Abstract
OBJECTIVES:
The goal of this study was to determine if Head Start participation is associated with healthy changes in BMI.
METHODS:
The sample included children participating in Head Start between 2005 and 2013 and children from 2 comparison groups drawn from a Michigan primary care health system: 5405 receiving Medicaid and 19 320 not receiving Medicaid. Change in BMI z score from the beginning to the end of each of 2 academic years and the intervening summer was compared between groups by using piecewise linear mixed models adjusted for age, gender, and race/ethnicity.
RESULTS:
The total sample included 43 748 children providing 83 239 anthropometric measures. The Head Start sample was 64.9% white, 10.8% black, and 14.4% Hispanic; 16.8% of the children were obese and 16.6% were overweight at the initial observation. Children who entered Head Start as obese exhibited a greater decline in the BMI z score during the first academic year versus the comparison groups (β = –0.70 [SE: 0.05] vs –0.07 [0.08] in the Medicaid group [P < .001] and –0.15 [SE: 0.05] in the Not Medicaid group [P < .001]); patterns were similar for overweight children. Head Start participants were less obese, less overweight, and less underweight at follow-up than children in the comparison groups.
CONCLUSIONS:
Preschool-aged children with an unhealthy weight status who participated in Head Start had a significantly healthier BMI by kindergarten entry age than comparison children in a primary care health system (both those receiving and those not receiving Medicaid).
Keywords: child, early childhood education, obesity
What’s Known on This Subject:
Head Start, a federally funded preschool program for low-income US children, has been reported to have beneficial effects on developmental outcomes. The association of Head Start participation with changes in children’s BMI has not been examined.
What This Study Adds:
Preschool-aged children with an unhealthy weight status who participated in Head Start had a significantly healthier BMI by kindergarten entry age than comparison children in a primary care health system (both those receiving and those not receiving Medicaid).
National data indicate that 22.8% of preschool-aged children are overweight or obese,1 with higher rates among lower socioeconomic groups.2 One in 4 US children aged <6 years lives in poverty (defined as <100% of the federal poverty line).3 Childhood overweight tracks into adulthood,4 and preventive interventions are needed.
Head Start is a federally funded preschool program that is free to 3- to 5-year-old US children living in poverty. The prevalence of obesity within Head Start programs is higher than national estimates.5–8 Head Start program regulations mandate nutritional and health services, adequate time and space for active play, and parental involvement.9 Given its expansive reach (42% of preschoolers in poverty10), Head Start could be an important setting for obesity intervention and prevention.
Although federal Head Start regulations mandate that programs monitor children’s height and weight,9 there is no centralized national data bank of these measures. One previous study has shown healthy changes in BMI during the academic year at Head Start, but the study sample was limited to a single Head Start program, and there was no comparison group.11 The present study analyzed changes in children’s BMI within 12 Head Start agencies in Michigan compared with BMI change in 2 age-matched samples drawn from a primary care health care system.
Methods
Participants
We invited all 51 Head Start programs in Michigan to participate, and 12 (23.5%) agreed. The participating agencies serve rural and urban communities. Head Start agencies have latitude in determining which risk factors give a child priority for enrollment, but the key federally defined eligibility criterion is a family income <100% of the federal poverty line.12 Head Start agencies provided anthropometric data collected between February 1, 2005, and August 1, 2013. For the 2 comparison groups, data were obtained from children who attended at least 1 primary care clinic visit within the University of Michigan Health System in the matched time interval and age range. These children were categorized into 2 groups: children insured by Medicaid and children not insured by Medicaid (“Not Medicaid”). No children were excluded a priori. The study was approved by the University of Michigan institutional review board.
Measures
Parent-reported demographic data (child birth date, gender, and race/ethnicity) were obtained from program/health records. Receipt of Medicaid was indicated in the electronic health record. Head Start agencies provided anthropometric data for 1 to 5 academic years. For the 2 health system comparison groups, weight and height measures were obtained from the electronic health record. BMI was calculated, and BMI percentiles and z scores were derived by using age- and gender-specific norms from the Centers for Disease Control and Prevention (CDC) growth charts. According to the CDC’s definitions, obese was defined as a BMI ≥95th percentile, overweight as a BMI ≥85th percentile but <95th percentile, healthy weight as a BMI ≥fifth percentile but <85th percentile, and underweight as a BMI <fifth percentile.
The study included all anthropometric measures obtained between ages 28.0 and 69.0 months taken within the first and second academic years and the summer between those 2 years (with a 0.5-month buffer on either side). From a total of 89 482 data points for 45 385 children, we excluded 0.03% with missing gender, 0.06% with missing weight, and 0.14% with missing height. The CDC cutoffs13 for extreme weight-for-age (WAz), height-for-age (HAz), weight-for-height, and BMI-for-age (BMIz) z scores were applied to remove biologically implausible values, resulting in the exclusion of an additional 2.01% of values. Longitudinal cleaning criteria were also applied. Because there are currently no standard longitudinal cleaning criteria for children’s anthropometric data, we examined the distributions of change in these measures over time within this sample and considered those changes that were >2 SDs from the sample distribution to be outliers. In this sample, values meeting the following criteria were therefore excluded: change in WAz, HAz, or BMIz of >1.5 SD units (based on CDC charts) per month; change in weight of >2.5 kg per month; loss in height of >5 cm over any time period or gain in height of >5 cm per month; or change in BMI of >2.5 kg/m2 per month, which resulted in the exclusion of an additional 4.00% of values. The mean number of BMI measures per child was 1.90 (SD: 1.12; range: 1–9). As a data quality assessment, we checked the assumption of constant variance in WAz, HAz, and BMIz overall and according to measurement site (ie, Head Start, health system); all SD units were between 0.97 and 1.19, which are within acceptable limits.14,15 In summary, the Head Start programs provided BMI data for 20 416 children, of whom 6.82% were excluded, resulting in a final sample size of 19 023 children in Head Start. The health system provided BMI data for 24 969 children, of whom 0.98% were excluded, resulting in a final sample size of 24 725 children. The sample of children included in the analysis versus the sample excluded due to implausible values was more likely to be female (P < .05) and white (P < .0001) but did not differ with regard to age.
Statistical Analysis
Piecewise linear mixed models were used to compare changes in BMIz during the time frame when the child was participating in Head Start (September 1–May 15) versus the time frame when the child was not participating in Head Start (May 16–August 31). Thus, we allowed for 3 potential different slopes corresponding to each of the 3 treatment periods: (1) the first academic year (September 1–May 15); (2) the summer break (not enrolled in Head Start; May 16–August 31); and (3) the second Head Start academic year (September 1–May 15). Repeated measures analysis was performed by using mixed models with random intercepts and slopes to account for clustering of children nested in the same centers. In addition, a repeated statement was used specifying a Gaussian serial correlation structure between repeated BMIz measures for the same child over the study period. The Bayesian information criterion was used to obtain the optimal correlation structure for the random effects. The study included a priori covariates known to have an association with weight status, including child gender (male versus female), child age at enrollment, and child race/ethnicity (non-Hispanic white versus not). Similar models were fitted for each of the 2 comparison groups (Medicaid and Not Medicaid). In addition, we tested for group differences between slopes in each observation period, differences between intercepts measured at the beginning and end of the observation period, and change in BMIz from the beginning to the end of the observation period. All analyses were stratified according to initial weight status categorized as obese, overweight, healthy weight, and underweight.
Results
Characteristics of the sample are shown in Table 1. The total sample included 43 748 children providing 83 239 anthropometric measures. The Head Start sample was 64.9% white, 10.8% black, and 14.4% Hispanic; 16.8% of the children were obese and 16.6% were overweight at the initial observation. The primary care health system Medicaid sample was 50.8% white, 33.0% black, and 4.8% Hispanic; 12.3% of the children were obese and 14.9% were overweight at the initial observation. The primary care health system Not Medicaid sample was 71.3% white, 8.2% black, and 2.2% Hispanic; 6.8% of the children were obese and 11.9% were overweight at the initial observation.
TABLE 1.
Characteristics of the Samples
| Characteristic | Head Start | Health Care System | Total | |
|---|---|---|---|---|
| Medicaid | Not Medicaid | |||
| No. of children | 19 023 (43.5) | 5405 (12.4) | 19 320 (44.2) | 43 748 |
| No. of BMI observations | 47 811 (57.4) | 8021 (9.6) | 27 407 (32.9) | 83 239 |
| Age at enrollment, y | 3.75 ± 0.55 | 3.23 ± 0.86 | 3.31 ± 0.88 | 3.49 ± 0.79 |
| Child gendera | ||||
| Male | 9569 (50.3) | 2790 (51.6) | 9946 (51.5) | 22 305 (51.0) |
| Female | 9454 (49.7) | 2615 (48.4) | 9374 (48.5) | 21 443 (49.0) |
| Race/ethnicitya | ||||
| White, non-Hispanic | 12 354 (64.9) | 2744 (50.8) | 13 780 (71.3) | 28 878 (66.0) |
| Black, non-Hispanic | 2054 (10.8) | 1781 (33.0) | 1578 (8.2) | 5413 (12.4) |
| Other, non-Hispanic | 1885 (9.9) | 621 (11.5) | 3527 (18.3) | 6033 (13.8) |
| Hispanic, any race | 2730 (14.4) | 259 (4.8) | 435 (2.2) | 3424 (7.8) |
| Weight status at beginning of observation perioda | ||||
| Obese | 3189 (16.8) | 663 (12.3) | 1314 (6.8) | 5166 (11.8) |
| Overweight | 3168 (16.6) | 804 (14.9) | 2305 (11.9) | 6277 (14.4) |
| Healthy | 11 864 (62.4) | 3654 (67.6) | 14 593 (75.5) | 30 111 (68.8) |
| Underweight | 802 (4.2) | 284 (5.2) | 1108 (5.7) | 2194 (5.0) |
| BMIz at beginning of observation period | 0.54 ± 1.21 | 0.37 ± 1.17 | 0.14 ± 1.08 | 0.34 ± 1.16 |
Data are presented as n (%) or mean ± SD.
Number (%) of participants.
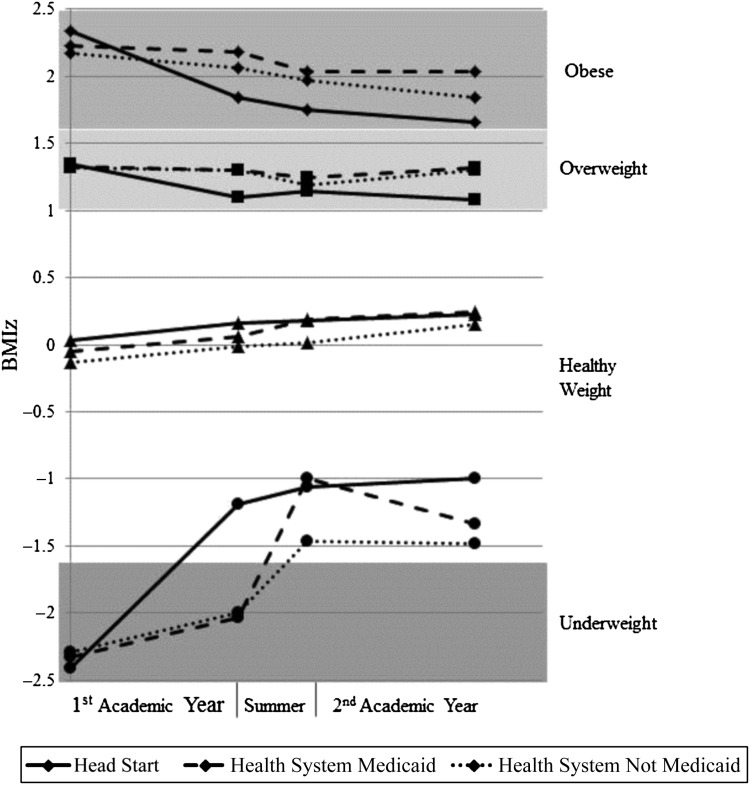
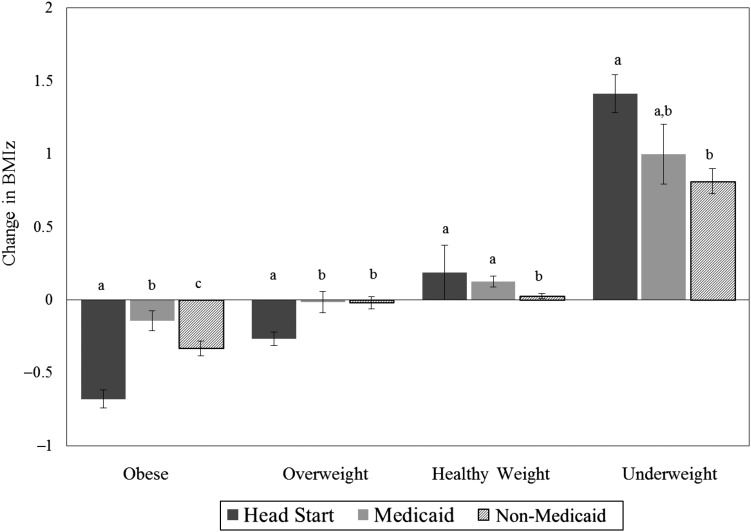
Results of the regression analyses are shown in Table 2 and Fig 1. Figure 2 shows the change in BMIz from the beginning to the end of the observation period according to weight status at the beginning of the observation period and according to group. Children who entered Head Start obese exhibited a statistically significant decline in BMIz over the first academic year (β = –0.70 [SE: 0.04]), which was greater than that of children in the Medicaid group (β = –0.07 [SE: 0.08]) and the Not Medicaid group (β = –0.15 [SE: 0.05]). Children who entered Head Start obese also exhibited a significant decline in BMIz over the subsequent summer (β = –0.31 [SE: 0.10]), although this finding was not statistically significantly greater than the declines in the comparison groups (β = –0.49 [SE: 0.23] in the Medicaid group and β = –0.33 [SE: 0.17] in the Not Medicaid group). There were no significant changes in BMIz during the second academic year among children who began the observation period obese in any group. By the end of the observation period, children who had entered Head Start obese had significantly lower mean ± SE BMIz (1.66 ± 0.06) than children in either comparison group (2.04 ± 0.08 in the Medicaid group and 1.84 ± 0.05 in the Not Medicaid group).
TABLE 2.
Means and SEs for BMIz Among Children in the Head Start and Comparison Groups, Stratified According to Weight Status at the Start of the Observation Period
| Initial Weight Status | Starting BMIz | Rate of Change in BMIz (per year) | Ending BMIz | ||
|---|---|---|---|---|---|
| 1st Academic Year | Summer | 2nd Academic Year | |||
| Obese | |||||
| Head Start | 2.34a (0.02)*** | −0.70a,e (0.04)*** | −0.31a,f (0.10)** | −0.13a,f (0.07) | 1.66a (0.06)*** |
| Medicaid | 2.23b (0.03)*** | −0.07b,e (0.08) | −0.49a,e (0.23)* | 0.00a,e (0.15) | 2.04b (0.08)*** |
| Not Medicaid | 2.17b (0.02)*** | −0.15b,e (0.05)** | −0.33a,e (0.17) | −0.18a,e (0.10) | 1.84c (0.05)*** |
| Overweight | |||||
| Head Start | 1.35a (0.01)*** | −0.36a,e (0.03)*** | 0.17a,f (0.08)* | −0.09a,g (0.05) | 1.08a (0.04)*** |
| Medicaid | 1.33a (0.01)*** | −0.04b,e (0.04) | −0.20b,e (0.14) | 0.10a,b,e (0.12) | 1.31b (0.07)*** |
| Not Medicaid | 1.32a (0.01)*** | −0.03b,e (0.02) | −0.36b,f (0.09)*** | 0.15b,g (0.07)* | 1.30b (0.04)*** |
| Healthy weight | |||||
| Head Start | 0.03a (0.01)** | 0.18a,e (0.02)*** | 0.08a,f (0.05) | 0.06a,f (0.03) | 0.22a (0.03)*** |
| Medicaid | −0.05b (0.02)* | 0.16a,e,f (0.04)*** | 0.43b,e (0.12)*** | 0.08a,b,f (0.07) | 0.25a (0.03)*** |
| Not Medicaid | −0.13c (0.01)*** | 0.17a,e (0.02)*** | 0.09a,e (0.06) | 0.19b,e (0.03)*** | 0.15b (0.01)*** |
| Underweight | |||||
| Head Start | −2.41a (0.05)*** | 1.72a,e (0.11) *** | 0.44a,f (0.31) | 0.10a,f (0.19) | −1.00a (0.12)*** |
| Medicaid | −2.33b (0.08)*** | 0.42b,e (0.19)* | 3.54b,f (0.53)*** | −0.47a,g (0.35) | −1.32a,b (0.19)*** |
| Not Medicaid | −2.29b (0.04)*** | 0.42b,e (0.09)*** | 1.80c,f (0.25)*** | −0.02a,g (0.15) | −1.48b (0.08)*** |
All analyses adjusted for age at start of observation period, child gender, and child race/ethnicity. Superscripts a, b, and c that differ from one another denote significant differences between Head Start, Medicaid, and Not Medicaid within each weight status group within the given observation period. Superscripts e, f, and g that differ from one another denote significant differences across observation periods within the given group (Head Start, Medicaid, and Not Medicaid) within the given weight status group. *** P < .001, ** P < .01, * P < .05.
FIGURE 1.
Change in BMIz across time among children in Head Start and comparison groups, stratified according to initial weight status. Adjusted for age, gender, and race/ethnicity.
FIGURE 2.
Change in BMIz from the beginning to the end of the observation period according to initial weight status and group. The letters above each bar that differ indicate statistically significant differences between groups within the given weight status.
Children who entered Head Start overweight showed a significant decline in BMIz over the first academic year (β = –0.36 [SE: 0.03]), which was greater than that of children in the Medicaid group (β = –0.04 [SE: 0.04]) and the Not Medicaid group (β = –0.03 [SE: 0.02]), neither of which showed a significant change. Children who entered Head Start overweight experienced a significant upward rebound of BMIz over the summer (β = 0.17 [SE: 0.08]), which was significantly greater than changes in the comparison groups (β = –0.20 [SE: 0.14]) in the Medicaid group and β = –0.36 [SE: 0.09]) in the Not Medicaid group). There was no significant change in BMIz during the second academic year among children who began the observation period overweight in the Head Start or Medicaid groups, but there was a significant increase in BMIz in the Not Medicaid group, which differed from the Head Start group. By the end of the observation period, children who had entered Head Start overweight had a significantly lower mean BMIz (1.08 [SE: 0.04]) than children in either comparison group (1.31 [SE: 0.07] in the Medicaid group and 1.30 [SE: 0.04] in the Not Medicaid group).
Children who entered Head Start at a healthy weight exhibited a significant increase in BMIz over the first academic year (β = 0.18 [SE: 0.02]), which did not differ from the significant increases in the comparison groups. During the subsequent summer, children who entered Head Start at a healthy weight showed no significant change in BMIz, which was similar to the Not Medicaid group but differed from the Medicaid group, which experienced a significant increase in BMIz during the summer. There was no significant change in BMIz during the second academic year among children who began the observation period at a healthy weight in the Head Start or Medicaid groups, but there was a significant increase in BMIz in the Not Medicaid group, which differed from the Head Start group. By the end of the observation period, children who had entered Head Start at a healthy weight had a mean BMIz (0.22 [SE: 0.03]) that was similar to that of children in the Medicaid group (0.25 [SE: 0.03]) but greater than that of children in the Not Medicaid group (0.15 [SE: 0.01]).
Children who entered Head Start underweight exhibited a significant increase in BMIz during the first academic year (β = 1.72 [SE: 0.11]) that was greater than the significant increases in both comparison groups (β = 0.42 [SE: 0.19]) in the Medicaid group and β = 0.42 [SE: 0.09]) in the Not Medicaid group). Children who began the observation period underweight and participated in Head Start showed no change over the summer, whereas children in both comparison groups exhibited significant increases. During the second academic year, there was no significant change in any of the 3 groups. By the end of the observation period, children who had entered Head Start underweight had a mean BMIz (–1.00 [SE: 0.12]) that was no different from that of children in the Medicaid group (–1.32 [SE: 0.19]) and greater than that of children in the Not Medicaid group (–1.48 [SE: 0.08]).
To examine the potential effects of differential attrition across groups, we repeated the analyses, restricting the sample to only those participants with at least 2 BMI measures >100 days apart. The proportions of children meeting these criteria were 67.1%, 41.7%, and 40.1% in the Head Start, Medicaid, and Not Medicaid groups, respectively. The results for the children who were initially obese, overweight, or a healthy weight were essentially unchanged in the analysis of the restricted sample. However, the models for initially underweight children in the Head Start group did not converge.
Discussion
Children who entered Head Start obese or overweight experienced a greater decline in BMIz over an academic year compared with each of the 2 comparison groups. In addition, children who entered Head Start underweight experienced a greater increase in BMIz compared with each of the 2 comparison groups. Children entering Head Start obese, overweight, or underweight all showed either maintenance of or ongoing improvement in the BMIz changes made during the first academic year of enrollment. During the second academic year of enrollment, changes were maintained, but there were no additional significant changes in BMIz in the Head Start group. Even though children in the Head Start group began the observation period more obese, equally overweight, and more underweight than children in the comparison groups, at the end of the observation period the initially obese and overweight Head Start children were substantially less obese and overweight than the children in the comparison groups. In addition, the initially underweight children were substantially less underweight than children in the Not Medicaid group. To our knowledge, this study is the first to document associations of Head Start participation with changes in children’s BMIz in a sample including more than a single Head Start program, while also including multiple comparison groups.
Head Start may exert beneficial effects on BMI through several mechanisms. The federally regulated quality of meals and snacks provided at Head Start9 may be higher than that in many eligible children’s homes or in other child care facilities that do not have to meet federal meal standards. Head Start nutrition guidelines are consistent with the recommendations of the Academy of Nutrition and Dietetics.16 Head Start programs are also required to adhere to the federal Child and Adult Care Food Program guidelines,17 which mandate a certain amount of fruits and vegetables at each meal and restrict sugar-sweetened beverages, each of which are recommended strategies for obesity prevention and treatment.18–21 Head Start programs self-report exceeding both federal performance standards and Child and Adult Care Food Program guidelines (eg, of 1583 programs, 97% serve a vegetable every day other than French fries, tater tots, or hash browns and 94% serve some fruit every day other than juice).22 Head Start regulations emphasize exercise and the development of gross motor skills,9 and children’s preschool environments strongly predict physical activity levels more than demographic characteristics.23 Head Start regulations also prohibit television viewing,9 a risk factor for preschool overweight,24 and require that programs facilitate children’s access to a continuous source of pediatric health care, which may contribute to a reduction in obesity risk. Head Start participation is associated with improvement in children’s ability to cope with stress and reductions in behavior problems,25 and psychosocial stress and poor behavioral self-regulation are each associated with obesity risk.26,27 Finally, by providing free child care, Head Start may allow families to allocate their limited financial resources to purchasing healthier food.
There are several limitations to our study. The ideal design would be a randomized controlled trial in which low-income children were randomized to participate in Head Start versus not participate., but given the currently accepted benefits of early childhood education, such a design would not be ethical or feasible. Our analysis was limited to data from a single state, and it is unknown whether the results would be generalizable to children from other states. Only a subset (23.5%) of Head Start programs in Michigan agreed to participate, and this subset may have had a greater focus on nutrition, physical activity, and obesity than the subset that declined participation. We did not have children’s attendance data, although all children in the analytic sample attended at least 85% of program days. The comparison groups were drawn from a single health system in southeastern Michigan, and some children in the health care system enrolled in Medicaid may also have been participating in Head Start. However, the fact that some children in the comparison group enrolled in Medicaid may also have been participating in Head Start provides a stronger test because it would be expected to weaken any observed differences between groups. Finally, anthropometric measurements were performed by Head Start or clinical practitioners, but we found that the percent excluded was small, and the quality of data comparable with similar studies.14,15
The results of the present study should be interpreted with several caveats. First, although differential attrition did not alter the findings among children who were initially obese, overweight, or a healthy weight, differential attrition led to instability of the models for initially underweight children in the Head Start group. Therefore, conclusions regarding associations of Head Start participation with improvements in BMI among underweight children should be made with caution. Second, this study did not compare impoverished children participating in Head Start with impoverished children not participating in Head Start. Rather, the study compared children participating in Head Start (the majority of whom are impoverished) with a group of impoverished children whose child care, preschool, or Head Start participation is unknown. Third, children in the comparison groups drawn from the health care system are a select group; that is, children not regularly accessing the health care system are not included. Furthermore, children in the health care system groups, compared with the Head Start group, were less likely to have 2 BMI measures at least 100 days apart, suggesting that the comparison groups may not be frequent health care users.
Conclusions
Head Start participation was associated with robust, early, and sustained beneficial effects on children’s BMI such that by the age of entry to kindergarten, children participating in Head Start had significantly healthier BMIs than children enrolled in Medicaid in general and children not enrolled in Medicaid. Head Start is associated with improved social and educational outcomes for low-income children.28 Healthy changes in BMI may be an additional benefit of Head Start participation.
Acknowledgments
The authors thank the Head Start agencies who participated in the study: Adrian Public Schools Head Start Early Childhood Programs; Blue Water Community Action; Branch Intermediate School District Head Start, Coldwater Michigan; Chippewa-Luce-Mackinac Community Action Agency, Head Start Program; Community Action Agency’s Children’s Programs in Jackson and Hillsdale; EightCAP, Inc 0-5 Head Start; FiveCAP Head Start Program; Livingston Educational Service Agency Early Childhood Programs; Matrix Vistas Nuevas Head Start; Michigan Family Resources, Head Start for Kent County; Northeast Michigan Community Service Agency, Head Start Program; and MCY, Inc./Renaissance Head Start Program.
Footnotes
Dr Lumeng conceptualized and designed the study and drafted the initial manuscript; Dr Kaciroti conceptualized and designed the study, conducted the analyses, and reviewed and revised the manuscript; Ms Sturza conducted the analyses and reviewed and revised the manuscript; Ms Krusky coordinated and supervised data collection and critically reviewed the manuscript; Drs Miller, Peterson, Lipton, and Reischl conceptualized and designed the study and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Health grant 5R21DK095695. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitaker RC, Orzol SM. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med. 2006;160(6):578–584 [DOI] [PubMed] [Google Scholar]
- 3.National Center for Children in Poverty. United States early childhood profile. Available at: www.nccp.org/profiles/pdf/profile_early_childhood_US.pdf. Accessed October 21, 2014
- 4.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488 [DOI] [PubMed] [Google Scholar]
- 5.Wiecha JL, Casey VA. High prevalence of overweight and short stature among Head Start children in Massachusetts. Public Health Rep. 1994;109(6):767–773 [PMC free article] [PubMed] [Google Scholar]
- 6.Hernandez B, Uphold CR, Graham MV, Singer L. Prevalence and correlates of obesity in preschool children. J Pediatr Nurs. 1998;13(2):68–76 [DOI] [PubMed] [Google Scholar]
- 7.Hu WT, Foley TA, Wilcox RA, Kozera RM, Morgenstern BZ, Juhn YJ. Childhood obesity among Head Start enrollees in southeastern Minnesota: prevalence and risk factors. Ethn Dis. 2007;17(1):23–28 [PubMed] [Google Scholar]
- 8.Feese M, Franklin F, Murdock M, et al. Prevalence of obesity in children in Alabama and Texas participating in social programs. JAMA. 2003;289(14):1780–1781 [DOI] [PubMed] [Google Scholar]
- 9.Office of Head Start. 45 CFR 1304 program performance standards for the operation of Head Start programs by grantees and delegate agencies. Available at: http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/ehsnrc/Early%20Head%20Start/supervision/management/fiscal_pps_00244_093005.html. Accessed October 31, 2014
- 10.Schmit S, Matthews H, Smith S, Robbins T. Investing in young children: a fact sheet on early care and education participation, access, and quality. Available at: www.nccp.org/publications/pdf/text_1085.pdf. Accessed October 31, 2014
- 11.Lumeng JC, Kaciroti N, Frisvold DE. Changes in body mass index z score over the course of the academic year among children attending Head Start. Acad Pediatr. 2010;10(3):179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Improving Head Start for School Readiness Act. In: 9801. Statute 1363, Public Law 110-134, Section 645; US; enacted December 12, 2007. Available at: https://eclkc.ohs.acf.hhs.gov/hslc/standards/law/HS_ACT_PL_110-134.pdf. Accessed October 31, 2014
- 13.US Centers for Disease Control and Prevention. A SAS program for the 2000 CDC growth charts (ages 0 to <20 y). Available at: www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed May 2, 2014
- 14.Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the Centers for Disease Control and Prevention pediatric nutrition surveillance, 1983 to 1995. Pediatrics. 1998;101(1). Available at: www.pediatrics.org/cgi/content/full/101/1/E12 [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Peterson KE, Scanlon KS, et al. Trends in overweight from 1980 through 2001 among preschool-aged children enrolled in a health maintenance organization. Obesity (Silver Spring). 2006;14(7):1107–1112 [DOI] [PubMed] [Google Scholar]
- 16.Benjamin Neelon SE, Briley ME, American Dietetic Association . Position of the American Dietetic Association: benchmarks for nutrition in child care. J Am Diet Assoc. 2011;111(4):607–615 [DOI] [PubMed] [Google Scholar]
- 17.Child and Adult Care Food Program Guidelines. Public Law 105-336, 112 statute 3143, enacted October 31, 1998; Part 226. Available at: www.fns.usda.gov/sites/default/files/CFR226.pdf. Accessed October 31, 2014
- 18.American Dietetic Association. Pediatric weight management: evidence-based nutrition practice guideline. Available at: www.adaevidencelibrary.com. Accessed October 31, 2014
- 19.Barlow SE, Expert Committee . Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192 [DOI] [PubMed] [Google Scholar]
- 20.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328(7450):1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357(9255):505–508 [DOI] [PubMed] [Google Scholar]
- 22.Whitaker RC, Gooze RA, Hughes CC, Finkelstein DM. A national survey of obesity prevention practices in Head Start. Arch Pediatr Adolesc Med. 2009;163(12):1144–1150 [DOI] [PubMed] [Google Scholar]
- 23.Pate RR, Pfeiffer KA, Trost SG, Ziegler P, Dowda M. Physical activity among children attending preschools. Pediatrics. 2004;114(5):1258–1263 [DOI] [PubMed] [Google Scholar]
- 24.Lumeng JC, Rahnama S, Appugliese D, Kaciroti N, Bradley RH. Television exposure and overweight risk in preschoolers. Arch Pediatr Adolesc Med. 2006;160(4):417–422 [DOI] [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services Administration for Children and Families. Head Start impact study: first year findings. Available at: www.acf.hhs.gov/sites/default/files/opre/first_yr_finds.pdf. Accessed October 21, 2014
- 26.Lumeng JC, Wendorf K, Pesch MH, Appugliese DP, Kaciroti N, Corwyn RF, et al. Overweight adolescents and life events in childhood. Pediatrics 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1506 [DOI] [PMC free article] [PubMed]
- 27.Seeyave DM, Coleman S, Appugliese D, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med. 2009;163(4):303–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Commissioner's Office of Research and Evaluation and the Head Start Bureau Administration on Children, Youth, and Families, US Department of Health and Human Services. Head Start FACES: longitudinal findings on program performance. Available at: www.acf.hhs.gov/sites/default/files/opre/perform_3rd_rpt.pdf. Accessed October 21, 2014