Abstract
Background: To evaluate the necessity of using nasogastric tube (NGT) for patients undergoing radical cystectomy with urinary diversion. Methods: Literature was searched from PubMed, EMBASE, and Cochrane Library. We identified randomized controlled trials, Cohort study, and Case-control analysis that compared the individuals with or without nasogastric tube after radical cystectomy with urinary diversion. We performed the meta-analysis to evaluate the role of nasogastric tube in decompression after radical cystectomy with urinary diversion. Result: Two randomized controlled trial and four Cohort studies (780 patients) fulfilled the inclusion criteria. There was significant difference between the time (days) commencement of a liquid diet and the development of bowel sounds in patients without nasogastric tube than those with NGT (nasogastric tube) [P < 0.0001, standard mean difference (SMD) = -0.35, 95% CI -0.52 to -0.18; P < 0.00001, SMD = -0.43, 95% CI -0.60 to 0.26, respectively]. Additionally, there was no significant differences in pulmonary complications and wound complication [P = 0.25, odds ratio (OR) = 0.60 95% CI 0.25 to 1.43; P = 0.66 OR = 1.16 95% CI 0.60 to 2.25, respectively]. But the differences were significant in the paralytic ileus or bowel obstruction (P = 0.010, OR = 0.60, 95% CI 0.41 to 0.88) after surgery. Furthermore, the difference of the duration of hospital stay (days) between the NGT group and Without NGT group (P = 0.0005, SMD = -0.30, 95% CI -0.47 to -0.13). Conclusion: It cannot shorten the time of gastrointestinal function recovery or reduce the incidence of complications after radical cystectomy by using the nasogastric tube routinely. Routinely use of nasogastric tube after radical cystectomy with urinary diversion was not recommended.
Keywords: Nasogastric tube, gastrointestinal decompression, radical cystectomy with urinary diversion, meta-analysis
Introduction
At present, while radical cystectomy with urinary diversion still remains the golden standard operation procedure for the patients with invasive bladder cancer, it is still associated with significant complications and mortality during the postoperation period [1-3]. In order to reduce the complication and mortality, perioperative care such as early removal of the nasogastric tube (NGT) after operation and improved surgical techniques have gained a lot of attention. Gastrointestinal decompression for people undergoing cystectomy with urinary diversion is commonly used nowadays in urology. However, this tradition has been questioned recently [4]. A lot of literatures both in general surgery and urology have proved that prolonged using of nasogastric tube is not necessary after abdominal surgery [5-9]. They hold the views that prolonged NGT inserted not only can not achieved the original goal which NGT can accelerate the gastrointestinal tract recovery and may result in more problems such as patients feel not comfortable or even has the potential risk to increase the incidence of pulmonary complications. But nowadays some urologist still overlooked these recommendations and continued to practice the NGT routinely perioperation. Thus whether necessary to insert nasogastric tube routinely after radical cystectomy with urinary diversion is still remained controversy. Therefore, the aim of this study was to conduct a meta-analysis to determine the necessity of nasogastric tube after radical cystectomy, to discuss whether the NGT inserted routinely can accelerate the gastrointestinal tract recovery and reduce the incidence of postoperation complication or not?
Materials and methods
Eligible criteria
We searched randomized controlled trials, cohort studies and case-control studies to compare the outcome of Without NGT to with NGT in the prevention of postoperative complication for people undergoing radical cystectomy with urinary diversion. Without NGT is defined as removing the NGT after operation immediately or within 24 hours. With NGT is defined as removing the NGT until the occurrence of the first flatus or the first bowel sound.
The primary outcome included the time of gastrointestinal tract recovery and the second outcome measures included postoperation complications such as paralytic ileus or bowel obstruction, pulmonary complication and wound complication, the length of hospital stay is also what we cared about.
Search strategy
We searched all literatures from the database of PubMed, EMBASE, and COCRANE LIBRARY since 1974 to September 2014. The search strategy was as follows (nasogastric decompression OR gastrointestinal decompression OR nasogastric tube) AND cystectomy.
Data extraction
Two researchers independently reviewed all the studies by extracting the abstracts, titles and research designs for every potential available article, then they confirmed the eligibility by retrieving and reviewing the full texts. Data were extracted according to endpoints and complications.
Statistical analysis
In the present meta-analysis, we used odds ratios (ORs) and its 95% confidence intervals (CIs) to express as Dichotomous outcomes. The OR value represents the ratio of an adverse event happening in the group Without NGT versus the group With NGT, and OR values less than 1 favor the group Without NGT. The point estimate of the OR value is considered statistically significant with P < 0.05 (and the 95% CI does not cross 1). The standardized mean difference (SMDs) was used for analysis of continuous variables. Similarly, there is no significant difference when the P > 0.05 or its 95% CI contains zero. And SMD values less than 0 favors the group Without NGT. We used the Chi-square test and I2 to evaluate the heterogeneity. It was considered statistically significant if P < 0.10 or I2 > 50%. All statistical analyses were performed using the Review Manager (RevMan) [Computer program]. Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Results
From the inclusion and exclusion criteria and the search strategy, a total of fifteen articles initially included in our study, after double blind reviewing by two investigators, finally there were six studies that included 780 patients (342 patients in the without NGT group and 438 patients in the with NGT group) were determined as appropriated to include into our research (Figure 1) [6,10-14]. Nine studies were excluded. The search inclusion and exclusion strategy are displayed in Figure 1. All studies compared the without NGT and with NGT, the characteristics of these studies are described in the Table 1.
Figure 1.
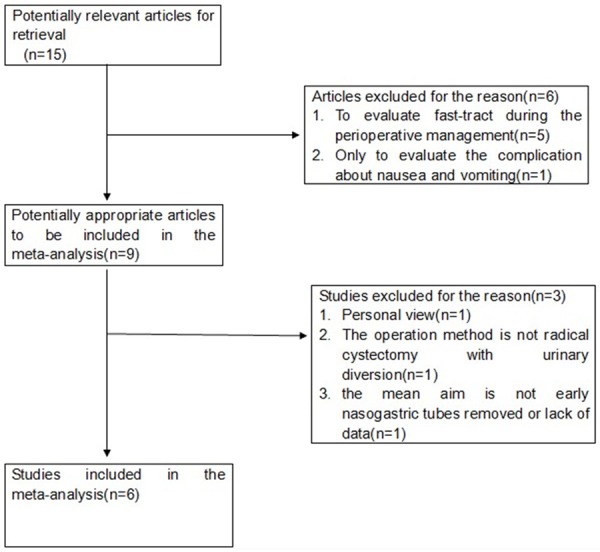
The strategy to select the potential studies.
Table 1.
Characteristics of trials included in the review and quality access
| Study | Methods | Prospective | Grouping (patients in Without NGT Vs. With NGT) | mean age (years) | Methods of Without NGT | Methods of With NGT |
|---|---|---|---|---|---|---|
| S.Machele 1999 | Cohort study | YES | 27 versus 54 | 66±8.7 vs. 65±9.3 | removed in the recovery room after extubation or the morning of postoperative day 1 (24 hours or less after surgery) | were not removed until the return of normal bowel sounds and the passage of flatus. |
| BRANTA. INMAN 2003 | Cohort study | NO | 199 versus 221 | 65.01 vs. 62.75 | Not referred | Not referred |
| HYOUNG KEUN PARK 2005 | Randomized | NO | 20 versus 81 | 65.4±8.8 vs. 60.5±12.2 | removed in the recovery room after extubation or the morning of postoperative day 1 (24 hours or less after surgery) | kept until the patient passed flatus |
| Ioannis 2011 | Randomized | YES | 22 versus 21 | 66.1±6.73 vs. 66.3±4.46 | removed 12 hours after the operation | remained in place until the appearance of the first flatus |
| Anap 2012 | Cohort study | NO | 23 versus 27 | 68.4 vs. 69.6 | Received first dose of avimopan (12 mg po) at least 1 hour prior to the induction of anesthesia and the nasogastric tube was removed at the time of extubation | Not received avimopan preoperatively, the nasogastric tube was removed based on bowel sound, flatus, and clinical status |
| R.R. de Vries 2012 | Cohort study | NO | 51 versus 34 | 66 vs. 59 | early enteral feeding via a postpyloric tube and direct removal of NGT | TPN by a central venous line and NGT removal after 24 h (the NGT remained in situ until first bowel movements, no nausea and a low NGT production) |
NGT, Nasogastric tube; TPN, Total Parenteral Nutrition.
Recovery of gastrointestinal tract function
The time for developing bowel sounds and the beginning of a liquid diet were examined in three studies, there was significant difference between the time commencement of a liquid diet and the development of bowel sounds in patients without NGT than those with NGT [P < 0.00001, SMD = -0.43, 95% CI -0.60 to -0.026; P < 0.001, SMD = -0.35, 95% CI -0.52 to -0.18, respectively (Figure 2A, 2B)]. In addition, three studies made to examine the length of hospital stay indicated obvious differences between group Without NGT and group With NGT [P = 0.005, SMD = -0.30, 95% CI -0.47 to -0.13 (Figure 2C)]. In the pooled data, the Without NGT group had a shorter time for the first bowel sound and the first liquid diet intake after radical cystectomy than the With NGT group. Similarly, aggregated study data showed that the length of hospital stay of Without NGT group also shorter than With NGT group.
Figure 2.
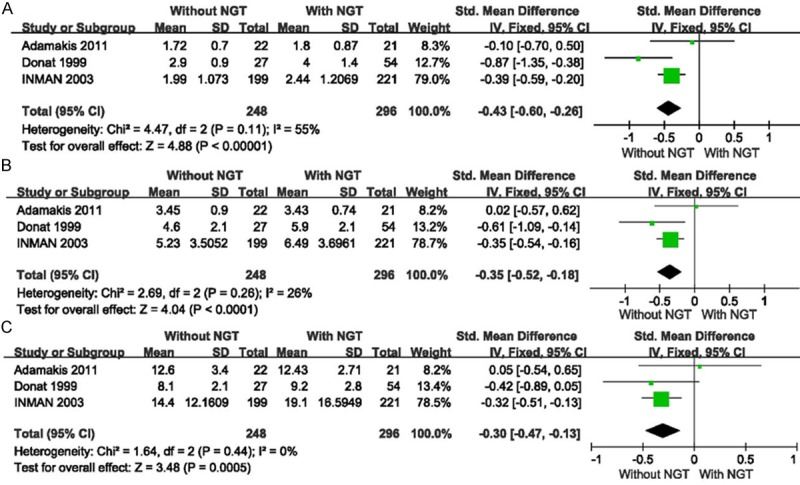
A: The time commencement of a liquid diet; B: The time of development to first bowel sound; C: The length of hospital stay.
Complications
Data on six studies examined the complications, included the incidence of postoperation ileus or small intestinal obstruction, pulmonary complications and wound complications. There was no considerable heterogeneity was found, thus the fixed effect model was used to aggregate the data on complications. The difference was significant between group without NGT and the group with NGT [P = 0.010, OR = 0.60, 95% CI 0.41 to 0.88 (Figure 3A)]. Meanwhile, there was no significant difference between the pulmonary and wound complication [P = 0.27, OR = 0.60 95% CI 0.25-1.43; P = 0.66, OR = 1.16, 95% CI 0.60-2.25; respectively (Figure 3B, 3C)].
Figure 3.
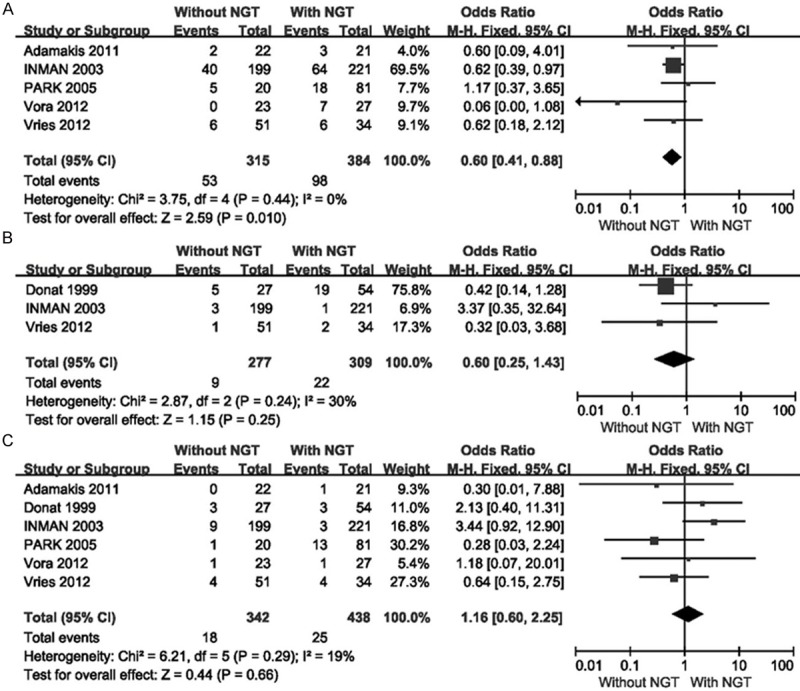
Complications: A: Postoperation ileus or small intestinal obstruction; B: Pulmonary complication; C: Wound complication.
Discussion
From the original of the fast track concept in abdominal surgery at the beginning of the 1990s, urologists have been successfully transplanted the fast track concept which can improve postoperative outcome and minimize morbidity in urology department [15-17]. One of the fast tract pathways is whether the nasogastric tube should be inserted routinely after radical cystectomy with urinary diversion. In recent years, many clinical studies and reviews demonstrated that routine nasogastric tube is unnecessary after radical cystectomy and even some emphasized that nasogastric tubes might have caused an increased incidence of complications [18]. In spite of these studies, some surgeons still continue to practice routine nasogastric tubes and hold the view that NGT can decrease the risk of postoperation complications. Therefore, the need of NGT after radical cystectomy with urinary diversion still remains controversial.
Can nasogastric tube accelerate the recovery of gastrointestinal tract function? Old conception considered that nasogastric tubes could accelerate the recovery of gastrointestinal tract function, but this conception has already been challenged by urologists based on contemporary advancement in medical technology. Clinically, the time of oral, bowel sound and the first flatus can indicate the speed of recovery of gastrointestinal function. But interestingly, our result showed that the patients without NGT after radical cystectomy with urinary diversion had a shorter time of first liquid diet intake and first bowel sound. Besides, Pruthi’s study [19] demonstrated that early institution of oral diet had a significant influence on early discharge or can result in a shorter length of hospital stay. The length of hospital stay was significantly shorter in group Without NGT than group use NGT routinely in our study (P = 0.005), and we believe the mean reason for the shorter length of hospital stay is the early oral diet and the earlier recovery of gastrointestinal tract function. Vora.’s study [13] indicated that Without NGT combine with a quaternary mu opioid receptor antagonist alvimopan for patients undergoing radical cystectomy with urinary diversion had a shorter hospital discharge (P = 0.047) and had a low incidences of prolonged ileus (0% vs. 25.9%, P = 0.012). In addition, William’s cost-effectiveness analysis [20] about alvimopan for prevention of postoperation paralytic ileus (POI) in radical cystectomy patients confirmed that alvimopan can reduce the incidence of POI and offered a saving cost during the hospital stay. Moreover, Donat and his colleagues [11] firstly conducted a prospective cohort study that combines a pro-kinetic agent metoclpramide with early nasogastric tube removal after cystectomy and urinary diversion, they had concluded that this pathway can speed the return of normal bowel function. But treatment with a prokinetic alone showed no differences in bowel recovery [21] and not reduce the incidence of the POI [3]. Our meta-analysis revealed that the use of NGT had not achieved accelerated time of gastrointestinal function (P = 0.010) and decreased length of hospital stay (P = 0.005).
The NGT used routinely actually had no advantages effect on the return of bowel function and it can prolonged the length of hospital stay, thus the traditional conception that NGT can promote the gastrointestinal tract function was unfounded.
Can nasogastric tubes reduce the incidence of postoperation complication? Although the present evidences not supported the NGTs used routinely, gastrointestinal decompression is still practiced by many urologists performing radical cystectomy with urinary diversion as concerning the incidence of complication such as ab-dominal distension, nausea, vomiting, especially postoperation ileus or small intestinal obstruction because POI has been the most important reason of prolonged the length of hospital stay in abdominal surgery and increased the cost of patients’ hospitalization [22,23]. However, against the traditional concepts which nasogastric tube can reduce the complications, in our result the incidence of postoperation paralytic ileus or bowel obstruction were significantly lower in the early nasogastric tube removed group than the traditional group (P = 0.010). At the meantime, there is no significant differences on other complications between the group Without NGT and With NGT, such as wound complication (P = 0.66). Nelson’s review [24] updated in the Cochrane library which included 5240 patients in abdominal surgery showed that those people who had not used NGT routinely experienced a decreased complications and the risk of POI, which similar our result. And some surgeons even suggest that NGT itself may promote aerophagia and abdominal distention and thereby prolong ileus [25]. Furthermore, not only nasogastric tubes does not increase the incidence of the postoperation complication, but there is no significance difference on pulmonary complication between the two groups (P = 0.25).
Nasogastric tube inserted also can make people fell obviously discomfort and irritability. Adamakis’s study [6] designed a simple question about which tube (NGT, drain, and catheter) patients would prefer to be removed first because of its discomfort after radical cystectomy. All patients chose to remove NGT indicated NGT was associated with patient discomfort. Carre`re N’s study [26] reported that an indwelling gastric tube is associated with discomfort in 70% of the patients and Mei JW and his colleagues [27] reported that the incidence of discomfort was as great as 98%.
Thus, routine NGT inserted neither did no beneficial to the recovery of gastrointestinal tract function, nor decreased the incidence of the postcomplication. Even increased the incidence of POI and prolonged the length of hospital stay and patients’ cost, meanwhile made patients fell discomfort. Routine NGT were not recommended for patients with radical cystectomy and urinary diversion. But for these patients with nausea and vomiting, nasogastric tubes replacement may be still useful.
To our knowledge, this is the first meta-analysis evaluated the necessity of nasogastric tube for people undergoing radical cystectomy. Though our results reveal that routine nasogastric tubes inserted is not recommendation, this meta-analysis is not without limitations. Firstly, perhaps the most important limitation is the quality of the data in the original studies. Even though every attempt was made to ensure accuracy in the data extraction, however, by definition, we have no idea to get all of the initial data from all studies. Furthermore, the limit of RCT studies and the rather small patients sample make it difficult to emphatically confirm that prolonged NGT inserted after radical cystectomy with urinary diversion offers no advantages. So we need a huge number of prospective randomized, double-blind study to reevaluate whether the nasogastric tube would be needed or not and exactly solve the important questions in urology.
Conclusions
Our meta-analysis revealed that routine nasogastric tube inserted after radical cystectomy with urinary diversion is unnecessary. Routine NGT neither accelerated the recovery of gastrointestinal tract function nor decreased the incidence of complications after operation. Meanwhile, nasogastric tube may adversely prolonged the time of POI and the length of hospital stay and may increase the patients’ cost. Though we have a result that routine NGTs were not recommendation for people who had undergoing radical cystectomy with urinary diversion, it is important to highlight the necessity of NGT after radical cystectomy with urinary diversion and to carry out more RCTs to further confirm the result of our analysis.
Acknowledgments
This study was supported by Science & Technology Department of Sichuan Province support program. Grant numbers: 2011SZ0144, 2011SZ0209.
Disclosure of conflict of interest
None.
References
- 1.Ramirez JA, McIntosh AG, Strehlow R, Lawrence VA, Parekh DJ, Svatek RS. Definition, incidence, risk factors, and prevention of paralytic ileus following radical cystectomy: a systematic review. Eur Urol. 2013;64:588–97. doi: 10.1016/j.eururo.2012.11.051. [DOI] [PubMed] [Google Scholar]
- 2.Liedberg F. Early Complications and Morbidity of Radical Cystectomy. European Urology Supplements. 2010;9:25–30. [Google Scholar]
- 3.Maffezzini M, Campodonico M, Canepa C, Gerbi G, Parodi D. Current perioperative management of radical cystectomy with intestinal urinary reconstruction for muscle-invasive bladder cancer and reduction of the incidence of postoperative ileus. Surg Oncol. 2008;17:41–8. doi: 10.1016/j.suronc.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Whittam BM, Cookson MS, Rowland RG. Routine use of nasogastric tubes after radical cystectomy. J Urol. 2011;185:1568–70. doi: 10.1016/j.juro.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 5.Ding J, Liao G, Xia Y, Zhang ZM, Pan Y, Liu S, Yan ZS. The necessity of indwelling gastrointestinal decompression after gastrectomy: a meta-analysis. J Surg Res. 2013;179:e71–81. doi: 10.1016/j.jss.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 6.Adamakis I, Tyritzis SI, Koutalellis G, Tokas T, Stravodimos KG, Mitropoulos D, Constantinides CA. Early removal of nasogastric tube is beneficial for patients undergoing radical cystectomy with urinary diversion. Int Braz J Urol. 2011;37:42–8. doi: 10.1590/s1677-55382011000100006. [DOI] [PubMed] [Google Scholar]
- 7.Cheadle WG, Vitale GC, Mackie CR, Cuschieri A. Prophylactic postoperative nasogastric decompression. A prospective study of its requirement and the influence of cimetidine in 200 patients. Ann Surg. 1985;202:361–6. doi: 10.1097/00000658-198509000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolff BG, Pembeton JH, van Heerden JA, Beart RW Jr, Nivatvongs S, Devine RM, Dozois RR, Ilstrup DM. Elective colon and rectal surgery without nasogastric decompression. A prospective, randomized trial. Ann Surg. 1989;209:670–3. doi: 10.1097/00000658-198906000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheatham ML, Chapman WC, Key SP, Sawyers JL. A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg. 1995;221:469–76. doi: 10.1097/00000658-199505000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park HK, Kwak C, Byun SS, Lee E, Lee SE. Early removal of nasogastric tube after cystectomy with urinary diversion: does postoperative ileus risk increase? Urology. 2005;65:905–8. doi: 10.1016/j.urology.2004.11.046. [DOI] [PubMed] [Google Scholar]
- 11.Donat SM, Slaton JW, Pisters LL, Swanson DA. Early nasogastric tube removal combined with metoclopramide after radical cystectomy and urinary diversion. J Urol. 1999;162:1599–602. [PubMed] [Google Scholar]
- 12.Inman BA, Harel F, Tiguert R, Lacombe L, Fradet Y. Routine nasogastric tubes are not required following cystectomy with urinary diversion: a comparative analysis of 430 patients. J Urol. 2003;170:1888–91. doi: 10.1097/01.ju.0000092500.68655.48. [DOI] [PubMed] [Google Scholar]
- 13.Vora AA, Harbin A, Rayson R, Christiansen K, Ghasemian R, Hwang J, Verghese M. Alvimopan provides rapid gastrointestinal recovery without nasogastric tube decompression after radical cystectomy and urinary diversion. Can J Urol. 2012;19:6293–8. [PubMed] [Google Scholar]
- 14.de Vries RR, Kauer P, van Tinteren H, van der Poel HG, Bex A, Meinhardt W, van Haarst EP, Horenblas S. Short-term outcome after cystectomy: comparison of two different perioperative protocols. Urol Int. 2012;88:383–9. doi: 10.1159/000336155. [DOI] [PubMed] [Google Scholar]
- 15.Cerruto MA, De Marco V, D’Elia C, Bizzotto L, De Marchi D, Cavalleri S, Novella G, Menestrina N, Artibani W. Fast track surgery to reduce short-term complications following radical cystectomy and intestinal urinary diversion with Vescica Ileale Padovana neobladder: proposal for a tailored enhanced recovery protocol and preliminary report from a pilot study. Urol Int. 2014;92:41–9. doi: 10.1159/000351312. [DOI] [PubMed] [Google Scholar]
- 16.Pruthi RS, Nielsen M, Smith A, Nix J, Schultz H, Wallen EM. Fast track program in patients undergoing radical cystectomy: results in 362 consecutive patients. J Am Coll Surg. 2010;210:93–9. doi: 10.1016/j.jamcollsurg.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 17.Pantelis D, Wolff M, Overhaus M, Hirner A, Kalff JC. [“Fast-track surgery”: Perioperative management] . Urologe A. 2006;45:W1193–200. doi: 10.1007/s00120-006-1049-z. quiz 1200-1201. [DOI] [PubMed] [Google Scholar]
- 18.Richards KA, Steinberg GD. Perioperative outcomes in radical cystectomy: how to reduce morbidity? Curr Opin Urol. 2013;23:456–65. doi: 10.1097/MOU.0b013e32836392bb. [DOI] [PubMed] [Google Scholar]
- 19.Pruthi RS, Chun J, Richman M. Reducing time to oral diet and hospital discharge in patients undergoing radical cystectomy using a perioperative care plan. Urology. 2003;62:661–5. doi: 10.1016/s0090-4295(03)00651-4. [DOI] [PubMed] [Google Scholar]
- 20.Hilton WM, Lotan Y, Parekh DJ, Basler JW, Svatek RS. Alvimopan for prevention of postoperative paralytic ileus in radical cystectomy patients: a cost-effectiveness analysis. BJU Int. 2013;111:1054–60. doi: 10.1111/j.1464-410X.2012.11499.x. [DOI] [PubMed] [Google Scholar]
- 21.Lightfoot AJ, Eno M, Kreder KJ, O’Donnell MA, Rao SS, Williams RD. Treatment of postoperative ileus after bowel surgery with low-dose intravenous erythromycin. Urology. 2007;69:611–5. doi: 10.1016/j.urology.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 22.Schuster TG, Montie JE. Postoperative ileus after abdominal surgery. Urology. 2002;59:465–71. doi: 10.1016/s0090-4295(01)01561-8. [DOI] [PubMed] [Google Scholar]
- 23.Iyer S, Saunders WB, Stemkowski S. Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm. 2009;15:485–94. doi: 10.18553/jmcp.2009.15.6.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007:CD004929. doi: 10.1002/14651858.CD004929.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis JW, Pisters LL, Doviak MJ, Donat SM. Early nasogastric tube removal combined with metoclopramide after postchemotherapy retroperitoneal lymph node dissection for metastatic testicular nonseminomatous germ cell tumor. Urology. 2002;59:579–83. doi: 10.1016/s0090-4295(01)01654-5. [DOI] [PubMed] [Google Scholar]
- 26.Carrère N, Seulin P, Julio CH, Bloom E, Gouzi JL, Pradère B. Is nasogastric or nasojejunal decompression necessary after gastrectomy? A prospective randomized trial. World J Surg. 2007;31:122–7. doi: 10.1007/s00268-006-0430-9. [DOI] [PubMed] [Google Scholar]
- 27.Mei JW, Li C, Xiang M, Chen MM, Yao XX, Yang QM, Yan C, Wang XY, Yan M, Zhu ZG. [Evaluation of the gastrointestinal decompression after gastrectomy: a prospective randomized controlled trial] . Zhonghua Wei Chang Wai Ke Za Zhi. 2009;12:452–5. [PubMed] [Google Scholar]


