Abstract
Background
Attention-deficit/hyperactivity disorder (ADHD) is presumed to be heterogeneous, but the best way to describe this heterogeneity remains unclear. Considerable evidence has accrued suggesting that inattention versus hyperactivity-impulsivity symptom domains predict distinct clinical outcomes and may have partially distinct etiological influence. As a result, some conceptualizations emphasize two distinct inputs to the syndrome. Yet formal testing of models that would accommodate such assumptions using modern methods (e.g., second-order factor and bifactor models) has been largely lacking.
Methods
Participants were 548 children (321 boys) between the ages of 6 and 18 years. Of these 548 children, 302 children met DSM-IV criteria for ADHD, 199 were typically developing controls without ADHD, and 47 were classified as having situational or subthreshold ADHD. ADHD symptoms were assessed via parent report on a diagnostic interview and via parent and teacher report on the ADHD Rating Scale.
Results
A bifactor model with a general factor and specific factors of inattention and hyperactivity-impulsivity fit best when compared with one-, two-, and three-factor models, and a second-order factor model.
Conclusions
A bifactor model of ADHD latent symptom structure is superior to existing factor models of ADHD. This finding is interpreted in relation to multi-component models of ADHD development, and clinical implications are discussed.
Keywords: ADHD, structural equation modeling, development
Attention-deficit/hyperactivity disorder (ADHD), as defined by the DSM-IV-TR (American Psychiatric Association, 2000), is characterized by two behavioral symptom domains: inattention and hyperactivity-impulsivity. This syndrome captures a heterogeneous group of youngsters (Nigg, Willcutt, Doyle, & Sonuga-Barke, 2005) and may reflect heterogeneous inputs to the symptom domains (Sonuga-Barke, 2002). Inattention and hyperactivity convey somewhat distinct long-term risks (Fischer, Barkley, Smallish, & Fletcher, 2007; Massetti et al., 2008; Sonuga-Barke, Auerbach, Campbell, Daley, & Thompson, 2005), even though they are substantially correlated and often co-occur. Yet conceptual models of ADHD structure do not accommodate this information. For example, the subtyping scheme in the DSM-IV is likely insufficient to capture the etiological or phenotypic structure of ADHD due, in part, to the fact that small variations in symptoms levels lead to large changes in subtype classification (Lahey, Pelham, Loney, Lee, & Willcutt, 2005).
There is better support for the two-dimensional model (inattention and hyperactivity-impulsivity), but that model is quite vulnerable to developmental changes in ADHD symptoms (Hart, Lahey, Loeber, Applegate, & Frick, 1995; Lahey et al., 2005). This raises a key conceptual question that is testable by statistical methods: does a multiple-component model of ADHD, specifying distinct influence on ADHD symptom domains, more accurately characterize the disorder compared to a single-component model, specifying uniform influence on the disorder? The answer to this question of phenotypic symptom structure has clear ramifications for how the disorder is conceptualized (e.g., in the DSM manuals) and for theories of etiological structure, as well as for clinical practice, assessment, and future epidemio-logical studies.
Despite the fact that ADHD symptoms can wax and wane (Lahey et al., 2005) and some children do recover (Faraone, Biederman, & Mick, 2006), ADHD is generally conceptualized by clinicians and researchers as a relatively stable condition across development. That is, it is typically assumed that a latent general or ‘g’ ADHD construct holds across situations and time, with or without specific or ‘s’ factorial components that may change over time (i.e., the child ‘has ADHD’ even though the symptom display may vary with context). However, factorial support for this idea has been lacking, leaving a gap between clinical understanding and statistical models of ADHD. The factorial literature on ADHD structure does not presume a ‘g’ factor for ADHD; it assumes a one-, two-, or three-factor structure, or occasionally a second-order factor structure.
Confirmatory factor analyses have tended to support a two-factor structure in clinical and population samples (Amador-Campos, Forns-Santacana, Martorell-Balanzo, Guardia-Olmos, & Pero-Cebollero, 2005, 2006; Bauermeister et al., 1992, 1995; Burns, Walsh, Owen, & Snell, 1997a; Burns et al., 1997b; Burns, Boe, Walsh, Sommers-Flanagan, & Teegarden, 2001; DuPaul et al., 1997; Gomez, Burns, Walsh, & Hafetz, 2005; Lahey et al., 1988; Pillow, Pelham, Hoza, Molina, & Stultz, 1998; Wolraich et al., 2003). Two-factor models are generally better supported than one-factor (unidimensional) or three-factor (separating impulsivity from hyperactivity) models (Burns et al., 2001). Yet none of these models are consistent with the way ADHD is thought of by clinicians or portrayed in the DSM-IV, nor do they account simultaneously for the overlap and stability, as well as distinctiveness and change, of ADHD symptom domains.
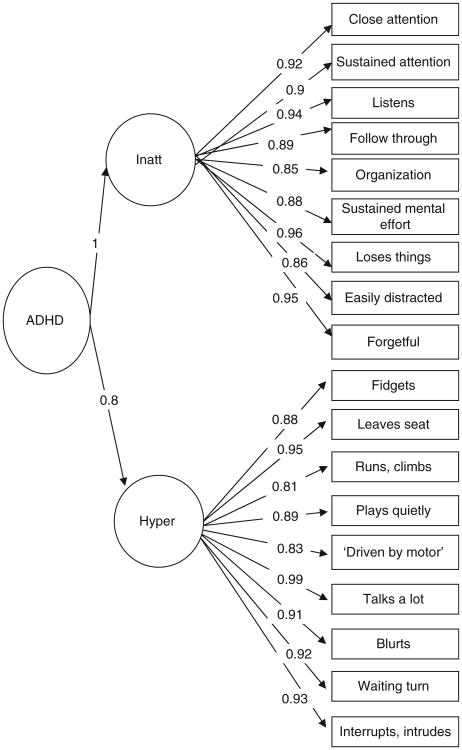
A second-order factor model or a bifactor model1 would provide meaningful alternatives to these simple factor models by enabling simultaneous estimation of general and specific factors. However, second-order and bifactor models still suggest quite different assumptions about underlying structure, support different etiological assumptions, and have different clinical implications (see Table 1). A second-order factor model allows inattentive and hyperactive-impulsive symptom domains to be modeled separately with both symptom domains being entirely encompassed by a higher-order ADHD factor, as shown in Figure 1. This idea is most in line with the DSM-IV model of a single ADHD diagnostic category, perhaps with subtypes, and with a single final pathway to this disorder, influenced by overlapping etiological inputs. In addition, support for a second-order factor model suggests that clinical intervention would be similarly effective for all children with ADHD, regardless of symptom profile, and that variation of symptom profile would not be especially important for assessing long-term risk of poor outcomes or for investigating etiology.
Table 1. Real-world implications of ADHD structural models.
| Single-order | Second-order | Bifactor | |
|---|---|---|---|
| Etiology | Unclear | Shared/overlapping | Distinct inputs/multiple |
| Fit to DSM-IV ADHD categorical diagnosis | Poor | Good | Somewhat |
| Fit to DSM-IV ADHD subtypes | Poor | Somewhat | Good |
| Fit to ADHD symptom domains | Good | Somewhat | Good |
| Sensitivity to developmental change | Somewhat | No | Yes |
| Treatment implications | Unclear | Similar for all | Should be tailored to symptom profile |
| How to predict outcomes | With severity of symptoms within each domain | With ADHD as adiagnostic category | With specific constellations of ADHD symptoms |
Figure 1. ADHD second-order factor model.
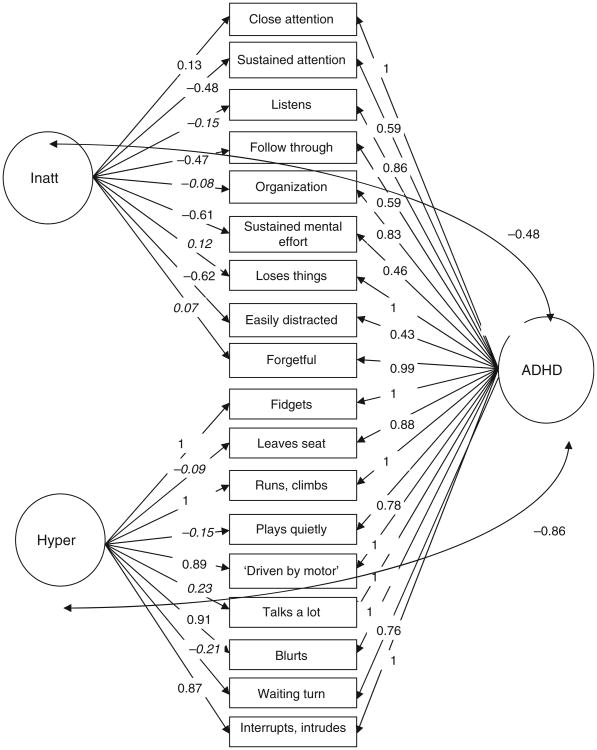
A bifactor model of ADHD, with a ‘g’ factor and two (or three) specific factors of inattention and hyperactivity-impulsivity, is conceptually distinct (see Table 1). It allows for individual ADHD symptoms to simultaneously load onto an overall, or ‘general’ (‘g’), ADHD factor along with completely or partially distinct (‘specific’ (‘s’)) inattention and hyperactive-impulsive latent components, as shown in Figure 2. Support for this model might explain contradictory findings of general and specific influences on ADHD symptom domains. It would further suggest that children with ADHD are characterized by substantial interindividual heterogeneity, with some children exhibiting high inattentive and hyperactive-impulsive symptoms and other children exhibiting a different kind of symptom profile with high symptoms in only one of the two symptom domains. Thus, this model is more compatible than any other model with the current subtype structure in DSM-IV, although not identical since general and specific risk are not necessarily part of the same diagnostic category (ADHD) in this model (i.e., general ADHD might be one diagnostic category with specific inattention being a different disorder and specific hyperactivity-impulsivity being a developmentally specific manifestation of general ADHD). A bifactor model suggests that there are distinct (rather than heavily overlapping) etiological influences that converge on the same syndrome (Chen, West, & Sousa, 2006; Krueger, Markon, Patrick, Benning, & Kramer, 2007). This model would be in line with multiple-pathway, or multiple component process, conceptions of the disorder (Nigg, Goldsmith, & Sachek, 2004; Sonuga-Barke, 2005). For clinicians, this would suggest that assessment of general risk for ADHD, specific risk for inattention, and specific risk for hyperactivity-impulsivity would provide valuable information about an individual child's profile and risk over time. In addition, it suggests that treatment for ADHD might benefit from being tailored to the symptom profile of the particular child (e.g., psychopharmacology for high inattentive symptoms, behavioral treatment for high hyperactive-impulsive symptoms, and combined treatment for children with high symptoms in both domains).
Figure 2. ADHD bifactor model.
The bifactor model approach has recently been used to describe externalizing behaviors in adults (Krueger et al., 2007). However, it has essentially not been tested for childhood ADHD, with two important exceptions. Toplak et al. (2009) fit a bifactor model of ADHD in a sample of clinic-referred adolescents. The bifactor model showed superior fit to simple factor models, although a second-order factor model was not examined. There has also been some empirical support for a bifactor model of inattention, hyperactivity, and impulsivity using the Achenbach (1991) Child Behavior Checklist (CBCL) item pool (somewhat different than the DSM-IV item pool; Achenbach, Bernstein, & Dumenci, 2005; Dumenci, McConaughy, & Achenbach, 2004).
This paper attempts a comprehensive evaluation and comparison of alternative models (including single-order factor, second-order factor, and bifactor models) using DSM-IV items in a community-recruited sample of cases and controls with a wide age range. Study hypotheses were that there would be support for both a general ADHD factor and orthogonal specific factors of inattention and hyperactivity-impulsivity, consistent with DSM-IV and multiple-component conceptualization of ADHD etiology.
Method
Participants
Overview
Participants were 548 children (321 boys), 6 to 18 years old, recruited from the community and then evaluated for study eligibility and diagnostic status. Children were initially included in one of two groups: ADHD (n = 302) and non-ADHD comparison youth (‘controls,’ n = 199). Forty-seven additional children who were classified as having situational or sub-threshold ADHD (did not meet criteria for either ADHD or control group as explained below) were included to provide more complete coverage of the dimensional trait space of ADHD (Levy, Hay, McStephen, Wood, & Waldman, 1997; Sherman, Iacono, & McGue, 1997).
The ADHD group included 110 children with ADHD-predominantly inattentive type (ADHD-PI; i.e., met criteria for six or more inattentive symptoms, plus impairment, onset, and duration, and never in the past met criteria for combined type) and 192 children with ADHD-combined type (ADHD-C; i.e., met criteria for six or more inattentive symptoms and six or more hyperactive-impulsive symptoms, plus impairment, onset, and duration). The current sample included no children with the hyperactive-impulsive ADHD subtype, fairly typical in this age range (e.g., Lahey et al., 2005; Shaw et al., 2007). Thus, the sample is viewed as representing the clinical presentation of ADHD in the community in this age range. As shown in Table 2, 161 children met DSM-IV criteria for oppositional-defiant disorder (ODD), and 19 were diagnosed with conduct disorder (CD). Children came from 468 families; 80 families had two children in the study. All families completed informed consent.
Table 2. Descriptive statistics on sample.
| ADHD | Control | Total | |
|---|---|---|---|
|
|
|
|
|
| n = 302 | n = 199 | N = 5481 | |
| Boys n (%) | 204 (67.5) | 96 (48.2) | 321 (58.6)** |
| Ethnic minority n (%) | 78 (25.8) | 54 (27.1) | 144 (26.3) |
| Age | 11.32 (2.93) | 12.5 (3.24) | 11.67 (3.06)** |
| IQ | 110.33 (14.92) | 103.78 (13.90) | 106.2 (14.7)** |
| Family income | 62643 (67080) | 75244 (51109) | 66694 (59532)* |
| ADHD-C n (%) | 192 (63.6) | – | 192 (35) |
| ADHD-PI n (%) | 110 (36.4) | – | 110 (20.1) |
| ODD n (%) | 118 (39.1) | 26 (13.1) | 161 (29.4)** |
| CD n (%) | 18 (6) | 1 (.5) | 19 (3.5)** |
| Inattentive Sx (P+T) | 6.02 (2.34) | .41 (1.04) | 3.77 (3.32)** |
| Hyperactive Sx (P+T) | 6.35 (2.38) | .53 (1.22) | 4.03 (3.44)** |
| Inattentive Sx (P) | 18.03 (5.03) | 3.23 (3.4) | 11.93 (8.41)** |
| Hyperactive Sx (P) | 11.97 (7.23) | 2.04 (2.21) | 7.9 (7.48)** |
| Inattentive Sx (T) | 14.89 (6.89) | 2.36 (3.18) | 9.68 (8.27)** |
| Hyperactive Sx (T) | 9.85 (7.94) | 1.35 (2.36) | 6.37 (7.49)** |
Note:
p<.05.
p<.01, via t-tests or chi-squares.
Forty-seven children were identified as having situational ADHD or were screened out of the study at a later point in time, but were included in study analyses because they had data on ADHD symptoms. ADHD-C = ADHD combined subtype. ADHD-PI = ADHD, predominantly inattentive subtype. ODD = Oppositional-Defiant Disorder. CD = Conduct Disorder. (P+T) = Parent+teacher rated symptoms. (P) = Parent-rated symptoms. (T) = Teacher-rated symptoms.
Recruitment and identification
A broad community-based recruitment strategy was used, with mass mailings to parents in local school districts, public advertisements, as well as flyers at local clinics, to mimic the recruitment strategy of the MTA study (Arnold et al., 1997), while including all ADHD subtypes and adding a typically-developing comparison group. Families who volunteered then passed through a standard multi-gate screening process to identify cases and non-cases eligible for the study. At Stage 1, all families were screened by phone to rule out youth prescribed long-acting psychotropic medication (e.g., antidepressants), neurological impairments, seizure history, head injury with loss of consciousness, other major medical conditions, or a prior diagnosis of mental retardation or autistic disorder, as reported by parent.
At Stage 2, parents and teachers of remaining eligible youth completed the following standardized rating scales: Child Behavior Checklist/Teacher Report Form (CBCL/TRF; Achenbach, 1991), Conners (1997) Rating Scales-Revised, and the ADHD Rating Scale (ADHD-RS; DuPaul, Power, Anastopolous, & Reid, 1998). In addition, parents completed a structured clinical interview to ascertain symptom presence, duration, and impairment. Children completed IQ and achievement testing.
The diagnostic interview used was dependent on the year of data collection. For participants who participated between 1997 and 2001 (N = 218), the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) was completed with the parent by telephone or during on-campus visits. A trained graduate student or advanced undergraduate with at least 10 hours of training administered the DISC-IV. Fidelity to interview procedure was checked by having the interview recorded with 5% reviewed by a certified trainer. For children who were administered the DISC-IV and met duration, onset, and impairment criteria for DSM-IV ADHD, an ‘or’ algorithm was used to establish the diagnostic group and to create the symptom count. Teacher-reported symptoms on the ADHD-RS (i.e., items rated as a ‘2’ or ‘3’ on the 0 to 3 scale) could be added to the parent-endorsed symptom total, up to a maximum of three additional symptoms, to get the total number of symptoms (Lahey et al., 1994). Children failing to meet cut-offs for all parent and teacher ADHD rating scales at the 80th percentile and having four or fewer symptoms of ADHD with the ‘or’ algorithm were considered controls. However, those in the in-between range were retained in the sample for analyses.
For participants who participated from 2002 to 2008, youth and their primary caregiver completed the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-E; Puig-Antich & Ryan, 1986). The data from the interviews and parent and teacher rating scales were then presented to a clinical diagnostic team consisting of a board-certified child psychiatrist and licensed clinical child psychologist. They were allowed to use the same ‘or’ algorithm described above in their diagnostic decision making. Their agreement rates were acceptable for ADHD diagnosis, subtypes, and current ODD and CD (all kappas ≥ .89).
Pooling the data across families that received the KSADS and the DISC was justified based on our analysis of agreement between the two methods in 430 youth for whom a parent completed both a KSADS and a DISC-IV. The two interviews had adequate agreement for total number of symptoms (inattention, ICC = .88; hyperactivity, ICC = .86), presence of six or more symptoms of ADHD (kappa = .79), presence of impairment (kappa = .64), and presence of ADHD (defined as six or more symptoms + cross situational impairment in each interview for purposes of computing agreement; kappa = .79).
Measures
Symptom counts
Maternal report on ADHD symptoms was available via report on diagnostic interview, and maternal and teacher report on ADHD symptoms was available via report on the ADHD-RS. Main study analyses utilized parent and teacher report symptom counts, using parent report on diagnostic interview and teacher report on the ADHD-RS, integrated using the ‘or’ algorithm (as discussed above and in Lahey et al., 1994). The ‘or’ algorithm was modified to avoid over-inclusiveness, as follows: children had to have elevated scores above the 80th percentile on at least one parent and teacher rating scale, and teacher report could add no more than three symptoms to the interview symptom count (similar to the MTA approach). The ‘or’ symptom count was chosen for the primary presentation of results to aid in economy of presentation. Because of controversy over the appropriate algorithm to combine parent and teacher reports, secondary analyses examine within-informant models using report on the ADHD-RS.
Data analysis
A series of confirmatory factor analyses was estimated using the Mplus software package (Muthén & Muthén, 2008). Missingness was minimal in the current study, affecting less than 3% of the sample, and was addressed using pairwise present analysis. The presence of siblings and the resulting non-independence of data points were addressed using the clustering feature of Mplus. Weighted least squares means and variance adjusted (WLSMV) estimation was used.
Model goodness of fit was evaluated using chi-square fit statistics, root mean square error of approximation (RMSEA), and comparative fit index (CFI). Smaller chi-square and RMSEA values and larger CFI values indicate better fit. Generally speaking, nonsignificant chi-square, RMSEA equal to or below .05, and CFI above .9 indicate good fit (Kline, 2005). All fit indices were considered in evaluating model fit, and the best model was determined by the best overall fit indices.
Results
Preliminary analyses: simple models
Simple models were first estimated, and model fit statistics are summarized in Table 3. The one-, two-, and three-factor models all exhibited inadequate fit by our criteria, as indicated by a large, significant chi-square value and an RMSEA value over .10 (one factor: X2[35] = 299.06, p < .01;RMSEA = .11;CFI = .98; two-factor: X2[35] = 299.95, p < .01; RMSEA = .12; CFI = .98; three factor: X2[34] = 292.18, p < .01; RMSEA = .12; CFI = .98).
Table 3. Confirmatory factor analysis fit statistics for parent and teacher ‘or’ algorithm symptom ratings.
| Chi-Square | df | CFI | RMSEA | |
|---|---|---|---|---|
| One-factor model | 299.06** | 35 | .98 | .11 |
| Two-factor model | 299.95** | 35 | .98 | .12 |
| Three-factor model | 292.18** | 34 | .98 | .12 |
| Second-order factor model | 293.03** | 34 | .98 | .12 |
| Bifactor model | 143.18** | 59 | .99 | .05 |
Note:
p < .01.
Primary hypothesis tests: complex models
Second-order factor model
In this model, inattentive and hyperactive-impulsive symptoms loaded onto separate factors, but these two factors in turn defined a higher-order factor, termed ADHD. Thus, this model assumes that ADHD as a diagnostic category satisfactorily accounts for the variation between inattentive and hyperactive-impulsive symptoms. As shown in Table 3 and Figure 1, this model also exhibited unsatisfactory fit, with a large chi-square and an RMSEA over .10 (X2[34] = 293.03, p < .01;CFI = .98; RMSEA = .12).
Bifactor model
In the bifactor model of ADHD, all symptoms were hypothesized to load onto a single general factor, termed ADHD. In addition, inattentive ADHD symptoms and hyperactive-impulsive ADHD symptoms were hypothesized to load onto their own specific factors. While the bifactor model assumes that ADHD symptoms share some common variance (captured by the general ADHD factor), it differs from the second-order factor model in that the two symptom domains are also assumed to capture variance that is unique from the overarching diagnostic category. In the traditional bifactor model, all three latent factors are orthogonal. If that model fit, it would strongly support a multiple-pathway model with separate general and specific factors, or components, of disorder. As an alternative, the two specific factors can be allowed to correlate with the general factor, but remain orthogonal with one another. This model would also support a multiple-pathway model of ADHD, although the relationship of the pathways to the general ADHD factor is more difficult to interpret.
The first (more traditional) bifactor model, with orthogonal general and specific factors, exhibited poor fit (X2[36] = 936.53, p < .01; CFI = .94; RMSEA = .22). The second bifactor model, with two specific factors orthogonal with each other, but allowed to correlate with the general factor, exhibited good fit to the data based on CFI and RMSEA, although the chi-square statistic was significant (X2[59] = 143.18, p<.01; CFI = .99; RMSEA = .05; shown in Figure 2). Thus, this bifactor model exhibited the best fit to the data of the models tested.
Data checks
Maternal versus teacher symptom ratings
As a check, all models were estimated separately for mother and teacher ADHD symptom ratings. Shown in Table 4, these results exhibited the same pattern as that depicted for the prior models that used the ‘or’ algorithm parent and teacher ratings. The bifactor model exhibited the best fit for both mother and teacher ratings.
Table 4. Confirmatory factor analysis fit statistics for mother and teacher symptom ratings.
| Chi-Square | df | CFI | RMSEA | |
|---|---|---|---|---|
| Mother ratings | ||||
| One-factor model | 950.99** | 34 | .90 | .20 |
| Two-factor model | 512.79** | 48 | .95 | .11 |
| Three-factor model | 503.65** | 49 | .95 | .11 |
| Second-order factor model | 512.79** | 48 | .95 | .11 |
| Bifactor model | 324.14** | 57 | .97 | .08 |
| Teacher ratings | ||||
| One-factor model | 759.86** | 19 | .94 | .25 |
| Two-factor model | 488.07** | 36 | .96 | .14 |
| Three-factor model | 468.01** | 37 | .96 | .13 |
| Second-order factor model | 488.07** | 36 | .96 | .14 |
| Bifactor model | 320.95** | 49 | .98 | .09 |
Note:
p<.01.
Three-factor models
In principle, second-order factor and bifactor models can have any number of constituent factors. Therefore, three-factor models of inattention, hyperactivity, and impulsivity were also examined in the second-order factor and bifactor model framework with similar results as the two-factor models depicted earlier. Namely, the bifactor model fit the best, but not as well as the two-factor bifactor model described earlier (second order model: X2[34] = 292.17, p < .01; CFI = .98; RMSEA = .12; bifactor model: X2[52] = 214.95, p < .01; CFI = .99; RMSEA = .08 with orthogonal specific factors; not shown).
Age, sex, and diagnostic differences
Because the loadings of individual symptoms might be expected to vary based on age, sex, or diagnostic status (and all were correlated with one of the factors when included as covariates), possible group differences in symptoms and model fit were examined. Three different fully constrained two-group models (age, sex, diagnosis) were estimated. In these models, all parameters except residual variances were constrained to be equal across the groups. A constrained two-group (age) model exhibited somewhat less than adequate fit to the data (χ2[66] = 191.62; p < .01; CFI = .99; RMSEA = .09). However, once the loadings of ‘close attention’ on the specific inattention factor and ‘sustained metal effort’ on the general ADHD factor were freed in the younger group, fit improved to nearly adequate (χ2[73] = 132.03, p < .01;CFI = .99; RMSEA = .06). A constrained two-group (sex) model also exhibited less than adequate fit to the data (χ2[68] = 211.68, p < .01; CFI = .99; RMSEA = .09). However, once the loading of ‘close attention’ on the specific inattention factor was freed for males, model fit improved to nearly adequate (χ2[74] = 167.75, p < .01; CFI = .99; RMSEA = .07). A constrained two-group (diagnostic status [ADHD vs. control]) model exhibited nearly adequate fit to the data (χ2[32] = 63.4, p < .01;CFI = .97; RMSEA = .06). In all, although there was some variation by age, sex, and diagnostic status in the factor weightings as indicated by the significant covariates, the two-group model analyses suggested that these group differences are relatively minor.
Discussion
The latent structure of ADHD has important research and clinical implications. To this end, the current study evaluated a series of structural models fit to parent- and teacher-rated ADHD symptoms. The primary question was whether ADHD could be best conceptualized as a syndrome with symptom domains that likely have similar etiological inputs and treatment implications (represented by a second-order factor model) or as a common final pathway for dual or multiple etiological inputs with differential treatment implications (represented by a bifactor model). A bifactor model provided the best fit to the data, suggesting that ADHD appears to be comprised of a single factor that captures common variance in inattentive and hyperactive-impulsive symptom domains, as well as two separate inattention and hyperactivity-impulsivity factors that capture unique variance. This model resembles the DSM-IV in suggesting symptom domains are distinct, but differs from the DSM-IV in that it suggests that general ADHD risk and specific risk for inattention and hyperactivity-impulsivity are distinct from one another, with potential implications for distinct etiological inputs, as well as differential assessment and treatment approaches tailored to individual symptom profiles.
This study supports the findings of Toplak et al. (2009), who used a clinic sample. Thus, studies in both clinic-recruited and community-recruited samples support the bifactor model of ADHD. The present study makes an important contribution to the literature by suggesting inadequate fit for a second-order factor model that is most in line with the current DSM-IV conceptualization of ADHD. The superior fit of the bifactor model sheds some light on the previous inconsistencies of confirmatory and exploratory approaches to symptom structure by suggesting that one- and two-factor models may both provide an approximation of ADHD symptom structure. However, a model that allows for one- and two-factor conceptualizations to exist simultaneously appears to provide superior fit.
A bifactor model of ADHD suggests that general risk for ADHD, specific risk for inattention, and specific risk for hyperactivity-impulsivity may need to be assessed separately to provide maximal information about the symptom profile of ADHD for each individual in order to accurately predict risk and outcome. Then, treatment may need to be tailored to the specific constellation of general and/or specific risk that characterizes the individual. For example, general ADHD risk may be best treated with a combination of medication and behavioral therapy. Specific inattention risk may be most effectively treated with medication alone, while specific hyperactivity-impulsivity may be most effectively treated with behavioral therapy.
This more nuanced understanding of the relations among individual ADHD symptoms and symptom domains also has implications for theoretical conceptualization of ADHD. In particular, these findings clarify that item loadings in a clinical sample reflect not a clean two-factor structure, but an ADHD ‘g’ factor, in addition to two specific symptom domain components. All ADHD symptoms loaded significantly on the general ADHD factor. However, five items from the nine-item inattention set (i.e., ‘close attention,’ ‘sustained attention,’ ‘follows through,’ ‘sustained mental effort,’ and ‘easily distractible’) also loaded significantly on the specific inattentive factor, and five items from the nine-item hyperactivity-impulsivity set (i.e., ‘fidgets,’ ‘runs/climbs,’ ‘driven by a motor,’ ‘blurts,’ and ‘interrupts/intrudes’) also loaded significantly on the specific hyperactive-impulsive factor. It appears that while all items index general ADHD liability, other items additionally index specific inattentive or hyperactive-impulsive ADHD liability. Further, inattention appears to be more distinct from the general ADHD factor than hyperactivity-impulsivity, as indicated by the correlations between the ADHD general factor and the specific inattentive and hyperactive-impulsive factors, suggesting it may be most important to assess independently from general ADHD risk. In fact, one might speculate that this suggests that specific inattention may be able to stand alone as a diagnostic category separate from general ADHD and specific hyperactivity-impulsivity (e.g., Barkley, 2006).
At the individual level, this suggests that some children exhibit a general liability for ADHD with evidence of both high inattentive and hyperactive-impulsive symptoms of ADHD, while other children exhibit more specific liability for only specific inattentive or hyperactive-impulsive symptoms. Although this idea could be seen as in line with the current DSM-IV subtypes of ADHD, it could suggest that general and specific forms of ADHD are even more distinct than previously believed. Perhaps most importantly, the finding suggests that the considerable variability in the pattern of symptom endorsement seen between children currently classified as ADHD in DSM-IV merits increased scrutiny.
The present results suggest important implications for the scientific pursuit of biological and genetic underpinnings of ADHD. In particular, the current results are in line with multiple-pathway models that posit two or more mechanistic inputs via the two symptom domains (Nigg, 2006; Sonuga-Barke, 2005), but additionally suggest a general, or ‘g,’ component that highlights the additive nature of the two symptom domains. Theoretical models may require modification to accommodate this insight.
There are likely both distinct and shared etiological inputs to the disorder (Levy, Hay, & Bennett, 2006). For example, one set of genes may confer risk for general ADHD, while a different set of genes specifically confers risk for inattention, and negative environmental experiences specifically confer risk for hyperactivity-impulsivity. This interpretation of the bifactor model is consistent with previous behavioral genetic work suggesting both (a) etiological overlap between inattention and hyperactivity-impulsivity (the ‘g’ factor) and (b) coexisting specific genetic and environmental effects on inattention and specific environmental effects on hyperactivity-impulsivity (the ‘s’ factors; Levy, McStephen, & Hay, 2001; McLoughlin, Ronald, Kuntsi, Asherton, & Plomin, 2007).
Despite the current study's support for a bifactor model, the data also suggest a need for further exploration of alternative models of ADHD. Although the bifactor model of ADHD tested in the current study provided the best fit to the data of all other models tested, it did not exhibit completely adequate fit. In addition, there is a need for further consideration of possible developmental differences and sex effects in the current models, although initial checks suggested that the bifactor model of ADHD symptom structure held adequately, if not perfectly, across age range and sex. Possible longitudinal changes in this structure should be explored, particularly between childhood and adulthood, since general ADHD and specific inattention and hyperactivity-impulsivity latent factors provide promising avenues for exploring stability and change in ADHD across development when normative levels of some behaviors markedly change and some DSM-IV symptoms are considered developmentally inappropriate. The bifactor model may be helpful for evaluation of heterotypical continuity across development via examination of differential stability of the general and specific factors and individual item weights at different ages.
Since the present study examined a community-recruited sample and Toplak et al. (2009) used a clinical sample, confirmation is now needed within a general population sample. Further validation should also occur via examination of psychological, family, and biological correlates of these factors with the idea that the general and specific ADHD factors should show somewhat distinct correlates. Other models (e.g., models of ADHD and common comorbid disorders; see Krueger et al., 2002, 2007) could be tested, but were outside the scope of this paper.
Overall, a bifactor model of ADHD with a coexisting general ADHD factor and specific, unique inattentive and hyperactive-impulsive symptom domain factors was best supported. This model helps explain the heterogeneous behavioral presentation of individuals with ADHD. General, inattentive, and hyperactive-impulsive ADHD symptoms may have different, partially dissociable, etiological inputs and correlates, and multiple-mechanism models of ADHD should receive increased attention as viable candidates for explaining the structure of ADHD. Further, comprehensive assessment of specific inattention, specific hyperactivity-impulsivity, and general ADHD symptoms should be emphasized in clinical assessment with possible implications for treatment and prediction of child outcomes.
Key points.
Attention-deficit/hyperactivity disorder (ADHD) is a heterogeneous behavioral disorder, but the best way to describe this heterogeneity remains unclear.
Formal testing of structural models of ADHD using modern methods (e.g., second-order factor and bifactor models) has been largely lacking.
A bifactor model with distinct factors of inattention and hyperactivity-impulsivity fit best in a community-recruited sample of children and adolescents with ADHD.
This finding supports recent multi-component models of ADHD.
A bifactor model of ADHD helps explain the heterogeneous clinical presentation of individuals with this syndrome and suggests the need for comprehensive clinical assessment of these domains.
Acknowledgments
This research was supported by NIH National Institute of Mental Health Grant R01-MH63146, MH59105, and MH70542 to Joel Nigg. We are indebted to the families and staff who made this study possible.
Footnotes
Related to multitrait-multimethod models (Campbell & Fiske, 1959), the bifactor model, also called hierarchical model, was introduced to methodologists decades ago (Holzinger & Swineford, 1937). However, it was not introduced to the psychopathology field until more recently (Gibbons & Hedeker, 1992).
Conflict of interest statement: No conflicts declared.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Bernstein A, Dumenci L. DSM-oriented scales and statistically based syndromes for ages 18 to 59: Linking taxonomic paradigms to facilitate multitaxonomic approaches. Journal of Personality Assessment. 2005;84:49–63. doi: 10.1207/s15327752jpa8401_10. [DOI] [PubMed] [Google Scholar]
- Amador-Campos JA, Forns-Santacana M, Martorell-Balanzo B, Guardia-Olmos J, Pero-Cebollero M. Confirmatory factor analysis of parents' and teachers' ratings of DSM-IV symptoms of attention deficit hyperactivity disorder in a Spanish sample. Psychological Reports. 2005;97:847–860. doi: 10.2466/pr0.97.3.847-860. [DOI] [PubMed] [Google Scholar]
- Amador-Campos JA, Forns-Santacana M, Martorell-Balanzo B, Guardia-Olmos J, Pero-Cebollero M. DSM-IV Attention Deficit Hyperactivity Disorder symptoms: Agreement between informants in prevalence and factor structure at different ages. Journal of Psychopathology and Behavioral Assessment. 2006;28:23–32. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th, text rev. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Arnold LE, Abikoff HB, Cantwell DP, Conners CK, Elliott G, Greenhill LL, et al. National Institute of Mental Health collaborative multimodal treatment study of children with ADHD (the MTA). Design challenges and choices. Archives of General Psychiatry. 1997;54:865–870. doi: 10.1001/archpsyc.1997.01830210113015. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 3rd. New York: Guilford Press; 2006. [Google Scholar]
- Bauermeister JJ, Alegria M, Bird HR, Rubio-Stipec M, et al. Are attentional-hyperactivity deficits unidimensioanl or multidimensional syndromes? Empircal findings from a community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:423–431. doi: 10.1097/00004583-199205000-00007. [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ, Bird HR, Canino G, Rubio-Stipec M, et al. Dimensions of attention deficit hyperactivity disorder: Findings from teacher and parent reports in a community sample. Journal of Clinical Child Psychology. 1995;24:264–271. [Google Scholar]
- Burns GL, Boe B, Walsh JA, Sommers-Flanagan R, Teegarden LA. A confirmatory factor analysis on the DSM-IV ADHD and ODD symptoms: What is the best model for the organization of these symptoms? Journal of Abnormal Child Psychology. 2001;29:339–349. doi: 10.1023/a:1010314030025. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Owen SM, Snell J. Internal validity of attention deficit hyperactivity disorder, oppositional defiant disorder, and overt conduct disorder symptoms in young children: Implications from teacher ratings for a dimensional approach to symptom validity. Journal of Clinical Child Psychology. 1997a;26:266–275. doi: 10.1207/s15374424jccp2603_5. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Patterson DR, Holte CS, Sommers-Flanagan R, Parker CM. Internal validity of the disruptive behavior disorder symptoms: Implications from parent ratings for a dimensional approach to symptom validity. Journal of Abnormal Child Psychology. 1997b;25:307–319. doi: 10.1023/a:1025764403506. [DOI] [PubMed] [Google Scholar]
- Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin. 1959;56:81–105. [PubMed] [Google Scholar]
- Chen FF, West SG, Sousa KH. A comparison of bifactor and second-order factor models of quality of life. Multivariate Behavioral Research. 2006;41:189–225. doi: 10.1207/s15327906mbr4102_5. [DOI] [PubMed] [Google Scholar]
- Conners CK. Conners Rating Scales–Revised. Toronto: Multi-Health Systems, Inc; 1997. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopolous AD, Reid R. ADHD Rating Scale—IV: Checklists, norms, and clinical interpretation. New York: Guilford Press; 1998. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey KE, Ikeda MJ. Teacher ratings of attention deficit hyperactivity disorder symptoms: Factor structure and normative data. Psychological Assessment. 1997;9:436–444. doi: 10.1037/pas0000166. [DOI] [PubMed] [Google Scholar]
- Dumenci L, McConaughy SH, Achenbach TM. A hierarchical three-factor model of inattention-hyperactivity-impulsivity derived from the attention problems syndrome of the teacher's report form. School Psychology Review. 2004;33:287–301. [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: Driving abilities, safe driving behavior, and adverse driving outcomes. Accident Analysis and Prevention. 2007;39:94–105. doi: 10.1016/j.aap.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker DR. Full-information item bi-factor analysis. Psychometrika. 1992;57:423–436. [Google Scholar]
- Gomez R, Burns GL, Walsh JA, Hafetz N. A multitrait-multisource confirmatory factor analytic approach to the construct validity of ADHD and ODD rating scales with Malaysian children. Journal of Abnormal Child Psychology. 2005;33:241–254. doi: 10.1007/s10802-005-1831-1. [DOI] [PubMed] [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Applegate B, Frick PJ. Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Holzinger KJ, Swineford F. The bi-factor method. Psychmetrika. 1937;2:41–54. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd. New York: Guilford Press; 2005. [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Personality. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, et al. DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Schaughency EA, Atkins MS, et al. Dimensions and types of attention deficit disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:330–335. doi: 10.1097/00004583-198805000-00011. [DOI] [PubMed] [Google Scholar]
- Levy F, Hay DA, Bennett KS. Genetics of attention deficit hyperactivity disorder: A current review and future prospects. International Journal of Disability, Development and Education. 2006;53:5–20. [Google Scholar]
- Levy F, Hay DA, McStephen M, Wood CH, Wald-man I. Attention-deficit/hyperactivity disorder: A category or a continuum? Genetic analysis of a large-scale twin study. American Academy of Child and Adolescent Psychiatry. 1997;36:737–744. doi: 10.1097/00004583-199706000-00009. [DOI] [PubMed] [Google Scholar]
- Levy F, McStephen M, Hay DA. The diagnostic genetics of ADHD symptoms and subtypes. In: Levy F, Hay DA, editors. Attention, genes and ADHD. Hove, East Sussex: Brunner-Routledge; 2001. pp. 35–57. [Google Scholar]
- Massetti GM, Lahey BB, Pelham WE, Loney J, Ehrhardt A, Lee SS, Kipp H. Academic achievement over 8 years among children who met modified criteria for attention-deficit/hyperactivity disorder at 4–6 years of age. Journal of Abnormal Child Psychology. 2008;36:399–410. doi: 10.1007/s10802-007-9186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoughlin G, Ronald A, Kuntsi J, Asherton P, Plomin R. Genetic support for the dual nature of attention deficit hyperactivity disorder: Substantial genetic overlap between the inattentive and hyperactive-impulsive components. Journal of Abnormal Child Psychology. 2007;35:999–1008. doi: 10.1007/s10802-007-9149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. fourth. Los Angeles, CA: Muthén&Muthén; 1998–2008. [Google Scholar]
- Nigg JT. What cchat goes wrong and why. New York: Guilford Press; 2006. [Google Scholar]
- Nigg JT, Goldsmith HH, Sachek J. Temperament and attention deficit hyperactivity disorder: The development of a multiple-pathway model. Journal of Clinical Child and Adolescent Psychology. 2004;33:42–53. doi: 10.1207/S15374424JCCP3301_5. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Willcutt EG, Doyle AE, Sonuga-Barke EJS. Causal heterogeneity in attention-deficit/hyperactivity disorder: Do we need neuropsychologically impaired subtypes? Biological Psychiatry. 2005;57:1224–1230. doi: 10.1016/j.biopsych.2004.08.025. [DOI] [PubMed] [Google Scholar]
- Pillow DR, Pelham WE, Hoza B, Molina BSG, Stultz CH. Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. Journal of Abnormal Child Psychology. 1998;26:293–309. doi: 10.1023/a:1022658618368. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Ryan N. Kiddie Schedule for Affective Disorders and Schizophrenia. Pittsburgh, PA: Western Psychiatric Institute; 1986. [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan MK, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): Description, differences from previous versions and reliability of some common diagnoses. Journal of American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shaw P, Gornick M, Lerch J, Addington A, Seal J, Greenstein D, et al. Polymorphisms of the dopamine D4 receptor, clinical outcome, and cortical structure in attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2007;64:921–931. doi: 10.1001/archpsyc.64.8.921. [DOI] [PubMed] [Google Scholar]
- Sherman DK, Iacono WG, McGue MK. Attention-deficit hyperactivity disorder dimensions: A twin study of inattention and impulsivity-hyperactivity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:745–753. doi: 10.1097/00004583-199706000-00010. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Psychological heterogeneity in AD/HD – a dual pathway model of behavior and cognition. Behavioural Brain Research. 2002;130:29–36. doi: 10.1016/s0166-4328(01)00432-6. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Causal models of attention-deficit/hyperactivity disorder: From common simple deficits to multiple developmental pathways. Biological Psychiatry. 2005;57:1231–1238. doi: 10.1016/j.biopsych.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Auerbach J, Campbell SB, Daley D, Thompson M. Varieties of preschool hyperactivity: Multiple pathways from risk to disorder. Developmental Science. 2005;8:141–150. doi: 10.1111/j.1467-7687.2005.00401.x. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Pitch A, Flora DB, Iwenofu L, Ghelani K, Jain U, Tannock R. The unity and diversity of inattention and hyperactivity-impulsivity in ADHD: Evidence for a general factor with separable dimensions. Journal of Abnormal Child Psychology. 2009;37:1137–1150. doi: 10.1007/s10802-009-9336-y. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Lambert EW, Baumgaertel A, Garcia-Tornel S, et al. Teachers' screening for attention deficit/hyperactivity disorder: Comparing multinational samples on teacher ratings of ADHD. Journal of Abnormal Child Psychology. 2003;31:445–555. doi: 10.1023/a:1023847719796. [DOI] [PubMed] [Google Scholar]