Abstract
BACKGROUND
Contemporary data on the epidemiology of myocardial infarction in the population are limited and derived primarily from cohorts of hospitalized myocardial infarction patients. We assessed temporal trends in incident and recurrent myocardial infarction, with further partitioning of the rates into prehospital deaths and hospitalized events, in a geographically defined community.
METHODS
All myocardial infarction events recorded among Olmsted County, Minnesota residents aged 25 years and older from 1995–2012, including prehospital deaths, were classified into incident and recurrent. Standardized rates were calculated and temporal trends compared.
RESULTS
Altogether, 5258 myocardial infarctions occurred, including 1448 (27.5%) recurrences; 430 (8.2%) prehospital deaths were recorded. Among hospitalized events, recurrent myocardial infarction was associated with greater mortality risk than incident myocardial infarction (age-, sex-, and year-adjusted hazard ratio, 1.49; 95% confidence interval, 1.37–1.61). Although the overall rate of myocardial infarction declined over time (average annual percent change, −3.3), the magnitude of the decline varied widely. Incident hospitalized myocardial infarction rate fell 2.7%/y, compared with decreases of 1.5%/y in recurrent hospitalized myocardial infarction, 14.1%/y in prehospital fatal incident myocardial infarction, and 12.3% in prehospital fatal recurrent myocardial infarction (all P for diverging trends < .05). These trends resulted in an increasing proportion of recurrences among hospitalized myocardial infarctions (25.3% in 1995–2000, 26.8% in 2001–2006, and 29.0% in 2007–2012, Ptrend = .02).
CONCLUSIONS
Over the past 18 years, a heterogeneous decline in myocardial infarction rates occurred in Olmsted County, resulting in transitions from incident to recurrent events and from prehospital deaths to hospitalized myocardial infarctions. Recurrent myocardial infarction confers a worse prognosis, thereby stressing the need to optimize prevention strategies in the population.
Keywords: Epidemiology, Myocardial infarction, Population, Prevention, Trends
The steady improvement in short-term survival after myocardial infarction,1–4 along with demographic changes and population aging,5 could have led to a larger pool of individuals at risk for recurrent myocardial infarction. However, the temporal decline in myocardial infarction incidence1–3 has offset, at least to some extent, the upward shift in reservoir volume. A recent report from the National Health and Nutrition Examination Survey suggested that the prevalence of myocardial infarction at midlife increased in women and decreased in men between 1988–1994 and 1999–2004,6 whereas an increase in the absolute number of persons with a history of myocardial infarction between 1988–1994 and 1999–2002 was estimated in another National Health and Nutrition Examination Survey publication.7 Furthermore, improved quality of care during the acute phase and implementation of effective secondary prevention strategies post myocardial infarction — albeit not equally attained by all population subgroups8–10 — have resulted in reduced risk of recurrence among myocardial infarction patients;11–13 still, their risk is much higher than that for the general population.14,15 These diverging and complex longitudinal changes in key determinants of recurrent myocardial infarction rates highlight the need for better understanding of the burden posed by myocardial infarction recurrences in the population. Indeed, previous studies evaluating recurrent myocardial infarction trends were conducted among cohorts of patients hospitalized with myocardial infarction,11–13,16,17 and are therefore unable to study the epidemiology of recurrent myocardial infarction from the population’s standpoint. This is important, however, as recurrent myocardial infarction confers a considerably worse prognosis than incident myocardial infarction,14,18–20 and is associated with substantial long-term cost of care.19,21
A related issue sometimes overlooked pertains to prehospital (“out-of-hospital”) myocardial infarction fatalities. Although many large-scale cohort studies and registries have been utilized to investigate case fatality in patients hospitalized with myocardial infarction,1–3,22 limited data are available on prehospital fatal myocardial infarction rates. With the risk of prehospital coronary heart disease death following myocardial infarction declining significantly over the past decades,23 there is some evidence for a decreasing proportion of such deaths out of all major coronary events.3,24 Whether this suggested trend has persisted over recent years is currently unknown.
We examined temporal trends in incident and recurrent myocardial infarction, with further partitioning of the rates into prehospital deaths and hospitalized events, in a geographically defined community. Our predefined hypothesis was that the proportion of re-infarctions among all myocardial infarctions has increased over time as a result of a steeper decline in incident compared with recurrent event rates, and that prehospital myocardial infarction death has declined.
METHODS
Study Setting
Olmsted County, Minnesota (2010 census population, 144,248) is 144 km southeast of Minneapolis and St. Paul. Except for a higher proportion being employed in the health care industry, the population characteristics are similar to those of US Whites.25–27
Olmsted County is a fertile ground for epidemiological research because of its relative isolation from other urban centers and because medical care is practically self-contained within the community. Nearly all acute cardiac care, for example, is provided by the Mayo Clinic, which has maintained a common medical record with its 2 affiliated hospitals (St. Marys Campus and Methodist Campus) for over 100 years. Recorded diagnoses are indexed through the unique medical records linkage system called the Rochester Epidemiology Project.25,26 Because virtually all Olmsted County residents are represented in this system, this data source provides an essentially complete enumeration of the source population for many decades.28
Study Design
The research protocol was approved by the appropriate Institutional Review Boards, and patients who did not provide authorization for medical record studies (8%) were excluded from the analysis. The percentage of patients not providing research authorization was stable during the study period (8% in 1995–2000, 8% in 2001–2006, and 9% in 2007–2012; P for trend = .68). Subsequently, a surveillance study was conducted to examine temporal trends in the incidence and recurrence rates of myocardial infarction in the population of Olmsted County. For this purpose, all hospitalized myocardial infarctions and prehospital deaths with myocardial infarction as the underlying cause (International Classification of Diseases, Ninth Revision [ICD-9] 410 code or ICD, Tenth Revision [ICD-10] I21–I22 codes) from 1995–2012 were included. Prehospital deaths were defined as those occurring outside of acute care or long-term care hospitals, including deaths occurring in emergency departments, private homes, public places, nursing or boarding care homes, and infirmaries, as well as deaths among persons declared dead on arrival at a hospital.23 Myocardial infarctions were classified as incident or recurrent (those with any prior code of hospitalized myocardial infarction). To accurately distinguish initial from recurrent events, medical histories that span each participant’s entire period of residency in the community were searched. Myocardial infarctions occurring within 28 days were treated as one event.15,29
In the assessment of prehospital fatal myocardial infarction rates, the potential bias resulting from changes in death certificate coding was addressed by performing 2 complimentary analyses. First, deaths occurring outside of the hospital whose primary cause on the death certificate was coronary heart disease (ICD-9, 410–414; ICD-10, I20–I25) were defined as “prehospital coronary heart disease death,”23 and were further partitioned into “myocardial infarction” and “other than myocardial infarction.” Second, “prehospital cardiovascular death” was defined (ICD-9, 390–459; ICD-10, I00–I99) with further partitioning into “myocardial infarction” and “other than myocardial infarction.” The rationale for these sensitivity analyses was to detect — by assessing temporal trends in rates of the above subcategories — a possible shift in coding practices from myocardial infarction to other ICD codes.
Mortality Follow-up
Death was ascertained through multiple sources, including autopsy reports, death certificates filed in Olmsted County, obituary notices, and electronic death certificates obtained from the Section of Vital Statistics, Minnesota Department of Health.1 Case fatality of hospitalized events was defined as death within 28 days after myocardial infarction.
Statistical Analysis
In calculating myocardial infarction rates, the entire population of Olmsted County aged ≥25 years was considered to be at risk. Specific counts (number of events) for each calendar year, age and sex, stratified by incident/recurrent myocardial infarction and by hospitalization status (ie, prehospital death/hospitalized myocardial infarction), were used as numerators. The nearest integer was used for age grouping, except for ≤50 years and ≥90 years, which were collapsed into 2 groups due to low yield rates. Respective denominators were estimated from an ongoing enumeration of Olmsted County residents by the Rochester Epidemiology Project.28 To assess variability, it was assumed that the number of myocardial infarction events follows a Poisson distribution; this allowed for the estimation of standard errors. Rates were directly age and sex standardized to the distribution of the 2010 US census population estimates. Temporal trends in myocardial infarction rates were explored by Poisson regression models, through which average annual percentage changes (APCs) were estimated. Comparisons of temporal trends across myocardial infarction categories and demographic subgroups were performed by including 2-way interaction terms of specific categories, with year after adjustment for their main effects, age, and sex (when applicable).
The hazard ratio (HR) for death associated with recurrent vs incident myocardial infarction was evaluated using Cox proportional hazards model,30 adjusting for age, sex, and year of myocardial infarction. Adjusted survival curves were estimated by the direct adjustment method based on a stratified Cox regression model, with incident/recurrent myocardial infarction status modeled as a stratification variable, which allows for a time-varying association.31 Analyses were performed using SAS statistical software, version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
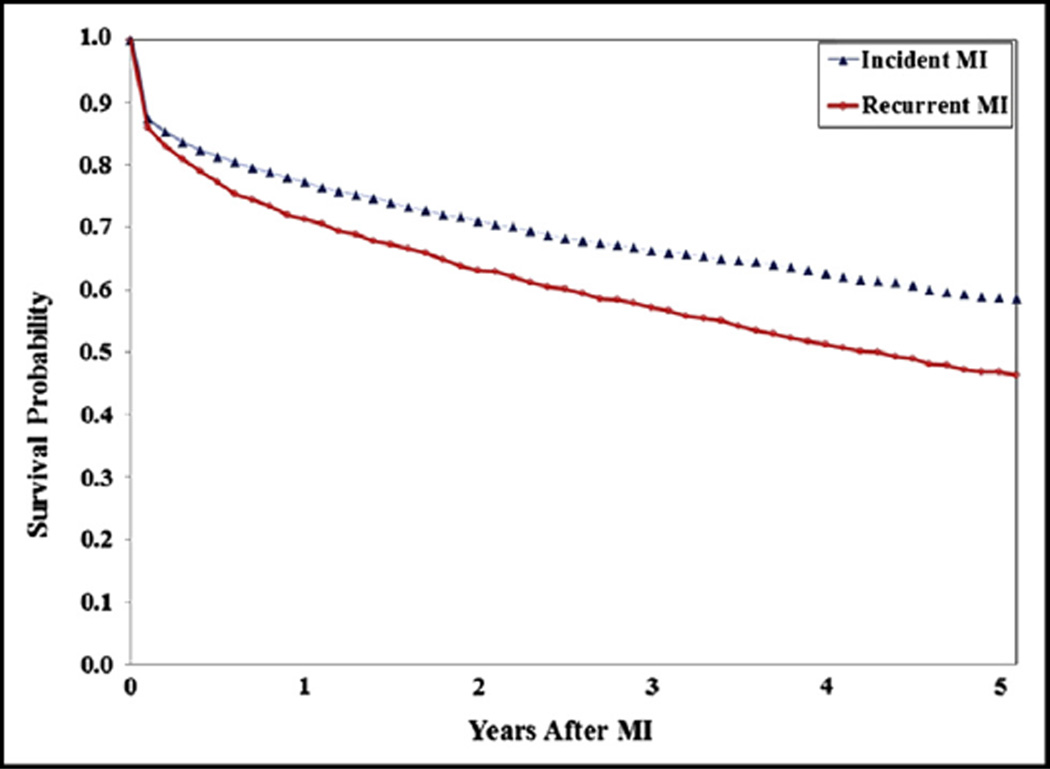
Between 1995 and 2012, 5258 myocardial infarction events were recorded in Olmsted County, of which 3810 (72.5%) were incident events and 1448 (27.5%) recurrent events. Of these, 287 incident events (7.5%) and 143 recurrent events (9.9%) were prehospital fatal myocardial infarctions (P for difference in proportions = .006); 344 recurrent events (23.8%) were the second or greater recurrence. On average, incident myocardial infarctions occurred at age 70.5 (SD 15.0) years and recurrent myocardial infarctions at age 74.9 (SD 13.1) years (P < .001), whereas no difference was observed in the sex distribution (59.1% vs 56.8% men, respectively, P = .12). Prehospital myocardial infarction fatalities occurred at a mean age of 75.3 (SD 14.8) years for incident events and 79.8 (SD 11.3) years for recurrent events (P < .001). Among hospitalized events, the 28-day case-fatality rates were 11.3% and 14.3% for incident and recurrent myocardial infarctions, respectively (P = .005). The long-term adjusted mortality risk was also greater for recurrent vs incident myocardial infarctions (Figure 1). At 5 years of follow-up, the age-, sex-, and year-adjusted survival estimates were 58.7% and 46.8% for incident and recurrent myocardial infarctions, respectively. The overall adjusted HR for mortality in recurrent vs incident hospitalized myocardial infarction was 1.49 (95% confidence interval [CI], 1.37–1.61). The greater adjusted mortality risk associated with recurrent vs incident myocardial infarctions applied both to men (HR 1.55; 95% CI, 1.39–1.74) and women (HR 1.41; 95% CI, 1.26–1.59), but was more pronounced (P for interaction < .001) among patients younger than 75 years (HR 1.93; 95% CI, 1.67–2.23) than among older patients (HR 1.32; 95% CI, 1.19–1.46).
Figure 1.
Adjusted survival curves for incident and recurrent events. Age-, sex-, and year-adjusted survival among Olmsted County, Minnesota, residents with myocardial infarction in 1995–2012. Survival probabilities were estimated with the direct adjustment method based on a stratified Cox model.31 MI = myocardial infarction.
Trends in Incident and Recurrent Myocardial Infarction Rates in the Population
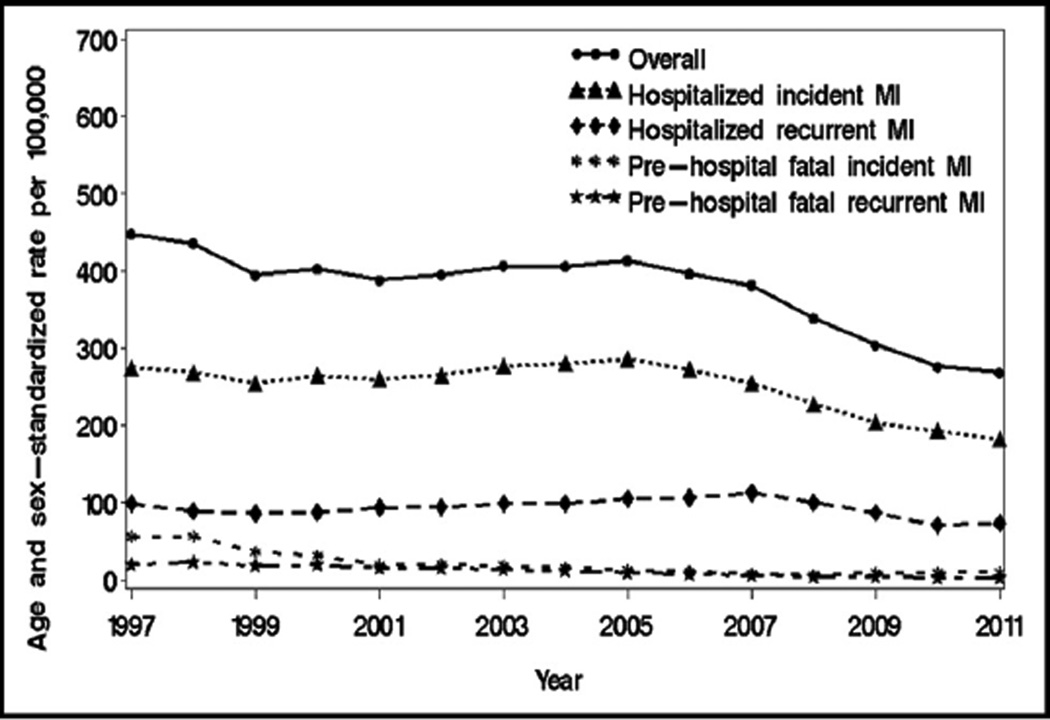
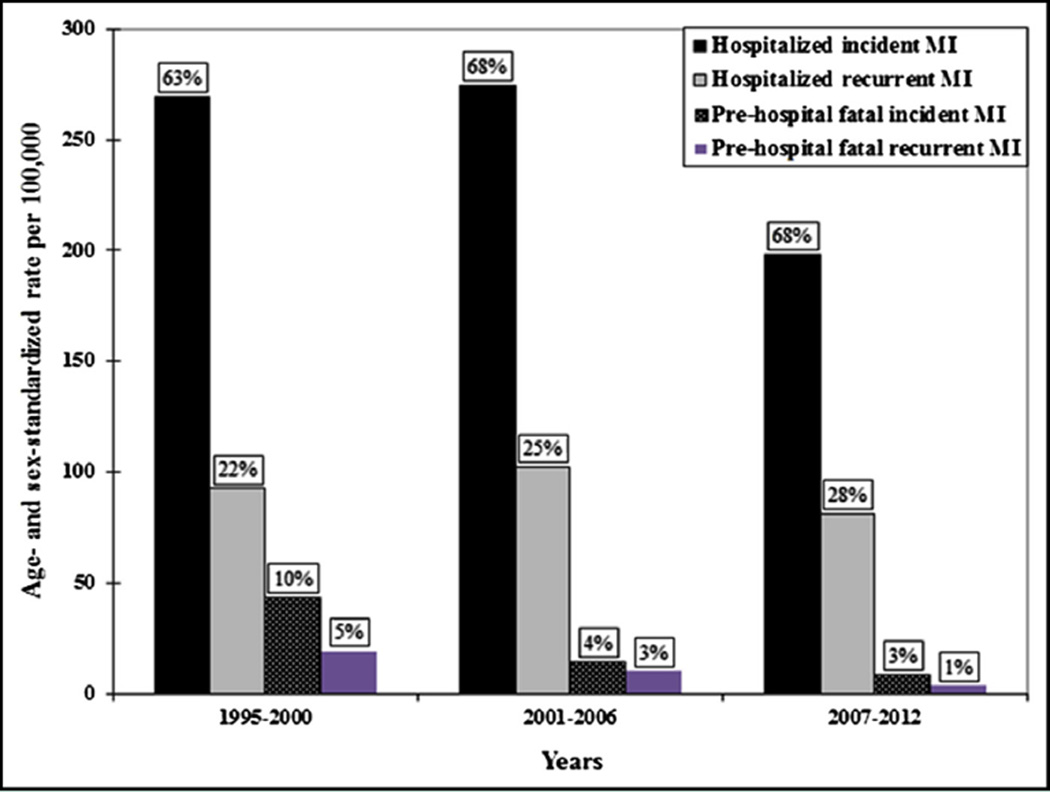
Temporal trends in the age- and sex-standardized incident and recurrent rates by prehospital death/hospitalized myocardial infarction are depicted in Figure 2; the corresponding APCs, overall and by age groups and sex, are summarized in the Table. Although the overall rate of myocardial infarction declined over time (APC −3.3; 95% CI, −2.8, −3.8), the magnitude of the decline varied widely. Incident hospitalized myocardial infarction rate fell 2.7%/y (95% CI, −2.1, −3.3), compared with decreases of 1.5%/y (95% CI, −0.5, −2.6) in recurrent hospitalized myocardial infarction, 14.1%/y (95% CI, −11.9, −16.2) in prehospital fatal incident myocardial infarction, and 12.3%/y (95% CI, −9.2, −15.2) in prehospital fatal recurrent myocardial infarction (all P for diverging trends < .05). These trends altered the relative contribution of the above categories to overall rates, with increasing proportions of hospitalized and recurrent myocardial infarctions (Figure 3). Among hospitalized myocardial infarctions, the proportion of recurrent events increased from 25.3% in 1995–2000 to 26.8% in 2001–2006, and to 29.0% in 2007–2012 (P for trend = .02). The average reduction in overall myocardial infarction rates was greater for residents aged 75 years or older than for younger people (P for interaction = .03). The latter interaction resulted primarily from a steeper decline in hospitalized incident myocardial infarction rates among older people. No additional interactions were detected, except for a greater decline in prehospital fatal incident myocardial infarction in men vs women (Table).
Figure 2.
Temporal trends in myocardial infarction rates. Myocardial infarction rates according to incident/recurrent and hospitalization status in Olmsted County, Minnesota, 1995 to 2012. Yearly rates (smoothed using 3-year moving average) per 100,000 persons have been standardized by the direct method to the age and sex distribution of the US population in 2010. MI = myocardial infarction.
Table.
Average Annual Percentage Change (95% Confidence Interval) in Rates of Myocardial Infarction (MI), Overall and in Selected Subgroups, Among Olmsted County, Minnesota, Residents from 1995–2012
| Sex | Age | ||||||
|---|---|---|---|---|---|---|---|
| MI Category | Overall | Men | Women | PInteraction | <75 Years | ≥75 Years | PInteraction |
| All MIs | −3.3 (−2.8, −3.8) | −3.4 (−2.8, −4.1) | −2.9 (−2.1, −3.6) | .20 | −3.0 (−2.3, −3.7) | −3.5 (−2.8, −4.3) | .03 |
| Hospitalized incident MI | −2.7 (−2.1, −3.3) | −2.6 (−1.8, −3.5) | −2.5 (−1.5, −3.5) | .69 | −2.5 (−1.6, −3.3) | −2.9 (−1.9, −3.8) | .07 |
| Hospitalized recurrent MI | −1.5 (−0.5, −2.6) | −1.8 (−0.4, −3.2) | −1.1 (0.5, −2.7) | .49 | −1.5 (0.1, −3.0) | −1.6 (−0.2, −3.0) | .93 |
| Prehospital fatal incident MI | −14.1 (−11.9, −16.2) | −16.1 (−13.1, −19.0) | −11.4 (−8.1, −14.6) | .03 | −14.3 (−11.1, −17.5) | −13.8 (−10.9, −16.6) | .43 |
| Prehospital fatal recurrent MI | −12.3 (−9.2, −15.2) | −14.3 (−10.2, −18.3) | −9.4 (−4.8, −13.9) | .11 | −16.2 (−9.7, −22.1) | −10.9 (−7.4, −16.3) | .11 |
Figure 3.
Changes over time in absolute and relative contribution of myocardial infarction categories to overall rates. Temporal trends in myocardial infarction rates (per 100,000 persons) in Olmsted County, Minnesota, from 1995 to 2012 partitioned into incident/recurrent status and prehospital death/hospitalized myocardial infarction. Rates have been standardized by the direct method to the age and sex distribution of the US population in 2010 and are shown in 6-year intervals. The labels represent the relative percentage of the myocardial infarction categories at each time interval. MI = myocardial infarction.
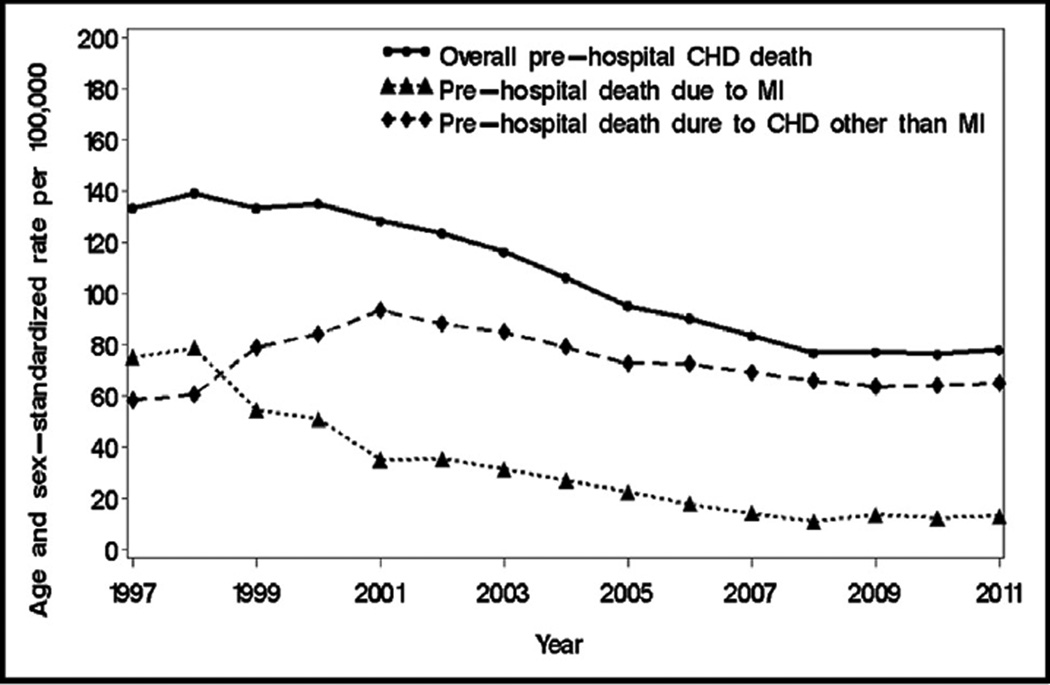
A sensitivity analysis was performed defining prehospital coronary heart disease death instead of prehospital myocardial infarction death (Figure 4). A temporal trend assessment revealed an average APC of −4.3 (95% CI, −3.3, −5.2) in prehospital coronary heart disease death rates. However, while prehospital death rates due to myocardial infarction declined steeply (APC −13.5; 95% CI, −11.7, −15.2), prehospital death rates due to coronary heart disease other than myocardial infarction did not change much (APC −0.4; 95% CI, 0.8, −1.6). The year-by-myocardial infarction/other coronary heart disease death interaction was highly significant (P < .001). Similarly, only a minor change was observed in prehospital death rates due to cardiovascular diseases other than myocardial infarction (APC −1.2; 95% CI, −0.4, −2.0), with a highly significant year-by-myocardial infarction/other cardiovascular death interaction (P < .001). Altogether, the results of these sensitivity analyses do not support any major or consistent shift in coding practices from myocardial infarction to other ICD codes.
Figure 4.
Temporal trends in prehospital coronary heart disease (CHD) death rates. CHD mortality rates partitioned into myocardial infarction and other coronary heart disease diagnoses in Olmsted County, Minnesota, 1995 to 2012. Yearly rates (smoothed using 3-year moving average) per 100,000 persons have been standardized by the direct method to the age and sex distribution of the US population in 2010. CHD = coronary heart disease; MI = myocardial infarction.
DISCUSSION
Summary of Findings
The present population-based surveillance study provides robust evidence for a temporal change in the case mix of myocardial infarction, with significant shifts toward recurrent events and hospitalized myocardial infarctions. Using data spanning 18 years (1995–2012), we demonstrated a steeper decline in incident than in recurrent myocardial infarction rates, which translated into an increasing proportion of recurrences over time. In addition, prehospital fatal myocardial infarction rates decreased substantially and became rare in recent years. As recurrent myocardial infarction confers a considerably worse prognosis than incident myocardial infarction, these findings stress the need to optimize prevention strategies.
Interpretation of Study Findings
The present study has several methodological strengths. The ability to accurately distinguish between incident and recurrent events in the population is rather unique to this setting because, through the Rochester Epidemiology Project, detailed medical histories that span each subject’s entire period of residency in the community are documented, indexed, and preserved.26,28 This is in contrast to previous studies, which have used a limited run-in (“lookback”) period (eg, 6 years in Smolina et al;14 7 years in Buch et al32) to distinguish incident from recurrent myocardial infarctions. Employing a run-in period can substantially overestimate the incidence rate (and underestimate the recurrence rate) if data covering a sufficient duration of time are unavailable.33 This may partly explain the large differences in the distribution of incident and recurrent myocardial infarctions found in previous studies. Indeed, the reported proportion of re-infarctions from all myocardial infarctions varied widely, ranging from 4%14 to 50% (for recurrent coronary heart disease).15 The observed proportion of recurrent myocardial infarction in our study was 28%, but has increased significantly over time. The latter proportion is comparable with the 31% reported by Rosamond et al3 in the Atherosclerosis Risk in Communities (ARIC) study from 1987–2008. However, we observed a steeper temporal decline in incident vs recurrent myocardial infarction rates, whereas in ARIC a more rapid decline in recurrent vs incident myocardial infarction was found. A possible explanation for this discrepancy may be the use of an upper age limit in ARIC. This is important considering the greater reduction in myocardial infarction rates in older (≥75 years) vs younger individuals observed herein from 1995–2012. In addition, different approaches were applied to define prehospital deaths.
As mentioned above, previous studies were inconsistent about the inclusion of prehospital deaths in their definition of myocardial infarction,1–3,14,15 which may introduce a sizable bias in rate estimates, particularly in the context of a temporal trend analysis. Indeed, a shift from fatal to nonfatal (hospitalized) myocardial infarction over time has been previously suggested, as a result of a steeper decline in the incidence of prehospital fatal myocardial infarction.24,34,35 Other studies used a broader definition of prehospital coronary heart disease death and found a less substantial secular reduction.3,36 Our data support a temporal shift from prehospital fatal to nonfatal hospitalized myocardial infarction, with relatively negligible changes in prehospital death rates due to coronary heart disease or cardiovascular diseases other than myocardial infarction.
Some limitations are important to consider. Temporal changes in diagnostic test validity, coding practice, and hospital admission policies may have impacted the observed trends. Troponin testing has attenuated downward trends in myocardial infarction incidence.1,3 Accordingly, the observed temporal decline in myocardial infarction rates may underestimate the true decline. The reliance on ICD codes as part of the algorithm used to define myocardial infarction is a limitation of such a surveillance approach. However, ICD code for acute myocardial infarction tends to be overall valid; indeed, in the ARIC study, 79% of the discharge ICD code 410 cases were confirmed as definite or probable myocardial infarction, whereas 14% were classified as no myocardial infarction.37 In the Corpus Christi Heart Project, ICD code 410 identified 81% of definite myocardial infarctions; 12% were classified as no myocardial infarction.38 Importantly, the validity of ICD code 410 to identify myocardial infarction in ARIC was stable from 1987 through 2000.39 Thus, misclassification of diagnostic coding is unlikely to have varied markedly during the study period, such that the trends described herein are robust.
These results from a single community, predominantly white, will need replication in other populations. Yet, comparisons of previous population-based studies of various chronic diseases in Olmsted County with those from other communities in the US indicate that the results for the population of this area can be extrapolated to a large part of the population of the country.25,27,28
Implications
Community-level event rates are the ultimate measures of successful clinical and public health efforts to reduce major causes of morbidity and mortality. Studies of myocardial infarction incidence and recurrence provide insight into the relative contribution of prevention and treatment to the decline in coronary heart disease rates.3 In general, the burden associated with myocardial infarction in the population is the result of both incidence rates, which are primarily driven by primary prevention, and recurrence rates, which are more influenced by quality of care during the acute phase, secondary prevention after discharge, and patients’ access to health care services.40,41 The shift toward recurrent myocardial infarction observed herein highlights the need to enhance secondary prevention efforts and quality efforts.40 Cardiac rehabilitation participation was shown to markedly reduce the risk of readmission and death after incident myocardial infarction.42 Yet, it remains underused, and improving participation rates could substantially impact postmyocardial infarction outcomes. Medication adherence is another key determinant of postmyocardial infarction outcome, with factors such as discharge medication counseling and postdischarge follow-up playing a potentially important role.43 In general, long-term risk factor control and lifestyle modification post myocardial infarction (eg, through smoking cessation, physical activity engagement, and improved dietary habits) may substantially reduce the risk of recurrent coronary heart disease events.44–46 Also of importance, however, is the recognition that preventing incident events will decrease the reservoir of patients at risk for recurrent myocardial infarction, thereby reducing recurrent myocardial infarction rates in the population.
CLINICAL SIGNIFICANCE.
Between 1995 and 2012, myocardial infarction (MI) rates declined in the community, but there were large differences in the trends according to incident/recurrent status and prehospital death/hospitalized MI.
This resulted in a temporal change in the case mix toward recurrent events and hospitalized MIs.
Recurrent MI confers a considerably worse prognosis than incident MI, stressing the need to optimize and update prevention strategies.
Acknowledgments
Funding: Funding was supported by the National Institutes of Health (R01 HL59205, R01 HL72435, and R01 HL120957) and made possible by the Rochester Epidemiology Project (R01 AG034676) from the National Institute on Aging.
Footnotes
Conflicts of Interest: None.
Authorship: All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: YG, SAW, and VLR.
Drafting of the manuscript: YG.
Critical revision of the manuscript for important intellectual content: YG, SAW, RJ, and VLR.
Statistical analysis: YG, SAW, and RJ.
Obtained funding: VLR.
Administrative, technical, and material support: VLR.
Study supervision: YG, VLR.
References
- 1.Roger VL, Weston SA, Gerber Y, et al. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 3.Rosamond WD, Chambless LE, Heiss G, et al. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.From the Centers for Disease Control and Prevention. Public health and aging: trends in aging—United States and worldwide. JAMA. 2003;289:1371–1373. [PubMed] [Google Scholar]
- 6.Towfighi A, Zheng L, Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med. 2009;169:1762–1766. doi: 10.1001/archinternmed.2009.318. [DOI] [PubMed] [Google Scholar]
- 7.Muntner P, DeSalvo KB, Wildman RP, et al. Trends in the prevalence, awareness, treatment, and control of cardiovascular disease risk factors among noninstitutionalized patients with a history of myocardial infarction and stroke. Am J Epidemiol. 2006;163:913–920. doi: 10.1093/aje/kwj124. [DOI] [PubMed] [Google Scholar]
- 8.Macchia A, Romero M, D’Ettorre A, et al. Temporal trends of the gaps in post-myocardial infarction secondary prevention strategies of comorbid and elderly populations vs. younger counterparts: an analysis of three successive cohorts between 2003 and 2008. Eur Heart J. 2012;33:515–522. doi: 10.1093/eurheartj/ehr410. [DOI] [PubMed] [Google Scholar]
- 9.Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 10.Koren A, Steinberg DM, Drory Y, Gerber Y. Socioeconomic environment and recurrent coronary events after initial myocardial infarction. Ann Epidemiol. 2012;22:541–546. doi: 10.1016/j.annepidem.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Gulliksson M, Wedel H, Koster M, Svardsudd K. Hazard function and secular trends in the risk of recurrent acute myocardial infarction: 30 years of follow-up of more than 775,000 incidents. Circ Cardiovasc Qual Outcomes. 2009;2:178–185. doi: 10.1161/CIRCOUTCOMES.108.802397. [DOI] [PubMed] [Google Scholar]
- 12.Jokhadar M, Jacobsen SJ, Reeder GS, et al. Sudden death and recurrent ischemic events after myocardial infarction in the community. Am J Epidemiol. 2004;159:1040–1046. doi: 10.1093/aje/kwh147. [DOI] [PubMed] [Google Scholar]
- 13.Crow RS, Hannan PJ, Jacobs DR, Jr, et al. Eliminating diagnostic drift in the validation of acute in-hospital myocardial infarction—implication for documenting trends across 25 years: the Minnesota Heart Survey. Am J Epidemiol. 2005;161:377–388. doi: 10.1093/aje/kwi048. [DOI] [PubMed] [Google Scholar]
- 14.Smolina K, Wright FL, Rayner M, Goldacre MJ. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ Cardiovasc Qual Outcomes. 2012;5:532–540. doi: 10.1161/CIRCOUTCOMES.111.964700. [DOI] [PubMed] [Google Scholar]
- 15.Nedkoff L, Briffa TG, Knuiman M, et al. Temporal trends in the incidence and recurrence of hospitalised atherothrombotic disease in an Australian population, 2000–07: data linkage study. Heart. 2012;98:1449–1456. doi: 10.1136/heartjnl-2012-302181. [DOI] [PubMed] [Google Scholar]
- 16.Shotan A, Gottlieb S, Goldbourt U, et al. Prognosis of patients with a recurrent acute myocardial infarction before and in the reperfusion era—a national study. Am Heart J. 2001;141:478–484. doi: 10.1067/mhj.2001.112998. [DOI] [PubMed] [Google Scholar]
- 17.Nakatani D, Sakata Y, Suna S, et al. Incidence, predictors, and subsequent mortality risk of recurrent myocardial infarction in patients following discharge for acute myocardial infarction. Circ J. 2013;77:439–446. doi: 10.1253/circj.cj-11-1059. [DOI] [PubMed] [Google Scholar]
- 18.Bata IR, Gregor RD, Wolf HK, Brownell B. Trends in five-year survival of patients discharged after acute myocardial infarction. Can J Cardiol. 2006;22:399–404. doi: 10.1016/s0828-282x(06)70925-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rasoul S, Ottervanger JP, de Boer MJ, et al. Poor outcome after recurrent acute myocardial infarction: a plea for optimal secondary prevention. Int J Cardiol. 2011;147:298–300. doi: 10.1016/j.ijcard.2010.12.046. [DOI] [PubMed] [Google Scholar]
- 20.Kikkert WJ, Hoebers LP, Damman P, et al. Recurrent myocardial infarction after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol. 2014;113:229–235. doi: 10.1016/j.amjcard.2013.08.039. [DOI] [PubMed] [Google Scholar]
- 21.Shetty S, Halpern R, McCollam PL. Cost of care for new versus recurrent acute coronary syndrome patients. J Med Econ. 2008;11:81–99. doi: 10.3111/13696990801913968. [DOI] [PubMed] [Google Scholar]
- 22.Rogers WJ, Frederick PD, Stoehr E, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1026–1034. doi: 10.1016/j.ahj.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 23.Adabag AS, Therneau TM, Gersh BJ, et al. Sudden death after myocardial infarction. JAMA. 2008;300:2022–2029. doi: 10.1001/jama.2008.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dudas K, Lappas G, Stewart S, Rosengren A. Trends in out-of-hospital deaths due to coronary heart disease in Sweden (1991 to 2006) Circulation. 2011;123:46–52. doi: 10.1161/CIRCULATIONAHA.110.964999. [DOI] [PubMed] [Google Scholar]
- 25.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 26.Rocca WA, Yawn BP, St Sauver JL, et al. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.St Sauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from The Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.St Sauver JL, Grossardt BR, Yawn BP, et al. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mendis S, Thygesen K, Kuulasmaa K, et al. World Health Organization definition of myocardial infarction: 2008–09 revision. Int J Epidemiol. 2011;40:139–146. doi: 10.1093/ije/dyq165. [DOI] [PubMed] [Google Scholar]
- 30.Cox DR. Regression analysis and life table. J R Stat Soc (Series B) 1972;34:187–222. [Google Scholar]
- 31.Zhang X, Loberiza FR, Klein JP, Zhang MJ. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Methods Programs Biomed. 2007;88:95–101. doi: 10.1016/j.cmpb.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 32.Buch P, Rasmussen S, Gislason GH, et al. Temporal decline in the prognostic impact of a recurrent acute myocardial infarction 1985 to 2002. Heart. 2007;93:210–215. doi: 10.1136/hrt.2006.092213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brameld KJ, Holman CD, Lawrence DM, Hobbs MS. Improved methods for estimating incidence from linked hospital morbidity data. Int J Epidemiol. 2003;32:617–624. doi: 10.1093/ije/dyg191. [DOI] [PubMed] [Google Scholar]
- 34.Briffa T, Nedkoff L, Peeters A, et al. Discordant age and sex-specific trends in the incidence of a first coronary heart disease event in Western Australia from 1996 to 2007. Heart. 2011;97:400–404. doi: 10.1136/hrt.2010.210138. [DOI] [PubMed] [Google Scholar]
- 35.Messner T, Lundberg V, Bostrom S, et al. Trends in event rates of first and recurrent, fatal and non-fatal acute myocardial infarction, and 28-day case fatality in the Northern Sweden MONICA area 1985–98. Scand J Public Health Suppl. 2003;61:51–59. doi: 10.1080/14034950310001388. [DOI] [PubMed] [Google Scholar]
- 36.McGovern PG, Jacobs DR, Jr, Shahar E, et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 37.White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 38.Pladevall M, Goff DC, Nichaman MZ, et al. An assessment of the validity of ICD Code 410 to identify hospital admissions for myocardial infarction: the Corpus Christi Heart Project. Int J Epidemiol. 1996;25:948–952. doi: 10.1093/ije/25.5.948. [DOI] [PubMed] [Google Scholar]
- 39.Rosamond WD, Chambless LE, Sorlie PD, et al. Trends in the sensitivity, positive predictive value, false-positive rate, and comparability ratio of hospital discharge diagnosis codes for acute myocardial infarction in four US communities, 1987–2000. Am J Epidemiol. 2004;160:1137–1146. doi: 10.1093/aje/kwh341. [DOI] [PubMed] [Google Scholar]
- 40.Kangovi S, Grande D. Hospital readmissions—not just a measure of quality. JAMA. 2011;306:1796–1797. doi: 10.1001/jama.2011.1562. [DOI] [PubMed] [Google Scholar]
- 41.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 42.Dunlay SM, Pack QR, Thomas RJ, Killian JH, Roger VL. Participation in cardiac rehabilitation, readmissions and death after acute myocardial infarction. Am J Med. 2014;127(6):538–546. doi: 10.1016/j.amjmed.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jackevicius CA, Li P, Tu JV. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation. 2008;117:1028–1036. doi: 10.1161/CIRCULATIONAHA.107.706820. [DOI] [PubMed] [Google Scholar]
- 44.Gerber Y, Myers V, Goldbourt U, et al. Long-term trajectory of leisure time physical activity and survival after first myocardial infarction: a population-based cohort study. Eur J Epidemiol. 2011;26:109–116. doi: 10.1007/s10654-010-9523-8. [DOI] [PubMed] [Google Scholar]
- 45.Gerber Y, Rosen LJ, Goldbourt U, et al. Smoking status and long-term survival after first acute myocardial infarction. J Am Coll Cardiol. 2009;54:2382–2387. doi: 10.1016/j.jacc.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 46.Li S, Chiuve SE, Flint A, et al. Better diet quality and decreased mortality among myocardial infarction survivors. JAMA Intern Med. 2013;173:1808–1818. doi: 10.1001/jamainternmed.2013.9768. [DOI] [PMC free article] [PubMed] [Google Scholar]