Abstract
Purpose
Injection of mitomycin C may increase the success of transurethral incision of the bladder neck for the treatment of bladder neck contracture. We evaluated the efficacy of mitomycin C injection across multiple institutions.
Materials and Methods
Data on all patients who underwent transurethral incision of the bladder neck with mitomycin C from 2009 to 2014 were retrospectively reviewed from 6 centers in the TURNS. Patients with at least 3 months of cystoscopic followup were included in the analysis.
Results
A total of 66 patients underwent transurethral incision of the bladder neck with mitomycin C and 55 meeting the study inclusion criteria were analyzed. Mean ± SD patient age was 64 ± 7.6 years. Dilation or prior transurethral incision of the bladder neck failed in 80% (44 of 55) of patients. Overall 58% (32 of 55) of patients achieved resolution of bladder neck contracture after 1 transurethral incision of the bladder neck with mitomycin C at a median followup of 9.2 months (IQR 11.7). There were 23 patients who had recurrence at a median of 3.7 months (IQR 4.2), 15 who underwent repeat transurethral incision of the bladder neck with mitomycin C and 9 of 15 (60%) who were free of another recurrence at a median of 8.6 months (IQR 8.8), for an overall success rate of 75% (41 of 55). Incision with electrocautery (Collins knife) was predictive of success compared with cold knife incision (63% vs 50%, p=0.03). Four patients experienced serious adverse events related to mitomycin C and 3 needed or are planning cystectomy.
Conclusions
The efficacy of intralesional injection of mitomycin C at transurethral incision of the bladder neck was lower than previously reported and was associated with a 7% rate of serious adverse events.
Keywords: contracture, urinary bladder neck obstruction, urinary incontinence, mitomycin, administration and dosage
Bladder neck contracture is a well described complication after radical prostatectomy and transurethral resection of the prostate with a reported incidence ranging from 4.1% to 16%.1–8 Transurethral incision of the bladder neck has been established as a successful first line treatment.9–11 However, in some patients BNC recurs rapidly and is resistant to further therapy, leaving open bladder neck reconstruction as the only option to restore lower urinary tract patency. Open bladder neck reconstruction is technically complex and associated with a high morbidity. Therefore, it is rarely attempted outside of tertiary medical centers, leaving many patients with recurrent BNC dependent on self-catheterization regimens, suprapubic cystotomy or urinary diversion, which are morbid and burdensome treatments. Several techniques have been suggested to augment TUIBN and prevent BNC recurrence in refractory cases. The treatment options studied include holmium laser incision followed by injection of triamcinolone and, more recently, incision followed by injection of the antiproliferative agent mitomycin C.12,13 Both studies reported low rates of recurrence and a good safety profile. However, they were limited by their small sample sizes.
Several study centers in the TURNS began using MMC in 2009 due to early reports of its success in patients with treatment refractory BNC and the potential benefit of offering a much less morbid treatment to patients compared to bladder neck reconstruction. We evaluated the efficacy and safety of intralesional injection of MMC in our multiinstitutional cohort.
MATERIALS AND METHODS
After institutional review board approval was obtained at each institution, a retrospective review of all consecutive patients who underwent TUIBN with injection of MMC from December 2009 through November 2013 was conducted at participating centers in the TURNS. The TURNS includes Baylor, Loyola and Ohio State University, and the Universities of Iowa, Kansas, Minnesota, Utah and Washington. Patients were included in the analysis if they had cystoscopy at least 3 months after MMC injection or if recurrence was detected by cystoscopy earlier than 3 months. Standard data collection at each institution included prior treatments for BNC, operative details, MMC concentration used, total amount of MMC injected, complication data and results of followup cystoscopic examination.
Operative Technique
Surgical technique varied slightly by institution, but generally included 3 or 4 deep incisions into the bladder neck contracture until fat was seen. Incisions were made with a cold knife or electrocautery (Collins knife). MMC was injected into each wound bed at doses ranging from 0.4 to 10 mg and concentrations ranging from 0.1 to 1 mg/ml at the discretion of the treating surgeon. A Foley catheter was left in place postoperatively for approximately 1 week.
Statistical Methods
The primary outcome was recurrence of BNC, defined as the inability to atraumatically pass an adult flexible cystoscope (approximately 16Fr) through the bladder neck into the bladder. Followup time and time to recurrence, for those in whom therapy failed, were calculated from the date of surgery to the last reported cystoscopic assessment.
Univariate analyses of predictors including demographic factors (age, prior radiation, BNC etiology and number of prior endoscopic procedures or dilations) and surgical variables (MMC dose, MMC concentration, incision type and postoperative catheter size) were restricted to the first treatment with MMC. The rationale was that focusing on the first treatment would yield greater power than a composite outcome of two failures (or focusing on only the second case of failure), and that the potential for treatment and patient health differences between the initial and the followup procedures would complicate interpretation of the results in a combined analysis. Finally, the relatively small sample size derived from the 6 contributing institutions also complicated the application of more sophisticated statistical methods. Odds of TUIBN success after the first MMC treatment were analyzed for each predictor using Firth’s penalized likelihood logistic regression implemented in the logistf package in R v.2.15.3 (http://cran.us.r-project.org/) to overcome the sparsity introduced by institutional strata.14,15 Odds ratios and 95% CIs were reported along with 2-tailed p values. The Kaplan-Meier method was used to plot the success of TUIBN+MMC over time.
RESULTS
Demographics
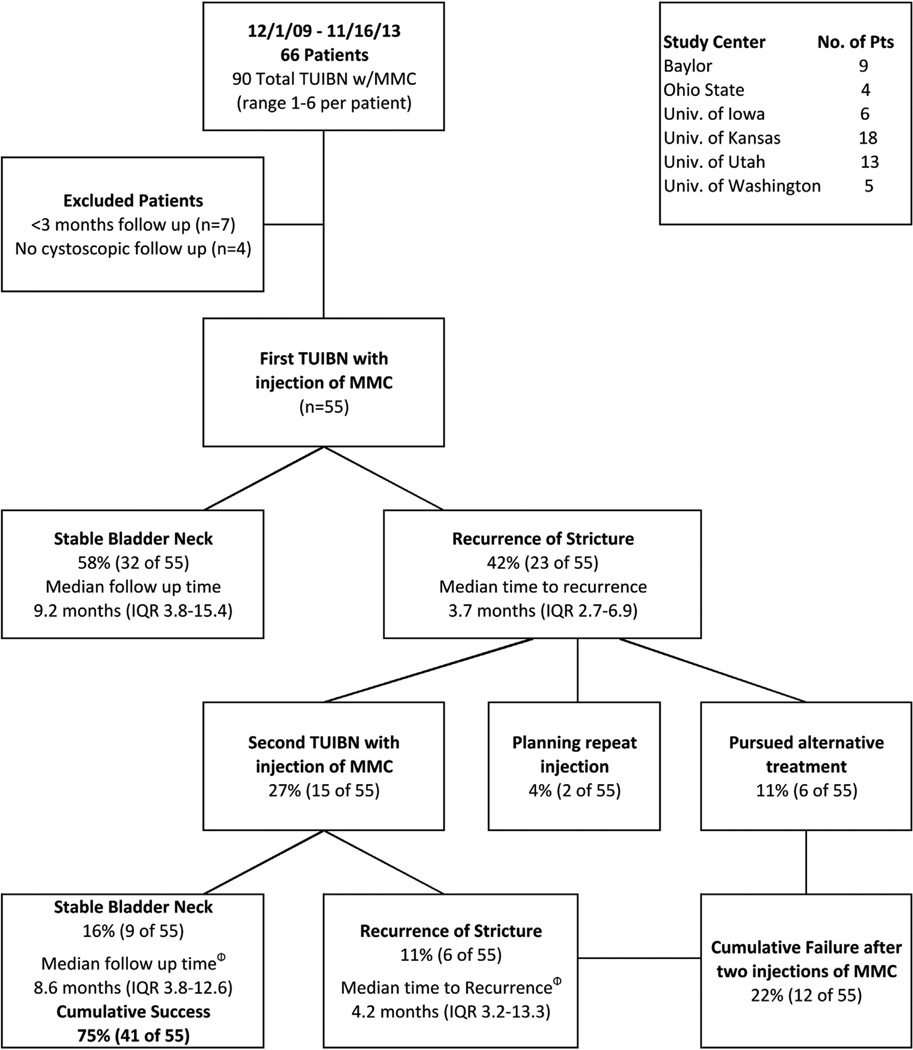
A total of 66 patients underwent TUIBN+MMC at various TURNS sites during the study period and 55 meeting the study inclusion criteria were included in the analysis (fig. 1). Of the 11 patients not meeting the study criteria 7 underwent cystoscopic assessment before 3 months postoperatively and have not undergone subsequent cystoscopy, and 4 were never evaluated cystoscopically. Mean patient age was 64.4 years (SD 7.6). The etiology of BNC is shown in table 1. Dilations or prior TUIBN had failed in the majority of patients (80%, 44 of 55) and 2 or more TUIBNs had failed in 47% (26 of 55). A history of pelvic radiation therapy for prostate cancer was present in 25% of the patients (14 of 55). An artificial urinary sphincter was placed in 45% (25 of 55) after achieving a stable bladder neck.
Figure 1.
Study population. Phi indicates recurrence and followup calculated from date of second injection.
Table 1.
Characteristics of study population
| No. BNC etiology: | ||
| Retropubic prostatectomy | 25 | |
| Transurethral resection of prostate | 12 | |
| Robotic prostatectomy | 8 | |
| Radical cystectomy + neobladder | 5 | |
| Radiotherapy for prostate Ca | 2 | |
| Proton beam therapy for prostate Ca | 1 | |
| Simple prostatectomy | 1 | |
| Pelvic fracture + urethral distraction defect | 1 | |
| No. prior radiation therapy (%) | 14 | (25) |
| No. failed prior treatment for BNC (%) | 44 | (80) |
| Median prior bladder neck releases (range) | 1 | (0–8) |
| Median prior dilations (range)* | 1 | (0–5) |
| No. surgical technique: | ||
| Cold knife incision | 30 | |
| Collins knife + electrocautery | 16 | |
| Transurethral resection of scarred tissue | 9 | |
| No. posttreatment artifical urethral sphincter placement (%) | 25 (45) |
Number of prior dilations unknown in 13 patients.
Surgical Outcomes
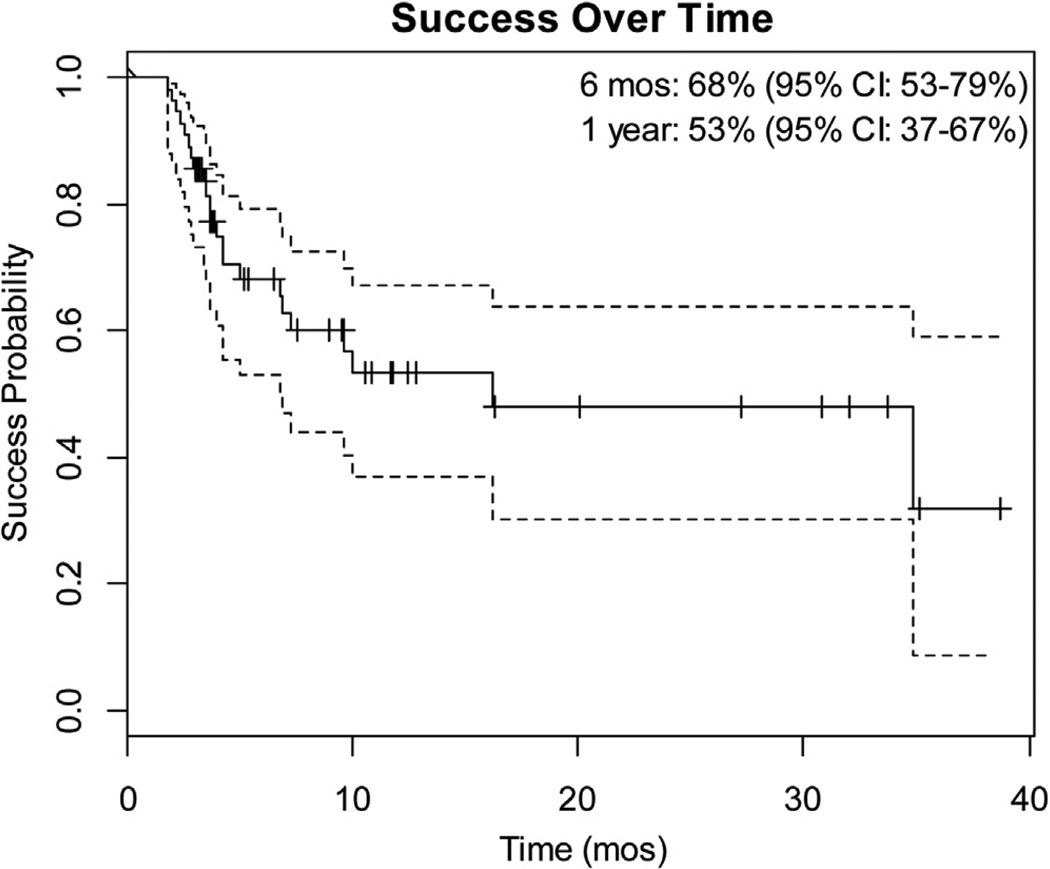
A combined total of 78 TUIBN+MMC procedures (range 1 to 6 per patient) were performed with an overall success rate of 55.1% when each injection was considered independently. This resulted in a stable bladder neck in 58% of patients after a single treatment at a median followup of 9.2 months (IQR 3.8–15.4). Recurrence was observed in 23 patients (42%) after the first injection of MMC with a median time to contracture recurrence of 3.7 months postoperatively (IQR 2.7–6.9). Success over time is shown in the Kaplan-Meier plot (fig. 2). Of the patients who underwent a second injection with MMC 60% (9 of 15) had a stable bladder neck at a median followup of 8.6 months (IQR 3.8–12.6). In those in whom treatment failed after a second MMC injection, contracture recurred at a median of 4.2 months, resulting in an overall success rate of 75% after 2 procedures. Five patients pursued a third TUIBN+MMC, which was successful in 2 (40%), and 1 patient underwent 6 injections unsuccessfully.
Figure 2.
Kaplan-Meier plot showing failures over time. Short vertical lines indicate censored data.
Of the 8 patients in whom primary TUIBN+MMC failed and who did not have a second TUIBN+MMC, 2 are planning on undergoing repeat injection in the near future. Definitive management in the remaining 6 patients included cystectomy and urinary diversion (2), open bladder neck reconstruction (1), repeat direct visual internal urethrotomy without MMC (2) and intermittent catheterization to keep the contracture open (1).
The mean dose of MMC injected for the first treatment in cases that achieved a stable bladder neck was 3.5 mg (range 0.4 to 10) vs 3.8 mg (range 1 to 10) in those cases of treatment failure (p=0.97). Mean concentration was also not predictive of success of the procedure (table 2).
Table 2.
Univariate analysis of study population controlling for source institution
| TUIBN Success | TUIBN Failure | OR (95% CI) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Mean pt age (SD) | 65.3 | (7.6) | 63.1 | (7.6) | 1.1 | (1–1.2) | 0.17 |
| No. prior radiation (%): | |||||||
| Yes | 9 | (64) | 5 | (36) | |||
| No | 23 | (56) | 18 | (44) | 0.5 | (0.1–2.1) | 0.36 |
| No. radical retropubic prostatectomy (%): | |||||||
| Yes | 14 | (56) | 11 | (44) | |||
| No | 18 | (60) | 12 | (40) | 1 | (0.3–3.2) | 0.99 |
| No. prior TUIBN (%): | |||||||
| 2 or Greater | 15 | (58) | 11 | (42) | |||
| Less than 2 | 17 | (58.6) | 12 | (41) | 1.4 | (0.5–4.4) | 0.54 |
| Mean mg total dose (SD) | 3.53 (2.1) | 3.84 (2.4) | 0.99 | (0.6–1.5) | 0.97 | ||
| Mean mg/ml concentration (SD) | 0.62 (0.3) | 0.76 (0.3) | 0.05 | (0–2.3) | 0.14 | ||
| No. technique (%): | |||||||
| Cold knife | 15 | (50) | 15 | (50) | Ref | ||
| Hot knife | 10 | (63) | 6 | (38) | 10.7 (1.2–197.0) | 0.03 | |
| Transurethral resection of prostate | 7 | (78) | 2 | (22) | 1.84 (0.2–29.2) | 0.62 | |
| No. catheter size (%):* | |||||||
| 18Fr or less | 21 | (78) | 6 | (22) | |||
| Greater than 18Fr | 10 | (53) | 9 | (47) | 0.44 (0.03–6.4) | 0.51 | |
Catheter size unavailable for 9 patients.
Surgical technique varied, and included cold knife incision, Collins knife incision with electrocautery and transurethral resection of the scarred tissue (table 1). When comparing surgical techniques, TUIBN with electrocautery (Collins knife) had a success rate of 63% vs 50% for cold knife TUIBN (p=0.03, table 2). Patient age, prior radiation treatment, BNC etiology (radical retropubic prostatectomy vs other etiology), number of prior TUIBNs and the size of the catheter left postoperatively were not predictive of success (table 2).
Adverse Events
Four (7%) patients experienced serious adverse events related to TUIBN+MMC. Osteitis pubis after MMC injection developed in 2 patients, presenting 8 weeks and 3 weeks, respectively, after injection. In both patients BNC recurred rapidly and was much more extensive, and both patients were eventually treated with cystectomy and continent cutaneous diversion for definitive management. Rectourethral fistula and necrosis of the bladder floor developed in a third patient at 3 months after TUIBN+MMC. He underwent fecal diversion, and is awaiting cystectomy, urinary diversion and fistula closure. Common to all 3 of these patients was a history of radiation therapy for prostate cancer. The fourth patient had extensive necrosis of the bladder neck extending to the bladder floor and trigone, as well as prolonged bladder pain. This complication was recognized on followup cystoscopy at 2 months. The patient had healed without further intervention at 6 months with resolution of pain. The total dose of MMC in these patients was 2 to 4.5 mg, and in 3 patients and in 1 the hot and cold knife was used for TUIBN, respectively. No patient in our database experienced any known systemic side effects attributable to MMC.
DISCUSSION
Recurrent BNC is rare in patients after prostatectomy or transurethral resection of the prostate. When BNC is resistant to conventional treatments, it becomes a long-term issue and patients often endure numerous repeat procedures with a lower chance of long-term success with each subsequent attempt. Significant morbidity and a reduction in quality of life occur as a result.4
Minimally invasive therapies such as transurethral incision of the fibrous bladder neck offer a quicker recovery with less morbidity than open reconstruction of the bladder neck. However, its efficacy in refractory cases10 has been challenged and, consequently, several centers have advocated for the use of adjuvant immune modulating agents such as steroids or MMC at TUIBN in an attempt to inhibit scar reformation at the bladder neck.
Eltahawy et al reported on their experience in 24 patients primarily with recurrent BNC treated with deep lateral incisions using the holmium laser followed by injection of the steroid triamcinolone.12 The proposed mechanism of action with this technique is enhancement of endogenous local collagenase activity via steroid injection. The overall success rate at a mean followup of 24 months (range 6 to 72) was 83% after 2 incisions, although objective followup data were lacking.
Vanni et al reported their results using MMC in 18 patients with treatment refractory BNC.13 MMC has a long history of use in various fields due to its antiproliferative properties, which have been shown to inhibit fibroblasts and collagen deposition, thereby reducing subsequent scar formation.16,17 The overall success rate was 89% after 2 procedures (72% primary success rate) and 94% after an average of 1.35 (SD 0.79) incisions. Objective followup included cystoscopy at 3 months and then only selectively after that.
Recently the need for intralesional injection was challenged in a retrospective review of BNC management by Ramirez et al, who demonstrated excellent primary (72%) and overall (86%) success rates at 16 months after deep incisions with electrocautery (Collins knife) alone.18 However, in a similar study Brede et al demonstrated much lower success rates with a cold knife, with a primary success rate of 51% and only 70% overall.19 The only technical difference between the 2 studies was the mechanism of incision (ie electrocautery vs cold knife). Although it must be acknowledged that the primary outcome of our study was successful stabilization of the bladder neck and not a comparison of surgical techniques, incision with electrocautery was predictive of success in our study, in line with the contrasting observations from Ramirez18 and Brede19 et al.
Our initial (58%) and overall (78%) success rates after a mean of 1.3 injections (SD 0.56) are lower than those reported by Vanni et al,13 and are similar to or even lower (Ramirez et al18) than those of recent studies not using any adjuvant injectable agent, calling into question the usefulness of the injection. However, it is important to note that our strict definition of anatomical success by cystoscopy may have yielded lower success rates as we may have detected asymptomatic mild recurrence.
We did not find any patient or BNC characteristics that predicted success. Importantly, a history of radiation did not adversely affect outcomes. In patients with recurrence we found that it happened rapidly, at a median of 4.2 months (IQR 2.9–7.2), which was in line with many other BNC studies.9–11,13,18,19 Interestingly in patients with recurrence with more than 1 TUIBN with MMC, there was a slight increase in the time between recurrences (3.7 to 4.2 months), similar to the findings of Vanni et al.13
Adverse Events
There were 4 patients (7%) who experienced Clavien grade IIIb adverse events after TUIBN+MMC, of whom 3 ultimately required or are planning cystectomy and permanent urinary diversion. The exact mechanism of these complications is unknown. However, asymptomatic ulcerations after intravesical administration, perivesical fat necrosis on cystectomy specimens and massive necrosis after extravasation into subcutaneous tissues have all been described after administration of MMC for the treatment of bladder cancer.20–22 Radiation injury was present in 3 of the 4 patients and these complications may have arisen independent of MMC injection. However, this seems unlikely as extensive necrosis is not typically seen in TUIBN. We presume that these events resulted from a dose that was too high (3 of 4 patients received 4 mg or more) or inadvertent extravesical administration, and have modified our practice to limit the dose to 2 mg at a concentration no greater than 0.4 mg/ml. We also now restrict the use of MMC to patients with treatment resistant strictures in whom prior dilation or incision without MMC failed.
Limitations
The results of this study should be interpreted cautiously, similar to any retrospective cohort study with a relatively small sample size. Our lack of a control group significantly limits our ability to make conclusions about the efficacy of MMC as we are forced to compare our success to the success witnessed in other studies that have similarly small or smaller sample sizes. The lack of a single technique (ie cold knife, hot knife etc) is an additional source of bias when interpreting our results. Followup regimens differ significantly among studies and symptomatic results are not necessarily comparable to cystoscopic examination of recurrent BNC. Prospective trials comparing MMC injection to incision alone using a standardized followup are needed to fully elucidate the effect, if any, that MMC has on long-term bladder neck patency. In addition, we did not evaluate numerous factors previously associated with recurrent disease such as a history of smoking, body mass index and medical comorbidities.
CONCLUSIONS
In a multi-institutional cohort the efficacy of intralesional injection of MMC at TUIBN is similar to the success rates reported for deep lateral incision alone, suggesting that technique, in particular deep incision down to the perivesical fat, may have more of a role than adjuvant agents in establishing long-term patency. This is also the first study, to our knowledge, to document serious adverse events related to the use of MMC during TUIBN and to question its safety as an adjuvant agent. Given these adverse events and a lower efficacy than initially reported, prospective controlled studies are needed to determine the efficacy and safety of TUIBN+MMC before its widespread adoption.
Acknowledgments
Supported by an educational grant in reconstructive urology from American Medical Systems, Inc., Minnetonka, Minnesota, and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through Grant 8UL1TR000105 (formerly UL1RR025764). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Study received institutional review board approval.
Abbreviations and Acronyms
- BNC
bladder neck contracture
- MMC
mitomycin C
- TUIBN
transurethral incision of the bladder neck
- TURNS
Trauma and Urologic Reconstruction Network of Surgeons
Footnotes
Financial interest and/or other relationship with American Medical Systems.
Financial interest and/or other relationship with American Medical Systems, Coloplast and Auxilium.
REFERENCES
- 1.Sandhu JS, Gotto GT, Herran LA, et al. Age, obesity, medical comorbidities and surgical technique are predictive of symptomatic anastomotic strictures after contemporary radical prostatectomy. J Urol. 2011;185:2148. doi: 10.1016/j.juro.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Elliott SP, Meng MV, Elkin EP, et al. Incidence of urethral stricture after primary treatment for prostate cancer: data from CaPSURE. J Urol. 2007;178:529. doi: 10.1016/j.juro.2007.03.126. [DOI] [PubMed] [Google Scholar]
- 3.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 4.Wang R, Wood DP, Hollenbeck BK, et al. Risk factors and quality of life for post-prostatectomy vesicourethral anastomotic stenoses. Urology. 2012;79:449. doi: 10.1016/j.urology.2011.07.1383. [DOI] [PubMed] [Google Scholar]
- 5.Kim HS, Cho MC, Ku JH, et al. The efficacy and safety of photoselective vaporization of the prostate with a potassium-titanyl-phosphate laser for symptomatic benign prostatic hyperplasia according to prostate size: 2-year surgical outcomes. Korean J Urol. 2010;51:330. doi: 10.4111/kju.2010.51.5.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee YH, Chiu AW, Huang JK. Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology. 2005;65:498. doi: 10.1016/j.urology.2004.10.082. [DOI] [PubMed] [Google Scholar]
- 7.Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283:354. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 8.Erickson BA, Meeks JJ, Roehl KA, et al. Bladder neck contracture after retropubic radical prostatectomy: incidence and risk factors from a large single-surgeon experience. BJU Int. 2009;104:1615. doi: 10.1111/j.1464-410X.2009.08700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pansadoro V, Emiliozzi P. Iatrogenic prostatic urethral strictures: classification and endoscopic treatment. Urology. 1999;53:784. doi: 10.1016/s0090-4295(98)00620-7. [DOI] [PubMed] [Google Scholar]
- 10.Giannarini G, Manassero F, Mogorovich A, et al. Cold-knife incision of anastomotic strictures after radical retropubic prostatectomy with bladder neck preservation: efficacy and impact on urinary continence status. Eur Urol. 2008;54:647. doi: 10.1016/j.eururo.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Yurkanin JP, Dalkin BL, Cui H. Evaluation of cold knife urethrotomy for the treatment of anastomotic stricture after radical retropubic prostatectomy. J Urol. 2001;165:1545. [PubMed] [Google Scholar]
- 12.Eltahawy E, Gur U, Virasoro R, et al. Management of recurrent anastomotic stenosis following radical prostatectomy using holmium laser and steroid injection. BJU Int. 2008;102:796. doi: 10.1111/j.1464-410X.2008.07919.x. [DOI] [PubMed] [Google Scholar]
- 13.Vanni AJ, Zinman LN, Buckley JC. Radial urethrotomy and intralesional mitomycin C for the management of recurrent bladder neck contractures. J Urol. 2011;186:156. doi: 10.1016/j.juro.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 14.Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80:27. [Google Scholar]
- 15.Heinze G, Puhr R. Bias-reduced and separation-proof conditional logistic regression with small or sparse data sets. Stat Med. 2010;29:770. doi: 10.1002/sim.3794. [DOI] [PubMed] [Google Scholar]
- 16.Simman R, Alani H, Williams F. Effect of mitomycin C on keloid fibroblasts: an in vitro study. Ann Plast Surg. 2003;50:71. doi: 10.1097/00000637-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Ayyildiz A, Nuhoglu B, Gülerkaya B, et al. Effect of intraurethral mitomycin-C on healing and fibrosis in rats with experimentally induced urethral stricture. Int J Urol. 2004;11:1122. doi: 10.1111/j.1442-2042.2004.00959.x. [DOI] [PubMed] [Google Scholar]
- 18.Ramirez D, Zhao LC, Bagrodia A, et al. Deep lateral transurethral incisions for recurrent bladder neck contracture: promising 5-year experience using a standardized approach. Urology. 2013;82:1430. doi: 10.1016/j.urology.2013.08.018. [DOI] [PubMed] [Google Scholar]
- 19.Brede C, Angermeier K, Wood H. Continence outcomes after treatment of recalcitrant postprostatectomy bladder neck contracture and review of the literature. Urology. 2014;83:648. doi: 10.1016/j.urology.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 20.Cliff AM, Romaniuk CS, Parr NJ. Perivesical inflammation after early mitomycin C instillation. BJU Int. 2000;85:556. doi: 10.1046/j.1464-410x.2000.00539.x. [DOI] [PubMed] [Google Scholar]
- 21.Doherty AP, Trendell-Smith N, Stirling R, et al. Perivesical fat necrosis after adjuvant intravesical chemotherapy. BJU Int. 1999;83:420. doi: 10.1046/j.1464-410x.1999.00951.x. [DOI] [PubMed] [Google Scholar]
- 22.Barr RD, Benton SG, Belbeck LW. Soft-tissue necrosis induced by extravasated cancer chemotherapeutic agents. J Natl Cancer Inst. 1981;66:1129. doi: 10.1093/jnci/66.6.1129. [DOI] [PubMed] [Google Scholar]