suicide attempt past year | 16.1% (n = 5); range = 0–2 | 20.0% (n = 6); range = 0–2 |
| DSH frequency in past 3 mos. | Mean = 35.5 ± 68.4 | Mean = 28.4 ± 39.4 |
| Inpatient hospitalization past year | 12.9% (n = 4) | 26.7% (n = 8) |
| Total hours/week of ongoing therapy | mean = 1.2 (SD = 1.4) | mean = 2.5 (SD = 2.6) |
| Hours/week individual therapy | mean = 0.7 (SD = 0.4) | mean = 1.0 (SD = 0.8) |
| Hours/week group therapy | mean = 0.4 (SD = 1.3) | mean = 0.6 (SD = 1.8) |
| Number psychiatric medications | mean = 1.9 (SD = 1.7) | mean = 2.1 (SD = 1.2) |
| Number mos. with individual therapist | mean = 15.5 (SD = 19.3) | mean = 14.9 (SD = 25.4) |
| Global Assessment of Functioning score | mean = 43.4 (SD = 24.6) | mean = 40.5 (SD = 19.8) |
| Diagnostic Data | ||
| Lifetime Axis I disorders | ||
| Mood disorder | 80.6% (n = 25) | 86.7% (n = 26) |
| Substance use disorder | 54.8% (n = 17) | 60.0% (n = 18) |
| Anxiety disorder | 74.2% (n = 23) | 86.7% (n = 26) |
| Posttraumatic Stress Disorder | 48.4% (n = 15) | 63.3% (n = 19) |
| Eating disorder | 36.7% (n = 11) | 42.9% (n = 12) |
| Current Axis I disorders | ||
| Mood disorder | 41.9% (n = 13) | 60.0% (n = 18) |
| Substance use disorder | 0.0% (n = 0) | 3.3% (n = 1) |
| Anxiety disorder | 54.8% (n = 17) | 70.0% (n = 21) |
| Posttraumatic Stress Disorder | 29.0% (n = 9) | 43.3% (n = 13) |
| Eating disorder | 16.7% (n = 5) | 10.7% (n = 3) |
| Axis II comorbidity | 40.0% (n = 12) | 53.3% (n = 16) |
| Cluster A PD | 6.7% (n = 2) | 10.0% (n = 3) |
| Cluster B PD (other than BPD) | 13.3% (n = 4) | 20.0% (n = 6) |
| Cluster C PD | 36.7% (n = 11) | 43.3% (n = 13) |
Note. None of the above demographic, clinical, or diagnostic variables differed significantly between conditions (ts < 1.50, χ2s < 3.49, ps > .15), with the exception of total hours/week of ongoing therapy.
Random assignment to the treatment or waitlist condition occurred as soon as enough participants had been screened; therefore, time between initial assessment and randomization ranged from < 1 week to approximately 4 months (mean = 29 days). Five treatment cohorts were recruited from June 2009 to December 2010. Pre-treatment and -waitlist assessments were completed within one week prior to the start of the group for participants in the treatment condition; post-treatment and -waitlist assessments were completed within one week following the end of the group. The post-waitlist assessment served as the pre-treatment assessment for participants in the waitlist condition, with their post-treatment assessment occurring within one week after the end of their group. For all participants, follow-up assessments were completed 9-months following completion of the post-treatment assessment. All assessments were conducted by trained assessors masked to participant condition.
Measures
The following instruments were administered during the initial assessment to screen participants and collect baseline clinical and diagnostic data: (a) the Diagnostic Interview for DSM-IV Personality Disorders (Zanarini et al., 1996); (b) the Structured Clinical Interview for DSM-IV Axis I Disorders (First et al., 1996); (c) a modified version of the Lifetime Parasuicide Count (Linehan & Comtois, 1996), used to assess lifetime suicidal behaviors; (d) an interview version of the Deliberate Self-Harm Inventory (Gratz, 2001), used to assess lifetime DSH; and (e) the Treatment History Interview (THI; Linehan & Heard, 1987), used to assess past-year psychiatric treatment.
The following measures were administered pre- and post-treatment or -waitlist, and at 9-months post-treatment (for participants in both conditions who received ERGT).
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report measure that assesses individuals’ typical levels of emotion dysregulation across six domains: emotional nonacceptance, difficulties controlling impulsive behaviors and engaging in goal-directed behaviors when distressed, limited access to effective regulation strategies, and lack of emotional awareness and clarity (α = 0.93 in this sample). The DERS has good test-retest reliability and construct and predictive validity (Gratz & Roemer, 2004; Gratz & Tull, 2010a).
The Deliberate Self-Harm Inventory (DSHI; Gratz, 2001) is a 17-item self-report questionnaire that assesses various aspects of DSH (including frequency) over specified time periods. The DSHI demonstrates adequate test-retest reliability and construct, discriminant, and convergent validity among diverse nonclinical and patient samples (Gratz, 2001; Fliege et al., 2006). A continuous variable measuring frequency of DSH over the specified time period (e.g., in the 3.5 months before the study, since the last assessment) was created by summing participants’ scores on the frequency questions for each item (α = 0.75). To account for the unequal intervals between assessments, DSH frequencies were scaled to be the frequency per 14 weeks.
The Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD; Zanarini, 2003) is a clinician-administered instrument for assessing change in BPD symptom severity over time, across four core areas of BPD pathology (affective, cognitive, impulsive, and interpersonal). The ZAN-BPD demonstrates good reliability and validity (Zanarini, 2003), and was used to provide an interviewer-based assessment of past-week severity of BPD affective, cognitive, impulsive, and interpersonal symptoms (α = 0.81). Interviews were conducted by clinical assessors trained to reliability with the PI (ICC = 0.92).
Treatment
Emotion regulation group therapy
This ERGT is based on the conceptualization of emotion regulation as a multidimensional construct involving the: (a) awareness, understanding, and acceptance of emotions; (b) ability to engage in goal-directed behaviors and inhibit impulsive behaviors when experiencing negative emotions; (c) use of situationally-appropriate strategies to modulate the intensity or duration of emotions, rather than to eliminate emotions; and (d) willingness to experience negative emotions as part of pursuing meaningful activities in life (Gratz & Roemer, 2004). ERGT draws from two acceptance-based behavioral therapies, Acceptance and Commitment Therapy (Hayes, Strosahl, & Wilson, 1999) and DBT (Linehan, 1993), and emphasizes the following themes: (a) the potentially paradoxical effects of emotional avoidance, (b) the emotion-regulating consequences of emotional acceptance and willingness, and (c) the importance of controlling behaviors when emotions are present, rather than controlling emotions themselves. A detailed manual has been developed and a full description of the specific topics addressed each week is available elsewhere (Gratz & Gunderson, 2006). Groups meet weekly for 90 minutes over 14 weeks and are limited to 6 patients per group. Treatment integrity data for this RCT are available elsewhere (see Gratz et al., 2014).
Treatment as usual
All participants were required to have an individual clinician, and all continued with their ongoing outpatient treatment over the course of the RCT. Participants had been meeting with their individual clinicians for an average of 15.5 months (SD = 21.1; range = 1 month to 9 years) prior to the start of the study, with 76% reporting a duration of ≥ 2 months. Few participants (23%) received group therapy outside of this ERGT, and 57% received less than one hour of individual therapy per week. Further information on participants’ TAU is provided in Table 1. With regard to the individual clinicians of participants, 20% were in private practice and the others worked in a community mental health center (43%), college counseling center (12%), or hospital (24%). In regard to their training, 69% had a master’s degree, 22% were clinical psychologists, and 10% were psychiatrists. Most participants (>60%) were receiving supportive or dynamic individual therapy (according to the THI and discussions with clinicians); however, 19.6% were receiving cognitive-behavioral therapy (although not DBT).
Results
Ninety-one women completed the initial assessment, and 61 were randomized to the treatment (n = 31) or waitlist (n = 30) condition. There were no significant between-group differences in the time between the initial assessment and randomization to condition (t = 0.67, p > .50). Detailed information on patient enrollment and disposition across the study is available elsewhere (see Gratz et al., 2014). Twelve participants dropped out of treatment (5 vs. 7 from the treatment and waitlist conditions, respectively; χ2 = 2.41, p > .10), for an overall treatment dropout rate of 23.5%. Four participants did not complete the post-treatment or -waitlist assessment in the RCT phase of the study, and three participants did not complete the 9-month follow-up assessment. Descriptive statistics for all outcome measures at pre- and post-treatment or -waitlist and 9-month follow-up are presented in a previous manuscript (Gratz et al., 2014).
Randomized controlled trial mediation analyses
To examine whether change in emotion dysregulation mediates the effects of this ERGT on DSH and BPD symptoms, we examined the direct and indirect (through change in emotion dysregulation) effects of condition membership (coded 1 for treatment, 0 for waitlist) on changes in DSH and BPD symptoms using the PROCESS macro for SPSS (Hayes, 2013). As shown in Table 2, path a captures the effect of condition on change in the mediator (ΔDERS), path b captures the effect of change in the mediator on change in the outcome (controlling for the effect of condition), and path c captures the effect of condition on change in the outcome. The indirect effect of condition on change in the outcome through ΔDERS is calculated as a x b, and path c′ captures the direct effect of condition membership on change in the outcome (i.e., the remainder of the effect not accounted for by the indirect effect; Preacher & Hayes, 2008). Following recommendations by Preacher and Hayes (2008), the current study used a bootstrapping technique to estimate the indirect effect; in this study, the estimate of the indirect effect was derived from the mean of 5000 bootstrap samples. Bias corrected and accelerated 95% confidence intervals were calculated, and indirect effect estimates were considered significant when the confidence intervals did not contain zero.
Table 2.
Summary of Path Coefficients for the RCT Mediation Analyses in the Intent-to-Treat Sample (N = 61)
| Independent Variable | Mediating Variable | Dependent Variable | Effect of IV on M | Effect of M on DV | Direct Effect | Indirect Effect | Total Effect | |
|---|---|---|---|---|---|---|---|---|
| (IV) | (M) | (DV) | (a) | (b) | (c′) | (a x b) | 95% CI | (c) |
| Condition | ΔDERS | ΔZAN-BPD-Cognitive | −.56* | .57*** | −.37 | −.32* | (−.65, −.09) | −.69** |
| ΔZAN-BPD-Affect | −.56* | .38*** | −.76** | −.21* | (−.43, −.04) | −.97*** | ||
| ΔZAN-BPD-Relationship | −.56* | .01 | −.77** | −.01 | (−.19, .12) | −.78** | ||
| ΔZAN-BPD-Impulsivity | −.56* | .04 | −.56* | −.02 | (−.21, .10) | −.59* | ||
| ΔDSHI | −.56* | .17 | −.77** | −.09 | (−.36, .07) | −.86*** | ||
Note. 5,000 bootstraps. All path coefficients are unstandardized effects. Δ = residualized gain score (pre- to post-treatment); DERS = Difficulties in Emotion Regulation total score; ZAN-BPD = Zanarini Rating Scale for Borderline Personality Disorder (Affect Disturbance, Cognitive Disturbance, Disturbed Relationship, and Impulsivity subscales); DSHI = Deliberate Self-Harm Inventory.
p < .05.
p < .01.
p < .001.
Prior to data analysis, we used a multiple imputation strategy to handle missing data (Enders, 2010), enabling an analysis of the intent-to-treat sample. Multiple imputation is among the optimal options for handling missing data (Kline, 2005), yielding relatively unbiased estimates and performing particularly well relative to other approaches in small samples (Graham & Schafer, 1999; Yuan et al., 2012) and when flexibility in analytic strategies is required (Allison, 2003; Schafer, 1999). To capture changes in the mediator and outcome variables, residualized gain scores (Tucker, Damarin, & Messick, 1966) were calculated for pre- and post-treatment or -waitlist scores on the measures of emotion dysregulation, DSH, and BPD symptoms.
Results of these mediation analyses are presented in Table 2. Across all analyses, results indicate a significant effect of treatment on change in the DERS (b = −.56, SE = .25, p < .05). Likewise, results indicate significant effects of treatment on changes in DSH (b = −.86, SE = .23, p < .001) and BPD cognitive (b = −.69, SE = .24, p < .01), affective (b = −.97, SE = .22, p < .001), relationship (b = −.78, SE = .24, p < .01), and impulsive (b = −.59, SE = .25, p < .05) symptoms. Finally, results provide partial support for the hypothesized mediating role of change in emotion dysregulation in the effects of this ERGT on DSH and BPD symptoms, revealing significant indirect effects of treatment on changes in BPD cognitive (b = −.32, SE = .14, CI = −.65, −.09) and affective (b = −.21, SE = .10, CI = −.43, −.04) symptoms through change in DERS. The indirect effects of treatment on changes in DSH and BPD relationship and impulsive symptoms through change in DERS were not significant (bs = −.09, −.01, and −.02, SEs = .10, .07, and .08, all confidence intervals contain zero; see Table 2).
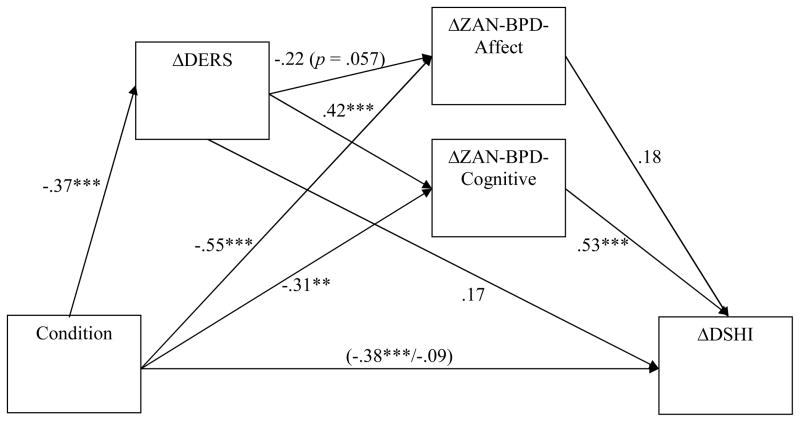
Given findings that change in emotion dysregulation mediated the effects of this ERGT on BPD cognitive and affective symptoms but not DSH (despite positive treatment effects for DSH), follow-up analyses testing a serial mediation model in which change in emotion dysregulation mediates the effect of this ERGT on change in DSH through change in BPD cognitive and affective symptoms were conducted (see Figure 1). Specifically, structural equation modeling (SEM) was used to examine the simultaneous indirect effects of ΔDERS through both ΔZAN-BPD-Cognitive and ΔZAN-BPD-Affect in the relation between condition membership and ΔDSHI. All variables were modeled as manifest indicators, and maximum likelihood estimation was used to test the model. As shown in Figure 1, addition of the mediator variables (i.e., ΔDERS, ΔZAN-BPD-Cognitive, ΔZAN-BPD-Affect) significantly reduced the magnitude of the coefficient for the effect of condition on ΔDSHI (from b = −.38 to b = −.09). Further, results revealed two significant indirect paths in this model: (1) Condition → ΔDERS → Δ ZAN-BPD-Cognitive → ΔDSHI (b = −.12, SE = .07, CI = −.30, −.04), and (2) Condition → Δ ZAN-BPD-Cognitive → ΔDSHI (b = −.24, SE = .13, CI = −.57, −.08). No other indirect effects emerged as significant (i.e., all other confidence intervals contained zero), including the indirect paths from (1) Condition → ΔDERS → ΔZAN-BPD-Affect → ΔDSHI (b = −.05, SE = .05, CI = −.18, 0), (2) Condition → ΔZAN-BPD-Affect → ΔDSHI (b = −.21, SE = .19, CI = −.65, .01), and (3) Condition → ΔDERS → ΔDSHI (b = .10, SE = .10, CI = −.01, .38).
Figure 1.
Analyses include intent-to-treat sample (N = 61). Standardized coefficients are presented. Δ = residualized gain score (pre- to post-treatment); DERS = Difficulties in Emotion Regulation Scale total score; ZAN-BPD = Zanarini Rating Scale for Borderline Personality Disorder (Affect and Cognitive Disturbance subscales); DSHI = Deliberate Self-Harm Inventory. *p < .05. **p <.01. ***p < .001.
Notably, when each of the BPD symptom domains from this serial mediation model was examined separately using the PROCESS macro (Hayes, 2013) as described above, results for the model including BPD cognitive symptoms were comparable to those reported above. Specifically, results revealed a significant indirect effect of condition on change in DSH through change in emotion dysregulation and, subsequently, change in BPD cognitive symptoms (Condition → ΔDERS → ΔZAN-BPD-Cognitive → ΔDSHI: b = −.20, SE = .09, CI = −.45, −.07). Contrary to the results for the larger serial mediation model reported above, however, results for the model including only BPD affective symptoms suggest that change in emotion dysregulation mediates the effect of this ERGT on change in DSH through change in BPD affective symptoms as well. Specifically, results revealed a significant indirect effect of condition on change in DSH through changes in emotion dysregulation and, subsequently, BPD affective symptoms (Condition → ΔDERS → ΔZAN-BPD-Affect → ΔDSHI; b = −.10, SE = .06, CI = −.29, −.02).
Analyses examining predictors of improvement in DSH during follow-up
Structural equation modeling of residualized gain scores was used to examine the extent to which change in emotion dysregulation during treatment predicted improvements in DSH from post-treatment through 9-month follow-up among the full sample of participants who began ERGT (across treatment and waitlist conditions; n = 51). Given the results of the serial mediation analyses presented above (which suggest the mediating role of changes in BPD cognitive and affective symptoms in the effects of this ERGT on DSH during treatment), changes in these BPD symptoms during treatment were also examined as predictors of improvement in DSH during follow-up. Furthermore, following the methodology of Gibbons et al. (2009), change in DSH from pre- to post-treatment was included in analyses as well (to account for change in this outcome during treatment). To this end, residualized gain scores reflecting changes in the mediator and outcome variables during treatment and in DSH during follow-up were calculated for pre- and post-treatment scores on the DERS, ZAN-BPD, and DSHI and for post-treatment and 9-month follow-up scores on the DSHI.
Changes in emotion dysregulation and BPD cognitive and affective symptoms during treatment were significantly positively correlated with improvements in DSH during the follow-up (rs = .44, .33, and .39, respectively, ps < .05). Further, these associations remained significant when accounting for change in DSH during treatment (partial rs = .44, .32, and .39, respectively, ps < .05). To examine the unique contributions of changes in emotion dysregulation and BPD symptoms during treatment to change in DSH during the 9-month follow-up, changes in all of these variables during treatment were modeled as predictors of change in DSH from post-treatment through 9-month follow-up in SEM. All variables were modeled as manifest indicators, and maximum likelihood estimation was used to test the model. Notably, only change in emotion dysregulation during treatment emerged as a significant unique predictor of change in DSH from post-treatment through 9-month follow-up (β = .32, p < .05). Changes in BPD cognitive and affective symptoms during treatment were not unique predictors of change in DSH during the follow-up (βs = .10 and .23, respectively; ps > .10).
Discussion
Drawing on theoretical and empirical literature highlighting the central role of emotion dysregulation in the development and maintenance of DSH, this ERGT was developed to directly target both DSH and its proposed underlying mechanism. However, research examining emotion regulation as the mechanism of change in this treatment has been limited to date, with only one study examining the mediating role of change in emotion dysregulation in improvements in DSH over the course of this treatment (Gratz et al., 2012). Results of the present study provide further support for emotion regulation as a mechanism of change in this treatment. Specifically, results revealed that improvements in emotion dysregulation over the course of this ERGT mediated the observed reductions in BPD cognitive and affective symptoms during treatment and predicted further improvements in DSH from post-treatment through a 9-month follow-up. Moreover, results of the serial mediation models revealed that reductions in emotion dysregulation during treatment mediated the effect of this ERGT on improvements in DSH through change in BPD cognitive symptoms (and, to a lesser extent, BPD affective symptoms). These results provide support for the theoretical model underlying this ERGT and add to the extant literature emphasizing the clinical utility of targeting emotion dysregulation in treatments for DSH among individuals with BPD (Gratz, 2007; Linehan, 1993; Lynch, Chapman, Rosenthal, Kuo, & Linehan, 2006).
Notably, and contrary to hypotheses, improvements in emotion dysregulation over the course of this treatment did not relate directly to the observed improvements in DSH during treatment. Rather, results provide support for a model wherein improvements in emotion dysregulation from pre- to post-treatment relate to enhanced BPD-related affective and cognitive functioning, which, in turn, relate to reductions in DSH. Although unexpected, these findings are not without support in the literature. With regard to the mediating role of BPD affective symptoms in particular, research indicates that heightened emotion dysregulation can increase emotional arousal and reactivity and interfere with the ability to control mood- and emotion-dependent behaviors (e.g., Campbell-Sills, Barlow, Brown, & Hoffman, 2006; Gratz, Paulson, Jakupcak, & Tull, 2009; McLaughlin, Hatzenbuehler, Mennin, & Nolen-Hoeksema, 2011; Williams, Bargh, Nocera, & Gray, 2009). Conversely, the use of adaptive emotion regulation strategies has been associated with reductions in emotional reactivity (e.g., Campbell-Sills et al., 2006; Williams et al., 2009). Thus, the finding that improvements in emotion dysregulation may be associated with improvements in DSH through reductions in BPD symptoms related to marked emotional reactivity and difficulties controlling the expression of these emotions (symptoms that DSH may once have been used to manage) is not surprising.
Findings suggesting the impact of emotion regulation skills on DSH via reductions in cognitive symptoms on the ZAN-BPD are also consistent with extant literature on the development and maintenance of DSH among individuals with BPD. Specifically, as assessed here, the cognitive symptoms of BPD include not only stress-related paranoid ideation and dissociation, but instability and disturbance of self-image and identity. Notably, self and identity disturbance have been theorized to play a central role in DSH among individuals with BPD, with one prominent theory of BPD suggesting that DSH functions to reestablish a coherent sense of self following destabilization of the self-structure in response to emotional distress and dysregulation (Bateman & Fonagy, 2004; Fonagy & Bateman, 2008; Fonagy et al., 2014). Indeed, acute distress and difficulties regulating that distress are considered key precipitants of the disintegration of the self-structure and identity destabilization that are theorized to precede DSH within this population (Bateman & Fonagy, 2004; Fonagy et al., 2014). Consistent with this theory, establishing a sense of self and identity (along with managing other BPD cognitive symptoms) are commonly cited motives for DSH (see Klonsky, 2007; Suyemoto, 1998). Moreover, research indicates that emotional distress exacerbates both cognitive dysfunction in general (Duncan & Feldman Barrett, 2007) and identity and self disturbance in particular (Koenigsberg et al., 2001; Suh, 2002). Together with emerging research documenting a relation between cognitive dysfunction and DSH (Dixon-Gordon, Gratz, McDermott, & Tull, in press; Franklin et al., 2010), these findings suggest that BPD-related cognitive disturbances may be an important and previously overlooked treatment target for reducing DSH within this population. However, further research is needed to pinpoint the particular aspects of cognitive dysfunction most relevant to DSH and the relation of emotion dysregulation to this behavior.
Several limitations warrant mention. First, the modest sample size increases the risk for both Type I and Type II error; thus, these findings should be considered preliminary and in need of further investigation and replication in future clinical trials. Moreover, given our exclusive focus on women with BPD, the generalizability of these findings to adolescents and men remains unclear. In addition, the cross-sectional nature of the serial mediation analyses precludes conclusions regarding the precise temporal relations of the proposed mediators and outcomes in the RCT. Although results of analyses examining predictors of improvement in DSH during the follow-up period indicate that change in emotion dysregulation precedes further improvements in DSH during follow-up, future studies should incorporate additional assessments of both emotion dysregulation and DSH throughout the treatment and follow-up periods (e.g., weekly assessments of these variables during treatment and monthly assessments during follow-up) to assess these causal relations. Likewise, although findings support emotion regulation as a mechanism of change in this ERGT across both treatment and a 9-month follow-up, longer follow-up periods are needed.
Furthermore, although assessments included both clinician-administered and self-report measures, future studies would benefit from the inclusion of behavioral and/or psychophysiological measures of emotion dysregulation as well (e.g., Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Hazlett et al., 2007; Thayer & Lane, 2000; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). Finally, although the present study extended previous research by examining both emotion dysregulation and BPD symptoms as potential mechanisms of change in this treatment, other mechanisms of change warrant investigation as well, including the enhancement of mentalization (i.e., the ability to understand and reflect upon one’s own and other’s internal states and their relationship to behaviors) and reflective function (see Bateman & Fonagy, 2004; Levy et al., 2006) and the acceptance of internal experiences (see Hayes, Luoma, Bond, Masuda, & Lillis, 2006; Hayes, Orsillo, & Roemer, 2010).
Despite limitations, the present study extends extant literature on emotion regulation as the mechanism of change in this treatment, examining the extent to which changes in emotion regulation during both treatment and follow-up relate to improvements in DSH and BPD symptoms during these periods. Building on past research, the results of this study paint a more dynamic and complex picture of the mechanisms of change in this ERGT. Specifically, findings point to the immediate impact of improvements in emotion dysregulation on two core domains of BPD pathology (i.e., cognitive and affective symptoms), and suggest that it is reductions in these symptoms that play an important role in improvements in DSH over the course of treatment. Nonetheless, findings that change in emotion dysregulation during treatment emerged as the only unique predictor of further improvements in DSH in the nine months following treatment highlight the robust impact of emotion dysregulation on the long-term desistence of this behavior. Mechanisms of change in treatment may vary based on the time course under examination (Kazdin & Nock, 2003); the results of the current study suggest that although the proximal impact of improved emotion regulation on DSH may be indirect through reductions in BPD symptoms, the ability to regulate emotions adaptively may take the forefront in the reduction of DSH in the long-term. Future research is needed to delineate the temporal relations between these and other relevant mechanisms of change in treatments for DSH within BPD.
Highlights.
Emotion dysregulation is theorized to underlie deliberate self-harm (DSH)
Research supports the efficacy of emotion regulation group therapy for DSH in BPD
We examined emotion regulation as the mechanism of change in this ERGT
Reductions in emotion dysregulation mediated the effects of ERGT on BPD symptoms
Reductions in emotion dysregulation predicted improvements in DSH during follow-up
Acknowledgments
This research was supported by National Institute of Mental Health Grant R34 MH079248, awarded to the first author (KLG). The authors wish to thank Drs. John Gunderson, Carl Lejuez, and Liz Roemer for consulting on this project, and Angela Cain (now Klein), Sarah Anne Moore, Nicole Weiss, Jessica Fulton, Rachel Brooks, Ashley Martin, and Melissa Soenke for their invaluable work on this project.
Footnotes
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kim L. Gratz, Email: klgratz@aol.com.
Joseph R. Bardeen, Email: jbardeen@auburn.edu.
Roy Levy, Email: roy.levy@asu.edu.
Katherine L. Dixon-Gordon, Email: katiedg@gmail.com.
Matthew T. Tull, Email: mtull@umc.edu.
References
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Bateman AW, Fonagy P. Mentalization-based treatment of BPD. Journal of Personality Disorders. 2004;18:36–51. doi: 10.1521/pedi.18.1.36.32772. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Effects of suppression and acceptance on emotional responses of individuals with anxiety and mood disorders. Behaviour Research and Therapy. 2006;44:1251–1263. doi: 10.1016/j.brat.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Clifton A, Pilkonis PA. Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Comprehensive Psychiatry. 2007;48:70–78. doi: 10.1016/j.comppsych.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Gratz KL, McDermott MJ, Tull MT. The role of executive attention in deliberate self-harm. Psychiatry Research. doi: 10.1016/j.psychres.2014.03.035. in press. [DOI] [PubMed] [Google Scholar]
- Duncan S, Feldman Barrett L. Affect is a form of cognition: A neurobiological analysis. Cognition and Emotion. 2007;21:1184–1211. doi: 10.1080/02699930701437931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders – patient edition (SCID-I/P, version 2.0) New York, NY: New York State Psychiatric Institute; 1996. [Google Scholar]
- Fliege H, Kocalevent R, Walter OB, Beck S, Gratz KL, Gutierrez PM, Klapp BF. Three assessment tools for deliberate self-harm and suicide behavior: Evaluation and psychopathological correlates. Journal of Psychosomatic Research. 2006;61:113–121. doi: 10.1016/j.jpsychores.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Bateman A. The development of borderline personality disorder – A mentalizing model. Journal of Personality Disorders. 2008;22:4–21. doi: 10.1521/pedi.2008.22.1.4. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Rossouw T, Sharp C, Bateman A, Allison L, Farrar C. Mentalization- based treatment for adolescents with borderline traits. In: Sharp C, Tackett JL, editors. Handbook of borderline personality disorder in children and adolescents. New York: Springer; 2014. pp. 313–332. [Google Scholar]
- Franklin JC, Hessel ET, Aaron RV, Arthur MS, Heilbron N, Prinstein MJ. The functions of nonsuicidal self-injury: Support for cognitive-affective regulation and opponent processes from a novel psychophysiological paradigm. Journal of Abnormal Psychology. 2010;119:850–862. doi: 10.1037/a0020896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons MBC, Crits-Christoph P, Barber JP, Stirman SW, Gallop R, Goldstein LA, Ring-Kurtz S. Unique and common mechanisms of change across cognitive and dynamic psychotherapies. Journal of Consulting and Clinical Psychology. 2009;77:801–813. doi: 10.1037/a0016596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW, Schafer JL. On the performance of multiple imputation for multivariate data with small sample size. In: Hoyle R, editor. Statistical Strategies for Small Sample Research. Thousand Oaks, CA: Sage; 1999. pp. 1–29. [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology & Behavioral Assessment. 2001;23:253–263. [Google Scholar]
- Gratz KL. Targeting emotion dysregulation in the treatment of self-injury. Journal of Clinical Psychology. 2007;63:1091–1103. doi: 10.1002/jclp.20417. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Gunderson JG. Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy. 2006;37:25–35. doi: 10.1016/j.beth.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Levy R, Tull MT. Emotion regulation as a mechanism of change in an acceptance-based emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Journal of Cognitive Psychotherapy. 2012;26:365–380. [Google Scholar]
- Gratz KL, Paulson A, Jakupcak M, Tull MT. Exploring the relationship between childhood maltreatment and intimate partner abuse: Gender differences in the mediating role of emotion dysregulation. Violence and Victims. 2009;24:68–82. doi: 10.1891/0886-6708.24.1.68. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy. 2008;37:14–25. doi: 10.1080/16506070701819524. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115:850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT. Emotion regulation as a mechanism of change in acceptance-and mindfulness-based treatments. In: Baer R, editor. Assessing mindfulness and acceptance: Illuminating the process of change. Oakland, CA: New Harbinger Publications; 2010a. pp. 105–133. [Google Scholar]
- Gratz KL, Tull MT. The relationship between emotion dysregulation and deliberate self-harm among inpatients with substance use disorders. Cognitive Therapy and Research. 2010b;34:544–553. doi: 10.1007/s10608-009-9268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT. Extending research on the utility of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Personality Disorders: Theory, Research, and Treatment. 2011;2:316–326. doi: 10.1037/a0022144. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Levy RL. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Psychological Medicine. 2014;44:2099–2112. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hayes SA, Orsillo SM, Roemer L. Changes in proposed mechanisms of action during an acceptance-based behavior therapy for generalized anxiety disorder. Behaviour Research and Therapy. 2010;48:238–245. doi: 10.1016/j.brat.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and Commitment Therapy: Model, processes, and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hazlett EA, Speiser LJ, Goodman M, Roy M, Carrizal M, Wynn JK, New AS. Exaggerated affect-modulated startle during unpleasant stimuli in borderline personality disorder. Biological Psychiatry. 2007;62:250–255. doi: 10.1016/j.biopsych.2006.10.028. [DOI] [PubMed] [Google Scholar]
- Heath NL, Toste JR, Nedecheva T, Charlebois A. An examination of nonsuicidal self-injury among college students. Journal of Mental Health Counseling. 2008;30:137–156. [Google Scholar]
- International Society for the Study of Self-injury. Definitional issues surrounding our understanding of self-injury. Conference proceedings from the annual meeting..2007. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 2. New York: Guilford Press; 2005. [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, New AS, Goodman M, Silverman J, Siever LJ. Are the interpersonal and identity disturbances in the borderline personality disorder criteria linked to the traits of affective instability and impulsivity? Journal of Personality Disorders. 2001;15:358–370. doi: 10.1521/pedi.15.4.358.19181. [DOI] [PubMed] [Google Scholar]
- Levy KN, Clarkin JF, Yeomans FE, Scott LN, Wasserman RH, Kernberg OF. The mechanisms of change in the treatment of borderline personality disorder with transference focused psychotherapy. Journal of Clinical Psychology. 2006;62:481–501. doi: 10.1002/jclp.20239. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Linehan MM, Comtois K. Lifetime parasuicidal history. University of Washington; Seattle, WA: 1996. Unpublished measure. [Google Scholar]
- Linehan MM, Heard HL. Treatment history interview (THI) University of Washington; Seattle, WA: 1987. Unpublished measure. [Google Scholar]
- Lynch T, Chapman A, Rosenthal M, Kuo J, Linehan M. Mechanisms of change in dialectical behavior therapy: Theoretical and empirical observations. Journal of Clinical Psychology. 2006;62:459–480. doi: 10.1002/jclp.20243. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy. 2011;49:544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and ressampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Multiple imputation: A primer. Statistical Methods in Medical Research. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Slee N, Spinhoven P, Garnefski N, Arensman E. Emotion regulation as mediator of treatment outcome in therapy for deliberate self-harm. Clinical Psychology and Psychotherapy. 2008;15:205–216. doi: 10.1002/cpp.577. [DOI] [PubMed] [Google Scholar]
- Suh E. Culture, identity consistency, and subjective well-being. Journal of Personality and Social Psychology. 2002;83:1378–1391. doi: 10.1037//0022-3514.83.6.1378. [DOI] [PubMed] [Google Scholar]
- Suyemoto K. The functions of self-mutilation. Clinical Psychology Review. 1998;18:531–554. doi: 10.1016/s0272-7358(97)00105-0. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders. 2000;61:201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Damarin F, Messick S. A base-free measure of change. Psychometrika. 1966;31:457–473. doi: 10.1007/BF02289517. [DOI] [PubMed] [Google Scholar]
- Tyrer P, Tom B, Byford S, Schmidt U, Jones V, Davidson K, Catalan J. Differential effects of manual assisted cognitive behavior therapy in the treatment of recurrent deliberate self-harm and personality disturbance: The POPMACT study. Journal of Personality Disorders. 2004;18:102–116. doi: 10.1521/pedi.18.1.102.32770. [DOI] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, Gatzke-Kopp LM. Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry. 2009;50:1357–1364. doi: 10.1111/j.1469-7610.2009.02172.x. [DOI] [PubMed] [Google Scholar]
- Williams LE, Bargh JA, Nocera CC, Gray JR. The unconscious regulation of emotion: Nonconscious reappraisal goals modulate emotional reactivity. Emotion. 2009;9:847–854. doi: 10.1037/a0017745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K, Yang-Wallentin F, Bentler PM. ML versus MI for missing data with violation of distribution conditions. Sociological Methods & Research. 2012;41:598–629. doi: 10.1177/0049124112460373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC. Zanarini rating scale for borderline personality disorder (ZAN-BPD): A continuous measure of DSM-IV borderline psychopathology. Journal of Personality Disorders. 2003;17:233–242. doi: 10.1521/pedi.17.3.233.22147. [DOI] [PubMed] [Google Scholar]
- Zanarini MC. Psychotherapy of borderline personality disorder. Acta Psychiatrica Scandinavica. 2009;120:373–377. doi: 10.1111/j.1600-0447.2009.01448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Young L. Diagnostic interview for DSM-IV personality disorders. Boston, MA: McLean Hospital; 1996. [Google Scholar]