Abstract
Disparities in pediatric health care quality are well described in the literature, yet practical approaches to decreasing them remain elusive. Quality improvement (QI) approaches are appealing for addressing disparities because they offer a set of strategies by which to target modifiable aspects of care delivery and a method for tailoring or changing an intervention over time based on data monitoring. However, few examples in the literature exist of QI interventions successfully decreasing disparities, particularly in pediatrics, due to well-described challenges in developing, implementing, and studying QI with vulnerable populations or in underresourced settings. In addition, QI interventions aimed at improving quality overall may not improve disparities, and in some cases, may worsen them if there is greater uptake or effectiveness of the intervention among the population with better outcomes at baseline. In this article, the authors review some of the challenges faced by researchers and frontline clinicians seeking to use QI to address health disparities and propose an agenda for moving the field forward. Specifically, they propose that those designing and implementing disparities-focused QI interventions reconsider comparator groups, use more rigorous evaluation methods, carefully consider the evidence for particular interventions and the context in which they were developed, directly engage the social determinants of health, and leverage community resources to build collaborative networks and engage community members. Ultimately, new partnerships between communities, providers serving vulnerable populations, and QI researchers will be required for QI interventions to achieve their potential related to health care disparity reduction.
Keywords: community health, quality improvement, health care disparity
Despite a proliferation of research, policy, and legislative efforts aimed toward eliminating racial/ethnic health disparities in the United States, pervasive inequities in health care persist.1 Since the Institute of Medicine’s seminal report on health disparities,2 an increasing number of pediatric-specific studies reveal that minority children receive poor quality health care across the spectrum of services, including primary care, chronic disease management, and patient safety.1,3–11 In primary care, minority children have lower rates of well child visits, weight and height checks during well child visits, counseling, and time alone with providers for teenagers.5,6 For chronic condition management, non-Hispanic black and Hispanic children with asthma are less likely to have daily inhaled antiinflammatory therapy.7,8 Among patient safety measures, minority children have higher rates of decubitus ulcers and preventable infections during hospitalization.1,4 The deficiencies in quality experienced by minority children are compounded by high rates of poverty and differential access to health care.12–14 With the increasing recognition that such barriers are deeply rooted and complexly intertwined, policy makers have gravitated toward the quality improvement (QI) framework as a solutions-based approach to reduce disparities among children.15,16 With a defined set of principles and intervention tools, QI offers an evidence-based, familiar, and potentially fertile platform for addressing disparities by targeting potentially modifiable aspects of care delivery and refining the approach over time. Yet disparities-focused QI remains a nascent field with little definition of core principles, methodologies, analytics, and expected outcomes. This article aims to (1) describe the rationale for disparities-focused QI, (2) summarize the existing evidence regarding disparities-focused QI, (3) discuss potential barriers to using QI to address pediatric health disparities, and (4) provide an agenda for merging health disparities research and QI into a rigorous, patient-centered field of study and implementation.
Rationale for Using QI to Address Pediatric Health Disparities
QI consists of systematic, data-guided, and continuous actions that aim to measurably improve health care services and the health status of targeted patient groups by improving uptake of best practices into clinical care.17 Although many types of programs and interventions may seek to improve some aspect of care quality, the QI interventions we refer to here explicitly aim to implement services and standards that are known or strongly believed to be effective in improving outcomes, yet have not been integrated adequately into care delivery. Multiple QI frameworks exist, but all aim to understand a health care organization’s current state, identify areas for improvement, design and implement a strategy to achieve that improvement, and then collect data to monitor progress and adjust the strategy as needed over time.18 All QI interventions involve on-going data collection and evaluation of the intervention effects. In some cases, the evaluation is also structured to generate generalizable knowledge about the particular intervention or the QI method; these more rigorous evaluations aimed at generalizable knowledge, rather than just local knowledge, are referred to as QI research or QI science.19 Although in some cases the distinction between a nonresearch QI intervention and QI science is clear, in other cases ambiguity exists. For example, the decision to more rigorously analyze and publish the results of a QI intervention may be made only after the initial results, collected as part of the QI approach, are known. In this article, most of the examples are drawn from the published literature and so by definition relate to QI science. However, the majority of our comments can be applied equally to nonresearch QI interventions, as these also require data collection and evaluation plans, and have the potential to address health care disparities. We will use the terms QI or QI intervention when discussing issues that generally apply to both research and nonresearch undertakings, and QI research or QI science when referring to aspects specifically related to formal research about a QI intervention.
Both QI interventions and QI research have the potential to meaningfully address health disparities, through a diverse set of empirically supported tools to both implement and encourage QI. These include standardized clinical pathways, benchmarking, performance incentives, public reporting, provider reminder systems, and decision aids. Part of the appeal of QI to address disparities lies in the fact that it offers a platform by which to address modifiable care delivery variables, instead of trying to ameliorate less readily mutable factors such as poverty and implicit bias among care providers.13,14,20,21 QI also has the potential to address many possible causes of suboptimal patient outcomes, by sequentially and iteratively targeting various aspects of the patient and provider experience based on on-going metric monitoring. Overall, the conceptual link between health care quality and improving equity has been strengthened by several developments. The Institute of Medicine laid the groundwork for using QI to address disparities by naming equity as a core domain of health care quality, then elevating it to its current status as a cross-cutting domain that should be considered within and across each of the other domains.22 The Agency for Healthcare Research and Quality (AHRQ) has formalized the important link between quality and equity with its annual quality and disparity reports. Legislation in the past several years has also mobilized more resources toward pediatric quality and disparities measurement, including the Children’s Health Insurance Program Reauthorization Act and the Affordable Care Act (ACA). The ACA in particular requires improved collection of race/ethnicity data and reporting of quality performance measures stratified by race/ethnicity.15 As a result, there is both a great deal of optimism at the clinician and organization levels that QI might address modifiable aspects of care delivery that are propagating disparities as well as a great deal of encouragement from policy and regulatory bodies to pursue those avenues. In this current environment, understanding the challenges, opportunities, and future directions of disparities-oriented QI is of relevance to all QI researchers and clinicians caring for underserved populations.
Evidence Base for Disparities-Focused QI
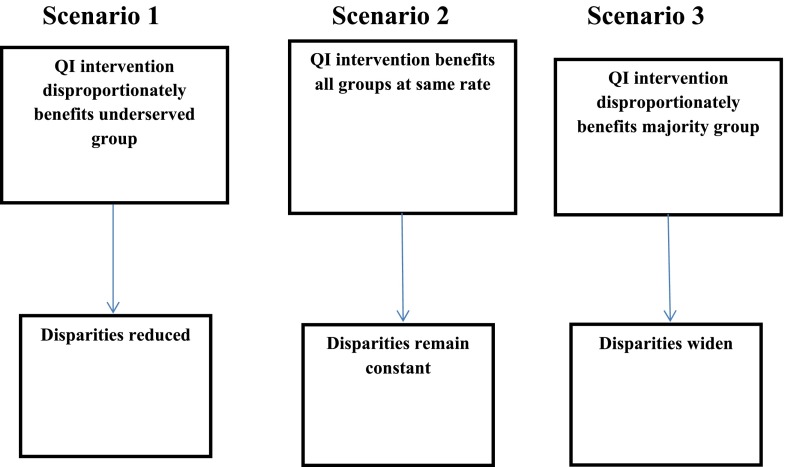
As enumerated by Weinick and Hasnain-Wynia,23 the projected outcomes of successful QI efforts aimed at general clinical populations may follow 3 distinct trajectories, all with differing impact on disparities (Fig 1). The ideal path would occur when application of a general QI intervention results in disparity reduction. In this case, the QI intervention would improve care for all children but have an amplified effect on the care of minority populations experiencing disparities. An early study among adults engendered a great deal of enthusiasm, in which a QI project involving patient outcome monitoring, performance data feedback, and clinician education was initiated to improve care for a diverse population of patients on hemodialysis.24 After multiple improvement cycles, the percentages of white and African American patients receiving appropriate hemodialysis dosages vastly improved. Concurrently, the gap between white and African American patients significantly decreased from 10% to 3%, demonstrating that a QI intervention could have an amplified effect for racial/ethnic minorities.
FIGURE 1.
Potential effects of QI interventions on health disparities. (Adapted from Weinick RM, Hasnain-Wynia R. Quality improvement efforts under health reform: how to ensure that they help reduce disparities—not increase them. Health Aff (Millwood). 2011;30[10]:1838–1839.)
In a second path, a QI intervention may improve quality at the same rate for all groups. If implementation of an intervention improves quality equally for all race/ethnicity groups, disparities remain constant. Multiple adult studies in diverse clinical settings have demonstrated that disparities persist after implementation of overall successful QI interventions.25–28
In a third trajectory, a QI intervention may result in differential rates of uptake or effect of an evidence-based intervention. In these scenarios, disadvantaged populations may benefit less, with a consequential widening of gaps in care between groups. If a provider in a high minority-serving practice lacks the resources to implement a particular decision aid tool that is implemented elsewhere, the gaps between well-resourced practices and poorly resourced practices may widen. Alternatively, QI interventions designed with data exclusively from majority populations (who are more likely to participate in research)29 may lead to initiatives that have efficacy in only those groups. For example, if a major driver of inhaled steroid underuse for minority patients is lack of trust between parents and providers, leading to lower adherence to provider recommendations, a decision support tool aimed at provider prescribing might not improve outcomes among minority patients, while being highly effective for nonminority patients. This phenomenon of QI exacerbating disparities has been observed in adult QI interventions. In 1 study, the public release of coronary artery bypass grafting report cards in New York was associated with a widening of the disparity in grafting use between white versus African American and Hispanic patients.30 This study highlighted the potential unintended consequences of public reporting, such as physicians avoiding high-risk patients to improve their ratings.
A systematic review by Chin et al31 provided pediatric-specific data on the potential for interventions focused on quality to reduce child disparities. Included studies were those that focused on reducing racial/ethnic disparities or in which at least 50% of study participants were from minority backgrounds. Study interventions had to target 1 or more aspects of health care quality or outcomes among children, but a QI framework or the iterative approach typically used in QI were not required. Successful interventions relied on lay health outreach workers, home visits, and integration of the intervention into existing community-based organizations. Many of the included studies did not assess changes in disparities between racial/ethnic groups as an outcome, but looked only at within-group improvement. However, these findings point toward attributes that may help QI interventions succeed to decrease disparities.
The evidence base for QI as a method for addressing disparities was most recently assessed by AHRQ in a systemic review that aimed to evaluate whether QI interventions were effective in reducing disparities.32 No pediatric studies met inclusion criteria. The review, consisting of 14 studies, concluded there was insufficient evidence to demonstrate that QI interventions can close disparity gaps. The authors of the review cited several challenges to conducting such a systematic review, including the paucity of studies assessing gaps between groups; the breadth and heterogeneity of clinical conditions, populations, QI strategies, comparators, clinical outcomes, and disparities of interest; and challenges to indexing QI strategies in medical literature databases. The overall findings of the AHRQ evidence report were consistent with a previous review by Beach et al33 demonstrating a lack of evidence supporting QI interventions designed to reduce disparities. In this review, 27 controlled trials (4 pediatric or adolescent-focused) were assessed. Only 2 QI studies specifically targeted reducing disparities, whereas the remaining studies were generic QI interventions. Overall, there was poor evidence to determine which interventions might reduce disparities between racial/ethnic minority patients and majority patients. This lack of compelling evidence for QI interventions to decrease disparities reflects the current state of the field and the need to address specific barriers in future research.
Setting an Agenda to Integrate QI and Pediatric Health Disparities Research
QI approaches face special challenges to reducing inequities in care, and these challenges are encountered at multiple levels, from the health care system to the patient population. First, many health care institutions do not routinely collect data on race/ethnicity or preferred language for care. Therefore, data according to relevant subgroups may not be available at the time that QI interventions are chosen, implemented, and evaluated. Second, QI interventions such as pay-for-performance programs and public reporting have the potential to undermine care for underserved populations in multiple ways.34 These include incentivizing providers to avoid caring for children who are perceived to be high-risk and financially penalizing providers without the resources to participate in costly QI programs.34,35 Third, patients in underserved communities may not have the capacity to fully engage in QI efforts because of economic, cultural, or language barriers. Therefore, any application of QI interventions to disparities must overcome these challenges through careful selection of conceptual frameworks, research design, and evaluation.
Despite an evidence base still in its infancy and substantial barriers to conducting QI interventions in underserved communities, QI remains a promising pathway toward addressing the modifiable aspects of care delivery that cause and propagate disparities. As others have noted, the difficulty in establishing a disparities-based QI agenda is the multifactorial nature of disparities attributable to the social determinants of health.16,36 The next critical maturation step in integrating health disparities research and QI interventions into a cohesive, robust field will require researchers to modify historical paradigms for conducting both health disparities and QI interventions. Below, we outline 5 key areas of focus for clinicians, researchers, and policy makers investing in advancing the field of QI disparities.
Consideration of Comparators
By definition, interventions aimed at decreasing disparities require data on both the minority group(s) in question and the majority group being used as a reference population, to track the disparity between the 2 over time. Although health disparities research has historically relied on such racial/ethnic comparators, the role of such comparators in QI evaluations may require reconsideration in some contexts for several reasons. As already mentioned, baseline race/ethnicity data are not consistently available for QI interventions, although this circumstance will likely improve because of the ACA.15 Second, there are no benchmarks for what constitutes a clinically important reduction of a racial/ethnic disparity. Third, QI studies may be underpowered to detect differences due to insufficient numbers of children in different racial/ethnic categories. Fourth, because many providers who serve minority patients tend to serve predominantly minority populations, nonminority reference groups may not be readily available within the same clinical setting. Therefore, some QI projects may be best conducted by targeting well-documented, high-risk populations for intervention, rather than trying to improve care for all children in a clinical setting simultaneously. This will allow better customization and cultural tailoring of QI initiatives, whereby specific root causes of disparities can be targeted, either with the initial intervention or iteratively over time in response to data monitoring. This approach may in turn increase the efficiency and effectiveness of interventions, and it is reflected in most of the currently published QI interventions to improve care for underserved children.31,37,38 Comparisons of outcomes according to race/ethnicity will still be important to monitor progress and guard against exacerbation of disparities with QI initiatives. However, for customized interventions targeted to single high-risk groups, such comparisons will not be feasible. Instead, comparisons made within a specifically targeted group, ideally between practices or hospitals serving similar populations, should be considered for robustly evaluating the impact of the QI intervention.
Rigor of QI Interventions Addressing Disparities
Increasing the methodological rigor of the development, implementation, and evaluation of QI interventions will be essential if we are to successfully leverage these techniques to decrease disparities. Uncontrolled, observational designs used by many QI intervention evaluations have impeded our ability to understand what works.39,40 This is a particular problem for lower-resourced health care settings, which are less likely to have a QI team of their own developing internal interventions, and more likely to be reliant on approaches developed and studied at well-resourced institutions. Improved methodological rigor and reporting from studies at well-resourced institutions will help those with fewer resources identify interventions that are more likely to work with their populations.
Specifically, groups undertaking QI research should consider robust evaluation methods, such as interrupted time series analysis,41 statistical process control,42 or stepped wedge design.43 These methods are particularly relevant for disparities-focused interventions, because they evaluate effectiveness in real-world settings, including the influence of structural and subconscious processes that are difficult to measure but contribute to disparities. They also help separate intervention effect from temporal and contextual influences, which is essential for successful translation of interventions from 1 setting into another. For example, Ratanawongsa et al’s44 use of a stepped wedge design to study a multilingual telephone coaching intervention for Medicaid-insured adults with diabetes illustrates the design’s strengths. The authors found that the gradual roll-out of the intervention allowed for practical allocation of their time and resources, and allowed the analysis to account for secular trends and iterative changes to the intervention over time. It also included a relevant comparison group without withholding a promising intervention from vulnerable patients, as a traditional control group would. In addition, preexisting race/ethnicity data are not needed for a stepped wedge design, as long as they are collected from the start of the evaluation. Speroff and O’Connor45 offer further examples of rigorous evaluation methods appropriate to disparities-oriented QI research.
Understanding Context and Intended Mechanism of Intervention
QI interventions focused on disparities would also benefit from a careful consideration of intervention mechanisms and context, both in selecting and evaluating interventions. To understand the likely impact of an intervention, provider groups who are looking to the literature or other institutions for QI interventions should carefully consider the care structure, processes, and outcomes currently in place in their health care setting; the context surrounding those care delivery attributes; how those compare with the ones described in the study; and whether they differ for different groups of patients. For example, family-centered rounds have been widely implemented, introducing a new process to engage patients and families in inpatient care and improve communication.46,47 However, the different preexisting processes for engaging and communicating with families with limited English proficiency were generally not taken into account. Even when professional interpreters were provided for family-centered rounds, the experiences and comprehension of families with limited English proficiency differed from those of English proficient families, highlighting the difficulties associated with implementing a single improvement initiative across multiple groups that have different preexisting processes.48,49 In other arenas, investigators have recognized that many low-income and minority families interface with the health care system in ways that differ from other families. For example, Patterson et al50 report on a QI intervention they developed to facilitate provision of overdue well-child services, including immunizations, developmental screening, and anticipatory guidance, at acute care visits, to improve services for families that might otherwise face financial and logistical barriers to coming in for nonurgent care. These examples illustrate the importance of understanding the potential mechanisms of action of the intervention and potential barriers or facilitators to uptake or effectiveness. In some cases, the addition of a novel, low-cost delivery approach with high use among vulnerable populations, such as text messaging,51 may enhance the effectiveness of an intervention developed among other populations. Careful attention should also be paid to the context in which a project is conducted, including the available resources, organizational culture, leadership involvement, and data infrastructure, because contextual factors can greatly facilitate or impede the success of the intervention.52–54 Understanding the context and intended mechanism of the intervention is critical to ensuring effective translation to a new setting or population.
Engagement of Social Determinants of Health
More direct engagement of social determinants of health in QI interventions may not only promote improved health outcomes in clinical settings but also advance population health in communities. Increasingly, researchers are assessing community factors to inform QI efforts and improve community health at multiple levels, beyond those normally directly involved in health care access or delivery. In a study by Beck et al,55 a geographic social risk index was found to be associated with asthma-related reutilization among children. The tool they developed and embedded in the electronic medical record was then used to inform targeted, patient-level interventions, including referral for reduction of in-home environmental risks such as mold.56 Such geographic data could also inform community level preventive approaches, targeting neighborhood hot spots that could benefit from public health initiatives. In a study by Woods et al,38 a comprehensive QI intervention improved health outcomes for urban, low-income children with asthma. This study addressed social determinants in several ways. First, program development used a community-based participatory approach involving Community and Family Advisory Boards. Second, the multidimensional intervention addressed several social determinants of health, including exposure to high levels of asthma triggers found in poor housing and deteriorating schools and chronic stress due to community violence. Intervention components consisted of providing all patients with high efficiency particulate air vacuums and bedding encasements, environmental materials tailored to their needs, and extermination as needed. Community health workers provided culturally effective communication about asthma treatment and addressed personal beliefs about asthma.
Leveraging Community Resources and Capacity to Overcome Resource Gaps
As many vulnerable populations receive care in underresourced health care settings, promotion of QI in these areas may require significant modification and adaptation of existing interventions, careful attention to both financial and intellectual resources, and creative approaches to funding and implementation. Previous research on health disparities collaboratives in community health centers demonstrates that QI efforts conducted with underserved populations can be effective with appropriate funding.57 Without such funding, collaboration with community-based organizations and integration of community-level mechanisms for patient outreach may provide opportunities to leverage resources and increase the sustainability of initiatives. For example, lay health workers have demonstrated some benefit in improving health outcomes for children with chronic conditions,58 by establishing effective links between clinics and community members through education and coaching.31 Such collaboration with community organizations and services may result in QI interventions more likely to meet community needs. These partnerships may also lead to funding opportunities through agencies such as the Patient Centered Outcomes Research Institute, where patient and stakeholder engagement is central in the research mission. The Patient Centered Outcomes Research Institute, which has an Addressing Disparities program, requires funded applicants to involve patients and relevant stakeholders on their research teams throughout the study, helping to identify research questions, choose comparators and outcomes, identify and recruit study populations, develop research materials, and interpret and disseminate findings.59
Conclusions
With improving quality established as a central tenet of ongoing health care system redesign, rigorously conducted QI interventions represent a core strategy toward achieving the triple aim of enhancing patient experience, lowering cost, and improving population health.60 For underserved children, QI holds promise as a method by which to address longstanding inequities in care delivery. The medical literature has yet to reveal a demonstrable impact of QI interventions on reducing disparities. However, these findings may speak to the complex nature of health disparities, measurement and evaluation challenges, and the structural barriers encountered in underresourced communities. Successful integration of QI and health disparities research will require reconsideration of comparators; improved methodological rigor in selecting and evaluating interventions; increased consideration of context; proactive attention to social determinants of health; and leveraging of community resources. More practically, it will necessitate new collaborative partnerships between QI researchers in highly resourced settings and frontline providers committed to improving the care of minority populations. Such efforts may foster more tailored, efficient interventions and inform initiatives to improve clinical outcomes, ultimately improving community and population health.
Footnotes
Dr Lion conceptualized the concept and design of the article, helped draft the initial manuscript, and critically revised the manuscript for important intellectual content; Dr Raphael conceptualized the concept and design of the article, drafted the initial manuscript, critically revised the manuscript for important intellectual content, and supervised the study; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this work were supported by National Institute of Child Health and Human Development grant 1K23 HD078507 (Dr Lion) and National Heart, Lung, and Blood Institute grant 1K23 HL105568 (Dr Raphael). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr. 2010;10(2):95–118 [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 3.Raphael JL, Beal AC. A review of the evidence for disparities in child vs adult health care: a disparity in disparities. J Natl Med Assoc. 2010;102(8):684–691 [DOI] [PubMed] [Google Scholar]
- 4.Flores G, Ngui E. Racial/ethnic disparities and patient safety. Pediatr Clin North Am. 2006;53(6):1197–1215 [DOI] [PubMed] [Google Scholar]
- 5.Hambidge SJ, Emsermann CB, Federico S, Steiner JF. Disparities in pediatric preventive care in the United States, 1993-2002. Arch Pediatr Adolesc Med. 2007;161(1):30–36 [DOI] [PubMed] [Google Scholar]
- 6.Coker TR, Rodriguez MA, Flores G. Family-centered care for US children with special health care needs: who gets it and why? Pediatrics. 2010;125(6):1159–1167 [DOI] [PubMed] [Google Scholar]
- 7.Cabana MD, Lara M, Shannon J. Racial and ethnic disparities in the quality of asthma care. Chest. 2007;132(suppl 5):810S–817S [DOI] [PubMed] [Google Scholar]
- 8.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109(5):857–865 [DOI] [PubMed] [Google Scholar]
- 9.Raphael JL, Guadagnolo BA, Beal AC, Giardino AP. Racial and ethnic disparities in indicators of a primary care medical home for children. Acad Pediatr. 2009;9(4):221–227 [DOI] [PubMed] [Google Scholar]
- 10.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3). Available at: www.pediatrics.org/cgi/content/full/115/3/e310 [DOI] [PubMed] [Google Scholar]
- 11.Raphael JL, Zhang Y, Liu H, Tapia CD, Giardino AP. Association of medical home care and disparities in emergency care utilization among children with special health care needs. Acad Pediatr. 2009;9(4):242–248 [DOI] [PubMed] [Google Scholar]
- 12.Duncan GJ, Brooks-Gunn J, Aber JL, eds. Neighborhood Poverty: Context and Consequences for Children. Vol 1. New York, NY: Russell Sage Foundation; 1997 [Google Scholar]
- 13.Duncan GJ, Brooks-Gunn J, eds. Consequences of Growing Up Poor. New York, NY: Russell Sage Foundation; 1997 [Google Scholar]
- 14.Duncan GJ, Brooks-Gunn J, Aber JL, eds. Neighborhood Poverty: Policy Implications in Studying Neighborhoods. Vol 2. New York, NY: Russell Sage Foundation; 1997 [Google Scholar]
- 15.Beal AC. High-quality health care: the essential route to eliminating disparities and achieving health equity. Health Aff (Millwood). 2011;30(10):1868–1871 [DOI] [PubMed] [Google Scholar]
- 16.Beal AC, Hasnain-Wynia R. Disparities and quality: the next phase for high-performing pediatric care. Acad Pediatr. 2013;13(suppl 6):S21–S22 [DOI] [PubMed] [Google Scholar]
- 17.Quality Improvement Methodology. 2014. Available at: www.hrsa.gov/quality/toolbox/methodology/qualityimprovement/index.html. Accessed September 17, 2014
- 18.Donabedian A. The effectiveness of quality assurance. Int J Qual Health Care. 1996;8(4):401–407 [DOI] [PubMed] [Google Scholar]
- 19.Baily MA, Bottrell M, Lynn J, Jennings B, Hastings Center . The ethics of using QI methods to improve health care quality and safety. Hastings Cent Rep. 2006;36(4):S1–S40 [DOI] [PubMed] [Google Scholar]
- 20.Zatzick DF, Koepsell T, Rivara FP. Using target population specification, effect size, and reach to estimate and compare the population impact of two PTSD preventive interventions. Psychiatry. 2009;72(4):346–359 [DOI] [PubMed] [Google Scholar]
- 21.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001 [PubMed] [Google Scholar]
- 23.Weinick RM, Hasnain-Wynia R. Quality improvement efforts under health reform: how to ensure that they help reduce disparities—not increase them. Health Aff (Millwood). 2011;30(10):1837–1843 [DOI] [PubMed] [Google Scholar]
- 24.Sehgal AR. Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA. 2003;289(8):996–1000 [DOI] [PubMed] [Google Scholar]
- 25.Areán PA, Ayalon L, Hunkeler E, et al. IMPACT Investigators . Improving depression care for older, minority patients in primary care. Med Care. 2005;43(4):381–390 [DOI] [PubMed] [Google Scholar]
- 26.Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166(6):675–681 [DOI] [PubMed] [Google Scholar]
- 27.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood). 2011;30(4):707–715 [DOI] [PubMed] [Google Scholar]
- 28.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353(7):692–700 [DOI] [PubMed] [Google Scholar]
- 29.Schmotzer GL. Barriers and facilitators to participation of minorities in clinical trials. Ethn Dis. 2012;22(2):226–230 [PubMed] [Google Scholar]
- 30.Werner RM, Asch DA, Polsky D. Racial profiling: the unintended consequences of coronary artery bypass graft report cards. Circulation. 2005;111(10):1257–1263 [DOI] [PubMed] [Google Scholar]
- 31.Chin MH, Alexander-Young M, Burnet DL. Health care quality-improvement approaches to reducing child health disparities. Pediatrics. 2009;124(suppl 3):S224–S236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McPheeters ML, Kripalani S, Peterson NB, et al. Quality Improvement Interventions to Address Health Disparities. Closing the Quality Gap: Revisiting the State of the Science. Evidence Report No. 208. Rockville, MD: Agency for Healthcare Research and Quality; 2012 [PMC free article] [PubMed]
- 33.Beach MC, Gary TL, Price EG, et al. Improving health care quality for racial/ethnic minorities: a systematic review of the best evidence regarding provider and organization interventions. BMC Public Health. 2006;6:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedberg MW, Safran DG, Coltin K, Dresser M, Schneider EC. Paying for performance in primary care: potential impact on practices and disparities. Health Aff (Millwood). 2010;29(5):926–932 [DOI] [PubMed] [Google Scholar]
- 35.Chien AT, Wroblewski K, Damberg C, et al. Do physician organizations located in lower socioeconomic status areas score lower on pay-for-performance measures? J Gen Intern Med. 2012;27(5):548–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Homer C. A tall order: improve child health. Acad Pediatr. 2013;13(suppl 6):S5–S6 [DOI] [PubMed] [Google Scholar]
- 37.Lob SH, Boer JH, Porter PG, Núñez D, Fox P. Promoting best-care practices in childhood asthma: quality improvement in community health centers. Pediatrics. 2011;128(1):20–28 [DOI] [PubMed] [Google Scholar]
- 38.Woods ER, Bhaumik U, Sommer SJ, et al. Community asthma initiative: evaluation of a quality improvement program for comprehensive asthma care. Pediatrics. 2012;129(3):465–472 [DOI] [PubMed] [Google Scholar]
- 39.Rotter T, Kinsman L, James E, Machotta A, Steyerberg EW. The quality of the evidence base for clinical pathway effectiveness: room for improvement in the design of evaluation trials. BMC Med Res Methodol. 2012;12:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McDonald KM, Schultz EM, Chang C. Evaluating the state of quality-improvement science through evidence synthesis: insights from the closing the quality gap series. Perm J. 2013;17(4):52–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309 [DOI] [PubMed] [Google Scholar]
- 42.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown CA, Lilford RJ. The stepped wedge trial design: a systematic review. BMC Med Res Methodol. 2006;6:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ratanawongsa N, Handley MA, Quan J, et al. Quasi-experimental trial of diabetes Self-Management Automated and Real-Time Telephonic Support (SMARTSteps) in a Medicaid managed care plan: study protocol. BMC Health Serv Res. 2012;12:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Speroff T, O’Connor GT. Study designs for PDSA quality improvement research. Qual Manag Health Care. 2004;13(1):17–32 [DOI] [PubMed] [Google Scholar]
- 46.Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126(1):37–43 [DOI] [PubMed] [Google Scholar]
- 47.Kuo DZ, Sisterhen LL, Sigrest TE, Biazo JM, Aitken ME, Smith CE. Family experiences and pediatric health services use associated with family-centered rounds. Pediatrics. 2012;130(2):299–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lion KC, Mangione-Smith R, Martyn M, Hencz P, Fernandez J, Tamura G. Comprehension on family-centered rounds for limited English proficient families. Acad Pediatr. 2013;13(3):236–242 [DOI] [PubMed] [Google Scholar]
- 49.Seltz LB, Zimmer L, Ochoa-Nunez L, Rustici M, Bryant L, Fox D. Latino families’ experiences with family-centered rounds at an academic children’s hospital. Acad Pediatr. 2011;11(5):432–438 [DOI] [PubMed] [Google Scholar]
- 50.Patterson BL, Gregg WM, Biggers C, Barkin S. Improving delivery of EPSDT well-child care at acute visits in an academic pediatric practice. Pediatrics. 2012;130(4). Available at: www.pediatrics.org/cgi/content/full/130/4/e988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mitchell SJ, Godoy L, Shabazz K, Horn IB. Internet and mobile technology use among urban African American parents: survey study of a clinical population. J Med Internet Res. 2014;16(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaplan HC, Froehle CM, Cassedy A, Provost LP, Margolis PA. An exploratory analysis of the model for understanding success in quality. Health Care Manage Rev. 2013;38(4):325–338 [DOI] [PubMed] [Google Scholar]
- 53.McDonald KM. Considering context in quality improvement interventions and implementation: concepts, frameworks, and application. Acad Pediatr. 2013;13(suppl 6):S45–S53 [DOI] [PubMed] [Google Scholar]
- 54.Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102(12):2308–2314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Beck AF, Simmons JM, Sauers HS, et al. Connecting at-risk inpatient asthmatics to a community-based program to reduce home environmental risks: care system redesign using quality improvement methods. Hosp Pediatr. 2013;3(4):326–334 [DOI] [PubMed] [Google Scholar]
- 57.Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care. 2010;48(8):668–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raphael JL, Rueda A, Lion KC, Giordano TP. The role of lay health workers in pediatric chronic disease: a systematic review. Acad Pediatr. 2013;13(5):408–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Selby JV, Lipstein SH. PCORI at 3 years—progress, lessons, and plans. N Engl J Med. 2014;370(7):592–595 [DOI] [PubMed] [Google Scholar]
- 60.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769 [DOI] [PubMed] [Google Scholar]