Abstract
Objective: To investigate methods for improving the preoperative management of patients with pheochromocytoma. Methods: We collected 155 cases diagnosed as adrenal pheochromocytoma and with hypertension. During preoperative preparation, 85 patients had antihypertensive therapy by using the selective α1-blocker doxazosin controlled-release tablets; 70 patients was controlled by using the nonselective α-blocker phenoxybenzamine; All 155 patients underwent qualitative diagnosis by determination of 24-hour urinary vanilmandelic acid (VMA) or [11C]meta-hydroxyephedrine (mHED) positron emission tomography computed tomography (PET-CT) and underwent computed tomography (CT) for tumor localization; Results: In doxazosin group, with the exception of two patients who had radical fluctuations in blood pressure during surgery, other patients showed a smooth blood pressure control during surgery. No hypertensive crisis and hypotensive shock appeared after surgery. In phenoxybenzamine group, ten patients had sharp fluctuations in blood pressure during surgery, and no hypertensive crisis and hypotensive shock appeared after surgery. Conclusion: Compared with phenoxybenzamine, doxazosin has minimal adverse reactions, with high security as a preoperative preparation for adrenal pheochromocytoma, and it is easy to be taken. MHED PET-CT examination has a clear diagnostic value for patients with normal 24-hour urinary VMA.
Keywords: Adrenal, pheochromocytoma, perioperative period, doxazosin controlled-release tablets, phenoxybenzamine
Introduction
Currently, the qualitative and localization diagnosis of adrenal pheochromocytoma is relatively mature. However, preoperative management methods are more diverse, and there is a no clear and unified solution. Today, the development of new drugs, improvement of anesthetic techniques and enhancement of intraoperative monitor methods provide new conveniences for the preoperative management of patients with adrenal pheochromocytoma. To minimize adverse reactions of drugs, increase surgical safety, reduce patient costs and the occurrence of various complications, from 2009 to 2014, doxazosin and phenoxybenzamine were adopted as preoperative antihypertensive drugs for 85 and 70 patients with adrenal pheochromocytoma, respectively in our department, and were used as postoperative antihypertensive drugs, as reported below.
Materials and methods
Statement: (1) informed consent was obtained from each patient included in the study. (2) the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Clinical data
Blood pressure of patients in two groups were 150-180/90-120 mmHg (1 mmHg = 0.133 Kpa). They were randomly divided into 2 groups. Doxazosin group had 85 patients, including 50 males and 35 females, aged from 22 to 60 years. Their mean age was 38 years. Fifty-five patients showed tumors in the left adrenal gland, and 30 showed tumors in the right adrenal gland. Sixty-one patients were treated because of hypertension but no symptoms, and 24 patients were treated because of paroxysmal dizziness and headache. The 24-hour urinary VMA of 70 patients were increased (20.0-64.8 mg/24 h), and that of 15 patients were in the normal range. CT showed tumor diameter of 65 patients was 1.5-3 cm, that of 9 patients was 3-5 cm, and that of 6 patients was larger than 5 cm. Eighty patients underwent laparoscopic surgery, and five patients underwent open surgery. Phenoxybenzamine group had 70 patients, inclusing 40 males and 30 females, aged from 25 to 59 years. Their mean age was 40 years. Thirty-nine patients showed tumors in the left adrenal gland, and 31 showed tumors in the right adrenal gland. Forty-nine patients were treated because of hypertension, and 21 patients were treated because of paroxysmal dizziness and headache. The 24-hour urinary VMA of 51 patients were elevated (20.0-64.8 mg/24 h), and that of 19 patients were in the normal range. CT showed tumor diameter of 60 patients was 1.5-3 cm, that of 6 patients was 3-5 cm, and that of 4 patients was 5-7 cm. Seventy-seven patients underwent laparoscopic surgery, and three underwent open surgery (Table 1). Preoperative general conditions of patients in two groups (American Association of Anesthetists ASA) were assessed as ASA I-II grade. Heart, lung, liver and kidney function as well as coagulation function were normal, blood routine examination was normal. Using combined intravenous inhalation anesthesia, heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure and blood oxygen saturation were monitored during surgery. Preoperative control target of all patients’ blood pressure is 125-150/80-100 mmHg.
Table 1.
The clinical data of two groups of patients
| Doxazosin (n = 85) | Phenoxybenzamine (n = 70) | |
|---|---|---|
| male/female | 50/35 | 70/30 |
| average age (years) | 38 | 40 |
| left/right | 55/30 | 39/31 |
| hypertesion/paroxysmal dizzy | 61/24 | 49/21 |
| VMA abnormal/normal | 70/15 | 51/19 |
| 1.5 CM ≤ D ≤ 3 CM | 65 | 60 |
| 3 CM < D ≤ 5 CM | 9 | 6 |
| 5 CM < D ≤ 7 CM | 6 | 4 |
| laparoscopic/open surgery | 80/5 | 66/4 |
D: diameter of tumor.
Improvement methods
In doxazosin group, the initial dose was 4 mg Qd. If the blood pressure is poorly controlled, it can be increased to 8 mg Qd (one time a day). In phenoxybenzamine group, the initial dose was 5 mg Qd. If the blood pressure did not reach the target, then dose was increased to 5 mg Bid (twice a day); and if failed again then changed to 5 mg Tid (three times a day). The preoperative blood pressure of all patients was controlled in the range required for surgery (Table 2), and recorded adverse drug reactions with different drug dose (Table 3). MHED PET-CT assistant qualitative diagnosis was conducted on patients with normal 24-hour urinary VMA. In doxazosin group, 13 of fifteen patients with normal VMA underwent mHED PET-CT, and in phenoxybenzamine group, 14 of nineteen patients with normal VMA had mHED PET-CT examination.
Table 2.
The required drug doses and respective number and proportion of patients for preoperative blood pressure control target: 125-150/80-100 mmHg
| Doxazosin (n = 85) | Phenoxybenzamine (n = 70) | ||||
|---|---|---|---|---|---|
|
|
|||||
| 4 mg Qd | 8 mg Qd | 5 mg Qd | 5 mg Bid | 5 mg Tid | |
| Number | 80 | 5 | 5 | 27 | 38 |
| Proportion | 94% | 6% | 7% | 39% | 54% |
Table 3.
The adverse drug reaction and respective number and proportion of patients for preoperative blood pressure control target: 125-150/80-100 mmHg
| Doxazosin (n = 85) | Phenoxybenzamine (n = 70) | ||||
|---|---|---|---|---|---|
|
|
|||||
| 4 mg Qd | 8 mg Qd | 5 mg Qd | 5 mg Bid | 5 mg Tid | |
| orthostatic hypotension | 0 | 2 | 2 | 2 | 3 |
| dizzy | 2 | 1 | 1 | 3 | 6 |
| palpitation | 2 | 0 | 1 | 2 | 4 |
| tachycardia | 3 | 1 | 1 | 2 | 5 |
| thirst | 0 | 1 | 0 | 3 | 3 |
| rhinobyon | 0 | 0 | 0 | 3 | 4 |
| gastrointestinal discomfort | 1 | 0 | 0 | 2 | 2 |
| total cases | 10 (11.8%) | 49 (70%) | |||
As a result, lesions showed tracer concentration phenomenon, whereas the adrenal on the healthy side presented no tracer concentration (Figure 1), being consistent with postoperative pathology.
Figure 1.
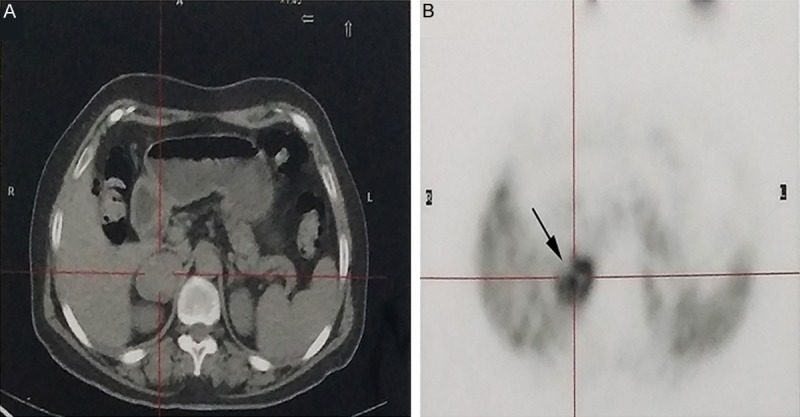
Images from a patient with right adrenal pheochromocytoma. A. Computed tomography (CT) scan demonstrates a clear right adrenal mass and a normal left adrenal mass. B. MHED PET scans show more prominent abnormal uptake in right adrenal mass.
Statistical analysis
Data were analyzed with GraphPad Prism v5.0, and the significance level was set at P<0.05. The results in Tables 2, 3, 4 and 5 were compared between doxazosin group and phenoxybenzamine group with Mean with SEM.
Table 4.
Respective number and proportion of intraoperative patients with 2 drugs in different fluctuation range of systolic blood pressure (mmHg)
| ≥ 200 or ≤ 100 | 160~200 | 100~160 | |
|---|---|---|---|
| Doxazosin (n = 85) | 2/85 (2%) | 4/85 (5%) | 79/85 (93%) |
| Phenoxybenzamine (n = 70) | 10/70 (14%) | 8/70 (11%) | 52/70 (74%) |
Table 5.
Respective number and proportion of postoperative patients with 2 drugs in different fluctuation range of systolic/diastolic blood pressure (mmHg)
| 120-140/80-90 | 140-150/90-100 | 150-160/100-110 | |
|---|---|---|---|
| Doxazosin (n = 85) | 70/85 (82%) | 11/85 (13%) | 4/85 (5%) |
| Phenoxybenzamine (n = 70) | 59/70 (84%) | 7/70 (10%) | 4/70 (6%) |
Results
In doxazosin group, 80 patients underwent laparoscopic surgery, and 5 patients underwent open surgery, among them, 4 patients preferred open surgery because of the large tumor, and 1 patient was transferred for open surgery because of intraoperative bleeding. 66 patients in phenoxybesnzamine group underwent laparoscopic surgery, 4 patients preferred open surgery because of the large tumor. Dramatic fluctuations in blood pressure appeared in 2 and 10 patients in two groups, respectively, blood pressure control in the remaining patients was relatively stable (Table 4), no hypertensive crisis and hypotensive shock presented after surgery (Table 5). For other adverse reactions, symptomatic treatments were given such as β-blocker metoprolol given for controlling tachycardia.
Discussion
Surgical excision is the most effective method for the treatment of pheochromocytoma. Pheochromocytoma has pathophysiological characteristics of low blood volume and hypertension, and high blood concentrations of catecholamine can lead to catecholamine cardiomyopathy. Therefore, hypertension control and improvement of blood vessel capacity are extremely important for improving surgical safety before surgery. Previously, we has used the non-selective α2-receptor blocker phenoxybenzamine as the drug to control hypertension and improve blood vessel capacity before surgery [1], but at least two negative factors present by using phenoxybenzamine: ① β2-receptors lose counteraction after the complete blocking of α2-receptor, easily inducing arrhythmias under the effect of high concentrations of catecholamines in the blood circulation [2,3]. ② After surgical resection of the tumor, persistent hypotension may occur due to vascular tension failure [4,5], and because of the pharmacokinetic characteristics of phenoxybenzamine itself, patients can still produce a variety of adverse reactions after taking the drug. In view of this, some scholars [6,7] applied selective α1-receptor blocker doxazosin controlled-release tablets for the preoperative preparation of patients with pheochromocytoma and found adverse reactions of the drug showed a low incidence, mild symptoms and short duration. The study of Conzo G et al [8] found that compared with patients using non-selective α2-receptor blockers, intraoperative hemodynamic changes were more stable in those using doxazosin [9]. The data of doxazosin group show that, with the exception of 2 patients (2%) whose intraoperative SBP was sharply increased over 200 mmHg or dropped below 100 mmHg for a while, intraoperative blood pressure of the other patients was smoothly controlled, no hypotensive shock presented after surgery, whereas 10 patients (14%) using phenoxybenzamine showed radical fluctuations. Patients (5%) whose SBP was fluctuated to 100-160 mmHg were also significantly less than those in phenoxybenzamine group (11%) (Figure 2C, P<0.05). But no significant difference (Figure 2D, P>0.05) could be found in fluctuations of postoperative blood pressure, which may due to the complete removal of the tumor or improvements in postoperative management, lacking a support of evidence-based medicine. 11.8% of patients in doxazosin group have adverse drug reactions, which is significantly less than 70% of those in phenoxybenzamine group (Figure 2A, P<0.05). 94% of patients with doxazosin could reach the control target by single dose, but almost 93% of patients with phenoxybenzamine need drug administration 2 or 3 times per day. It shows the application of doxazosin for the preoperative preparation of adrenal pheochromocytoma can stabilize blood pressure, reduce fluctuation range and has higher security, patients need only a single daily dose of medication and their compliance is better (Figure 2B). However, there are also some shortcomings in this study: First, we have not collected all patients with pheochromocytoma, including sporadic tumor, ectopic pheochromocytoma, huge pheochromocytoma (diameter >7 cm) and elderly patients (age >60), because these patients show a small proportion, are not typical and have complex disease conditions. Second, only the fluctuation range of the intraoperative SBP was compared, while DBP was not compared. In addition, different anesthesia may also generate different results, so large-scale comparative studies need to be conducted. On the other hand, we conducted mHED PET-CT assistant qualitative diagnosis on patients with normal 24-hour urinary VMA in the study. As we all know, in the past qualitative diagnosis of pheochromocytoma, 24-hour urinary VMA, 24-hour urinary catecholamine (CA), plasma free metanephrines (MN) and methoxy norepinephrine (NMN) are often measured. But only 24-hour urinary VMA can be detected in many hospitals, including our hospital. Although the specificity of the method is up to 95% [10], the false-negative rate can reach 25% [11], often resulting in the incapability of accurate preoperative diagnosis. Therefore, we performed mHED PET-CT examination on most patients with normal VMA. As a result, lesions showed tracer concentration phenomenon, whereas the normal adrenal presented no tracer concentration, being consistent with postoperative pathology. This demonstrate that the method is feasible. However, its reliability could not yet been confirmed in all patients due to the limitations of collected patients, requiring further multicenter studies.
Figure 2.
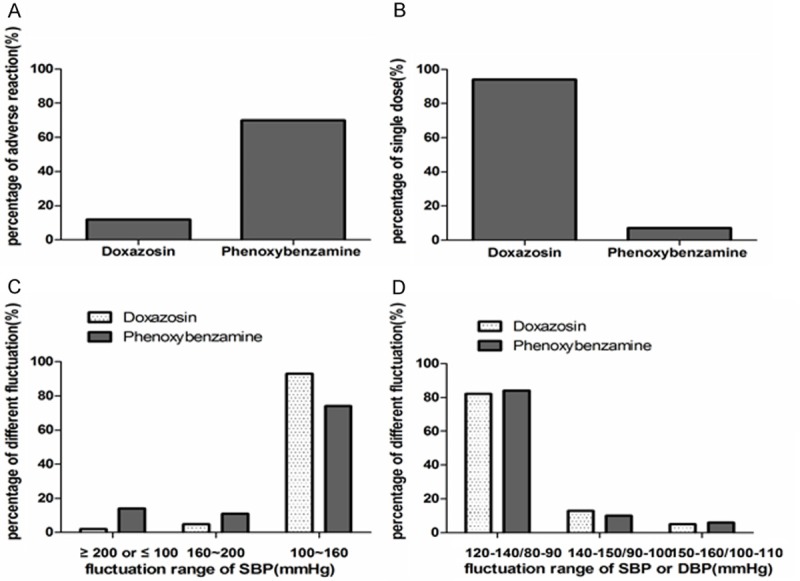
Comparison between doxazosin group and phenoxybenzamine group (A-D).
Disclosure of conflict of interest
None.
References
- 1.Mihai R, Sadler GP, Bridge H. Adrenergic blockade with phenoxybenzamine and propranolol in a cohort of 60 patients undergoing surgery for phaeochromocytoma. Eur J Anaesthesiol. 2008;25:508–510. doi: 10.1017/S0265021507002955. [DOI] [PubMed] [Google Scholar]
- 2.Badri M, Gibbons AV, Popii V, Yih D, Cohen-Stein DL, Patel SM. Perioperative management of a patient with a nonresectable pheochromocytoma. Endocr Pract. 2013;19:e74–76. doi: 10.4158/EP12343.CR. [DOI] [PubMed] [Google Scholar]
- 3.Paragliola RM, Ricciato MP, Gallo F, De Rosa A, Ianni F, Locantore P, Senes P, Pontecorvi A, Corsello SM. [Preoperative and postoperative management of adrenal masses] . G Chir. 2010;31:332–335. [PubMed] [Google Scholar]
- 4.Weingarten TN, Cata JP, O’Hara JF, Prybilla DJ, Pike TL, Thompson GB, Grant CS, Warner DO, Bravo E, Sprung J. Comparison of two preoperative medical management strategies for laparoscopic resection of pheochromocytoma. Urology. 2010;76:508, e506–511. doi: 10.1016/j.urology.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 5.Agrawal R, Mishra SK, Bhatia E, Mishra A, Chand G, Agarwal G, Agarwal A, Verma AK. Prospective study to compare peri-operative hemodynamic alterations following preparation for pheochromocytoma surgery by phenoxybenzamine or prazosin. World J Surg. 2014;38:716–723. doi: 10.1007/s00268-013-2325-x. [DOI] [PubMed] [Google Scholar]
- 6.Prys-Roberts C, Farndon JR. Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World J Surg. 2002;26:1037–1042. doi: 10.1007/s00268-002-6667-z. [DOI] [PubMed] [Google Scholar]
- 7.Miura Y, Yoshinaga K. Doxazosin: a newly developed, selective alpha 1-inhibitor in the management of patients with pheochromocytoma. Am Heart J. 1988;116:1785–1789. doi: 10.1016/0002-8703(88)90230-x. [DOI] [PubMed] [Google Scholar]
- 8.Conzo G, Musella M, Corcione F, Depalma M, Stanzione F, Della-Pietra C, Palazzo A, Napolitano S, Pasquali D, Milone M, Agostino-Sinisi A, Ferraro F, Santini L. Role of preoperative adrenergic blockade with doxazosin on hemodynamic control during the surgical treatment of pheochromocytoma: a retrospective study of 48 cases. Am Surg. 2013;79:1196–1202. [PubMed] [Google Scholar]
- 9.Mazza A, Armigliato M, Marzola MC, Schiavon L, Montemurro D, Vescovo G, Zuin M, Chondrogiannis S, Ravenni R, Opocher G, Colletti PM, Rubello D. Anti-hypertensive treatment in pheochromocytoma and paraganglioma: current management and therapeutic features. Endocrine. 2014;45:469–478. doi: 10.1007/s12020-013-0007-y. [DOI] [PubMed] [Google Scholar]
- 10.Bravo EL, Tagle R. Pheochromocytoma: state-of-the-art and future prospects. Endocr Rev. 2003;24:539–553. doi: 10.1210/er.2002-0013. [DOI] [PubMed] [Google Scholar]
- 11.Mannelli M, Ianni L, Cilotti A, Conti A. Pheochromocytoma in Italy: a multicentric retrospective study. Eur J Endocrinol. 1999;141:619–624. doi: 10.1530/eje.0.1410619. [DOI] [PubMed] [Google Scholar]


