Abstract
Purpose: Positioning of the patient during and after surgery can have significant implications on recovery. Therefore, the purpose of the present study was to determine the influence of placing patients in a lateral decubitus position for 15 min after combined use of hyperbaric and hypobaric ropivacaine and assess hemodynamic characteristics during spinal anesthesia for caesarean section. Methods: One hundred-forty patients undergoing elective cesarean delivery with combined use of hyperbaric and hypobaric ropivacaine were included in the present study. Patients meeting inclusion criteria (134) were randomly allocated into Group A: immediately turned to the supine position after induction of spinal anesthesia (n = 67) or Group B: maintained in a lateral decubitus position for 15 min before being turned to the supine position (n = 67). Primary endpoints of the study were to compare hemodynamic characteristics and sensory blockade levels in the two groups, while a secondary endpoint was to observe the incidence of complications. Results: Both groups showed similar effects of the combined anesthetic treatment. Incidence of hypotension (43% vs 18%, P = 0.001), systolic AP < 90 mmHg (36% vs. 16%, P = 0.011), usage of ephedrine (43% vs. 18%, P = 0.001) and the total dose of ephedrine [0 (0-24) vs 0 (0-18), P = 0.001] were significantly higher in Group A compared to Group B. Group A had a higher incidence of nausea compared to Group B (25% vs 7%, P = 0.005). Conclusions: Combined use of hyperbaric and hypobaric ropivacaine had satisfactory anesthetic effects and a more stable hemodynamic characteristic than either drug used alone. Maintaining the patient in a lateral decubitus position for 15 min can significantly decrease the incidence of hypotension.
Keywords: Spinal anesthesia, hyperbaric ropivacaine, hypobaric ropivacaine, caesarean section, lateral decubitus position
Introduction
Hypotension occurs in 50-70% of patients receiving spinal anesthesia for caesarean section, which is mainly caused by extensive sympathetic nerve blockade following spinal anesthesia, and oppression of the uterus on the inferior vena cava is another pathogenesis [1,2]. This double effect leads to decreased blood volume, causing reduced cardiac output. We hypothesized that patients maintained in a lateral decubitus position for 15 min before being turned to a supine position after spinal anesthesia could avoid the synergistic effects of sympathetic nerve blockade and compression of the uterus on the inferior vena cava. This design could benefit the establishment of compensatory mechanisms and decrease the incidence of hypotension. However, single treatment with either a hypobaric or hyperbaric anesthetic should not be chosen for patients undergoing prolonged time in the lateral decubitus position.
Isobaric anesthetics have been found to be influenced by many uncontrollable factors, which could lead to an unpredictability of the level of sensory blockade [3]. Thus, in the present study the combined use of hyperbaric and hypobaric ropivacaine was hypothesized to avoid sensory blockade with tilting the patient to one side. The purpose of the present study was to observe the influence of a lateral decubitus position for 15 min following combined use of hyperbaric and hypobaric ropivacaine on hemodynamic characteristics of spinal anesthesia used for caesarean section.
Materials and methods
Study design and subject allocation
All patients provided written informed consent prior to study inclusion. One hundred-forty ASA physical status I or II patients (gestational age ≥ 37 weeks, singleton) undergoing elective cesarean delivery under combined spinal-epidural anesthesia were included in the study. Exclusion criteria included age < 18 years or > 35 years, height < 150 cm or > 180 cm, weight < 50 kg or > 100 kg, operation time > 60 min, hypertension, multiple pregnancy, placenta previa, cardiovascular and cerebrovascular diseases, macrosomia, known abnormal fetal development, or contraindications for intraspinal anesthesia or signs of onset of labor.
All patients were fasted preoperatively for 8 hours and water deprived for more than 4 hours. The patients were maintained in a supine position with a 15° left lateral tilt after entering the operating room. Each patient was rapidly administered 7 mL/kg of 6% hydroxyethyl starch (200/0.5) within 10 min via a 16-gauge cannula placed in the forearm veins. Infusion speed was then adjusted to 7 mL/kg•h. Multifunctional monitoring was used to measure blood pressure 5 mins following infusion, and the mean value of three consecutive detections was recorded.
Anesthetics used in this study consisted of two parts (#1 and #2), which are shown as follows: Syringe #1: 1 mL 0.5% hyperbaric ropivacaine, composed of 0.5 mL 1% ropivacaine, 0.1 mL 0.0001% fentanyl and 0.4 mL 10% glucose; Syringe #2: 1 mL 0.5% hypobaric ropivacaine, composed of 0.5 mL 1% ropivacaine, 0.1 mL 0.0001% fentanyl and 0.4 mL sterile distilled water.
A combined spinal-epidural procedure was performed at the L2-3 interspace with the patient maintained in a left lateral decubitus position. Anesthetics in syringes #1 and #2 were successively injected upwards when the needle entered the subarachnoid space. The injection speed of the anesthetics was 0.1 mL/s.
The spinal anesthesia needle was withdrawn and 3 cm of the epidural catheter was placed into the epidural space. Subjects were randomized by a computer generated random number table into two groups. Immediately following spinal anesthesia, patients in Group A were turned to the supine position with a left lateral tilt of 15°. In contrast, patients in Group B were maintained in a lateral decubitus position for 15 min before being turned to a supine position with a left lateral tilt of 15°. The upper sensory blockade level was checked every 1 min until the beginning of the operation by assessing for loss of pain sensation along the collarbone midline using a 20-gauge sterilized needle. If the T6 sensory blockade level was not achieved, an epidural supplement of 2% lidocaine was administered to maintain a T6 sensory level.
Hypotension was defined as systolic arterial pressure (AP) < 90 mmHg or a decrease in systolic AP > 20% from baseline. When perioperative systolic AP was decreased to this level, 6 mg ephedrine was administered every 2 min until the systolic AP was maintained within normal range. Atropine (0.3 mg) was used to treat bradycardia (heart rate < 50/min). Patients who had an operation time > 60 min or an insertion time of the epidural catheter > 3 min were excluded from further study.
Hemodynamic data, upper sensory blockade level, insertion time of the epidural catheter, complete analgesia time [beginning of intrathecal injection to a visual analogue scale (VAS) > 0], operation time, usage rate of ephedrine, total dose of ephedrine in each patient and incidence of complications (including nausea, vomiting, shivering and dizziness) were recorded. Operative conditions were evaluated by a gynecologist according to the adequacy of muscle relaxation (0 = poor, 1 = moderate, 2 = good, 3 = very good). Neonatal conditions were assessed using Apgar scores at 1 and 5 min.
Statistical analyses
Primary outcomes included hemodynamic characteristics such as incidences of hypotension, systolic blood pressure < 90 mmHg and ephedrine usage, and the height of sensory block ≥ T2. Sample size was calculated according to preliminary data. For example, to determine the incidence of hypotension or usage rate of ephedrine, a sample size of 56 patients per group had a 80% power at the 5% significance level. While considering the dropout rate (presumably 15%), 67 patients were enrolled in each of the two groups. Secondary outcome was the incidence of complications.
SPSS 17.0 software was used for statistical analyses. Data were analyzed using the Shapiro-Wilks test to determine distribution. If normally distributed, the data are presented as mean ± SD and two independent groups were compared using a Student’s t-test. Data distributed non-normally are presented as median (min-max) and analyzed using a Mann-Whitney U test. Categorical variables were analyzed using a chi-square test, or Fisher’s exact test if the number of subjects in any contingency table cell was less than five. P < 0.05 was considered statistically significant.
Results
One hundred-forty patients were assessed for study eligibility; six patients did not meet inclusion criteria (operation time > 60 min), and 134 patients were randomized with 67 in each group (Figure 1).
Figure 1.
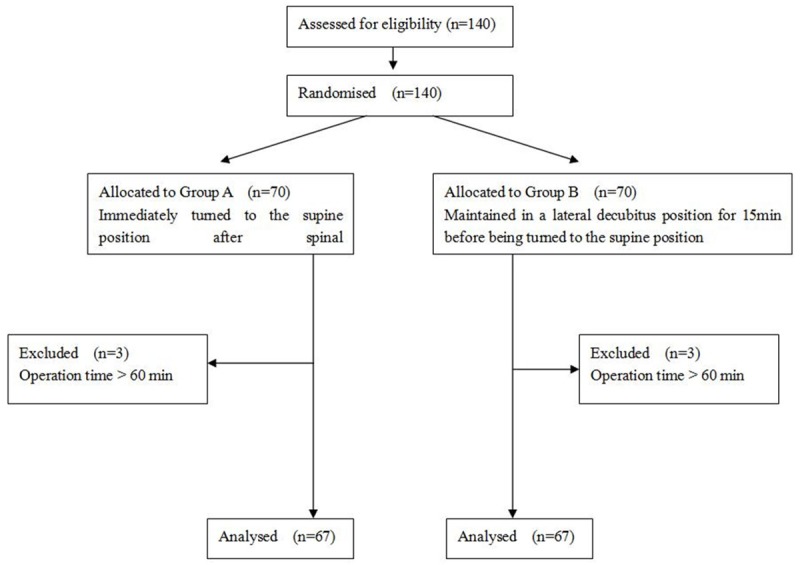
Study flow diagram for 134 patients undergoing elective caesarean section under a combined spinal-epidural procedure.
Baseline characteristics of the patients including insertion time of the epidural catheter, operation time, operative condition evaluation and complete analgesia time were not statistically different between groups (Table 1). Hemodynamic data from intrathecal injection to shoulder delivery suggested that the incidences of hypotension (43% vs 18%, P = 0.001), systolic AP < 90 mmHg (36% vs. 16%, P = 0.011), usage rate of ephedrine (43% vs 18%, P = 0.001) and the total dose of ephedrine [0 (0-24) vs 0 (0-18), P = 0.001] were significantly higher in Group A compared to Group B. The number of patients with height of sensory blockade ≥ T2 in Group A was significantly greater than those in Group B (45% vs. 8%, P < 0.001, Table 2). Neonatal characteristics were also comparable (Table 3).
Table 1.
Baseline characteristics of all patients meeting inclusion criteria
| Group A (n = 67) | Group B (n = 67) | P value | |
|---|---|---|---|
| Age (yr) | 28 (18-41) | 27 (18-37) | 0.121 |
| Height (cm) | 162 (152-172) | 160 (146-171) | 0.142 |
| Weight (kg) | 73 (52-93) | 74 (58-88) | 0.679 |
| Gestational age (wk) | 38 (36-39) | 38 (37-40) | 0.104 |
| Catheter insertion time (min) | 2 (1-3) | 2 (1-5) | 0.122 |
| Operation time (min) | 37 (29-48) | 39 (26-50) | 0.290 |
| Scores of operative conditions | 2.7 ± 0.46 | 2.6 ± 0.49 | 0.509 |
| Complete analgesia time (min) | 135 ± 21 | 138 ± 14 | 0.461 |
| Baseline | |||
| Systolic AP (mmHg) | 130 ± 10 | 128 ± 11 | 0.209 |
| Diastolic AP (mmHg) | 62± 9 | 63 ± 10 | 0.632 |
| Mean AP (mmHg) | 86 ± 8 | 85 ± 7 | 0.377 |
| HR (beats/min) | 83 ± 10 | 81 ± 11 | 0.619 |
Values presented as mean ± SD or median (min-max).
Table 2.
Hemodynamic data and blockade characteristics of the patients
| Beginning of induction to delivery | Group A (n = 67) | Group B (n = 67) | P value |
|---|---|---|---|
| Incidence of hypotension (%) | 29 (43%) | 12 (18%) | 0.001 |
| Systolic blood pressure < 90 mmHg | 24 (36%) | 11 (16%) | 0.011 |
| Usage rate of ephedrine (%) | 29 (43%) | 12 (18%) | 0.001 |
| Total dose of ephedrine (mg) | 0 (0-24) | 0 (0-18) | 0.001 |
| Height of sensory block ≥ T2 | 30 (45%) | 5 (8%) | < 0.001 |
Values presented as n (%) or median (min-max).
Table 3.
Neonatal characteristics
| Group A (n = 67) | Group B (n = 67) | P value | |
|---|---|---|---|
| Apgar at 1 min | 9 (7-10) | 9 (7-10) | 0.895 |
| Apgar at 5 min | 10 (8-10) | 10 (9-10) | 0.117 |
| Birth weight (kg) | 3.31 (2.5-4.2) | 3.26 (2.4-4.2) | 0.511 |
Values presented as mean ± SD or median (min-max).
Group A had a higher incidence of nausea compared to Group B (25% vs 7%, P = 0.005). There were no statistical differences in the incidence of other complications between the two groups (Table 4). No supplemental anaesthetics were administered into the epidural space or veins perioperatively in both groups and no patients had a perioperative VAS > 0.
Table 4.
Incidence of patient complications
| Group A (n = 67) | Group B (n = 67) | P Value | |
|---|---|---|---|
| Nausea | 17 (25%) | 5 (7%) | 0.005 |
| Vomiting | 4 (6%) | 2 (3%) | 0.680 |
| Shivering | 34 (51%) | 29 (43%) | 0.387 |
| Dizziness | 0 (0%) | 0 (0%) | - |
| Sleepiness | 0 (0%) | 0 (0%) | - |
Values presented as n (%).
Discussion
In the present study, patients maintained in a lateral decubitus position for 15 min before being turned to a supine position following spinal anesthesia (Group B) had decreased incidence of hypotension and usage rate of ephedrine. This could be due to the fact that the lateral decubitus position for 15 min avoids the synergistic effect of sympathetic nerve blockade and oppression of the uterus on the inferior vena cava following spinal anesthesia. The effective blood volume could be redistributed during this time and lead to a decreased incidence of hypotension and nausea. This method significantly alleviated the severe hemodynamic changes induced by rapid onset of spinal anesthesia.
Previous studies showed that vasoactive agents and body position changes are the most effective methods to prevent or treat hypotension during caesarean section, and new progress was mainly reported from the studies on body position changes [3-10]. The incidence of hypotension decreased by 20% and the number of ephedrine usage decreased by 25% in patients maintained in a sitting position for 5 min before being turned to a supine position after the induction of spinal anesthesia compared with those immediately turned to the supine position [6,11]. However, spinal anesthesia should be performed in a sitting position and maintained for 5 min, which is not comfortable for patients (compared to a lateral decubitus position). At least two people are needed to place the patient in the supine position after sitting for 5 min. Therefore, we induced spinal anesthesia in the lateral decubitus position and maintained the position for 15 min until turning them to a supine position. This time was determined because previous studies indicated that hemodynamic changes were most severe at 15 min following spinal anesthesia [12-14]. In addition, the level of anesthesia is usually fixed 15 min after spinal anesthesia [15,16].
Studies have shown that the spread of spinal anesthetics in the subarachnoid space is influenced by many uncontrollable factors, which could lead to an unpredictability of the level of sensory blockade. One important reason is that cerebrospinal fluid is not only affected by gender and pregnancy, but also has unique physical properties including capacity, density and temperature [17-22]. Thus, it is difficult to prepare an isobaric solution with a density equal to the cerebrospinal fluid of the patient. For this reason, we used hyperbaric combined with hypobaric ropivacaine treatment. Half dose of hyperbaric and the other half of hypobaric solutions were administered successively into the intrathecal space. In this condition, the initial half dose of the hyperbaric solution may spread inferiorly, and the second half dose of the hypobaric solution may move superiorly. Therefore, the solutions spread uniformly to the left and right side of the patients, which avoid the level of anesthesia tilting to one side.
Vasopressors are usually given as an intravenous bolus and continuous infusion with constant speed in caesarean section following spinal anesthesia [23]. This mode of administration might lead to a risk of transient hypertension and is particularly dangerous for patients with preeclampsia. It is worthy to ascertain whether maintaining patients in a lateral decubitus position for 15 min is beneficial for receiving continuous and constant infusions of vasopressors, which could avoid the use of single bolus, and decrease the incidence of transient hypertension.
In conclusion, the combined use of hyperbaric and hypobaric ropivacaine has satisfactory anesthetic effects and maintaining patients in a lateral decubitus position for 15 min can significantly decrease the incidence of hypotension.
Disclosure of conflict of interest
None.
References
- 1.Loubert C, Hallworth S, Fernando R, Columb M, Patel N, Sarang K, Sodhi V. Does the baricity of bupivacaine influence intrathecal spread in the prolonged sitting position before elective cesarean delivery? A prospective randomized controlled study. Anesth Analg. 2011;113:811–7. doi: 10.1213/ANE.0b013e3182288bf2. [DOI] [PubMed] [Google Scholar]
- 2.Leo S, Sng BL, Lim Y, Sia AT. A randomized comparison of low doses of hyperbaric bupivacaine in combined spinal-epidural anesthesia for cesarean delivery. Anesth Analg. 2009;109:1600–5. doi: 10.1213/ANE.0b013e3181b72d35. [DOI] [PubMed] [Google Scholar]
- 3.Maayan-Metzger A, Schushan-Eisen I, Todris L, Etchin A, Kuint J. Maternal hypotension during elective cesarean section and short-term neonatal outcome. Am J Obstet Gynecol. 2010;202:56, e1–5. doi: 10.1016/j.ajog.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Shin BS, Kim CS, Sim WS, Lee CJ, Kim ST, Kim GH, Bang SR, Lee SH, Hyun SJ, Kim GS. A comparison of the effects of preanesthetic administration of crystalloid versus colloid on intrathecal spread of isobaric spinal anesthetics and cerebrospinal fluid movement. Anesth Analg. 2011;112:924–30. doi: 10.1213/ANE.0b013e31820d93d8. [DOI] [PubMed] [Google Scholar]
- 5.Sanansilp V, Trivate T, Chompubai P, Visalyaputra S, Suksopee P, Permpolprasert L, von Bormann B. Clinical characteristics of spinal levobupivacaine: Hyperbaric compared with isobaric solution. ScientificWorldJournal. 2012;2012:169076. doi: 10.1100/2012/169076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coppejans HC, Hendrickx E, Goossens J, Vercauteren MP. The sitting versus right lateral position during combined spinal-epidural anesthesia for cesarean delivery: Block characteristics and severity of hypotension. Anesth Analg. 2006;102:243–7. doi: 10.1213/01.ane.0000189049.11005.26. [DOI] [PubMed] [Google Scholar]
- 7.Miyabe M, Sato S. The effect of head-down tilt position on arterial blood pressure after spinal anesthesia for cesarean delivery. Reg Anesth. 1997;22:239–42. doi: 10.1016/s1098-7339(06)80008-8. [DOI] [PubMed] [Google Scholar]
- 8.Loke GP, Chan EH, Sia AT. The effect of 10 degrees head-up tilt in the right lateral position on the systemic blood pressure after subarachnoid block for caesarean section. Anaesthesia. 2002;57:169–72. doi: 10.1046/j.1365-2044.2002.02227.x. [DOI] [PubMed] [Google Scholar]
- 9.Mendonca C, Griffiths J, Ateleanu B, Collis RE. Hypotension following combined spinal-epidural anaesthesia for caesarean section. Left lateral position vs. Tilted supine position. Anaesthesia. 2003;58:428–31. doi: 10.1046/j.1365-2044.2003.03090.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly JD, McCoy D, Rosenbaum SH, Brull SJ. Haemodynamic changes induced by hyperbaric bupivacaine during lateral decubitus or supine spinal anaesthesia. Eur J Anaesthesiol. 2005;22:717–22. doi: 10.1017/s0265021505001183. [DOI] [PubMed] [Google Scholar]
- 11.Kohler F, Sorensen JF, Helbo-Hansen HS. Effect of delayed supine positioning after induction of spinal anaesthesia for caesarean section. Acta Anaesthesiol Scand. 2002;46:441–6. doi: 10.1034/j.1399-6576.2002.460419.x. [DOI] [PubMed] [Google Scholar]
- 12.El-Hakeem EE, Kaki AM, Almazrooa AA, Al-Mansouri NM, Alhashemi JA. Effects of sitting up for five minutes versus immediately lying down after spinal anesthesia for cesarean delivery on fluid and ephedrine requirement; a randomized trial. Can J Anaesth. 2011;58:1083–9. doi: 10.1007/s12630-011-9593-4. [DOI] [PubMed] [Google Scholar]
- 13.Quan Z, Tian M, Chi P, Cao Y, Li X, Peng K. Influence of phenylephrine or ephedrine on maternal hemodynamics upon umbilical cord clamping during cesarean delivery. Int J Clin Pharmacol Ther. 2013;51:888–94. doi: 10.5414/CP201974. [DOI] [PubMed] [Google Scholar]
- 14.Sng BL, Tan HS, Sia AT. Closed-loop double-vasopressor automated system vs manual bolus vasopressor to treat hypotension during spinal anaesthesia for caesarean section: a randomised controlled trial. Anaesthesia. 2014;69:37–45. doi: 10.1111/anae.12460. [DOI] [PubMed] [Google Scholar]
- 15.Ngan Kee WD, Lee SW, Khaw KS, Ng FF. Haemodynamic effects of glycopyrrolate pre-treatment before phenylephrine infusion during spinal anaesthesia for caesarean delivery. Int J Obstet Anesth. 2013;22:179–87. doi: 10.1016/j.ijoa.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Kim JT, Lee JH, Cho CW, Kim HC, Bahk JH. The influence of spinal flexion in the lateral decubitus position on the unilaterality of spinal anesthesia. Anesth Analg. 2013;117:1017–21. doi: 10.1213/ANE.0b013e3182a1ee53. [DOI] [PubMed] [Google Scholar]
- 17.Lilot M, Meuret P, Bouvet L, Caruso L, Dabouz R, Deléat-Besson R, Rousselet B, Thouverez B, Zadam A, Allaouchiche B, Boselli E. Hypobaric spinal anesthesia with ropivacaine plus sufentanil for traumatic femoral neck surgery in the elderly: A dose-response study. Anesth Analg. 2013;117:259–64. doi: 10.1213/ANE.0b013e31828f29f8. [DOI] [PubMed] [Google Scholar]
- 18.Carpenter RL, Hogan QH, Liu SS, Crane B, Moore J. Lumbosacral cerebrospinal fluid volume is the primary determinant of sensory block extent and duration during spinal anesthesia. Anesthesiology. 1998;89:24–9. doi: 10.1097/00000542-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Higuchi H, Hirata J, Adachi Y, Kazama T. Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Anesthesiology. 2004;100:106–14. doi: 10.1097/00000542-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Horlocker TT, Wedel DJ. Density, specific gravity, and baricity of spinal anesthetic solutions at body temperature. Anesth Analg. 1993;76:1015–8. doi: 10.1213/00000539-199305000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Heller AR, Zimmermann K, Seele K, Rossel T, Koch T, Litz RJ. Modifying the baricity of local anesthetics for spinal anesthesia by temperature adjustment: Model calculations. Anesthesiology. 2006;105:346–53. doi: 10.1097/00000542-200608000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan JT, Grouper S, Walker MT, Parrish TB, McCarthy RJ, Wong CA. Lumbosacral cerebrospinal fluid volume in humans using three-dimensional magnetic resonance imaging. Anesth Analg. 2006;103:1306–10. doi: 10.1213/01.ane.0000240886.55044.47. [DOI] [PubMed] [Google Scholar]
- 23.Rosseland LA, Hauge TH, Grindheim G, Stubhaug A, Langesaeter E. Changes in blood pressure and cardiac output during cesarean delivery: The effects of oxytocin and carbetocin compared with placebo. Anesthesiology. 2013;119:541–51. doi: 10.1097/ALN.0b013e31829416dd. [DOI] [PubMed] [Google Scholar]


