Abstract
Introduction
Oral Submucous Fibrosis (OSMF) is precancerous condition caused by areca nut chewing characterized by restricted mouth opening, burning sensation and stiffness & blanching of oral mucosa. Complete regression of the condition had not been achieved in all cases with any of the present treatment regimens. Curcumin is (diferuloylmethane), a yellow pigment in curry powder, exhibits anti-oxidant, anti-inflammatory, and pro-apoptotic activities. Hence an interventional study was undertaken to establish the efficacy of curcumin in OSMF patients.
Settings & design
A randomized open label, interventional study was conducted in forty patients with clinically and histologically proven Oral Submucous Fibrosis.
Materials & methods
Forty patients with clinically and histologically proven Oral Submucous Fibrosis were selected for the study and were randomly divided into 2 groups. The first group was treated with weekly intralesional injection of 4 mg Dexamethasone & 1500 I.U Hyaluronidase and the second group by oral administration of two Curcumin tablets (Turmix 300 mg) per day for 3 months each. Improvement of burning sensation, interincisal distance and tongue protrusion was evaluated on a weekly basis.
Results
Burning sensation improved in both the groups from early to late stages. Complete resolution of burning sensation was noted with turmix. The mean increase in interincisal distance was 3.13 mm and 1.25 mm respectively in groups 1 &2. The interincisal distance improved in both the groups, with significant results at the end of first month. Tongue protrusion showed greater recovery at the end of 1st month in group 1 when compared with group 2.
Conclusion
Turmix is beneficial and effective in reducing burning sensation in early OSMF patients.
Keywords: Conventional therapy, Curcumin, Intralesional dexamethasone, Oral Submucous Fibrosis, Turmix
Key message.
In the earlier studies, Curcumin had not been compared with intralesional steroid therapy in OSMF patients. This study encourages the use of curcumin as it effectively reduced burning sensation and also improved the mouth opening.
1. Introduction
Pindborg has defined Oral Submucous Fibrosis (OSMF) as “an insidious chronic disease affecting any part of the oral cavity and occasionally extending to the pharynx and esophagus, although, occasionally preceded by and/or associated vesicle formation. It is always associated with juxta-epithelial inflammatory reaction followed by fibroelastic changes in the lamina propria, with epithelial atrophy leading to stiffness of the oral mucosa causing trismus and difficulty in eating”.1 The prevalence in India had increased in the recent years to 6.42% with a higher predominance in the southern parts of the subcontinent.2 OSMF is seen commonly in males between 20 and 40 yrs age. The common sites involved are labial mucosa, buccal mucosa, retromolar pads, soft palate and floor of the mouth. Fibrotic changes of the pharynx, esophagus and paratubal muscles of eustachian tubes had been reported.2 Early features of OSMF include burning sensation, hypersalivation/xerostomia and mucosal blanching with marble like appearance. The mucosa later becomes leathery and inelastic with palpable fibrous bands resulting in restricted mouth opening. Eventually, OSMF leads to restriction of tongue movements, difficulty in swallowing, speech & hearing defects and defective gustatory sensation.3
The etiopathogenesis of OSMF is complex and incompletely understood. Oral Submucous Fibrosis is a potentially malignant disorder attributed to areca nut (betel nut) chewing. The other proposed etiological factors include excessive chilly consumption, vitamin B and iron deficiency, autoimmunity, genetic and environmental factors.2–5 Areca nut consists of alkaloids like arecoline, arecaidine, guvacine and guvacoline apart from flavanoids, tannins, catechin and copper. The alkaloids stimulate the fibroblasts to produce more collagen, while its structure is stabilized by catechin and tannins. The increased crosslinkage of collagen results from upregulation of the copper dependent enzyme lysyl oxidase.4,5 Documented evidence favors areca nut as the main etiological agent owing to cytotoxic, apoptotic and proliferative effects. The cytotoxic effects, in addition to the release of free radical induced mutations by areca nut, induces genotypic & phenotypic alterations, a key point in the pathogenesis of OSMF.6 Apart from areca nut, commercial products like gutkha, mawa and pan masala have been shown to cause OSMF rapidly due to larger amounts of areca nut in these processed products and/or the synergistic action of nicotine over arecoline.6–8 The ideal goals of therapy of this potentially malignant disorder include not only amelioration of the symptoms (burning sensation, restriction of mouth opening), but also stop further disease progression and malignant transformation. Complete regression of this mucosal condition had not been achieved in any of the case studies reported till date, despite the number of drugs or interventions tried, hence an attempt at finding a permanent cure is still going on.6,9,10
Plants have been widely used as medicinal cure since ancient times among which Turmeric had always occupied an important place.11 Turmeric (the common name for Curcuma longa) is an Indian spice derived from the rhizomes of the plant and is used in Ayurvedic medicine to treat inflammatory conditions. The primary active constituent of turmeric ‘Curcumin’ (diferuloylmethane), had been identified in 1910 by Lampe, Milobedzka.12 Curcumin is a pleiotropic molecule that targets molecular mediators of inflammation. It had been widely used in inflammatory bowel disease, pancreatitis, rheumatoid arthritis, etc. with good results. The medicinal activity had been attributed to various pharmacological activities, including antioxidant, antimicrobial, pro-apoptotic and anti-inflammatory effects.12,13 Zhang SS et al have demonstrated antifibrotic activity of curcumin on human myofibroblasts and suggested that it may be of use in the treatment of OSMF.13
It may hence be hypothesized that the anti-inflammatory, antioxidant and antifibrotic properties of curcumin acting simultaneously, may interfere with the progression of OSMF at multiple stages in the pathogenesis of this complex disease. These invaluable properties of a commonly available, well tolerated, house hold ingredient with a non invasive route of administration prompted us to undertake this study. Intralesional steroid therapy in the management had been well documented and accepted for its beneficial effects.9,10,14 However, Thakur N et al report that management of OSMF by various surgical and intralesional injections results in scarring and fibrosis in the long term.6
Hence, the current study was undertaken to assess the efficacy of curcumin in OSMF by comparing it with the most accepted therapy viz. intralesional steroid injections.
2. Materials and method
2.1. Study design
A randomized open label, interventional study was conducted in forty patients with clinically and histologically proven Oral Submucous Fibrosis.
2.2. Subjects
Forty OSMF patients attending dept. of Oral Medicine & Radiology, Career Dental College, over a period of 8 months, were included in the final study as shown in Fig. 1. Institutional ethical clearance for the study was obtained. Informed consent was taken from all the study participants. Diagnosis and clinical staging of OSMF was based Khanna & Andrade classification.15
Fig. 1.
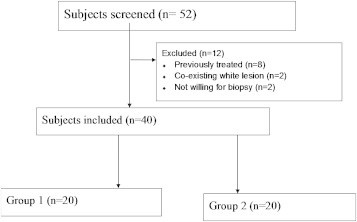
Flow diagram of the study.
2.3. Inclusion & exclusion criteria
Patients within the age group of 20–40 years, with a histological diagnosis of OSMF were included in the study. Patients presenting with co existing malignancy/white lesions, known allergies to drugs or previously treated for OSMF and not willing for biopsy were excluded from the study.
2.4. Procedure
Detailed history with special emphasis on type, frequency in a day and duration of habit (areca nut, gutkha or combination of both), whether they swallowed the product or spitted it out were noted. The findings of clinical examination were recorded on a specially designed proforma which were supplemented along with clinical photographs. Patients were encouraged for habit cessation and were subjected to oral prophylaxis to motivate them for abstinence. The clinical grading was based on Khanna & Andrade classification.15 The routine hematological and blood sugar investigations were conducted. Incisional biopsy was taken from the buccal/labial mucosa, depending on the severity, under local anesthesia and was subjected to histopathological evaluation.
The subjects with confirmed histopathological diagnosis were then randomly divided into 2 groups of 20 each by using table of random numbers. The first group was given weekly submucosal intralesional injections of Dexamethasone (Inj Decadran 4 mg/ml, marketed by Merck & Co, Inc), 1500 International units of Hyaluronidase (Hynidase 1500 I.U.) along with 0.5 ml of 2% (1:80,000) Lignocaine Hydrochloride. The selection of the sites of injection was based on clinical judgment. Injections were given at multiple sites with a 26 guage needle, given on alternate sides for a period of three months. The combination of dexamethasone & hyaluronidase is long acting, hence was injected on alternate sides. The second group was given oral administration of 2 tablets of Turmix (Film coated tablet containing C. longa 300 mg, Piperine 5 mg, Sanat Pharma Ltd) given once daily for a period of 3 months. No alternative or supplementary forms of therapy were used in any of the study participants, except the study medications. No side effects such as nausea, stomach upsets, diarrhea were reported by any patient. Both groups were treated for a period of 12 weeks.
2.5. Follow-up
Clinical evaluation was done during their subsequent visits through the assessment of improvement of subjective symptoms like burning sensation, objective signs like interincisal distance (IID) and tongue protrusion (TP). Patients were explained about visual analog scale (VAS) and were asked to mark the severity of burning sensation on it. The patients were enquired for the improvement of burning sensation or the inability to take hot & spicy food at the subsequent visits and were asked to mark it again on a VAS scale. Burning sensation was then recorded on a percentage reduction basis. Interincisal distance (IID) was measured with vernier calipers between the right maxillary and mandibular central incisors on maximum opening. If these teeth were missing, they were measured on the corresponding teeth of the left arches. The measurements at subsequent visits were done at the previously recorded sites only, to avoid misinterpretation. Tongue protrusion was measured with a scale as the distance of movement of the tongue beyond the incisal tips of the lower incisors. These parameters were analyzed at baseline, at the end of 1st, 2nd and 3rd months. All measurements were taken by the same examiner (MY) to avoid observer variability.
2.6. Statistical analysis
The baseline profile between the groups was compared using Students t test. The improvement observed within the group by the end of 1st month, 2nd and 3rd months was tabulated and analyzed. The clinical improvement of a particular regimen (within the same group) before and after treatment was analyzed using paired t test. The improvement observed serially within the same group was evaluated using repeated measures ANOVA. Comparison between the two groups was done using unpaired t test.
3. Results
The study participants consisted of 31 males and 9 females, with a mean age of 32 yrs. Twenty percent of them were college students, 20% were unemployed/housewives, 25% were daily wage laborers and the rest were holding desk jobs. Eighty seven point five percent of the patients used commercially available gutkha products, while the rest 12.5% used either areca nut or gutkha depending on the availability. Only 2 patients reported the concomitant use of betel leaves along with areca nut occasionally. The quid was placed in the right or left lower buccal vestibule for more than half an hour by 85%, while the rest used it for a duration of 5–10 min. None of them had a habit of swallowing the contents. The average frequency per day and total duration of gutkha/areca nut chewing were 4.5 times and 5.4 years respectively. None of them had reported the concomitant use of smoking or alcohol.
The clinical sites of involvement were labial mucosa, buccal mucosa, soft palate, floor of the mouth, retromolar area and tongue. All the study participants had multiple areas of involvement. Buccal mucosa was involved in all the cases, followed by soft palate in 60%, tongue & floor of the mouth in 20% of the cases, retromolar area in 55% of cases. Eighteen patients had clinical grading of Grade II (early cases) and 22 had Grade III (moderately advanced). Fibrous bands were palpable in the buccal mucosa, labial mucosa in 25 and 9 patients respectively.
The mean values of burning sensation, interincisal distance and tongue protrusion were 100%, 23.4 mm and 18.7 mm respectively. The comparison of baseline profiles between the groups is not statistically significant as shown in Table 1. This indicates that the patients included in both groups had similar clinical profiles.
Table 1.
Comparison between the clinical profile of two groups.
| Parameter | Units | Group 1(Conventional)a | Group 2 (Turmix)a | P value |
|---|---|---|---|---|
| Age | years | 40.8 (14.9) | 37.9 (10.5) | 0.5203 |
| Sex M:F | 16:4 | 15:5 | 0.7050 | |
| Burning sensation improvement baseline | 0 | 0 | – | |
| IID baseline | mm | 22.4 (4.3) | 24.5 (3.3) | 0.1153 |
| Tongue protrusion baseline | mm | 18.7 (2.5) | 18.7 (2.5) | 0.9999 |
Mean (SD).
All the study participants tolerated the treatment regimens well, without any side effects. All observed parameters improved with both the interventions. Burning sensation improved in both the groups at the end of 1st month (mean values of 22.4 & 63.5 in group 1 & 2 respectively), to the end of 3rd month (15.6 & 0 in groups 1 & 2 respectively). Complete resolution of burning sensation was noted with turmix. Reduction in burning sensation with turmix was statistically significant when compared with conventional therapy (P < 0.001).
The mean increase in IID was 3.13 mm and 1.25 mm respectively in groups 1 & 2. The IID improved in both the groups, with significant results at the end of first month as shown in Table 2. Tongue protrusion showed greater recovery at the end of 1st month in group 1 when compared with group 2 (P = 0.004). Mean increase in TP at the end of the study period was noted to be 2.56 mm and 0.38 mm in group 1 & 2 respectively.
Table 2.
Comparison between clinical improvement of the 2 groups.
| Stage | Burning sensation |
Interincisal distance |
Tongue protrusion |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | P value | Group 1 | Group 2 | P value | Group 1 | Group 2 | P value | |
| 1st month | 22.4 (8.7)a | 63.5 (24.7) | <0.0001 | 0.58 (0.79) | 0 (0) | 0.0046 | 1.52 (1.38) | 0.11 (0.5) | 0.0004 |
| 2nd month | 18.5 (10.4) | 36.5 (24.7) | 0.0096 | 1.1 (0.8) | 0.23 (0.66) | 0.0021 | 0 (0) | 0 (0) | – |
| 3rd month | 15.6 (11.2) | 0 (0) | <0.0001 | 1.5 (1) | 0.82 (1.1) | 0.0877 | 0.9 (0.9) | 0.23 (0.66) | 0.0195 |
| P* | 0.2516 | <0.0001 | 0.0295 | 0.0256 | 0.0006 | 0.3588 | |||
Mean (SD); P* - Repeated measures ANOVA.
When the clinical improvement was analyzed serially in group 1 & 2, burning sensation had improved completely and rapidly in group 2 when compared with group 1 (p < 0.0001). Similar sequential improvement of IID was observed with both modalities as shown in Table 2. No significant improvement of TP was observed with turmix, whereas it was maximal at the end of 1st month with conventional therapy (P = 0.0006).
4. Discussion
In our study, 31 were males and 9 were females. This male preponderance was in accordance with various studies. The higher male preponderance probably reflects their easier access to the abusive habits or less social restrictions.6,14 The majority of the study participants had used commercially available tobacco products probably due to the attractiveness of the multicolored packets, ease of availability or the influence of advertising campaigns of gutkha companies.4,5 Economic status or employability did not seem to affect the choice of product in our series as 85% of them used commercial products, even when 40% of them were either students or unemployed. The average duration of chewing was around 5.4 years, with a frequency of 4.5 per day.
Turmeric is non toxic and is extremely safe even at higher doses.11,12 This is in agreement with our study since none of the participants in our study reported with any side effects. Our study showed early, rapid and complete improvement of burning sensation with turmix. These findings are similar to those reported by Das DA et al.11 The maximum and minimum reduction in burning sensation with conventional therapy was 80% and 40% respectively, with a mean 15.6% residual burning sensation at the end of therapy. This could have been due to the improper diffusion of the drug to all sites of affected mucosa due to the local drug delivery system. The complete resolution of burning sensation in the turmix group could be due its anti-inflammatory properties. Curcumin modulates the inflammatory response by.
-
a)
Down-regulating the activity of cyclooxygenase-2 (COX-2), lipoxygenase, and inducible nitric oxide synthase (iNOS) enzymes.
-
b)
Inhibits the production of the inflammatory cytokines, tumor necrosis factor-alpha (TNF-alpha), interleukin (IL) −1, −2, −6, −8, and −12, monocyte chemoattractant protein (MCP), and migration inhibitory protein.12
In our study, group 2 (turmix) participants showed mild gradual improvement of interincisal distance and tongue protrusion towards the end of 3rd month. This infers that turmix could cause improvement of IID & TP when given for longer duration. Improvement in interincisal distance and tongue protrusion were higher with conventional therapy when compared with turmix. This difference could be due to the potent anti-inflammatory properties of steroid when compared with that of curcumin or the poor bioavailability of turmix with the existing dose and formulation. Previous studies have indicated poor absorption of curcumin leading to low systemic availability. The systemic availability can be improved by complexing curcumin to a phospholipid, since curcumin is lipid soluble.12,16 Manufacturing curcumin as a phospholipid preparation may improve its bioavailability. The exact reasons for better improvement of tongue protrusion in group 1, despite no injections given in the floor of the mouth or base of the tongue are unknown but may be at least partly attributed to increase in mouth opening in these patients.
Das DA et al reported a mean increase of 0.87 cm of mouth opening with turmeric oil and turmeric capsules in contrast to our finding of 1.25 mm with turmix. These differences could be attributed to the variation in the formulations, dosages or clinical profile of the patients included. Jurenka JS in his review, reported that same dose of different formulations may give rise to different mean serum curcumin concentrations, the reason being unclear. They had also reported that low doses resulted in lesser concentrations in serum.12 With turmix, the interincisal distance improved better than tongue protrusion in our study, probably due to the anti-inflammatory and antifibrinolytic activity of turmix.12,13 Das DA et al reported better response in tongue protrusion with turmeric oil than with systemic administration of turmeric.
None of the patients of groups 1 & 2 have deteriorated in their clinical condition. This in both groups could be due to the effective pharmacological action of the drugs used. Some trials have even reported the regression or stabilization of malignancies with the use of curcumin. The antioxidative and scavenger properties of curcumin, make it a very effective chemopreventive agent in the prevention of cancer.12,16
The strengths of our study include randomization of subjects into the 2 groups, similar clinical profile in both the groups, 100% follow-up for 3 months. The limitations of our study include small sample size, data from a single centre and lack of histopathological confirmation of improvement at the end of the study period.
Our study has certain implications which include the early use of turmix in OSMF patients to provide rapid symptomatic relief. In addition to its anti-inflammatory and anti-fibrolytic properties, it possesses excellent anti oxidant properties. Moreover, the non invasive nature of this therapy makes it attractive.11 Further long term, prospective, large scale studies with higher doses are required to confirm the findings of this preliminary report.
To conclude, turmix is beneficial and effective in the management of early OSMF.
Conflicts of interest
All authors have none to declare.
References
- 1.Pindborg J.J., Sirsat S.M. Oral submucous fibrosis. Oral Surg Oral Med Oral Path. 1966;22:764–779. doi: 10.1016/0030-4220(66)90367-7. [DOI] [PubMed] [Google Scholar]
- 2.Hazarey V.K., Erlewad D.M., Mundhe K.A., Ughade S.N. Oral submucous fibrosis: a study of 1000 cases from central India. J Oral Pathol Med. 2007;36:12–17. doi: 10.1111/j.1600-0714.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 3.Rajendran R. Oral submucous fibrosis. J Oral Maxillofac Pathol. 2003;7:1–4. doi: 10.4103/0973-029X.86678. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Nigam N.K., Aravinda K., Dhillon Manu, Gupta Siddharth, Reddy Satheesha, Srinivas Raju M. Prevalence of oral submucous fibrosis among habitual gutkha and areca nut chewers in Moradabad district. J Oral Biol Craniofacial Res. 2014;4(1):8–13. doi: 10.1016/j.jobcr.2013.10.005. http://dx.doi.org/10.1016/j.jobcr.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shahid R.A. Coming to America: betel nut and oral submucous fibrosis. JADA. 2010;141:423–428. doi: 10.14219/jada.archive.2010.0194. [DOI] [PubMed] [Google Scholar]
- 6.Thakur N, Keluskar V, Bagewadi A, Shetti A. Effectiveness of micronutrients and physiotherapy in the management of oral submucous fibrosis. IJCD; 12():101–105.
- 7.Tilakaratne W.M., Klinikowski M.F., Saku Takashi, Peters T.J. Oral submucous fibrosis: review on aetiology and pathogenesis. Oral Oncol. 2006;42:561–568. doi: 10.1016/j.oraloncology.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Babu S., Bhat R.V., Kumar P.U. A comparative clinicopathological study of oral sub mucous fibrosis in habitual chewers of pan masala and betel quid. Clin Toxicol. 1996;34:317–322. doi: 10.3109/15563659609013796. [DOI] [PubMed] [Google Scholar]
- 9.Karemore V.T., Karemore V.A. Etiopathogenesis and treatment strategies of Oral submucous fibrosis. JIAOMR. 2011;23:598–602. [Google Scholar]
- 10.Taneja L., Nagpal A., Vohra P., Arya V. Oral submucous fibrosis: an oral physician approach. J Innovative Dent. 2011;1 [Google Scholar]
- 11.Das D.A., Balan A., SreeLatha K.T. Comparative study of the efficacy of curcumin and turmeric oil as chemopreventive agents in oral submucous fibrosis: a clinical and histopatholgical evaluation. JIAOMR. 2010;22:88–92. [Google Scholar]
- 12.Jurenka J.S. Anti-inflammatory properties of curcumin, a Major constituent of curcuma longa: a review of preclinical and clinical research. Altern Med Rev. 2009;14:141–153. [PubMed] [Google Scholar]
- 13.Zhang S.S., Gong Z.J., Li W.H., Wang X., Ling T.Y. Antifibrotic effect of curcumin in TGF-β1-induced myofibroblasts from human oral mucosa. Asian Pac J Cancer Prev. 2012;13:289–294. doi: 10.7314/apjcp.2012.13.1.289. [DOI] [PubMed] [Google Scholar]
- 14.Aara A., Satishkumar G.P., Vani C., Venkat Reddy M., Sreekanth K., Ibrahim M. Comparative study of intralesional dexamethasone, hyaluronidase and oral pentoxifylline in patients with oral submucous fibrosis. Glob J Med Res. 2012;12:1–14. [Google Scholar]
- 15.Khanna J.N., Andrade N.N. Oral submucous fibrosis: a new concept in surgical management. Report of 100 cases. Int J Oral Maxillofac Surg. 1995;24:433–439. doi: 10.1016/s0901-5027(05)80473-4. [DOI] [PubMed] [Google Scholar]
- 16.Tuba A.K., Gulcin I. Antioxidant and radical scavenging properties of curcumin. Chem Biol Interact. 2008;174:21–31. doi: 10.1016/j.cbi.2008.05.003. [DOI] [PubMed] [Google Scholar]


