Abstract
The reliability and accuracy of five portable blood lactate (BLa) analysers (Lactate Pro, Lactate Pro2, Lactate Scout+, Xpress™, and Edge) and one handheld point-of-care analyser (i-STAT) were compared to a criterion (Radiometer ABL90). Two devices of each brand of analyser were assessed using 22 x 6 mL blood samples taken from five subjects at rest and during exercise who generated lactate ranging ~1-23 mM. Each sample was measured simultaneously ~6 times on each device. Reliability was assessed as the within-sample standard deviation (wsSD) of the six replicates; accuracy as the bias compared with the ABL90; and overall error (the root mean squared error (√MSE)) was calculated as the square root of (wsSD2 and bias2). The √MSE indicated that both the Edge and Xpress had low total error (~0-2 mM) for lactate concentrations <15 mM, whereas the Edge and Lactate Pro2 were the better of the portable analysers for concentrations >15 mM. In all cases, bias (negative) was the major contribution to the √MSE. In conclusion, in a clinical setting where BLa is generally <15 mM the Edge and Xpress devices are relevant, but for athlete testing where peak BLa is important for training prescription the Edge and Lactate Pro2 are preferred.
Key points.
The reliability of five common portable blood lactate analysers were generally <0.5 mM for concentrations in the range of ~1.0-10 mM.
For all five portable analysers, the analytical error within a brand was much smaller than the biological variation in blood lactate (BLa).
Compared with a criterion blood lactate analyser, there was a tendency for all portable analysers to under-read (i.e. a negative bias), which was particularly evident at the highest concentrations (BLa ~15-23 mM).
The practical application of these negative biases would overestimate the ability of the athlete and prescribe a training intensity that would be too high.
Key words: Bias, precision, root mean squared error, analytical performance
Introduction
Monitoring of blood lactate (BLa) concentration during exercise is commonplace in sports physiology laboratories and in the field. This is due to the ease of capillary blood sampling and the predictive and evaluative power of the lactate response to incremental exercise (Wasserman et al., 1973). Blood lactate concentration during a graded exercise step test is used to identify the transition between aerobic and anaerobic energy contribution to exercise and therefore assess endurance capacity and performance potential (Faude et al., 2009). The underlying exponential relationship between intensity (workload) and BLa concentration (Binder et al., 2008) allows sport scientists to quantitatively evaluate training adaptation, exercise work rate and to prescribe training intensities (Beneke et al., 2011, Faude et al., 2009). Furthermore, lactate thresholds (LT) are considered superior to measurements of maximal oxygen uptake (VO2max) when differentiating endurance performance in elite athletes (Bentley et al., 2007).
When interpreting BLa test results, consideration should be given to the reliability and accuracy of the equipment used. Several studies have evaluated commonly used hand-held analysers such as the Lactate Pro (Arkray, Japan) (McNaughton et al., 2002; Pyne et al., 2000; van Someren et al., 2005) and the Lactate Scout+ (SensLab GmbH, Germany). The most recent of these was conducted by Tanner et al. (2010) who noted that the Lactate Pro and the Lactate Plus (Nova Biomedical, USA) displayed good reliability and accuracy compared with a criterion laboratory analyser. However, the Lactate Pro and associated consumables, currently used in laboratories worldwide, has been superseded with a new model, the Lactate Pro2. Other models of portable lactate analysers have entered the market in the last few years and, consequently, an evaluation of the suitability of a range of next-generation portable BLa analysers is warranted. The aim of the current study was twofold; first to assess the reliability and accuracy of five portable lactate analysers, as well as one handheld point-of-care analyser (i-STAT) and, secondly, to quantify the effect of any bias upon calculated power/lactate and heart-rate/lactate thresholds, since these are common applications of blood lactate data.
Methods
Subjects
Three male and two female recreationally active staff members (age = 25 ± 1.8 years, height = 1.74 ± 0.13 m and body mass = 73.2 ± 16.9 kg) from the Australian Institute of Sport Physiology Discipline were recruited to participate in the study. All subjects were healthy and engaged regularly in ≥ 120 minutes of physical activity per week. They each signed an informed consent form prior to commencement of the study, which was approved by the Ethics Committee of the Australian Institute of Sport.
Lactate analysers
Five portable BLa analysers (Lactate Pro, Lactate Pro2, Lactate Scout+, StatStrip® Xpress™ Meter and The Edge) and one point-of-care analyser (i-STAT) were evaluated concurrently against a criterion blood analyser (Model ABL90, Radiometer, Copenhagen, Denmark). A second laboratory analyser (Model ABL715, Radiometer, Copenhagen, Denmark) was also used for a small number of comparisons to the ABL90, since the ABL715 has been used as a criterion in two previous evaluations of portable lactate analysers (Pyne et al., 2000; Tanner et al., 2010). All portable/point-of-care analysers operate on a similar principle; an enzymatic amperometric detection method (Table 1). These devices interpret the electrical signal produced as a result of the reaction between lactate in the blood and the enzyme lactate oxidase on the inserted sensor. The voltage signal corresponds directly to the lactate concentration of the sample. The Nova Statstrip® Xpress Meter (Xpress) operates using a slightly different analysis technology. The Xpress biosensor is housed in the pre-calibrated StatStrip® Multi-Well test strip that corrects for interfering substances such as haematocrit, acetaminophen, uric acid and ascorbic acid.
Table 1.
Specifications for five portable and one (i-STAT) point-of-care blood lactate analysers.
| Radiometer ABL90 |
Lactate Pro |
Lactate Pro2 |
Lactate Scout+ |
Nova Statstrip Xpress |
Edge | i-STAT | |
|---|---|---|---|---|---|---|---|
| Manufacturer | Radiometer, Denmark | Arkray KDK, Japan | Arkray KDK, Japan | EKF Diagnostics, Germany | Nova Biomedical, USA | Transatlantic Science, USA | Abbott Laboratories, USA |
| Method | Amperometric metabolite sensor | Amperometric reagent | Amperometric reagent | Enzymatic amperometric | Electrochemical biosensor StatStrip® Multi-well design | Electrochemical biosensor | Amperometric CG4+ cartridge |
| Sample VOL, µL | 65 | 5 | 0.3 | 0.5 | 0.7 | 3 | 95 |
| Analysis time, s | 65 | 60 | 15 | 10 | 13 | 45 | 280 |
| MEAS range, mM | 0.1-31.0 | 0.8-23.3 | 0.5-25.0 | 0.5-25.0 | 0.3-20.0 | 0.7-22.2 | 0.30-20.0 |
VOL = volume; MEAS = measurement
The Radiometer ABL90 (Radiometer, Copenhagen, Denmark) operates using an amperometric metabolite sensor involving two electrodes and one anode covered by a multi-layer membrane bound to the sensor board. The lactate concentration in a sample is calculated by measuring the amount of electrical current flowing through the electrode chain, which is proportionate to the concentration of lactate being oxidised. The same measurement methodology is employed in the previous-generation ABL-700 and -800 series analysers. The ABL90 is traceable to primary standards at Radiometer (Copenhagen, Denmark) and according to its operating manual has a bias of 0.02 mM at 0.17 mM and 0.03 at 12.50 mM. Multiple metabolite sensors are housed in a compact cassette form with automated calibration and quality control procedures. The ABL90 requires a 65 µL blood sample. The measuring time is 35 s and the full analysis cycle including rinsing is 65 s. It is for these reasons the ABL90 was chosen over previous models that require larger sample volume and longer analysis time.
Experimental design
A nested repeated measures study design was employed using ~6 mL venous blood samples taken from each of five subjects at rest, as well as during four to six levels of treadmill exercise. A total of 22 blood samples were obtained; four samples from each of four subjects and six samples from one subject. Each blood sample was aliquotted into 11 capillary tubes that were analysed repeatedly (~4-6 replicates) on one of the eight different lactate analysers. Finally, two devices of each of the six portable/point-of-care analysers were assessed concurrently.
Subjects were prepared with a 21 g cannula (Jelco, Smiths Medical, Southington, USA) inserted into a forearm vein to enable blood to be drawn at selected times using a 6 mL sodium heparin Vacutainer (Greiner Bio-One – Kremsmünster, Austria). To obtain lactate values across the physiological range, blood samples were drawn at rest as well as after subjects had completed multiple 5-minute treadmill workloads designed to elicit lactate concentrations that could be classified as low (0.5 – 4 mM), moderate (>4-<8 mM) and high (>8 mM). As such, treadmill workloads were individualised to each subject; after five minutes at each nominated workload a finger-prick lactate sample was taken to assess if the target lactate concentration (via Lactate Pro) had been achieved, if not, exercise recommenced at the same speed with 1% increases in gradient each minute thereafter until the target range was reached. After each 6 mL blood sample was drawn, the Vacutainer was mixed thoroughly by hand and aliquotted promptly into eleven 100 µL balanced heparin capillary tubes to ensure all samples were of a consistent lactate concentration. The eleven capillary tubes were filled simultaneously in groups of two or three and all eleven tubes were filled in ~ 80 s. The capillary tubes of each blood sample were distributed to the researchers in random order to minimise any order and time effects. Blood collection and processing were conducted in the laboratory at 22-24 oC and at 26-41% relative humidity.
Seven researchers were used to run blood samples through the different brands of analysers concurrently, to minimise the change in lactate over time in vitro (Jones et al., 2007; Seymour et al., 2011). Aside from the Radiometer ABL90, each researcher tested two devices of the same brand so that between-device within-brand reliability could be investigated. For the portable analysers, five 100 µL capillary tubes (one per brand) were used to run six replicates through each portable analyser device in random order. All replicates were time matched to the sample run through the Radiometer ABL90. The researcher testing the i-STAT devices used the remaining volume in the 6 mL Vacutainer to pipette blood into the i-STAT cartridges for analysis, also time-matched to the Radiometer ABL90 replicates. However, due to the longer analysis time of the i-STAT only three replicates were run. All analysers were calibrated prior to testing according to the manufacturer’s instructions. The researcher operating the Radiometer ABL90 acted as a timekeeper ensuring synchronicity of the analyses. In addition, three-to-four replicates of six blood samples were run on one Radiometer ABL715 analyser at the same time as on the designated criterion Radiometer ABL90, to enable a truncated comparison between two different laboratory analysers from the same manufacturer.
Statistical analysis
Although the treadmill workloads were designed to elicit lactate concentrations that could be classified as low, moderate and high, analysis was conducted with the concentrations in five bands as follows 0-1.9, 2.0-4.9, 5.0-9.9, 10.0-14.9 and >15.0 mM. Given that the within-sample variability of the data increased as the mean increased, consideration was given to transforming the data using logs.
Blood lactate stability over time: Linear regression of lactate values on time (between drawing the blood sample and its analysis) was used to estimate the slopes of the change in measured lactate after the sample was collected. Slopes were estimated separately for each of the samples using each of the 14 analysers (seven brands with two devices per brand). Most analysers used 22 samples, though the two Scout+ devices used 21 samples, the two i-STAT devices used eight samples, and the Radiometer 715 only six samples.
Reliability and bias: For each blood sample, and separately for each device for each brand of analyser, reliability was calculated as the within-sample standard deviation (SD) and bias as the difference between the mean for the particular analyser and the mean of the criterion analyser (Radiometer ABL90). The data used in these analyses were all matched by time; that is, seconds after the taking of the blood sample.
Overall error (√Mean Squared Error) and correction for Bias: The square root of the (estimated) mean squared error (√MSE) of the 22 blood samples was used to generate an overall measure of error for each brand. The MSE provides a way of combining the within-sample SD and the sample bias into a single measure, which is calculated as follows:
Taking the square-root of the MSE provides a measure that has the same units as the within-sample SD and the bias; for the untransformed data the units are (all) mM.
All of the larger values of MSE were found to be associated with larger values of the bias, rather than larger values of the within-sample SD, so it might be possible to improve matters by reducing the bias. A simple way to do this is to fit a linear regression of Radiometer ABL90 values on the values obtained with one of the other analysers, and then to use this relationship to predict the Radiometer ABL90 reading using the reading on the other analyser. This concept of correcting for bias was assessed using the Edge analysers as an example. Linear regressions of Radiometer ABL90 data on Edge were fitted separately for the two Edge analysers (device A and B). These equations were then applied to both the EdgeA and EdgeB data, and revised biases calculated for each sample. The idea behind using the formulae obtained using the EdgeB data on the EdgeA data is that it is likely to be a better indication of how the formulae might work on future data.
Between-device within-brand variation and analytical error: For each band of lactate values and each brand of analyser, and with Device and Sample treated as random effects, the lme4 package (Bates et al., 2014) available as part of R (R Foundation for Statistical Computing, 2014) was used to estimate the between-devices within-brands and the analytical (or residual) error standard deviations. The analytical error consists mainly of measurement error but also includes variation due to differences between measurements made at different times as ‘time’ was not allowed for in the models fitted here. With only two devices per brand of analyser, estimates of the between-devices SDs have poor precision and to assist with interpretation of results, tests of differences between the pairs of devices, for each band and each brand, were also carried out with Device treated as a fixed effect. In order to obtain estimates of the analytical error standard deviations that could be directly compared to those reported in other studies (for instance, McNaughton et al., 2002), the random effects model was also, somewhat inappropriately, fitted separately for each brand of analyser using all of the samples for the brand. One of the assumptions of the model fitted is that the error standard deviation is constant over the range of data used, and while this assumption is reasonable within each of the five lactate concentration bands, for each brand, it is not reasonable over the combined bands. In addition it should be noted that any estimates obtained using combined data will depend on the distribution of lactate values that happen to be used so that any differences reported by different studies could be due, solely, to different distributions of lactate values.
Practical implications: From the AIS laboratory records, a representative de-identified data set of BLa concentration versus power was selected randomly for each of cycling and rowing incremental step-tests (Bourdon, 2013), and it was assumed that these values were generated using the criterion BLa concentration from the Radiometer ABL90. In order to quantify the practical impact different analysers would have on the comparison of longitudinal training prescription, the respective mean bias within each concentration band, for each portable analyser, were entered into ADAPT software (Australian Institute of Sport, 1995). This software fits a third order polynomial to lactate versus exercise intensity data to derive the power at both the first and second lactate thresholds (LT), referred to as LT1 (the lowest intensity at which there is a sustained increase in BLa concentration above resting values) and LT2 (the intensity that causes a rapid increase in BLa when production exceeds clearance), respectively (Bourdon, 2013). Specifically, the calculated LT’mod’ option within ADAPT was used to calculate LT2 using a ‘modified’ Dmax method of Cheng et al. (1992).
Results
This study design generated 1384 measurements of blood lactate (Table 2).
Table 2.
Sample sizes (number of replicates) for each brand of analyser used to estimate variance components.
| Analyser Brand |
Lactate concentration band (mM) | Total | ||||
|---|---|---|---|---|---|---|
| 0-1.9 | 2.0-4.9 | 5.0-9.9 | 10.0-14.9 | 15+ | ||
| Edge | 40 | 36 | 66 | 36 | 71 | 249 |
| i-STAT | 5 | 7 | 16 | 6 | 4 | 38 |
| Lactate Pro | 40 | 36 | 63 | 36 | 70 | 245 |
| Lactate Pro2 | 40 | 36 | 63 | 36 | 70 | 245 |
| Radiometer ABL90 | 23 | 21 | 38 | 21 | 41 | 144 |
| Radiometer 715 | 14 | 12 | 14 | 40 | ||
| Scout+ | 30 | 12 | 47 | 36 | 62 | 187 |
| Xpress | 40 | 36 | 63 | 33 | 70 | 242 |
| Total | 195 | 177 | 330 | 183 | 361 | 1384 |
Transformations
An inspection of the data clearly showed that the within-sample variability increased as the sample mean increased. This is typical for such data and often results in the use of a transformation to produce, approximate, constant variability. The transformation most commonly used is the log transformation, which will result in constant variance in situations where the coefficient of variation (CV) is constant. Here, while the log transformation did result in reasonably constant variation for samples with larger lactate values, the variability of the transformed data for samples with small values (lactate < 2 mM) was considerably greater than that for the other concentration bands. This was possibly due, in part, to the fact that lactate readings are only recorded to one decimal place, and whereas a difference of 0.1 represents only a 1% change for values around 10, it represents a 10% change for values around 1.
Qualitatively the results obtained with and without transforming the data were very similar and, for ease of interpretation, only the results obtained using the untransformed data are reported here.
Blood lactate stability over time
A change in lactate concentration over time for serial measures on the same blood sample was not consistently observed; the slope was estimated separately for each device for each blood sample, with samples measured an average of 5.5 times (range 2 to 7, median 6). Of the 262 individual slopes that were estimated, 25 were statistically significant (p < 0.05), of which seven were positive and 18 were negative (Table 3). Of the seven significant positive slopes, five were associated with mean blood lactate (from Radiometer ABL90) <5 mM, whereas of the 18 significant negative slopes, 13 were associated with mean lactate >10 mM. Overall, the mean pooled data for all brands of analyser show a trend to larger negative slopes at higher concentrations (Table 4, bottom row), with the largest negative slopes of -0.050 and -0.035 mM·min-1 at 10-14.9 and >15 mM, respectively.
Table 3.
Number and direction (positive or negative) of slopes for blood lactate concentration over time for each portable and laboratory analyser. For example, between 2.0 and 4.9 mM Edge B analysed three slopes; one of which was positive and two of which were negative as well as significant.
| Analyser Brand |
Lactate concentration band (mM) | All bands | ||||
|---|---|---|---|---|---|---|
| 0-1.9 | 2.0-4.9 | 5.0-9.9 | 10.0-14.9 | 15+ | ||
| Number Slopes (number +’ve/ number –’ve) | ||||||
| Edge A | 4(2/2) | 3(1/2) | 6(1/5) | 3(0/3*) | 6(1/5*) | 22 |
| Edge B | 4(2/2) | 3(1/2**) | 6(0/6) | 3(0/3**) | 6(0/6*) | 22 |
| i-STAT A | 1(1/0) | 2(2/0) | 3(3/0) | 1(1/0) | 1(1/0) | 8 |
| i-STAT B | 1(1*/0) | 2(2/0) | 3(3/0) | 1(0/1) | 1(1/0) | 8 |
| Lactate Pro A | 4(4/0) | 3(1/2) | 6(3/3) | 3(0/3*) | 6(0/6) | 22 |
| Lactate Pro B | 4(3/1) | 3(1/2) | 6(2/4) | 3(1/2) | 6(4/2) | 22 |
| Lactate Pro2 A | 4(2/2) | 3(2/1) | 6(3/3) | 3(1/2) | 6(1/5) | 22 |
| Lactate Pro2 B | 4(3/1) | 3(2/1) | 6(4/2) | 3(1/2) | 6(3/3) | 22 |
| Radiometer ABL90 | 4(2*/2) | 3(3*/0) | 6(3/3**) | 3(1/2) | 6(3/3) | 22 |
| Radiometer 715 | 2(1/1) | 2(1/1) | 2(1/1) | 6 | ||
| Scout+ A | 4(1/3*) | 2(1/1) | 6(0/6) | 3(0/3**) | 6(2/4**) | 21 |
| Scout+ B | 4(0/4) | 2(2/0) | 6(1/5) | 3(1/2*) | 6(0/6**) | 21 |
| Xpress A | 4(4/0) | 3(3/0) | 6(3*/3) | 3(1/2) | 6(2*/4) | 22 |
| Xpress B | 4(4*/0) | 3(3/0) | 6(3/3) | 3(1/2) | 6(5*/1) | 22 |
| All analysers |
46 (293*/173*) |
37 (251*/122*) |
74 (301*/442*) |
35 (8/277*) |
70 (242*/466*) |
262 |
* p < 0.05
Table 4.
Mean slope of lactate concentration over time for each of the portable and laboratory analysers.
| Analyser Brand |
Lactate concentration band (mM) | All bands | ||||
|---|---|---|---|---|---|---|
| 0-1.9 | 2.0-4.9 | 5.0-9.9 | 10.0-14.9 | 15+ | ||
| Mean slope (mM/min) | ||||||
| Edge A | -.010 | -.009 | -.027 | -.100 | -.077 | -.045 |
| Edge B | -.009 | -.032 | -.033 | -.152 | -.068 | -.054 |
| i-STAT A | .006 | .018 | .031 | .022 | .050 | .026 |
| i-STAT B | .008 | .073 | .025 | -.002 | .059 | .036 |
| Lactate Pro A | .008 | .000 | .033 | -.067 | -.050 | -.012 |
| Lactate Pro B | .002 | .000 | -.008 | -.021 | .004 | -.004 |
| Lactate Pro2 A | -.003 | .006 | .002 | -.011 | -.054 | -.015 |
| Lactate Pro2 B | .007 | .009 | .008 | -.038 | -.036 | -.010 |
| Radiometer ABL90 | .005 | .017 | -.019 | -.026 | -.038 | -.016 |
| Radiometer 715 | .005 | -.005 | -.007 | -.002 | ||
| Scout+ A | -.019 | -.011 | -.048 | -.083 | -.091 | -.056 |
| Scout+ B | -.016 | .028 | -.024 | -.040 | -.113 | -.045 |
| Xpress A | .017 | .018 | -.007 | -.025 | -.006 | -.001 |
| Xpress B | .015 | .042 | -.003 | -.024 | .110 | .034 |
| All analysers | .000 | .010 | -.008 | -.050 | -.035 | -.017 |
Reliability and bias
For each of the (up to) 22 samples, plots of the within-sample standard deviation versus the estimated bias (from the criterion Radiometer ABL90 readings), are given in Figure 1 with separate panels for the two devices (arbitrarily labelled A and B) of each brand of analyser and sub-panels for the different brands. By definition, all of the biases for the Radiometer ABL90 instrument are zero. Comparing the two panels for each brand of analyser it is evident that results from the two devices were very similar, both in terms of within-sample variability and bias.
Figure 1.
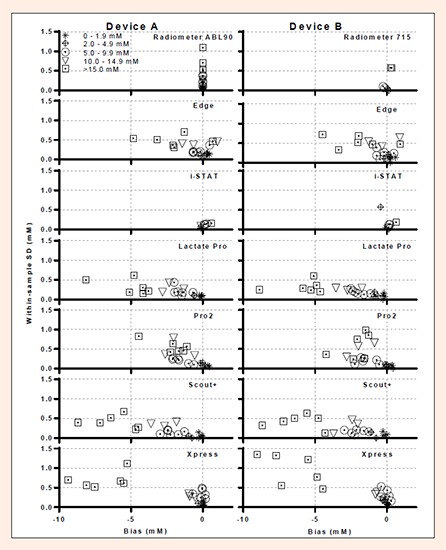
Mean Reliability (within-sample standard deviation (SD)) and Bias of the seven blood lactate analysers relative to the mean values obtained on the criterion analyser (Radiometer ABL90). The left panel show data for one device of each brand and the right panel show data for the second device of each brand including two laboratory based criterion analysers (Radiometer ABL90 and Radiometer 715). Each data point is the mean, or standard deviation, of an average of approximately six observations per sample.
All portable analysers except the i-STAT analyser showed mostly negative biases with the greatest bias seen when the BLa concentration was >15 mM (Figure 1).
√Mean Squared Error and correction for Bias
The √MSE indicated that both the Edge and Xpress had low ‘total’ error (~0-2 mM) for lactate concentrations <15 mM (Figure 2). The Lactate Pro2 was the best of the portable analysers for concentrations >15mM, whereas the Lactate Pro, Scout+ and Xpress each had large √MSE (~4-10 mM) for BLa >15 mM. The i-STAT devices and two Radiometers had the lowest error (~0-1 mM) throughout the measurement range evaluated.
Figure 2.

Total error calculated as square root of the mean squared error for the 14 blood lactate analysers (two devices for each of seven Brands) expressed relative to the mean lactate concentrations obtained on the criterion analyser (Radiometer ABL90).
The regression equations to correct the Edge for bias were:
| Radiometer ABL90 = -0.5538 + 1.12469 EdgeA, |
and
| Radiometer ABL90 = -0.5275 + 1.11769 EdgeB |
With the possible exception of lactate values in the range 10-14.9, use of these regressions reduced the bias of the Edge devices throughout the measurement range, and especially for the two extreme bands; from a mean of ~0.5 mM to 0.1 mM at lactate concentrations of 0-1.9 mM and from a mean of ~–2 mM to –0.5 mM at lactate concentrations >15 mM (Figure 3).
Figure 3.
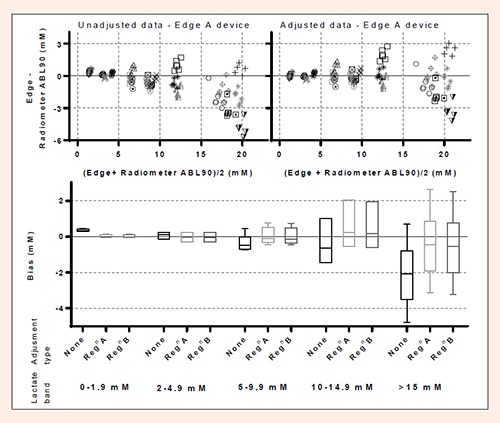
Bland-Altman plots of repeated sample measurements of blood lactate for one of the Edge devices (Device B) before (left top panel) and after (right top panel) correction using the Edge data to predict the criterion (Radiometer ABL90) measurements (see Methods for details). The bottom panel contains box plots of the overall mean data within one of five bands of lactate concentration before and after bias correction on Edge analyser (Device B) using its own regression-corrected data (RegnB) or the regression correction from the second device (RegnA); boxes indicate the (lower and upper) quartiles and whiskers the ranges, while the lines within the boxes indicate medians.
Between-device within-brand variation
There was generally very good agreement between the two devices of the same brand regardless of lactate concentration with many of between-device standard deviations estimated to be zero (to two decimal places) and few in excess of 0.1 mM, which is the precision to which lactate values are recorded (Table 5). The largest standard deviations were for the pair of Lactate Pro analysers for which the estimates ranged from 0.07 to 0.54 mM, increasing as the mean lactate increased. The corresponding CVs (based on the means of the Radiometer readings), decreased from 5.0% to 2.7%; where the mean for the five concentration bands for the Radiometer ABL90 were 1.28, 3.51, 7.89, 12.20 and 19.71 mM. Only one other CV exceeded 2%, namely 5.7% for i-STAT (in the 2-4.9 mM band), but this was based on just seven observations. With Device treated as a fixed effect, differences between the pair of Lactate Pro analysers were statistically significant for all five bands of lactate values (Table 5). Only three of the other 28 comparisons achieved statistical significance, one for each of the i-STAT, Pro2 and Xpress comparisons. It should be noted that the total numbers of observations available for the i-STAT and Radiometer comparisons were only 38 and 40, respectively, compared with 187 for Scout+ and in excess of 240 for the other brands (Table 2).
Table 5.
Estimates of between-device within-brand variation expressed as a) standard deviation and b) coefficient of variation (%) based on means of Radiometer ABL90.
| Analyser Brand |
Lactate concentration band (mM) | ||||||
|---|---|---|---|---|---|---|---|
| 0-1.9 | 2.0-4.9 | 5.0-9.9 | 10.0-14.9 | 15+ | All | ||
| Standard deviation (mM) | |||||||
| Edge | .00 | .00 | .01 | .06 | .00 | .03 | |
| i-STAT | .00 | .20 | .00 | .19* | .00 | .00 | |
| Lactate Pro | .07† | .14‡ | .30‡ | .37‡ | .54‡ | .32‡ | |
| Lactate Pro2 | .00 | .00 | .08† | .00 | .00 | .00 | |
| Radiometera | .05 | .14 | .15 | .00 | |||
| Scout+ | .01 | .05 | .02 | .00 | .00 | .00 | |
| Xpress | .00 | .00 | .00 | .13 | .27* | .11 | |
| Coefficient of variation (%) | |||||||
| Edge | .0 | .0 | .1 | .5 | .0 | .3 | |
| i-STAT | .0 | 5.7 | .0 | 1.5 | .0 | .0 | |
| Lactate Pro | 5.0 | 4.1 | 3.8 | 3.0 | 2.7 | 3.6 | |
| Lactate Pro2 | .0 | .0 | 1.0 | .0 | .0 | .0 | |
| Radiometera | 1.5 | 1.7 | .8 | .0 | |||
| Scout+ | .8 | 1.3 | .3 | .0 | .0 | .0 | |
| Xpress | .0 | .0 | .0 | 1.1 | 1.4 | 1.2 | |
*p < 0.05
† p < 0.01
‡ p < 0.001.
a Comparison between Radiometer 715 versus the criterion Radiometer ABL90.
Analytical variation
The analytical error, which is essentially the measurement error for a random sample at a random time after collection, ranged from ~0.2-0.4 mM for all brands, but was 0.5 mM for the Xpress (‘All’ column of Table 6). The corresponding CVs were ~2-4%, whereas the Xpress was ~6%. Within the lactate concentration bands, the residual error was ~0.1 mM for the lowest band for all brands, and increased to ~0.4 mM for the highest band for most brands, with the exception of the i-STAT (0.15 mM) and the Xpress (0.87 mM).
Table 6.
Estimates of within-band analytical error for each brand of analyser expressed as a) standard deviation and b) coefficient of variation (%) based on means of Radiometer ABL90.
| Analyser Brand |
Lactate concentration band (mM) | ||||||
|---|---|---|---|---|---|---|---|
| 0-1.9 | 2.0-4.9 | 5.0-9.9 | 10.0-14.9 | 15+ | All | ||
| Standard deviation (mM) | |||||||
| Edge | .13 | .14 | .22 | .47 | .51 | .35 | |
| i-STAT | .04 | .45 | .13 | .06 | .15 | .20 | |
| Lactate Pro | .10 | .12 | .21 | .30 | .38 | .29 | |
| Lactate Pro2 | .06 | .11 | .22 | .52 | .60 | .40 | |
| Radiometera | .09 | .18 | .47 | .31 | |||
| Scout+ | .09 | .09 | .15 | .35 | .44 | .31 | |
| Xpress | .10 | .13 | .34 | .29 | .87 | .53 | |
| Coefficient of variation (%) | |||||||
| Edge | 10.3 | 4.0 | 2.8 | 3.9 | 2.6 | 4.0 | |
| i-STAT | 3.7 | 11.7 | 1.6 | 0.4 | 0.8 | 2.5 | |
| Lactate Pro | 7.6 | 3.5 | 2.7 | 2.4 | 1.9 | 3.3 | |
| Lactate Pro2 | 5.1 | 3.0 | 2.7 | 4.3 | 3.0 | 4.4 | |
| Radiometera | 2.4 | 1.9 | 2.4 | 2.9 | |||
| Scout+ | 7.1 | 2.7 | 1.9 | 2.9 | 2.2 | 3.5 | |
| Xpress | 7.5 | 3.7 | 4.4 | 2.4 | 4.4 | 5.9 | |
a Comparison between Radiometer 715 versus the criterion Radiometer ABL90.
Practical implications
Using representative cycling data, small differences of -2 to +5 W between the criterion (Radiometer ABL90) and each analyser were apparent at LT1. But at LT2 most analysers showed zero difference in power except the Xpress meter, which read 23 W below the criterion and the i-STAT which read 4 W above the criterion (Figure 4, Table 7). Using representative rowing data, there were differences of +1 to +9 W at LT1 and differences of -5 to +18W at LT2 compared to values predicted by the criterion.
Figure 4.
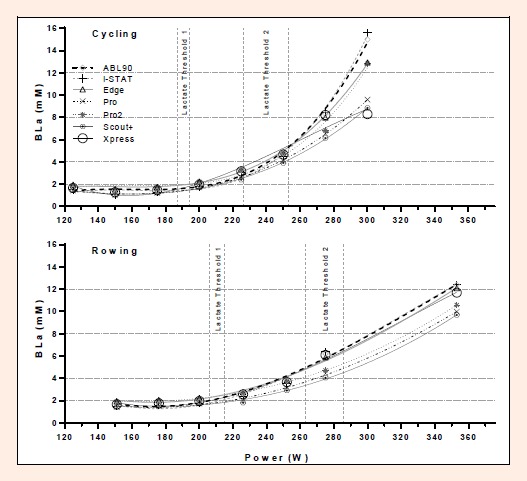
Comparison of blood lactate (BLa) versus intensity curves for representative cycling and rowing data sets computed using ADAPT software (Australian Institute of Sport, 1995). The reference curve (3rd order polynomial) was established using the BLa values from the Radiometer ABL90 with zero bias. The remaining curves were generated using mean bias of the respective analysers for each concentration band (Table 7).
Table 7.
Bias (calculated as the difference between the criterion ABL90 and each analyzer) for blood lactate concentration, and the effect of the bias on power at calculated Lactate Threshold One (LT1) and Two (LT2). Bias calculations used the average of Device A and B combined. Threshold calculations employed the ‘modified’ Dmax method in ADAPT software (Australian Institute of Sport, 1995) using representative cycling and rowing data from incremental step tests.
| Lactate concentration band (mM) | Analyser | ||||||
|---|---|---|---|---|---|---|---|
| ABL90 | Edge | i-STAT | Lactate Pro | Lactate Pro2 | Scout+ | Xpress | |
| Bias (mM) | |||||||
| 0-1.9 | 0.0 | 0.34 | -0.12 | -0.17 | 0.32 | -0.17 | 0.06 |
| 2.0-4.9 | 0.0 | 0.07 | -0.29 | -0.70 | -0.06 | -0.89 | -0.13 |
| 5.0-9.9 | 0.0 | -0.32 | 0.17 | -1.76 | -1.48 | -2.15 | -0.09 |
| 10.0-14.9 | 0.0 | -0.29 | 0.00 | -2.41 | -1.81 | -2.71 | -0.70 |
| 15.0+ | 0.0 | -2.05 | 0.62 | -5.40 | -2.16 | -6.15 | -6.70 |
| Threshold intensity | Cycling | ||||||
| LT1 Power (W) | 189 | 191 | 194 | 191 | 187 | 192 | 190 |
| LT2 Power (W) | 249 | 249 | 253 | 249 | 249 | 249 | 226 |
| Rowing | |||||||
| LT1 Power (W) | 206 | 209 | 209 | 211 | 207 | 215 | 209 |
| LT2 Power (W) | 268 | 277 | 263 | 281 | 281 | 286 | 263 |
Discussion
The results of the current study indicate that no single portable analyser is both highly accurate and reliable throughout the range of ~1-23 mM; although most pairs of analysers of the same brand were in close agreement with each other, which supports the practice of interchanging different analysers of the same brand between testing sessions. Two portable analysers, specifically the Edge and Xpress, have low ‘total error’ (as assessed by the √MSE) for BLa values in the range of ~1-15 mM, while the Edge and Lactate Pro2 have low √MSE for values in the range of ~15-23 mM. The i-STAT point-of-care hand-held analyser has very low √MSE throughout the measurement range of ~1-23 mM, but with relatively long analysis time. Ultimately, the ideal portable analyser will depend upon the end user requirements since, in a clinical setting, the ability to measure very high concentrations of BLa may not be as important as for those working with elite athletes.
Blood lactate stability over time
Previous research using resting blood samples has noted progressive increase in lactate over time for blood samples stored in vitro at room temperature (Calatayud and Tenias., 2003; Jones et al., 2007; Mikesh and Bruns., 2008; Seymour et al., 2011), with the magnitude of between ~0.012 to ~0.022 mM·min-1. The rate of accumulation is attenuated to ~0.42 mM·hour-1 (0.0007 mM·min-1) from blood samples obtained after exercise (Astles et al., 1994). In contrast, we showed a decay of lactate of ~0.05 mM·min-1 in the range of ~10-23 mM; and the corresponding change in resting lactate in the range of 0-1.9 mM was estimated as a mean of 0.00 mM·min-1 (range +0.017 to –0.019 mM·min-1). No other study we could locate conducted repeated measures on each blood sample to quantify the time course of BLa measurements, including those that measured resting lactate in the first 10 – 15 min after collection (Calatayud and Tenias., 2003; Jones et al., 2007; Mikesh and Bruns., 2008; Seymour et al., 2011). The only exception was McCaughan et al. (1999), who made duplicate measurements, but stored blood in tubes containing sodium fluoride, which inhibits glycolysis (Astles et al., 1994). Using six replicates we established that the within-sample standard deviation of resting blood lactate is ~0.1 mM, which implies that an increase (or decrease) of less than this magnitude is within the random variation and consequently will likely be obfuscated without a large number of observations. Our results challenge the veracity of other studies which have reported increases in BLa of ~0.1 mM in 10 minutes after blood collection using small sample sizes (Seymour et al., 2011). However, the evidence from blood storage studies conducted over days to weeks illustrate irrefutably the progressive increase in lactate (Bennett-Guerrero et al., 2007; D’Alessandro et al., 2013).
In the current study, the high concentrations of BLa were derived from exercise blood samples, and therefore are associated with lower blood pH, where acidity has been shown to attenuate red blood cell metabolic activity (Bennett-Guerrero et al., 2007). But this does not explain why we saw a clear decrease in BLa for these exercise blood samples, which was most apparent above 10 mM where analytical error is relatively low (Table 6). Based upon six replicates per sample we have good confidence in the current results and suggest that more research is needed to carefully quantify how BLa responds in heparinised tubes during the first 10-15 minutes after collection. Regardless of the increase or decay over time, our study was designed so that blood samples from the different analysers were time-matched allowing all devices to analyse an equivalent concentration at the same time.
Reliability and analytical variation
The within-sample standard deviations (reliability) of the five portable analysers were generally <0.5 mM for concentrations in the range of ~1.0-10 mM (Figure 1), with greater imprecision (~1 mM) for the highest concentrations; that is BLa >15 mM. Interestingly, the reliability of the portable analysers was not noticeably worse than for the two Radiometer laboratory analysers (Figure 1), where the Radiometer ABL90 has been used as the criterion analyser. The SD of the Radiometer ABL90 means that some of the bias discussed subsequently (and hence the √MSE) may be partially a consequence of imprecision of the reference analyser, which is to be anticipated since all measurement systems have some degree of error/uncertainty.
The reliability (a combination of both biological variation and analytical error) of BLa measures during submaximal exercise testing is reported as 52, 21 and 11% at mean BLa concentrations of ~2.0, 2.7 and 5.2 mM, respectively (Saunders et al., 2004). Saunders et al. (2004) completed these lactate measurements using a Radiometer ABL700 series analyser, and the corresponding CVs from our Radiometer in the current experiment were 2.2 and 2.1% at mean BLa concentration of 3.5 and 7.9 mM (Table 6). If we assume that the biological variation and analytical errors are independent (Gore et al., 2005), for our CV data we can deduce that the biological variation could be in the range of ~20.9-10.8% (i.e. √(212 – 2.22) or √(112 – 2.12)). Even at the lowest BLa concentrations using the highest CV (from the Edge, 10.3%) from the current study at a mean lactate of 1.28 mM, the biological variation could be ~51% (i.e. 522 – 10.32). Thus, we conclude that biological variation of BLa during exercise is the dominant source of variation compared with the analytical error of the portable blood lactate analysers.
Where comparisons were possible to previously published studies or to the manufacturer’s specifications, our results for analytical error within a brand (Table 6) were generally alike and very much smaller than the biological variation in BLa as described above. For the Lactate Pro, McNaughton et al. (2002) calculated CVs of 10.0, 4.1 and 3.1% at low (~1 mM), moderate (~4 mM) and high (~12 mM) BLa concentrations; the corresponding CVs in the current study were 7.6, 3.5 and 2.7%, respectively. Our overall measurement error of 3.3% for the Lactate Pro was also in agreement with the 3% CV reported by the manufacturer, Arkray (McNaughton et al., 2002). The manufacturers of the Edge and Scout+ report measurement errors of ≤5% and 3%, respectively (Artic Medical, 2011, SensLab GmbH, 2012), similar to our overall results of 4.0 and 3.5% (Table 6). For the i-STAT using quality control solutions instead of blood the manufacturer (Abbott Point of Care Inc, 2013) reports measurement errors (as SDs) of 0.03 and 0.08 mM at mean values 0.8 and 6.4 mM, respectively, which are consistent with our values of 0.04 and 0.13 mM at mean BLa concentrations of 1.3 and 7.9 mM. Our data for the Radiometer brand is a comparison between two different models, but nevertheless use identical technologies to measure BLa and each provide an index of the analytical error. The Radiometer reference manual for the 700 series analyser reports analytical SDs of 0.15 and 0.30 mM at concentrations of 2 and 10 mM, respectively; the closest corresponding SDs in the current study were 0.09 and 0.18 mM at mean concentrations of 3.5 and 7.9 mM. Likewise the Radiometer reference manual for the ABL90 reports that the analytical imprecision for a measurement of BLa on venous blood at a concentration 3.9 and 25 mM of 0.10 and 0.21 mM, respectively, whereas our equivalent SDs at 3.5 and 19.7 mM were 0.09 and 0.47 mM.
Accuracy/bias
There was a tendency for all portable analysers to under-read the same time-matched sample analysed by the Radiometer ABL90, which was particularly evident at the highest concentrations (BLa ~15-23 mM). However, both the Edge and the Lactate Pro2 had a small positive bias for resting concentrations (BLa ~1.0-2.0 mM). Biases could possibly be explained by differences in analysis methodology between lab-based and portable analysers, and further influenced by the proprietary manufacturer algorithms used to convert voltage to BLa for their respective amperometric methods. The small bias of the Xpress analyser at concentrations under 15 mM (Figure 1) suggests that this analyser would be well suited to a clinical setting, where for instance BLa ranges from 0-10 mM when sampling umbilical whole blood to determine foetal hypoxia (Kruger et al., 1999).
The possibility of adjusting for bias via the use of a simple linear regression model was examined for the Edge data and resulted in appreciable improvements in bias at both the lowest (1-2 mM) and highest (15-23 mM) BLa concentrations (Figure 3). This approach would require the user to have a short algorithm (or look-up table) to amend the BLa displayed on the Edge to a predicted value that would have been obtained using the Radiometer ABL90. In these days of ubiquitous technology (e.g. Apple - iPhone or Samsung - Galaxy), such an algorithm should be straightforward to implement in the field. It would be recommended that a laboratory generate their own linear prediction equations for their specific portable blood lactate analysers; they would require access to a criterion analyser (for instance a Radiometer) in order to do so.
The Radiometer ABL90 is a cassette-operated analyser for use in small labs and, although it employs the same analysis methodology as the ABL-700 and -800 series, it is less frequently used in research studies on athletes. A comparison between the two Radiometer analysers involving only six blood samples (each measured ~ 3-5 times) was performed as part of the current study and the mean bias was zero for the ABL715 versus the ABL90. These results suggest that blood lactate data from Radiometer ABL90 are comparable to that of Radiometer 715 and that these models of Radiometer analysers can be used interchangeably. This finding of nil bias between Radiometer analysers facilitates comparison of the current performance of Lactate Pro with previous research, which also shows a tendency of the Lactate Pro to under read the criterion laboratory Radiometer analyser (Pyne et al., 2000; Tanner et al., 2010).
An interesting observation of our data (Figure 3 – top two panels) is the clustering of repeated measurements of the same blood sample within an analyser (and consistent between the different brands of analysers – data not shown), which is particularly obvious at the higher concentrations of BLa, >10 mM. We are unable to explain this observation but speculate whether there is too much lactate for conversion by the lactate oxidase enzyme of the test strips. Indeed the largest negative bias is associated with the very highest blood lactate concentration (inverted triangles in Figure 3). However, counter to our conjecture, clustering of repeated measurements on the same blood sample is also evident at the lower blood lactate concentrations.
√Mean squared error
We have used root Mean Squared Error to combine both reliability and bias to assist with decision making about the ‘best’ portable analyser (Figure 2), which indicates that the answer depends upon the user requirements. It is clear that each portable BLa analyser had both strengths and weaknesses, and that in most cases bias was the major contributor to the MSE (the root MSE can be interpreted as the distance of points from the origin in Figure 1, provided the same scale is used on both axes).
It is well established that low total error (that is, good accuracy and reliability) of analysers is most important for BLa concentrations between 0 and 8 mM, for the derivation of lactate thresholds, identification of metabolic efficiency and buffering capacity, and the prescription of training intensity (Beneke et al., 2011; Bentley et al., 2007; Faude et al., 2009; Wasserman et al., 1973). In this context any of the examined analysers would be appropriate because of the relatively high biological variation compared with analytical variation. However, the maximal lactate that an athlete can produce is of much interest, consequent to the use of peak BLa achieved in an exercise step test for the calculation of Lactate Threshold 2 (LT2) via the Dmax method (Cheng et al., 1992). This requirement indicates that a preferred analyser should also be accurate and reliable at higher concentrations, for which both the Edge and Lactate Pro2 were the better of the portable analysers as reflected by their lower √MSE due, primarily, to lower bias. The i-STAT point-of-care analyser would also be superior to either the Edge or Lactate Pro2, but its purchase cost, analysis time and consumables costs are several times higher than these other analysers (Table 1).
Between-device within-brand variation
Estimates of the between-device within-brand standard deviations show that interchanging two units of the one brand is likely acceptable, with the exception of the Lactate Pro. However, given that only two devices of each brand were assessed, the between-devices variability is poorly estimated with estimates having only one degree of freedom. Six devices of the same brand would be needed to obtain a reasonable estimate of the between-devices variation. A priori, one would anticipate that the variation between two factory-manufactured devices should be small, but our results for the Lactate Pro suggest that a prudent scientist would use the exact same unit of any particular brand of analyser for all of their blood lactate measurements on an individual athlete, and/or conduct regular between devices comparisons to ensure correct calibrations.
Our estimate of the variation between one Radiometer ABL90 and one Radiometer ABL715 analyser also showed very close agreement (Table 5). Despite quite limited data this suggests that the previous results of Tanner et al. (2010) are comparable to the current results, which used the newer ABL90. But again, this statement is tenuous given that we only use a single analyser of each model.
In general terms, our results quantifying the imprecision between two Lactate Pro devices (Table 5) agree with previously published data. Tanner et al. (2010) reported an overall CV of 5.2% across the measurement range of 1.2-15.6 mM, and in the current study the corresponding CV was 3.6% (Table 5) for range 1.3-19.7 mM. Likewise, Pyne et al. (2000) reported a SD of 0.3 mM for the range of 1-18 mM and in the current study the SD was 0.32 mM.
Practical implications
For cycling, the ADAPT calculations of training zones were unaffected by the biases of the different brands of analysers except for the Xpress and i-STAT analysers (Table 7). For rowing, the negative bias for BLa >15 mM on most portable analysers influenced LT2 calculations (Figure 4), such that all analysers except the Xpress and i-STAT analysers over-estimated LT2 compared with the criterion by between 9 and 18 W. These biases would increase the calculated Training zones 4 and 5 (T4 - threshold, and T5 - maximal aerobic zones (Bourdon, 2013)) effectively overestimating the ability of the athlete and prescribing a training intensity that would be too high. The inverse would be true for the Xpress and i-STAT which both underestimated LT2 by 5 W for rowing. The difference in rowing compared with cycling data can be attributed to the elongated upper tail of lactate-power curve produced in response to a typically large increase in power during the final stages of an incremental rowing test. These results imply that when choosing a BLa analyser and comparing results across time, consideration must be given to the sport with which the device will be used as well as to the different methods implemented to determine lactate thresholds and training zones.
Limitations
This investigation was a laboratory-based comparison using cannula-derived venous blood samples performed under controlled environmental conditions. Use in the field, using finger prick/earlobe blood sampling may produce slightly different results.
Conclusion
Since biological variation of blood lactate concentrations swamps analytical variation, our results suggest that any of the evaluated analysers could be used over time to reliably derive BLa thresholds and prescribe training intensities within an individual, and that analysers from the same manufacturer can be used interchangeably to do so. With regards to accuracy, no single portable analyser was perfect; however the Edge and Xpress analysers each had low bias for BLa <15 mM, whereas the Edge and Lactate Pro2 had relatively low bias for high lactate concentrations which can be particularly influential for training zone prescription.
Acknowledgements
We gratefully acknowledge the assistance of the National Sport Science Quality Assurance Program.
Biographies

Jacinta BONAVENTURA
Employment
Accredited exercise physiologist
Degree
BExSS (Hons)
Research interests
Reliability and accuracy, neurological impairments in sport and exercise.
E-mail: jacinta.bonaventura@uqconnect.edu.au
Ken SHARPE
Employment
Consultant Statistician for the Statistical Consulting Centre, Department of Mathematics and Statistics at the University of Melbourne.
Degree
PhD
Research interests
Detection of elicit doping by athletes and other sports-related areas.
E-mail: k.sharpe@ms.unimelb.edu.au

Emma KNIGHT
Employment
Statistician, Performance Research, Australian Institute of Sport
Degree
PhD
Research interests
Applied statistics
E-mail: emma.knight@ausport.gov.au

Kate FULLER
Employment
Manager, National Sport Science Quality Assurance Program, Performance Science and Innovation, Australian Institute of Sport
Degree
BSc
Research interests
Validation of metabolic carts
E-mail: kate.fuller@ausport.gov.au

Rebecca TANNER
Employment
Technical Services Manager, Faculty of Health, University of Canberra
Degree
BAppSc (Hons)
Research interests
Quality assurance in sport science, equipment reliability and validity
E-mail: rebecca.tanner@canberra.edu.au

Christopher GORE
Employment
Head of Physiology, Australian Institute of Sport
Degree
PhD
Research interests
Minimising measurement error in laboratory settings
E-mail: chris.gore@ausport.gov.au
References
- Abbott Point of Care Inc. (2013) Lactate/Lac cartridge and test information sheet, item: 714184-00M Abbott Park, IL USA. [Google Scholar]
- Artic Medical. (2011) The edge – blood lactate monitoring system, Folkestone, Kent. Available from URL: http://www.arcticmedical.co.uk/UK/html/the_edge.html [Google Scholar]
- Astles R., Williams C., Sedor F. (1994) Stability of plasma lactate in vitro in the presence of antiglycolytic agents. Clinical Chemistry 40, 1327-1330. [PubMed] [Google Scholar]
- Australian Institute of Sport. (1995) ADAPT, version 6.7, computer software Physiology Department, Australian Institute of Sport, Belconnen ACT. [Google Scholar]
- Bates D., Maechler M., Bolker B., Walker S. (2014) lme4: Linear mixed-effects models using eigen and s4: R package, version 1.1-6, computer software. Available from URL http://CRAN.R-project.org/package=lme4 [Google Scholar]
- Beneke R., Leithauser R., Ochentel O. (2011) Blood lactate diagnostics in exercise testing and training. International Journal of Sports Physiology and Performance 6, 8-24. [DOI] [PubMed] [Google Scholar]
- Bennett-Guerrero E., Veldman T., Doctor A., Telen M., Ortel T., Reid T., Mulherin M., Zhu H., Buck R., Califf R., McMahon T. (2007) Evolution of adverse changes in stored RBCs. PNAS 104, 17063-17068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley D., Newell J., Bishop D. (2007) Incremental exercise test design and analysis: Implications for performance diagnostics in endurance athletes. Sports Medicine 37, 575-586. [DOI] [PubMed] [Google Scholar]
- Binder R., Wonisch M., Corra U., Cohen-Solal A., Vanhees L., Saner H., Schmid J. (2008) Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing. European Journal of Cardiovascular Prevention and Rehabilitation 15, 726-734. [DOI] [PubMed] [Google Scholar]
- Bourdon P. (2013) Blood lactate thresholds. Physiological tests for elite athletes. Tanner R., Gore C.2 nd edition. USA: Human Kinetics. [Google Scholar]
- Calatayud O., Tenias J. (2003) Effects of time, temperature and blood cell counts on levels of lactate in heparinized whole blood gas samples. Scandinavian Journal of Clinical & Laboratory Investigation 63, 311-314. [PubMed] [Google Scholar]
- Cheng B., Kuipers H., Snyder A., Keizer A., Jeukendrup A., Hesselink M. (1992) A new approach for the determination of ventilatory and lactate thresholds. International Journal for Sports Medicine 13, 518-522. [DOI] [PubMed] [Google Scholar]
- D’Alessandro A., Gevi F., Zolla L. (2013) Red blood cell metabolism under prolonged anaerobic storage. Molecular BioSystems 9, 1196-1209. [DOI] [PubMed] [Google Scholar]
- Faude O., Kindermann W., Meyer T. (2009) Lactate threshold concepts: How valid are they? Sports Medicine 39, 469-490. [DOI] [PubMed] [Google Scholar]
- Gore C., Hopkins W., Burge C. (2005) Errors of measurement for blood volume parameters: A meta-analysis. Journal of Applied Physiology 99, 1745-1758. [DOI] [PubMed] [Google Scholar]
- Jones A., Leonard M., Hernandex-Nino J., Kline J. (2007) Determination of the effect of in vitro time, temperature and tourniquet use on whole blood venous point-of-care lactate concentrations. Society for Academic Emergency Medicine 14, 587-591. [DOI] [PubMed] [Google Scholar]
- Kruger K., Hallberg B., Blennow M., Kublickas M., Westgren M. (1999) Predictive value of fetal scalp blood lactate concentration and pH as markers of neurologic disability. American Journal of Obstetrics and Gynecology 18, 1072-1078. [DOI] [PubMed] [Google Scholar]
- McCaughan H., McRae R., Smith H. (1999) The stability of lactate concentration in preserved blood microsamples. International Journal of Sports Medicine 21, 37-40. [DOI] [PubMed] [Google Scholar]
- McNaughton L., Thompson D., Phillips G., Backx K., Crickmore L. (2002) A comparison of the lactate pro, accusport, analox GM7 and kodak ektachem lactate analysers in normal, hot and humid conditions. International Journal of Sports Medicine 23, 130-135. [DOI] [PubMed] [Google Scholar]
- Mikesh L., Bruns D. (2008) Stabilization of glucose in blood specimens: Mechanism of delay in fluoride inhibition of glycolysis. Clinical Chemistry 54, 930-932. [DOI] [PubMed] [Google Scholar]
- Pyne P., Boston T., Martin D., Logan A. (2000) Evaluation of the lactate pro blood lactate analyser. European Journal of Applied Physiology 82, 112-116. [DOI] [PubMed] [Google Scholar]
- R Foundation for Statistical Computing (2014) R: A language and environment for statistical computing, computer software, Vienna, Austria. Available from http://www.R-project.org/ [Google Scholar]
- Saunders P., Pyne D., Telford D., Hawley J. (2004) Reliability and variability of running economy in elite distance runners. Medicine and Science in Sports and Exercise 36, 1972-1976. [DOI] [PubMed] [Google Scholar]
- SensLab GmbH. (2012) EKF Lactate Scout+ product specification sheet, Leipzig, Germany. [Google Scholar]
- Seymour C., Carlbom D., Cooke C., Watkins T., Bulger E., Rea T., Baird G. (2011) Temperature and time stability of whole blood lactate: Implications for feasibility of pre-hospital measurement. BMC Research Notes 4, 169-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner R., Fuller K., Ross M. (2010) Evaluation of three portable blood lactate analysers: Lactate Pro, Lactate Scout and Lactate Plus. European Journal of Applied Physiology 109, 551-559. [DOI] [PubMed] [Google Scholar]
- van Someren K., Howatson G., Nunan D., Thatcher R., Shave R. (2005) Comparison of the lactate pro and analox GM7 blood lactate analysers. International Journal of Sports Medicine 26, 657-661. [DOI] [PubMed] [Google Scholar]
- Wasserman K., Whipp B., Koyal S., Beaver W. (1973) Anaerobic threshold and respiratory gas exchange during exercises. Journal of Applied Physiology 35, 236-243. [DOI] [PubMed] [Google Scholar]


