Abstract
Median raphe cysts are a rare, congenital entity. We present a case and review the literature in respect to a 35-year-old man with a non-visible, painless midline swelling in the anterior perineum initially thought to be a liposarcoma. Subsequent histopathological examination confirmed a median raphe cyst.
Background
Median raphe cysts are a rare congenital condition and, although eminently amenable to surgical excision, can cause concern to the patient as well as to the attending physician due to their clinical presentation and differential diagnoses. First described by Mermet1, the condition has occasionally appeared in journals and paediatric reference texts but not in adult urology textbooks despite its potential extension into the scrotal area.
Case presentation
A 35-year-old man presented with a 12-month history of a non-visible, albeit palpable midline painless swelling from the bottom of his scrotum and extending down into the perineum (figure 1). He had a normal voiding pattern and normal erections.
Figure 1.

Image of patient's perineum.
On examination, the penis and testicles were normal on palpation and there was no palpable inguinal lymphadenopathy. The patient had a mobile midline soft swelling that extended along the midline perineum and into the scrotal raphe.
Investigations
Ultrasonography demonstrated an isoechoic scrotal soft tissue mass with no internal vascularity on Doppler. A 3 T MRI (with gadolinium) of the pelvis was performed preoperatively to characterise the lesion (figure 2). A 6.4 cm×2.5 cm long soft tissue lesion was identified in the midline from the scrotum into the perineum. It had a very low signal on T2-weighted imaging with no appreciable enhancement with contrast. It had a well-defined surrounding capsule and was discrete to the testicle although it abutted the tunica vaginalis.
Figure 2.

MRI of the pelvis demonstrating fluid filled cyst in the anterior perineum (see black arrow).
Differential diagnosis
Owing to the rarity of the condition, other more common diagnoses were considered first. These included: Cowper gland cyst, steatocystoma, glomus tumour, dermoid cyst, urethral diverticulum, pilonidal disease, perianal polyp, haemorrhoids, sarcoma and other neoplastic conditions.
Treatment
The lesion was excised completely with a sheath of connective tissue around it through a midline incision in the perineum extending to the scrotum. At the time of surgery, it was easy to identify a plane that could be developed between the lesion and normal tissue (figure 3).
Figure 3.

Excised median raphe cyst.
Outcome and follow-up
The patient was seen 6 weeks later with complete resolution of his symptoms and no evidence of recurrence at 1 year.
Discussion
Median raphe cysts are rare and, despite the involvement of the external genitalia, their description is primarily limited to case reports, small series, and paediatric and dermatology reference texts. Although other terms have been used, such as ‘mucoid cyst’, ‘genitoperineal cyst’, ‘hydrocystadenoma’, ‘apocrine cystadenoma’ and ‘urethroid cyst’, they have been reclassified as median raphe cysts due to the similar clinical and histologic characteristics.2
The diagnosis relies on clinical radiological and pathological examination. Although present in childhood they often remain undiagnosed until adolescence or adulthood due to their indolent nature. More often than not the cyst is asymptomatic, although presentations of infection, difficulty in voiding, haematuria, haematospermia, ulceration, sexual dysfunction and cosmetic effects have been reported in up to 27% of cases.3 4 Although predominantly found along the penile shaft, they can occur anywhere along the midline from the tip of the penis and rarely at the margin of the anus.3 5 6
Imaging in these cases can help identify the anatomy and point towards the diagnosis. Use of ultrasound, CT and MRI has been described.7–9 In one case, MRI and CT identified a cystic tumour, which was confirmed at histology to be a benign median raphe cyst.7
There have been three recognised patterns of histopathology including the most common urethral type (resembling epithelium of the male urethra), epidermis type (squamous epithelium) and mixed.2 10 Consequently, it was felt that the histopathological findings were related to the embryonic origin and median raphe cysts were a consequence of ‘tissue trapping’ during the fusion of the urethral folds or outgrowths of the epithelium after closure.11–13 Other histological variants including a glandular type and a ciliated form have been described, although these have been limited to case reports.3 5 14 In this case, pathological examination of the associated cyst demonstrated mixed type with squamoid and pseudostratified columnar epithelium with eosinophilic secretions (figures 4–6).
Figure 4.
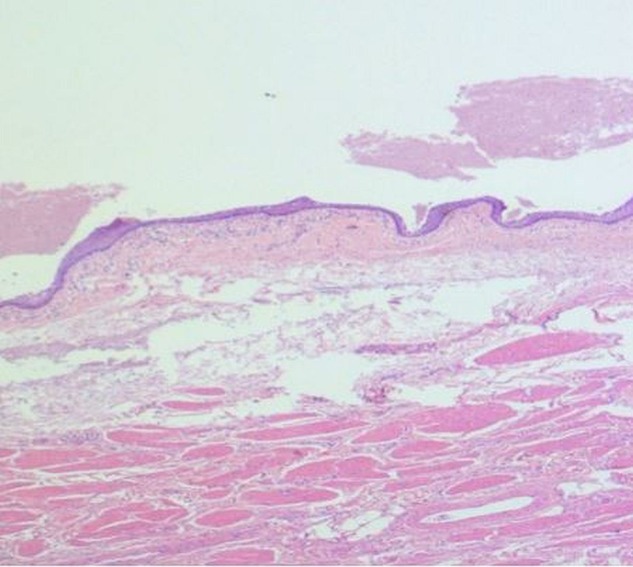
H&E stain of cyst demonstrating epithelial lining containing epithelial secretions.
Figure 5.
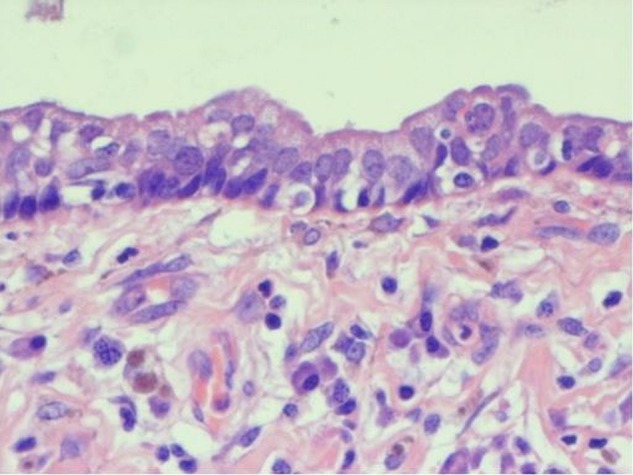
H&E stain of cyst lining demonstrating pseudostratified columnar epithelium.
Figure 6.

H&E stain of cyst lining demonstrating squamoid epithelial lining.
Treatment for median raphe cysts centres on surgical excision and primary closure where there is diagnostic doubt or patients are symptomatic. Although this is a benign condition, recurrences have been described, although it is worth noting that our case was with a patient who was managed by aspiration of the cyst rather than excision.10 Conservative management could be considered for small asymptomatic lesions. Spontaneous regression has been described once.15
Learning points.
Median raphe cysts are rare.
Swelling can occur anywhere along the median raphe from anus to scrotum.
Median raphe cysts can be classified into three separate histological types.
Although diagnosis is predominantly clinical, preoperative MRI (or ultrasound scan in the paediatric population) may help in aiding diagnosis and in identifying anatomical relationships prior to surgery.
Excision is an effective strategy in symptomatic patients.
Footnotes
Contributors: ASP wrote and submitted the manuscript. AF and AK provided the images and reviewed the manuscript. AM provided the clinical data, contributed to the writing of the manuscript and reviewed the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mermet P. Congenital cysts of the genitoperineal raphe. Rev Chir 1895;15:382–435. [Google Scholar]
- 2.Navarro HP, Lopez PC, Ruiz JM et al. Median raphe cyst. Report of two cases and literature review. Arch Esp Urol 2009;62:585–9. [PubMed] [Google Scholar]
- 3.Shao IH, Chen TD, Shao HT et al. Male median raphe cysts: serial retrospective analysis and histopathological classification. Diagn Pathol 2012; 7:121 10.1186/1746-1596-7-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menendez Lopez V, Funez R, Osman Agha G et al. [Cysts of median raphe]. Actas Urol Esp 1997;21:800–2. [PubMed] [Google Scholar]
- 5.Sagar J, Sagar B, Patel AF et al. Ciliated median raphe cyst of perineum presenting as perianal polyp: a case report with immunohistochemical study, review of literature, and pathogenesis. ScientificWorldJournal 2006;6:2339–44. 10.1100/tsw.2006.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Golitz LE, Robin M. Median raphe canals of the penis. Cutis 1981;27: 170–2. [PubMed] [Google Scholar]
- 7.Takano Y, Yokokawa K, Namiki M et al. Perineal epidermal cyst. Urol Int 1994;53:53–5. 10.1159/000282634 [DOI] [PubMed] [Google Scholar]
- 8.Sadler BT, Greenfield SP, Wan J et al. Intrascrotal epidermoid cyst with extension into the pelvis. J Urol 1995;153:1265–6. 10.1016/S0022-5347(01)67583-9 [DOI] [PubMed] [Google Scholar]
- 9.Ohyama C, Tochigi T, Kuwahara M et al. Intrascrotal epidermoid cyst: report of two cases. Int J Urol 1996;3:245–7. 10.1111/j.1442-2042.1996.tb00527.x [DOI] [PubMed] [Google Scholar]
- 10.Otsuka T, Ueda Y, Terauchi M et al. Median raphe (parameatal) cysts of the penis. J Urol 1998;159:1918–20. 10.1016/S0022-5347(01)63196-3 [DOI] [PubMed] [Google Scholar]
- 11.Nagore E, Sanchez-Motilla JM, Febrer MI et al. Median raphe cysts of the penis: a report of five cases. Pediatr Dermatol 1998;15:191–3. 10.1046/j.1525-1470.1998.1998015191.x [DOI] [PubMed] [Google Scholar]
- 12.Asarch RG, Golitz LE, Sausker WF et al. Median raphe cysts of the penis. Arch Dermatol 1979;115:1084–6. 10.1001/archderm.1979.04010090034019 [DOI] [PubMed] [Google Scholar]
- 13.Cole LA, Helwig EB. Mucoid cysts of the penile skin. J Urol 1976;115:397–400. [DOI] [PubMed] [Google Scholar]
- 14.Dini M, Baroni G, Colafranceschi M. Median raphe cyst of the penis: a report of two cases with immunohistochemical investigation. Am J Dermatopathol 2001;23:320–4. 10.1097/00000372-200108000-00008 [DOI] [PubMed] [Google Scholar]
- 15.Shibagaki N, Ohtake N, Furue M. Spontaneous regression of congenital multiple median raphe cysts of the raphe scroti. Br J Dermatol 1996;134: 376–8. 10.1111/j.1365-2133.1996.tb07640.x [DOI] [PubMed] [Google Scholar]


