Abstract
OBJECTIVE:
To develop guidelines for performing an initial skeletal survey (SS) for children <24 months of age presenting with bruising in the hospital setting, combining available evidence with expert opinion.
METHODS:
Applying the Rand/UCLA Appropriateness Method, a multispecialty panel of 10 experts relied on evidence from the literature and their own clinical expertise in rating the appropriateness of performing SS for 198 clinical scenarios characterizing children <24 months old with bruising. After a moderated discussion of initial ratings, the scenarios were revised. Panelists re-rated SS appropriateness for 219 revised scenarios. For the 136 clinical scenarios in which SS was deemed appropriate, the panel finally assessed the necessity of SS.
RESULTS:
Panelists agreed that SS is “appropriate” for 62% (136/219) of scenarios, and “inappropriate” for children ≥12 months old with nonpatterned bruising on bony prominences. Panelists agreed that SS is “necessary” for 95% (129/136) of the appropriate scenarios. SS was deemed necessary for infants <6 months old regardless of bruise location, with rare exceptions, but the necessity of SS in older children depends on bruise location. According to the panelists, bruising on the cheek, eye area, ear, neck, upper arm, upper leg, hand, foot, torso, buttock, or genital area necessitates SS in children <12 months.
CONCLUSIONS:
The appropriateness and necessity of SS in children presenting for care to the hospital setting with bruising, as determined by a diverse panel of experts, depends on age of the child and location of bruising.
Keywords: bruise, child abuse, child maltreatment, skeletal survey, trauma
What’s Known on This Subject:
Bruising is common in young victims of physical abuse as well as in cases of accidental trauma. There is uncertainty regarding which young children with bruising require evaluation with skeletal survey for possible abuse.
What This Study Adds:
The results of this study provide guidelines, based on the literature and knowledge of experts, for identifying children <24 months presenting for care in the hospital setting with bruises, who should and should not undergo skeletal survey.
Bruising is the most common injury experienced by young victims of physical abuse.1 Although abusive bruising usually does not require medical intervention, bruising may be the only visible sign of serious injuries, such as fractures or traumatic brain injury.2,3 Abusive bruising also is a frequent precursor to more severe forms of physical abuse, including fatal head trauma.4–6 Accurate recognition and evaluation of abusive bruising can lead to identification of additional injuries requiring treatment and allow for intervention and prevention of further injury.3,4,6,7 Performing an evaluation for suspected physical abuse is, however, not without risks and should not be performed if abuse is unlikely.
Evaluation for suspected physical abuse in injured children <2 years old requires performance of a skeletal survey (SS), a series of ∼20 radiographs, to diagnose occult fractures.8,9 Although SSs expose children to radiation and contribute to costs, identification of occult fractures can prompt changes to medical treatment and inform the decision to diagnose abuse.9,10 In 1 study, nearly 10.8% (76 of 703) of initial SSs performed due to concerns for possible abuse revealed occult fractures.10 In one-half of cases with occult fractures, results from SS influenced clinicians’ decisions to diagnose abuse. A similar study reported that SSs revealed additional fractures in 13% (124 of 930) of children <2 years old evaluated for suspected abuse.11 Even higher incidences (25%–30%) of occult fractures have been reported in studies of children <2 years old diagnosed with physical abuse.12,13 Given the substantial likelihood of occult fractures in young victims of physical abuse, the American Academy of Pediatrics recommends performing SS in all cases of suspected physical abuse in children <2 years old, but not in cases in which abuse and occult fractures are unlikely.8
Identifying which children with bruising warrant an evaluation for abuse and SS can be challenging, especially in mobile older infants and toddlers who frequently experience accidental bruising.14,15 Several studies have identified characteristics of bruises associated with abusive versus accidental injury, but clear guidelines for clinicians regarding when to perform an initial SS for abuse in young children with bruising have not been developed.1,16
Accordingly, the goal of this study was to develop guidelines for performing initial SS in children <2 years old presenting with bruising. This set of guidelines focuses on children presenting for care in a hospital-based setting, primarily the emergency department or the inpatient unit, and may not be applicable to children presenting in the primary care setting.
Methods
We applied the Rand/UCLA Appropriateness Method to identify clinical scenarios in which initial SS is appropriate and scenarios in which initial SS is necessary as well as appropriate. Details on the application of the Rand methodology to identify scenarios in which SSs are inappropriate, appropriate, or necessary for children <2 years was previously described by Wood and colleagues.17 The Rand methodology, a modified Delphi process, informs clinical decision-making by combining expert opinion with evidence from the literature to qualify the benefit-harm ratio of tests and screening procedures for varying clinical scenarios. Unlike similar consensus methods, Rand methodology provides the experts with an opportunity to discuss their judgments, and has been shown to have high content, construct, and predictive validities for developing appropriateness criteria.18–21 A procedure is appropriate for a clinical scenario if the expected health benefit exceeds the expected negative consequences “by a sufficiently wide margin to make it worth doing, exclusive of cost.”21 A procedure deemed appropriate can also be considered necessary if it meets these additional criteria: (1) not offering the procedure would be improper, (2) there is a reasonable chance that the procedure will benefit the patient, and (3) the magnitude of the benefit is not small.21
Per Rand protocol, we (1) compiled literature reviews on bruising, SSs, and suspected abuse; (2) generated a set of clinical scenarios characterizing children with bruising for whom SS might be considered; and (3) convened a panel of medical experts (Fig 1).17 The subsequent sequential phases of scenario rating are as follows: (1) panelists rated the appropriateness of SS for each clinical scenario (Round 1); (2) panelists reviewed the Round 1 ratings and made revisions to scenarios during a moderated discussion; (3) panelists re-rated the appropriateness of SS for the revised scenarios (Round 2); (4) we categorized SS as appropriate, uncertain, or inappropriate for respective scenarios based on Round 2 ratings; (5) panelists rated the necessity of SS in scenarios for which SS was categorized as appropriate (Round 3); and (6) we categorized scenarios for which SS was deemed appropriate as necessary or unnecessary for SS based on Round 3 ratings.
FIGURE 1.
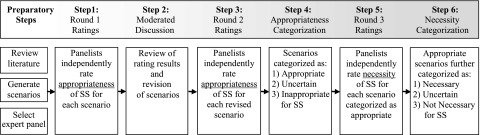
Procedure of the Rand/University of California Los Angeles appropriateness method for assessing appropriateness and necessity of SS. Figure previously published in Wood et al.17
The Children’s Hospital of Philadelphia’s Institutional Review Board exempted this study as non–human subjects research.
Literature Review
The expert panel received the results of a comprehensive review of the features of bruises indicative of abuse that was published in 2005 by Maguire and colleagues, and an update to that review published in 2013.14,22 These reviews were supplemented with a literature review on the efficacy, risks, utilization patterns, costs, and risks of SS in children with suspected abuse. This supplemental review was performed in PubMed/Medline of English-language journals published between 1990 and 2011, and excluded surveys, reviews, editorials, and case studies. This supplemental review identified 18 relevant articles from which data were abstracted and summarized for the expert panel.10–13,23–36
Expert Panel Assembly
We recruited 10 experts from key pediatric fields, including child abuse, emergency medicine, and inpatient pediatrics (Supplemental Information) after identifying candidates through the following mechanisms: (1) nominations, including self-nominations, from individuals with leadership roles in national professional organizations; (2) review of the literature to identify individuals publishing in the field; and (3) and solicitations of recommendations from colleagues. Selection purposively ensured diversity of clinical views across specialty, practice location, gender, and years in practice.21,37,38
Appropriateness Criteria: Development of Scenarios and Round 1
We generated a list of 198 clinical scenarios characterizing children with bruising for which SS might be considered based on review of the literature. The clinical scenarios included a wide range of patients who might present with bruising and explored the role of the following parameters, which were identified based on review of the literature, on the decision to obtain SS in a child with a bruising: (1) child’s age (<6 months, 6–<9 months, 9–<12 months, and 12–<24 months); (2) caregiver’s reported history of trauma to explain bruising (none, fall, rough play by peer, and accidentally hit with object); (3) location of bruise(s); (4) number of bruises; and (5) type of bruising (patterned or nonpatterned). The scenarios were presented by using a Web-based questionnaire developed in Research Electronic Data Capture hosted at Children’s Hospital of Phildadelphia.39 Scenarios were pilot-tested with physicians outside the panel for clarity and modified as needed.
Each panelist received, via E-mail, an introduction, an electronic link to the questionnaire, literature review results, and standard instructions on rating the appropriateness of performing initial SS for each scenario on a Likert scale of 1 to 9, with 1 = Extremely Inappropriate, 5 = Uncertain, and 9 = Extremely Appropriate. Panelists were advised to use evidence from the literature review and their own clinical judgment to rate SS appropriateness considering the average patient who presents for care with conditions specified in each scenario. We asked panelists to make the following assumptions unless otherwise specified in the scenario: (1) patient is not a victim of a motor vehicle crash or other independently witnessed accidental trauma, (2) there is no known history of underlying bleeding disorder (eg, hemophilia, von Willebrand disorder), (3) physical examination does not reveal additional injuries suggestive of abuse (eg, whip marks, burns, frenulum tears), and (4) there is not a history of birth trauma explaining the bruising. In the first round, panelists rated the appropriateness of SS for each bruise scenario independently, without interaction with other panelists.
Appropriateness Criteria Rating: Moderated Conference Call, Rounds 2 and 3
In preparation for Round 2, each panelist received an anonymized summary of the distribution of the panel’s ratings and their own individual ratings for each scenario from Round 1. During a moderated telephone conference, panelists discussed the ratings focusing on scenarios in which there was disagreement. If the description of a scenario was ambiguous, panelists proposed and voted on modifications. Based on consensus at the conference, we modified some bruise location categories. We also condensed groups of multiple scenarios with similar ratings into single scenarios. For example, panelists rated SS as “appropriate” for all scenarios involving bruising in infants <6 months old with no history of trauma regardless of the bruise location, and they agreed to collapse these scenarios into a single scenario. Based on feedback from the panelists, scenarios with a reported history of accidental trauma were modified to specify that the child presented for care specifically for evaluation of trauma and bruising. An additional set of scenarios was added for bruising noted during an evaluation for unrelated medical concerns (eg, pneumonia) and where, on questioning, a history of accidental trauma was provided by the caregiver. Revisions proposed during the moderated discussion resulted in a revised list of 219 scenarios. In Round 2, the panelists independently rated the appropriateness of SS for each of the 219 revised scenarios.
For each scenario from Round 2, we calculated the median rating (rounded to the nearest whole number) and the dispersion of ratings. Per Rand/UCLA methodology, we classified scenarios for which ratings of 3 or fewer panelists were outside each 3-point region containing the median (1–3, 4–6, or 7–9) as having agreement (eg, median = 7 and 3 or fewer panelists’ ratings were <7), and scenarios for which 4 or more panelists’ ratings were in each extreme (1–3 and 7–9) as having disagreement (eg, median = 7, at least 4 panelists’ ratings were between 1 and 3).27 Scenarios with median ratings of 7 to 9 without disagreement were categorized as “appropriate,” and those with median ratings of 1 to 3 without disagreement were deemed “inappropriate.” Scenarios with median ratings of 4 to 6 or any median with disagreement were categorized as “uncertain.”
In Round 3, panelists independently rated the necessity of SS for scenarios that were classified as appropriate in Round 2. Scenarios with median ratings of 7 to 9 without disagreement were categorized as “necessary” and those with median ratings of 1 to 3 without disagreement were categorized as “appropriate but not necessary.” Median ratings of 4 to 6 or any median with disagreement were categorized as “appropriate but uncertain whether necessary.”
Summary guidelines were synthesized by the study team based on categorizations of scenarios from Rounds 2 and 3.
Results
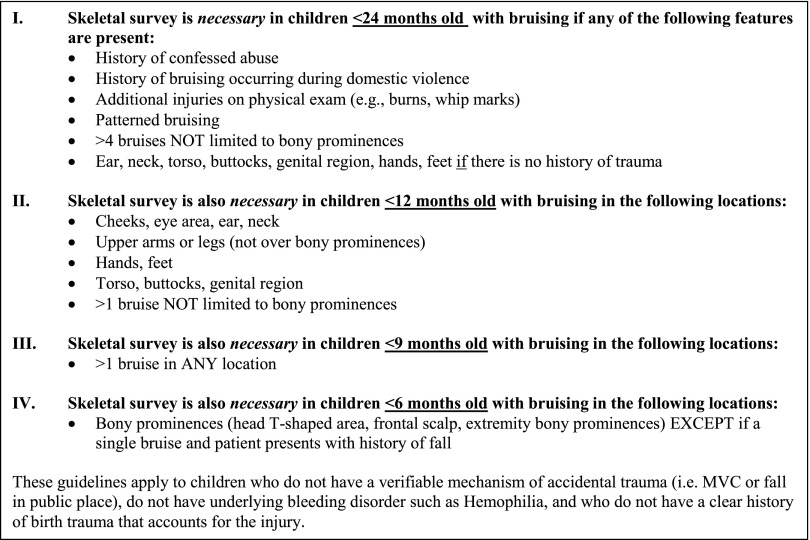
Panelists agreed that initial SS is appropriate for 62% (136), uncertain for 18% (39), and inappropriate for 20% (44) of 219 revised scenarios rated in Round 2 (Tables 1–3). For 37 of 39 scenarios categorized as uncertain, panelists agreed that there was uncertainty about the appropriateness of SS, whereas there was disagreement in 2 scenarios. Of the scenarios for which SS was deemed appropriate, SS was confirmed necessary for 95% (129/136) of scenarios. The panelists’ ratings of these scenarios enabled the development of guidelines for conducting SS in children <24 months old presenting with bruising (Fig 2).
TABLE 1.
Appropriateness and Necessity of SS for Children <24 Months Old Presenting With Bruises: General Scenarios
| Clinical Scenario | |
|---|---|
| Witnessed or confessed history of abuse causing bruise | N |
| History of domestic violence causing bruise | N |
| History of accidental trauma with additional injuries on examination (eg, whip mark, burn) | N |
| Patterneda bruise and no history of trauma | N |
| Patterned bruise and history of accidental trauma | N |
Summary of panelists’ ratings on broad clinical scenarios related to presentations of bruising in children <24 mo old. N, SS appropriate and necessary.
Patterned bruise defined as a bruise that has the imprint of an object.
TABLE 3.
Appropriateness and Necessity of SS for Children Presenting With Multiple Bruises
| Age, mo | No. of Bruises | Bruise Location | Caregiver-Reported History of Traumaa | ||||
|---|---|---|---|---|---|---|---|
| None | Rough Play With Older Sibling/Playmate | Accidental Blunt Trauma With Object | Fall | Previous History of Accidental Trauma | |||
| <6 | 2–4 | Only over bony prominences | N | N | N | N | N |
| Not just over bony prominences | N | N | N | N | N | ||
| >4 | Only over bony prominences | N | N | N | N | N | |
| Not just over bony prominences | N | N | N | N | N | ||
| 6–<9 | 2–4 | Only over bony prominences | N | N | N | N | N |
| Not just over bony prominences | N | N | N | N | N | ||
| >4 | Only over bony prominences | N | N | N | N | N | |
| Not just over bony prominences | N | N | N | N | N | ||
| 9–<12 | 2–4 | Only over bony prominences | U | U | U | I | U |
| Not just over bony prominences | N | N | N | N | N | ||
| >4 | Only over bony prominences | U | N | N | U | N | |
| Not just over bony prominences | N | N | N | N | N | ||
| 12–<24 | 2–4 | Only over bony prominences | I | I | I | I | I |
| Not just over bony prominences | U | N | N | U | U | ||
| >4 | Only over bony prominences | I | I | I | I | U | |
| Not just over bony prominences | U | N | N | N | N | ||
Summary of panelists’ ratings on clinical scenarios related to presentations of bruises, stratified by age. A, SS appropriate but not necessary; I, SS inappropriate; N, SS appropriate and necessary; U, uncertain whether SS is appropriate or not.
In the scenarios presented in the first column (“None”), no history of trauma is provided. For scenarios in columns 2–4, the child presents for medical care with the listed caregiver-reported history. In the fifth column, the child presents for unrelated medical concerns, is noted to have bruising on physical examination, and on questioning, the caregiver provides a history of previous accidental trauma.
FIGURE 2.
Summary of key SS guidelines for examination in the emergency department or inpatient setting of children <24 months old with bruising.
Confessed Abuse, Intimate Partner Violence, Additional Injuries, and Patterned Bruises
Panelists determined that SS is necessary for children <24 months old with bruising from reported abuse or intimate partner violence (Table 1). SS was also deemed necessary for all children with additional injuries unrelated to the bruising (specifically, burns, whip marks, frenulum tears) or with patterned bruises (ie, bruises having the imprint of an object), regardless of any history of trauma. When reported abuse or intimate partner violence, additional injuries, and patterned bruises were absent, the appropriateness and necessity of SS was determined by the child’s age, reported history of accidental trauma, number of bruises, and location of bruises, as presented in the following paragraphs.
Bruising in Young, Nonmobile Infants (<6 months old)
Panelists agreed that SS is necessary in infants <6 months old with bruising, regardless of the number and location of bruises, except in infants presenting with a history of a fall and a single bruise located on the head T-shaped zone (forehead, upper lip, chin), frontal scalp, or extremity bony prominence (Tables 2 and 3).
TABLE 2.
Appropriateness and Necessity of SS for Children <24 Months Old Presenting With a Single Bruise
| Age, mo | Bruise Location | Caregiver-Reported History of Traumaa | ||||
|---|---|---|---|---|---|---|
| None | Rough Play With Older Sibling/Playmate | Accidental Blunt Trauma With Object | Fall | Previous History of Accidental Trauma | ||
| <6 | Head T-shaped areab | N | N | N | U | N |
| Frontal scalp | N | N | N | U | N | |
| Nonfrontal scalp | N | N | N | N | N | |
| Extremity bony prominences | N | N | N | A | N | |
| Cheek/eyes | N | N | N | N | N | |
| Upper arm/upper leg | N | N | N | N | N | |
| Ear/neck/torsoc/hand/foot | N | N | N | N | N | |
| 6–<9 | Head T-shaped area | A | N | U | U | N |
| Frontal scalp | U | N | U | U | U | |
| Nonfrontal scalp | N | N | U | U | N | |
| Extremity bony prominences | U | A | U | U | N | |
| Cheek/eyes | N | N | N | N | N | |
| Upper arm/upper leg | N | N | N | N | N | |
| Ear/neck/torsoc/hand/foot | N | N | N | N | N | |
| 9–<12 | Head T-shaped area | I | I | I | I | I |
| Frontal scalp | U | I | U | I | I | |
| Nonfrontal scalp | U | U | U | I | U | |
| Extremity bony prominences | I | I | I | I | I | |
| Cheek/eyes | N | N | N | N | N | |
| Upper arm/upper leg | N | N | N | N | N | |
| Ear/neck/torsoc/hand/foot | N | N | N | N | N | |
| 12–<24 | Head T-shaped area | I | I | I | I | I |
| Frontal scalp | I | I | I | I | I | |
| Nonfrontal scalp | I | I | I | I | I | |
| Extremity bony prominences | I | I | I | I | I | |
| Cheek/eyes | U | A | U | U | U | |
| Upper arm/upper leg | U | A | U | U | U | |
| Ear/neck/torsoc/hand/foot | N | N | A | A | U | |
Summary of panelists’ ratings on clinical scenarios related to presentations of children <24 mo old with a solitary bruise. A, SS appropriate but not necessary; I, SS inappropriate; N, SS appropriate and necessary; U, uncertain whether SS is appropriate or not.
In the scenarios presented in the first column (“None”), no history of trauma is provided. For scenarios in columns 2–4, the child presents for medical care with the listed caregiver-reported history. In the fifth column, the child presents for unrelated medical concerns, is noted to have bruising on physical examination, and on questioning, the caregiver provides a history of previous accidental trauma.
Head T-shaped area includes the forehead, upper lip, and chin.
Torso area includes chest, abdomen, back, genitals, and buttocks.
Bruising in Young, Premobile Infants (6–<9 months old)
In infants 6 to <9 months old, the panelists deemed SS necessary, regardless of the provided history of trauma, if there were multiple bruises or if bruising was located on the cheek/eye area, upper arm, upper leg, ear, neck, torso (abdomen/chest/buttocks/genitalia), hand, or foot (Tables 2 and 3). The appropriateness and necessity of SS for infants with a single bruise in other locations varied depending on the history provided.
Bruising in Young, Mobile Infants (9–<12 months old)
Panelists judged SS to be necessary in infants 9 to <12 months old if the bruise was located on the cheek/eye area, upper arm, upper leg, ear, neck, torso, hand, or foot, regardless of the history of trauma provided (Tables 2 and 3). They considered SS to be of uncertain appropriateness or even inappropriate in cases with a single bruise on the head T-shaped zone (forehead, upper lip, chin), scalp, or extremity bony prominence and in cases involving multiple (2–4) bruises on bony prominences. The presence of more than 2 bruises not limited to bony prominences, however, led panelists to judge SS as necessary.
Bruising in Young Toddlers (12–<24 months old)
Routine initial SS was deemed inappropriate in children 12 to <24 months old with a single bruise located on the head T-shaped zone (forehead, upper lip, chin), scalp, or extremity bony prominence. SS was deemed necessary in children in this age group with a single bruise only if the bruise is located over the ear, neck, torso, hand, or foot and if there is no history of trauma or a history of rough play or handling explaining the bruise. In most scenarios involving multiple bruises over the bony prominences, SS was deemed inappropriate. In cases of multiple bruises not limited to bony prominences, panelists determined that appropriateness varied with history of trauma provided (Tables 2 and 3).
Discussion
Drawing on evidence in the literature and their own clinical experience, a multispecialty expert panel of pediatric experts agreed on 129 clinical scenarios for which SS is appropriate and necessary in children <24 months old presenting with bruising and on 44 scenarios in which survey is inappropriate, allowing development of guidelines in this population. First, panelists agreed that SS should be performed in children whenever bruising is attributed to abuse or domestic violence. Second, panelists endorsed SS for infants <6 months old with bruising, regardless of history of trauma provided or location of bruising, with the exception of a single bruise over the head T-shaped area (forehead, chin, upper lip) or frontal scalp attributed to a fall. Third, panelists agreed that SS is necessary in all infants <12 months old with bruising located over the cheek/eye area, ear, neck, torso, upper arm, upper leg, hand, or foot. Finally, panelists regarded SS as inappropriate for children 12 to <24 months old with bruising over bony areas including the scalp, extremity bony prominences, and head T-shaped area in the absence of other findings on history or physical injury suggestive of abuse.
Given the rarity of accidental bruising in young nonmobile infants <6 months old,40 the guidelines advocate for almost universal SS imaging in this population. Universal imaging in this population, however, is not currently the norm, as evidenced by the frequency of missed opportunities to diagnose abuse in young infants presenting with bruises.4,6 Previous research has suggested that injury-specific and age-specific SS guidelines could decrease disparities in care and increase abuse detection.41
Our use of Rand methodology in this study is not without limitations. First, the opinions of our selected experts, although drawn from the fields of child abuse pediatrics, emergency medicine, and inpatient pediatrics, might not reflect the views of colleagues in their respective fields. Second, additional clinical details that were not included in the scenarios, such as the size or shape of the bruise, previous history of maltreatment, and observed caregiver-child interactions, might influence determinations of appropriateness and necessity of SS in actual clinical settings. Third, although the expert panel used a systematic review of the literature to inform their ratings, available evidence is limited. Thus, the panelists incorporated their own clinical experience and opinions in decision-making. Fourth, because the guidelines have not been validated, there is uncertainty about their accuracy in identifying those children with bruising at the highest risk of having occult fractures from abuse. Fifth, these guidelines were developed for the hospital setting without input from primary care clinicians, and the degree to which a primary care panel would equally endorse these guidelines is unknown.
Despite the limitations, these results provide detailed consensus guidelines for performing initial SS in children with bruising. The guidelines in this study are not intended to conflict with the recommendation of the Committee on Child Abuse and Neglect to perform SSs in cases of suspected physical abuse in children <24 months old.8 Instead, they are proposed as additional guidance to clinicians regarding when to order initial SS for young children with bruising. A logical next step would be to test the predictive performance of these expert-based guidelines. Recent research reporting occult fracture rates of 10% in children 24 to 36 months old evaluated by child abuse pediatricians for suspected abuse suggests that SS guidelines also may need to be developed for children ≥24 months old.42
Conclusions
A multispecialty panel of pediatric experts reached agreement on clinical bruising scenarios involving children <24 months old in the hospital setting for which initial SS is appropriate and necessary, as well as scenarios for which SS is inappropriate, permitting synthesis of guidelines for performing initial SS in this population. Evaluation of these guidelines is needed to determine whether they can accurately distinguish children who are likely to have occult fractures from counterparts who are unlikely to have occult fractures, thereby increasing detection of cases of abuse while decreasing unnecessary use of SS. Recognizing that the population of children presenting to the primary care setting with bruising might differ from those presenting to the emergency department and inpatient settings, additional work must be done to develop and then validate guidelines specifically for the primary care setting.
Supplementary Material
Acknowledgments
We thank the panelists for the time, effort, and expertise they dedicated to this project. See the Supplemental Information for a profile of panelists.
Footnotes
Dr Wood conceptualized and designed the study, acquired the data, analyzed and interpreted the data, drafted the initial manuscript, and, as corresponding author, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; Drs Rubin, Feudtner, and Localio conceptualized and designed the study, analyzed and interpreted the data, and reviewed and revised the manuscript for important intellectual content; Mr Fakeye conceptualized and designed the study, acquired the data, analyzed and interpreted the data, and reviewed and revised the manuscript for important intellectual content; Ms Mondestin acquired the data, analyzed and interpreted the data, and reviewed and revised the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and take public responsibility for the content presented in the manuscript.
FINANCIAL DISCLOSURE: Dr Wood’s institution has received payment for expert witness court testimony that Dr Wood provided in cases of suspected child abuse for which she was subpoenaed to testify; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by grant 1K23HD071967-01 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Kemp AM, Maguire SA, Nuttall D, Collins P, Dunstan F. Bruising in children who are assessed for suspected physical abuse. Arch Dis Child. 2014;99(2):108–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feldman KW. The bruised premobile infant: should you evaluate further? Pediatr Emerg Care. 2009;25(1):37–39 [DOI] [PubMed] [Google Scholar]
- 3.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281(7):621–626 [DOI] [PubMed] [Google Scholar]
- 4.Sheets LK, Leach ME, Koszewski IJ, Lessmeier AM, Nugent M, Simpson P. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics. 2013;131(4):701–707 [DOI] [PubMed] [Google Scholar]
- 5.Petska HW, Sheets LK, Knox BL. Facial bruising as a precursor to abusive head trauma. Clin Pediatr (Phila). 2013;52(1):86–88 [DOI] [PubMed] [Google Scholar]
- 6.Pierce MC, Kaczor K, Acker D, et al. Bruising missed as a prognostic indicator of future fatal and near-fatal physical child abuse. Poster presented at: Pediatric Academic Societies 2008 Annual Meeting; May 3–6, 2008; Honolulu, HI. Available at: www.abstracts2view.com/pasall/view.php?nu=PAS08L1_3204. Accessed April 26, 2011
- 7.Pierce MC, Smith S, Kaczor K. Bruising in infants: those with a bruise may be abused. Pediatr Emerg Care. 2009;25(12):845–847 [DOI] [PubMed] [Google Scholar]
- 8.Kellogg ND, American Academy of Pediatrics Committee on Child Abuse and Neglect . Evaluation of suspected child physical abuse. Pediatrics. 2007;119(6):1232–1241 [DOI] [PubMed] [Google Scholar]
- 9.Section on Radiology. American Academy of Pediatrics . Diagnostic imaging of child abuse. Pediatrics. 2009;123(5):1430–1435 [DOI] [PubMed] [Google Scholar]
- 10.Duffy SO, Squires J, Fromkin JB, Berger RP. Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics. 2011;127(1). Available at: www.pediatrics.org/cgi/content/full/127/1/e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karmazyn B, Lewis ME, Jennings SG, Hibbard RA, Hicks RA. The prevalence of uncommon fractures on skeletal surveys performed to evaluate for suspected abuse in 930 children: should practice guidelines change? AJR Am J Roentgenol. 2011;197(1):W159–W163 [DOI] [PubMed] [Google Scholar]
- 12.Belfer RA, Klein BL, Orr L. Use of the skeletal survey in the evaluation of child maltreatment. Am J Emerg Med. 2001;19(2):122–124 [DOI] [PubMed] [Google Scholar]
- 13.Day F, Clegg S, McPhillips M, Mok J. A retrospective case series of skeletal surveys in children with suspected non-accidental injury. J Clin Forensic Med. 2006;13(2):55–59 [DOI] [PubMed] [Google Scholar]
- 14.Maguire S, Mann MK, Sibert J, Kemp A. Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child. 2005;90(2):182–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Labbé J, Caouette G. Recent skin injuries in normal children. Pediatrics. 2001;108(2):271–276 [DOI] [PubMed] [Google Scholar]
- 16.Pierce MC, Kaczor K, Aldridge S, O’Flynn J, Lorenz DJ. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 2010;125(1):67–74 [DOI] [PubMed] [Google Scholar]
- 17.Wood JN, Fakeye O, Feudtner C, et al. Development of guidelines for skeletal survey in young children with fractures. Pediatrics. 2014;134(1):45–53 [DOI] [PMC free article] [PubMed]
- 18.Yermilov I, McGory ML, Shekelle PW, Ko CY, Maggard MA. Appropriateness criteria for bariatric surgery: beyond the NIH guidelines. Obesity (Silver Spring). 2009;17(8):1521–1527 [DOI] [PubMed] [Google Scholar]
- 19.Shekelle PG, Schriger DL. Evaluating the use of the appropriateness method in the Agency for Health Care Policy and Research Clinical Practice Guideline Development process. Health Serv Res. 1996;31(4):453–468 [PMC free article] [PubMed] [Google Scholar]
- 20.Shekelle PG, Chassin MR, Park RE. Assessing the predictive validity of the RAND/UCLA appropriateness method criteria for performing carotid endarterectomy. Int J Technol Assess Health Care. 1998;14(4):707–727 [DOI] [PubMed] [Google Scholar]
- 21.Fitch K, Bernstein SJ, Aguilar MS, et al. The RAND/UCLA Appropriateness Method User’s Manual Santa Monica, CA: RAND; 2001. Available at: www.rand.org/pubs/monograph_reports/MR1269.html. Accessed April 26, 2011 [Google Scholar]
- 22.Maguire S, Mann M. Systematic reviews of bruising in relation to child abuse—what have we learnt: an overview of review updates. Evid Based Child Health. 2013;8(2):255–263 [DOI] [PubMed] [Google Scholar]
- 23.Drubach LA, Johnston PR, Newton AW, Perez-Rossello JM, Grant FD, Kleinman PK. Skeletal trauma in child abuse: detection with 18F-NaF PET. Radiology. 2010;255(1):173–181 [DOI] [PubMed] [Google Scholar]
- 24.Mandelstam SA, Cook D, Fitzgerald M, Ditchfield MR. Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child. 2003;88(5):387–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGraw EP, Pless JE, Pennington DJ, White SJ. Postmortem radiography after unexpected death in neonates, infants, and children: should imaging be routine? AJR Am J Roentgenol. 2002;178(6):1517–1521 [DOI] [PubMed] [Google Scholar]
- 26.Kleinman PK, Marks SC, Jr, Richmond JM, Blackbourne BD. Inflicted skeletal injury: a postmortem radiologic-histopathologic study in 31 infants. AJR Am J Roentgenol. 1995;165(3):647–650 [DOI] [PubMed] [Google Scholar]
- 27.Vogelbaum MA, Kaufman BA, Park TS, Winthrop AL. Management of uncomplicated skull fractures in children: is hospital admission necessary? Pediatr Neurosurg. 1998;29(2):96–101 [DOI] [PubMed] [Google Scholar]
- 28.Lane WG, Rubin DM, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288(13):1603–1609 [DOI] [PubMed] [Google Scholar]
- 29.Hansen KK, Campbell KA. How useful are skeletal surveys in the second year of life? Child Abuse Negl. 2009;33(5):278–281 [DOI] [PubMed] [Google Scholar]
- 30.Wood JN, Christian CW, Adams CM, Rubin DM. Skeletal surveys in infants with isolated skull fractures. Pediatrics. 2009;123(2). Available at: www.pediatrics.org/cgi/content/full/123/2/e247 [DOI] [PubMed] [Google Scholar]
- 31.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408–414 [DOI] [PubMed] [Google Scholar]
- 32.Laskey AL, Holsti M, Runyan DK, Socolar RR. Occult head trauma in young suspected victims of physical abuse. J Pediatr. 2004;144(6):719–722 [DOI] [PubMed] [Google Scholar]
- 33.Hicks RA, Stolfi A. Skeletal surveys in children with burns caused by child abuse. Pediatr Emerg Care. 2007;23(5):308–313 [DOI] [PubMed] [Google Scholar]
- 34.Degraw M, Hicks RA, Lindberg D, Using Liver Transaminases to Recognize Abuse (ULTRA) Study Investigators . Incidence of fractures among children with burns with concern regarding abuse. Pediatrics. 2010;125(2). Available at: www.pediatrics.org/cgi/content/full/125/2/e295 [DOI] [PubMed] [Google Scholar]
- 35.Ravichandiran N, Schuh S, Bejuk M, et al. Delayed identification of pediatric abuse-related fractures. Pediatrics. 2010;125(1):60–66 [DOI] [PubMed] [Google Scholar]
- 36.Hong TS, Reyes JA, Moineddin R, Chiasson DA, Berdon WE, Babyn PS. Value of postmortem thoracic CT over radiography in imaging of pediatric rib fractures. Pediatr Radiol. 2011;41(6):736–748 [DOI] [PubMed] [Google Scholar]
- 37.Coulter I, Adams A, Shekelle P. Impact of varying panel membership on ratings of appropriateness in consensus panels: a comparison of a multi- and single disciplinary panel. Health Serv Res. 1995;30(4):577–591 [PMC free article] [PubMed] [Google Scholar]
- 38.Leape LL, Park RE, Kahan JP, Brook RH. Group judgments of appropriateness: the effect of panel composition. Qual Assur Health Care. 1992;4(2):151–159 [PubMed] [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sugar NF, Taylor JA, Feldman KW, Puget Sound Pediatric Research Network . Bruises in infants and toddlers: those who don’t cruise rarely bruise. Arch Pediatr Adolesc Med. 1999;153(4):399–403 [DOI] [PubMed] [Google Scholar]
- 41.Rangel EL, Cook BS, Bennett BL, Shebesta K, Ying J, Falcone RA. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surg. 2009;44(6):1229–1234, discussion 1234–1235 [DOI] [PubMed] [Google Scholar]
- 42.Lindberg DM, Berger RP, Reynolds MS, Alwan RM, Harper NS, Examining Siblings To Recognize Abuse Investigators . Yield of skeletal survey by age in children referred to abuse specialists. J Pediatr. 2014;164(6):1268–1273.e1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.