Abstract
The objective of this study is to valuate two biomarkers that may guide nutritional assessment during follow up after intestinal transplantation. We performed a retrospective study on prospectively collected data of insulin-like growth factor-1 (IGF-1) and effluent calprotectin in patients undergoing intestinal transplantation. Optimal nutritional status (ONS) was defined by using the Malnutrition Universal Screening Tool (MUST). IGF-1 and calprotectin were correlated with ONS by Pearson correlation. Eighteen cadaveric intestinal transplants were performed over 1,650 days (median follow up 425 days, range 29–1,650 days). Mean IGF-1 and calprotectin were significantly associated with independent nutrition. Seven patients became malnourished on one or more occasions. During malnutrition the mean IGF-1 was 22 ± 14 ng/ml and calprotectin 1,597 ± 1,055 mcg/g. Mean weight during episodes of malnutrition changed from 64.77 ± 8.76 kg to 59.05 ± 8.5 kg (–8.9 ± 1.25%). Both IGF-1 and calprotectin negatively correlated with ONS (Pearson’s r, –0.612, p = 0.014). Patients broadly aligned with three groups: nutritionally replete (normal IGF-1 and normal calprotectin), nutritionally equivocal (normal or low normal IGF-1 and high calprotectin), and malnourished (low IGF-1 and high calprotectin). Patients with low IGF-1 and high calprotectin may have a benign clinical presentation. However it is in their interests to have parenteral nutrition restarted pending further investigation.
Keywords: IGF-1, calprotectin, intestinal transplantation, nutritional status
Introduction
Intestinal transplantation (ITx) has added a new dimension to the management of patients with irreversible intestinal and parenteral nutrition failure.(1) A good measure of its success not only involves having a patient alive, well and off parenteral nutrition (PN), but having a patient that is nutritionally replete. Thus evaluating successful nutritional function after transplant needs objective measures to avoid delays in decision making that might compromise the graft.
The aim of this study is to determine whether IGF-1 and calprotectin in combination can act as potential biomarkers, to stratify patients into distinct nutritional categories. These may range from being nutritionally replete to malnourished. The patients that have clinical signs of bowel dysfunction are easy to spot, however it is the ones that are clinically ’well’ that are the focus of this article.
Materials and Methods
Between October 2008 and January 2013, our centre performed 18 cadaveric intestinal transplantations. There were 11 males and 7 females. Mean age at transplantation was 43.8 years (range 23–73). The cause of intestinal insufficiency was Crohn’s disease in 4/18 (23%), mesenteric infarction in 4/18 (23%), visceral neuropathy in 3/18 (17%), radiation enteritis in 2/18 (11%), desmoid tumour in 2/18 (11%), volvulus in 1/18 (5%), necrotizing enterocolitis in 1/18 (5%) and ulcerative colitis in 1/18 (5%). The patients were consecutive and all operations were performed by one surgeon. Two patients underwent a modified multi-visceral ITx, 10 isolated small bowel, 1 isolated small bowel and kidney and 5 isolated small bowel and abdominal wall transplant.
We have been prospectively measuring IGF-1 levels in patients undergoing intestinal transplantation at the following time lines: pre-transplant, at 3 month intervals for a year and then annually. IGF-1 is a protein that is encoded by the IGF1 gene. IGF-1 is a hormone similar in molecular structure to insulin. It plays an important role in childhood growth and continues to have anabolic effects in adults. IGF-1 represents a biochemical marker of malnutrition and a sensitive index of nutritional repletion.(2) Measurement of IGF-1 with the available commercial kits is easy and inexpensive, and in clinical practice it may be useful both to provide better diagnostic information and to monitor nutritional changes during treatment.(2)
Effluent calprotectin levels were measured at 3 month intervals for a year and then annually. Calprotectin is a 36 kDa calcium and zinc binding protein expressed by the gene S100 calcium-binding protein A8, S100A8. It accounts for 30 to 40% of neutrophils’ cytosol. In vitro studies show it has bacteriostatic and fungistatic properties. It is resistant to enzymatic degradation, and can be easily measured in faeces.(3) Measurement of faecal calprotectin is a biochemical test for inflammatory bowel disease. An increased Calprotectin concentration in stool is the direct consequence of neutrophil degranulation due to mucosal damage. The main diseases that cause an increased excretion of faecal calprotectin are Crohn’s disease, ulcerative colitis and neoplasms (cancer). Levels of faecal calprotectin are normal in patients with irritable bowel syndrome (IBS).(4)
Optimal nutritional status (ONS) was defined by using the Malnutrition Universal Screening Tool (MUST) (Accessed 21 Jan 2014, http://www.bapen.org.uk/screening-for-malnutrition/must/introducing-must). A patient was defined as being malnourished with a score of 1 and above.
IGF-1 and calprotectin were correlated with ONS by Pearson correlation. A grading scheme reflecting optimal nutritional status was derived using these IGF-1 and effluent calprotectin values symbiotically.
Analyses were conducted using SPSS 21.0 (SPSS Inc, Chicago, IL). Descriptive statistics were calculated for all variables. Normality of data was checked using the Shapiro-Wilk test. Normally distributed continuous variables were expressed as mean ± SD and compared with the t test; otherwise they were expressed as median and interquartile range (IQR) and the Mann-Whitney test was used. All reported p values are two-sided and a p value of <0.05 was considered statistically significant.
Results
Eighteen cadaveric intestinal transplants were performed over 1,650 days (median follow up 425 days, range 29–1,650 days). All patients successfully weaned from parenteral to enteral nutrition. Mean IGF-1 and calprotectin were significantly associated with independent nutrition (p = 0.039 and 0.008 respectively). IGF-1 increased two-fold (mean 17 ± 5 ng/ml before and 36 ± 16 ng/ml 1 year after transplant, p = 0.003). Effluent calprotectin was 55 ± 43 mcg/g at 1 year.
Post transplantation, 7 patients became malnourished on one or more occasions. MUST score was 2 for 2 patients and 1 for 5, during episodes of malnutrition. During malnutrition (n = 7/18) the mean IGF-1 was 22 ± 14 ng/ml and calprotectin 1,597 ± 1,055 mcg/g. Mean weight during episodes of malnutrition decreased from 64.77 ± 8.76 kg to 59.05 ± 8.5 kg (–8.9 ± 1.25%).
IGF-1 and calprotectin levels show a strong negative correlation coefficient at –0.612 (Pearson’s r, p = 0.144). When compared to routine levels, mean IGF-1 and calprotectin levels during malnutrition episodes show statistical significance (p = 0.039 and 0.008 respectively).
Discussion
As intestinal transplantation takes its place as a recognized option for patients with irreversible intestinal failure, objective measurement of functional outcomes has become an important factor in assessing its success.
Being nutritionally replete without the need for total parenteral nutrition (TPN) is a desired outcome after successful transplant. But how does one measure this status of being nutritionally replete? Furthermore, is there more than one category of nutritionally replete patients after successful transplantation? Is it possible that even though patients are independent from TPN, they are still not nutritionally replete due to some underlying process that may come to light to cause bowel dysfunction? And finally, more importantly, can we objectively identify these patients, long before there is irreversible damage to the bowel?
Nutritional management is a key component of post-ITx management, in the context of possible previous malnourishment and a newly created intestinal anatomy. However, the nutritional biomarkers that can guide us through appropriate decision making, i.e., amending the nutritional regimen have yet to be determined.
Our results suggest that IGF-1 levels show statistically significant increase as early as 3 months post-ITx. This is what we would expect from patients that have achieved full clinical nutritional autonomy. Calprotectin levels remain fairly stable during periods of uneventful allograft function. However, during episodes of malnutrition Calprotectin levels increase significantly and IGF-1 decrease. Our results confirm a strong negative correlation coefficient that almost reaches statistical significance (p = 0.144).
Our study is a retrospective cohort study with potential limitations. The number of patients included in our study is small and therefore significant conclusions cannot be safely extracted. Relatively short follow up is another limitation and therefore our results will have to be verified by longer studies.
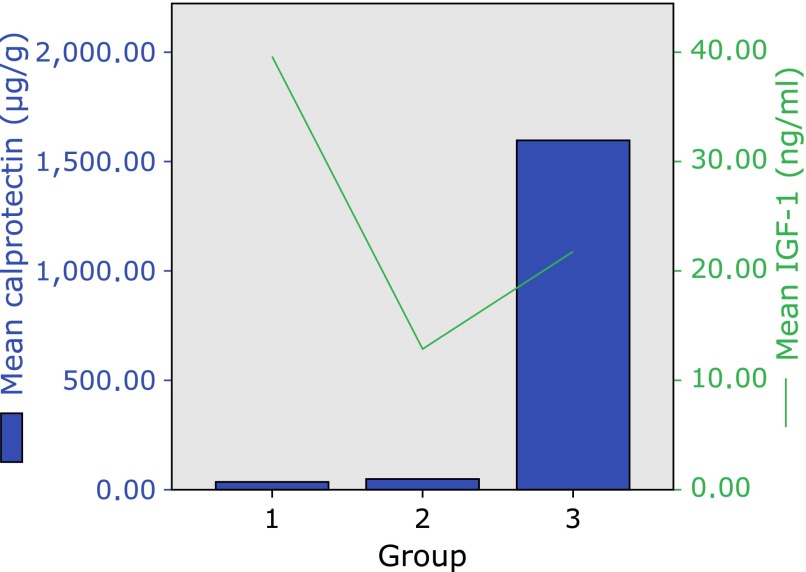
Three groups of patients were evident from this analysis. Group 1 (Nutritionally replete): Patients with normal IGF-1 and normal calprotectin. Group 2 (equivocal nutritional parameters): Patients with normal or low normal IGF-1 and high calprotectin. Group 3 (malnourished): Patients with low IGF-1 levels and high calprotectin. Fig. 1 depicts the mean IGF-1 and calprotectin levels for the 3 distinct groups.
Fig. 1.
This graph depicts the advantage of a dynamic measurement of a patient’s nutritional status. Group 3 in particular shows a high Calprotectin and a low to normal IGF-1. In this scenario appropriate interventions are required to assure that the IGF-1 does not drop.
By stratifying ITx patients into 3 groups we introduce a guide for appropriate decision making. Group 1 patient is at optimal nutritional status and can be followed up routinely. These patients perhaps do not require frequent intensive monitoring. Group 2 patient presents with equivocal findings and follow up/investigations may have to be tailored for the individual patient. Group 3 patients are at high risk of loss of graft. These patients need to be further investigated as the biomarkers suggest malnutrition and bowel inflammation. Rejection and infection need to be excluded and nutrition optimized.
Furthermore, we propose that group 3 (low IGF-1 levels and high calprotectin) should have enteral feeding interrupted and be put back on TPN till cause of high calprotectin is determined.
Conflict of Interest
No potential conflicts of interest were disclosed.
References
- 1.Fishbein TM. Intestinal transplantation. N Engl J Med. 2009;361:998–1008. doi: 10.1056/NEJMra0804605. [DOI] [PubMed] [Google Scholar]
- 2.Caregaro L, Favaro A, Santonastaso P, et al. Insulin-like growth factor 1 (IGF-1), a nutritional marker in patients with eating disorders. Clin Nutr. 2001;20:251–257. doi: 10.1054/clnu.2001.0397. [DOI] [PubMed] [Google Scholar]
- 3.Tibble J, Teahon K, Thjodleifsson B, et al. A simple method for assessing intestinal inflammation in Crohn’s disease. Gut. 2000;47:506–513. doi: 10.1136/gut.47.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Costa F, Mumolo MG, Ceccarelli L, et al. Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn’s disease. Gut. 2005;54:364–368. doi: 10.1136/gut.2004.043406. [DOI] [PMC free article] [PubMed] [Google Scholar]