Abstract
Nutrition plays an important role in osteoporosis prevention and treatment. Substantial progress in both laboratory analyses and clinical use of biochemical markers has modified the strategy of anti-osteoporotic drug development. The present review examines the use of biochemical markers in clinical research aimed at characterising the influence of foods or nutrients on bone metabolism. The two types of markers are: (i) specific hormonal factors related to bone; and (ii) bone turnover markers (BTM) that reflect bone cell metabolism. Of the former, vitamin D metabolites, parathyroid hormone, and insulin-like growth factor-I indicate responses to variations in the supply of bone-related nutrients, such as vitamin D, Ca, inorganic phosphate and protein. Thus modification in bone remodelling, the key process upon which both pharmaceutical agents and nutrients exert their anti-catabolic or anabolic actions, is revealed. Circulating BTM reflect either osteoclastic resorption or osteoblastic formation. Intervention with pharmacological agents showed that early changes in BTM predicted bone loss and subsequent osteoporotic fracture risk. New trials have documented the influence of nutrition on bone-tropic hormonal factors and BTM in adults, including situations of body-weight change, such as anorexia nervosa, and weight loss by obese subjects. In osteoporosis-prevention studies involving dietary manipulation, randomised cross-over trials are best suited to evaluate influences on bone metabolism, and insight into effects on bone metabolism may be gained within a relatively short time when biochemical markers are monitored.
Keywords: Bone-related hormones, Bone turnover markers, Clinical nutrition trials
Introduction
The aim of the present report is to review how biochemical markers can be used to evaluate the potential benefit of foods or nutrients on adult bone health and in primary and secondary osteoporosis prevention. Nutrition and physical activity are key behavioural determinants of the development and progression of several chronic diseases, including osteoporosis. In primary prevention, nutrition combined with moderate physical activity plays an important role in attenuating age-related bone loss. In secondary prevention, adequate nutrition is adjuvant to specific anti-osteoporotic medications, thus enabling their full therapeutic effects.
This review focuses on the clinical application of biochemical analyses that can respond to nutritional interventions aimed at either preserving bone integrity or attenuating bone loss in adults.
Effects of foods and nutrients on Ca and inorganic phosphate (Pi) economy( 1 ) can be measured using bone-related circulating hormonal markers, such as vitamin D metabolites( 2 ), parathyroid hormone (PTH)( 3 , 4 ) and insulin-like growth factor (IGF)-I( 5 ), as well as bone turnover markers (BTM) that reflect bone formation and resorption( 6 – 9 ).
New findings on BTM have improved how they are viewed in the design, follow-up and interpretation of clinical trial outcomes, particularly in postmenopausal women and the elderly( 8 , 9 ). Indeed, BTM changes can predict the later influence of pharmaceutical agents on bone mineral density (BMD)/content and fragility fractures( 6 – 9 ). This will be discussed in the context of bone health-related claims as they relate to evidence-based knowledge of nutritional benefits. Examples of clinical trials are presented that document how nutrients influence bone-trophic hormones and biochemical markers of bone remodelling. Finally, appropriate study designs using both biochemical markers and new tools for assessing bone structure and function, as well as biomechanical properties, will be discussed, taking into account distinct adult populations.
Osteoporosis, a major health problem
Osteoporosis is a systemic skeletal disease characterised by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture that worsens with ageing( 10 ). Osteoporosis causes more than 8·9 million fractures annually worldwide( 10 ). The lifetime risk for wrist, hip or vertebral fracture is estimated to be 30 to 40 % in developed countries. Epidemiological studies in both the USA and UK indicate that one in two women aged 50 years or older will have an osteoporotic fracture in their remaining life; for men it is one in five( 11 ). The most serious osteoporotic fracture, at the proximal femur, typically results when subjects having an intrinsic bone fragility caused by both reduced mineral density and impaired structural design have fallen. These fractures show an exponential age-related increase and have a severe detrimental effect on the health of elderly populations( 10 , 11 ). Fragility fractures in elderly individuals are the long-term pathological consequence of an imbalance between bone resorption and bone formation leading to bone loss with micro-structural alterations of both cortical and trabecular structures( 10 , 11 ).
Therapeutic options and limitations
There are many efficacious pharmaceutical options that have been shown, in large and well-designed randomised controlled trials (RCT), to significantly reduce the risk of fracture in postmenopausal women and the elderly( 12 , 13 ). Nevertheless, insufficient compliance in terms of both adherence and persistence to drug prescription limits their effectiveness for the management of individual patients in the real-world conditions of medical practice( 14 – 17 ).
It is relevant to note that in the stepwise drug development phases, virtually all testing of major anti-osteoporotic medications relied on BTM measurement to assess efficacy.
Evidence-based criteria in osteoporosis management
Clinical evidence arises from the analysis of various research approaches with the aim of proposing the most reliable recommendations for practical disease management. The RCT is at the top of the strength-of-evidence hierarchy. These RCT usually measure non-vertebral fractures, and require that thousands of patients be followed for at least 3 years to reach a sufficient statistical power. However, some well-designed RCT testing specific pharmaceutical agents in postmenopausal women have failed to demonstrate efficacy for preventing hip fracture( 12 ). The incidence of hip fracture depends not only on the drug efficacy for improving bone structure and metabolism, but also on extra-skeletal factors, mainly those related to the occurrence and circumstances of falling. This makes hip fracture a stochastic event, largely independent of bone-active medications. Furthermore, RCT for osteoporosis typically provide both treatment and placebo groups with sufficient Ca and vitamin D, which may have independent benefits on bone metabolism and attenuate the potential effect size on hip fracture reduction.
Concept of evidence-based nutrition in bone health and osteoporosis
Clinical research related to the impact of foods and/or nutrients on bone metabolism and structure is hampered by the difficulty to reach a level of evidence( 18 , 19 ) similar to that required of clinical trials that test pharmaceutical drugs for osteoporosis management( 20 – 22 ). It is difficult to prove the efficacy of drugs for preventing fragility fracture using large RCT designed for this purpose (see below), but it is even more challenging to use the RCT approach to evaluate whether foods or nutrients can reduce the risk of fragility fracture( 18 , 19 ). There is a major difference in the level of strength evidence required for foods or nutrients as compared with drugs, to evaluate not only benefits but also risks( 23 – 26 ). As explicitly stated by Heaney & Blumberg, ‘…we cannot get RCT-level evidence from many, and perhaps most, nutritional questions…’( 25 ). Therapeutic decisions using anti-osteoporotic drugs require evidence based on high-quality RCT that have as their main outcome the reduction of fragility fractures( 20 ). Inferences are weakened when studies rely on surrogate endpoints such as BMD or BTM( 20 ). Testing the efficacy of a food or nutrient with the reduction of hip fracture risk as the main outcome will probably never be amenable to RCT because it would require that thousands of patients remain compliant to the intervention for at least 3 to 4 years( 18 , 19 , 23 ). Industry is unlikely to sponsor these large RCT because, in contrast to drugs, marketing the products is not dependent on the results of RCT. However, as compared with foods or nutrients, the risk:benefit ratio is much greater with drugs, as they may cause more severe adverse side effects( 18 , 19 , 24 , 25 ).
In the nutrition field, valuable information could be obtained from RCT that have BTM endpoints reflecting bone metabolism. The change in BTM can be detected at a shorter time than the time for assessing effects on fragility fracture rate. The validity of results obtained from short-term RCT is strengthened by preclinical studies carried out in reliable animal models of human osteoporosis( 27 – 31 ). The next sections will deal with the scientific basis underlying these concepts.
Bone-related biomarkers: biochemical analyses and clinical application
Both hormonal factors and biomarkers of bone remodelling can be useful to assess the baseline status and the response to an intervention in the context of prevention or treatment of osteoporosis.
Bone mass can be estimated by measuring BMD, i.e. areal BMD (aBMD) using dual-energy X-ray absorptiometry (DXA). While low aBMD is an important determinant of fracture risk, its measurement does not capture all the risk factors for fracture( 32 ). In fact, up to half of patients with incident fractures have baseline spinal or hip aBMD assessed by DXA above the diagnostic threshold of osteoporosis defined as a T-score of − 2·5 sd or more below the average value of young healthy adults (i.e. WHO definition of osteoporosis)( 33 , 34 ). Using peripheral measurement devices, 82 % of postmenopausal women with fracture had T scores better than − 2·5( 35 ). Furthermore, there is increasing evidence that the decision to use pharmacological intervention for the prevention of fracture should be based on the fracture probability rather than only on the presence of osteoporosis as defined by aBMD T-score( 32 ). Therefore, in selecting patients for treatment, the risk of fracture in individual subjects is now calculated by the use of algorithms which include a number of recognised independent risk factors for fracture in addition to aBMD, such as age, sex, BMI, family history, past history of fracture, secondary causes of osteoporosis such as rheumatoid arthritis, use of medications such as glucocorticoids, smoking and excessive alcohol intake( 32 ). FRAX® (WHO Fracture Risk Assessment Tool) is such a fracture risk calculator for the next 10 years (www.shef.ac.uk/FRAX/).
Bone-related circulating hormonal factors
Hormonal changes to insufficient supply of calcium, vitamin D and protein
The main consequence of vitamin D insufficiency, as expressed by a low circulating level of 25-hydroxyvitamin D (25(OH)D), is a decrease in the intestinal absorption of both Ca and Pi. The reduction in the supply of Ca from the intestinal tract leads to an increase in the production of PTH to, at least partially, compensate for hypocalcaemia by stimulating both tubular Ca reabsorption and osteoclastic bone resorption. The secondary hyperparathyroidism also contributes to the associated hypophosphataemia resulting from the reduced tubular Pi reabsorption.
When associated with a deficiency of protein, as expressed by a low serum level of the anabolic agent IGF-I, osteoblastic bone formation rate no longer is matched to osteoclastic bone resorption rate. Moreover, insufficient dietary protein, in concert with insufficient vitamin D status, results in low intestinal Ca absorption. At the kidney, the reabsorption of Pi and the synthesis of the active metabolite of vitamin D, 1,25-dihydroxyvitamin D, tend also to be depressed. Overall, the insufficient dietary supply of these bone-trophic nutrients leads to an uncoupling between the resorption and the formation rate of the bone mineralised organic matrix that favours resorption. Intermediate and long-term possible consequences are measurable bone loss, by DXA or by high-resolution peripheral computed tomography( 36 ) and increased risk of fragility fracture.
In the course of dietary interventions aimed at correcting these nutrient insufficiencies, reliable biochemical assays are available to monitor changes in serum levels of 25(OH)D, PTH and IGF-I. In order to link these hormonal changes to the response of bone metabolism, BTM can concurrently be measured during the dietary intervention trial (see below).
Biochemical determination of bone-trophic hormonal factors: parathyroid hormone
A recommendation has been made to establish reference ranges for serum PTH in vitamin D-replete healthy individuals( 37 ), and to measure PTH in postmenopausal osteoporotic women to exclude secondary osteoporosis due to primary hyperparathyroidism( 3 , 38 ). Further, secondary hyperparathyroidism resulting from inadequate Ca intake and/or vitamin D deficiency, leading to an increase in bone resorption, is thus an important determinant of hip fractures in the elderly( 39 – 41 ). It has been shown by several investigators that acute oral Ca load or longer-term Ca supplementation (i.e. fortified dairy products) have favourable effects on bone metabolism by decreasing PTH and bone resorption markers( 42 , 43 ).
Biochemical determination of bone-trophic hormonal factors: 25-hydroxyvitamin D
The measurement of serum 25(OH)D is the best assessment of vitamin D status. The level associated with optimal suppression of circulating PTH levels has been used to define criteria for vitamin D insufficiency, because of the inverse relationship between serum 25(OH)D and PTH. However, this relationship may be influenced by age, Ca intake, physical inactivity, renal function, ethnicity and other factors. Furthermore, the use of different assays for 25(OH)D and PTH( 44 , 45 ) may also influence the apparent threshold of 25(OH)D concentration at which secondary hyperparathyroidism occurs. Conservatively, a 25(OH)D level of 50 nmol/l (20 ng/ml) is considered as vitamin D sufficient, representing a level above which there is no further suppression of PTH, not much further reduction in BTM, and not much further improvement of muscle function( 46 ). The Institute of Medicine also considers that serum levels of vitamin D above 50 nmol/l are the level that is needed for good bone health for practically all individuals, and set a recommended daily intake of 600 IU/d for children and adults and 800 IU for women and men 71 years or older based on this cut-off( 47 ). However, more recently, the clinical practice guidelines of the Endocrine Society defined vitamin D deficiency as 25(OH)D levels below 50 nmol/l (20 ng/ml) and vitamin D sufficiency as 25(OH)D levels greater than 75 nmol/l (30 ng/ml)( 48 ). In a cross-sectional analysis (National Health and Nutrition Survey (NHANES) 2003–2006) in the US population, maximum PTH suppression expected to occur when vitamin D is sufficient, corresponding to the zero slope between 25(OH)D and PTH, did not occur until a serum 25(OH)D level of approximately 100–125 nmol/l (40–50 ng/ml)( 49 ). Debate about the optimal vitamin D status continues( 49 – 51 ). There is evidence that Ca in combination with vitamin D supplementation reduces the risk of fracture( 52 – 55 ), bone loss( 56 ) and non-vertebral fracture risk( 52 ); these effects are more efficacious at 800 IU/d (20 μg/d) than 400 IU/d (10 μg/d).
Biochemical determination of bone-trophic hormonal factors: insulin-like growth factor-I
Measurement of serum IGF-I is an important tool with growth hormone (GH) not only in the diagnosis of various stature disorders( 57 ), but also as a nutritional marker, particularly of protein intake( 58 , 59 ). IGF-I and GH are regulators of bone homeostasis and are important for the acquisition of bone mass during adolescence, for the achievement of peak bone mass and for the maintenance of skeletal architecture during adult life( 60 , 61 ). Although GH may act directly on skeletal cells, most of its effects are mediated by IGF-I, which is present in the systemic circulation. Systemic IGF-I is synthesised in the liver under the influence of GH. IGF-I is also produced by a variety of cell types and acts in a paracrine fashion in many tissues. Availability of IGF-I is regulated by IGF binding proteins (IGFBP). Serum IGF-I levels are associated with bone mass. IGF-I levels peak at puberty when bone acquisition is maximal but levels of GH, IGF-I, and some IGFBP that regulate IGF activity decrease with age( 61 – 63 ). This decline in GH and IGF-I secretion has been correlated with bone loss in postmenopausal women. A relationship between IGF-I levels and fracture risk has also been reported( 64 , 65 ). However, it is not entirely clear how IGF-I is involved in the pathogenesis of osteoporosis, as serum IGF-I levels are strongly influenced by catabolic states, undernutrition and advanced age, all factors that increase the risk for fracture.
Dietary proteins influence both the production and action of IGF-I. Protein restriction is associated with reduced IGF-I levels by inducing a resistance to the GH action in the liver, and by an increased IGF-I metabolism. Decreased IGF-I levels are observed in states of undernutrition (i.e. also in anorexia nervosa). On the other hand, increased protein intake can prevent the decrease in IGF-I in hypoenergetic states. Experimental and clinical observational data suggest that IGF-I plays an important role in the pathophysiology of osteoporosis, osteoporotic fractures and its complications. Correcting altered IGF-I in the elderly by protein replenishment may favourably influence not only bone mass, but also muscle mass and strength that are important determinants for the risk of falls. The changes of IGF-I levels in nutrition-related changes in body weight are described below.
Bone turnover markers
Importance of bone remodelling in osteoporosis
Bone remodelling is an important process that continuously renews the cortical and trabecular envelopes throughout life. It repairs micro-damage, maintains mineral homeostasis and ensures mechanical competence by modifying the micro-architecture. Bone remodelling is regulated by a variety of systemic and local factors as well as by nutritional factors (Fig. 1). Bone remodelling follows a sequence of events that includes activation, recruitment of osteoclasts to begin resorption, degradation and removal of bone, reversal, and formation of new bone by osteoblasts (Fig. 1). After this phase, a quiescent or resting period occurs. Remodelling begins with release of cytokines from osteoblast precursors, leading to recruitment of osteoclast precursors, which differentiate in multinucleated osteoclasts and subsequently attach to the bone surface. Resorption of the skeletal matrix releases growth factors such as IGF-I and transforming growth factor-β, which recruit lining cells and early osteoblast precursors that eventually form new bone (Fig. 1). Osteoblasts that do not undergo apoptosis remain on the bone surface as lining cells or become entrapped as osteocytes into the new bone matrix. These osteocytes respond to gravitational forces and can signal to lining cells to initiate remodelling. Antiresorptive and anabolic agents influence bone structure by affecting remodelling. Likewise, supply in Ca, vitamin D and protein influences bone remodelling. The presence of Ca and vitamin D inhibits bone resorption, and protein stimulates bone formation (Fig. 1). Ca, Pi and vitamin D are necessary for adequate mineralisation of the newly formed bone matrix (Fig. 1).
Fig. 1.
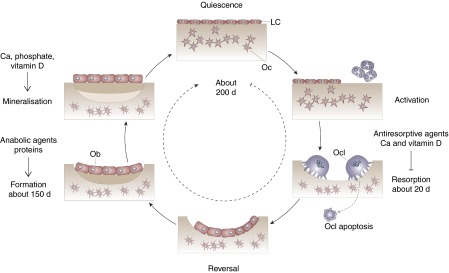
Bone remodelling cycle. Bone turnover follows a sequence of events that includes activation, recruitment of osteoclasts (Ocl) to begin resorption, degradation and removal of bone, reversal, and formation of new bone by osteoblasts (Ob). After this phase a quiescent or resting period occurs. LC, lining cell; Oc, osteocyte.
In young adulthood, the amount of bone removed by the osteoclasts is equal to the amount of bone formed by the osteoblasts, so that bone mass is maintained. After the menopause and with ageing in both sexes, there is a progressive bone loss due to an imbalance between bone resorption and formation.
There is a substantial body of evidence that accelerated bone turnover is associated with a higher risk of fracture, independent of other parameters such as age or BMD (see below). BTM are not included in the fracture risk calculator (FRAX®), mainly for the reason that their relationships with other established risk factors included in the risk calculator are not clarified and because different markers and different methodologies for their assessment have been used across studies. This has led to the recommendation for the standardisation of BTM measurements in future studies and it is suggested that serum carboxy terminal telopeptide of collagen type I (s-CTX) is used as the reference bone resorption marker and serum procollagen type I N-terminal propeptide (sPINP) as the reference bone formation marker, measured by standardised assays( 66 ).
Bone markers reflecting bone formation and bone resorption
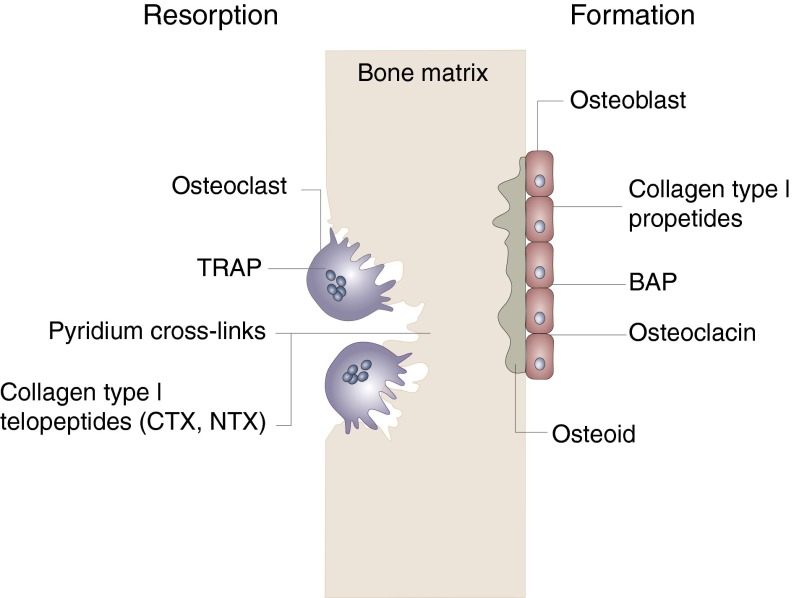
The BTM can be divided into two groups: markers of resorption and markers of formation (Fig. 2). The principal, specific markers of bone formation, measured in serum by immunoassays, are bone alkaline phosphatase (BAP), osteocalcin (OC) and PINP. Most assays are now adapted to automated platforms( 7 ) (Fig. 2). Markers of bone resorption are the pyridinium cross-links (pyridinoline and deoxypyridinoline) and their associated peptides (telopeptides), released during collagen breakdown( 6 ). Markers of osteoclast number include tartrate-resistant acid phosphatase isoenzyme 5b (TRAP 5b), the osteoclast-specific isoform of total TRAP, and, potentially, cathepsin K (Fig. 2). These enzymes are expressed and released by osteoclasts( 67 ). TRAP 5b is the most commonly used marker of osteoclast number.
Fig. 2.
Diagram of the relationship between bone resorption or formation and bone turnover markers. On the resorption side, tartrate-resistant acid phosphatase (TRAP) reflects osteoclast number and activity, whereas pyridium cross-links, carboxy terminal telopeptide (CTX) and N-terminal telopeptide (NTX) are markers of bone matrix resorption. On the formation side, collagen type I propeptides, such as procollagen type I N-terminal propeptide (PINP), bone alkaline phosphatase (BAP) and osteocalcin reflect mainly osteoblastic bone formation. Osteoid corresponds to the non-mineralised bone matrix.
TRAP 5b is predominantly expressed by osteoclasts, and immunoassays to detect this isoform have been developed( 68 – 70 ). In absolute terms, the response of TRAP 5b to antiresorptive therapy is not as great as the response of s-CTX, but within-subject variability is significantly lower. TRAP 5b has a lower diurnal variability than s-CTX and lower acute effect of feeding, possibly due to a longer circulating half-life, making it less susceptible to short-term influences( 71 ). Furthermore, TRAP 5b is not cleared by the kidney, and thus does not accumulate in renal failure( 69 , 71 ).
Predictive value of early changes in bone markers in response to pharmaceutical agents on later effects on bone mineral density/content and fragility fractures: bone turnover markers and the rate of bone loss
There is evidence that bone turnover increases rapidly after menopause and persists for up to 40 years( 72 , 73 ). In postmenopausal women bone turnover rate accounts for >50 % of the variation in bone mass, whereas in premenopausal women it is 0–10 %( 74 , 75 ).
Several prospective studies have demonstrated correlations between levels of BTM and rates of bone loss assessed by serial measurement of aBMD or bone mineral content at different skeletal sites over a time period spanning 13 years( 76 ). These studies support an inverse relationship between BTM and aBMD. This inverse relationship becomes stronger with advancing age and the relationship is significantly stronger for resorption markers than for formation markers, due to the fact that the increase of bone resorption with ageing is greater than the increase in bone formation( 77 ). However, this inverse correlation between BTM and aBMD does not seem to apply to all skeletal sites. A significant correlation between the rate of turnover and rate of bone loss at the hip or radius has been demonstrated in postmenopausal women, but not for the bone loss at the spine( 78 , 79 ). Extra-skeletal calcification and/or compression fracture occurring with advancing age can overestimate aBMD measurements at the spine. There is also evidence indicating that bone resorption markers can detect ‘rapid losers’ (>3 % loss in aBMD per year) in a follow-up period of 2–12 years( 80 – 82 ). At the present time a single measurement of a biochemical marker cannot predict the absolute rate of bone loss in a single individual. However, increased BTM can be regarded as a risk factor for rapid bone loss.
Predictive value of early changes in bone markers in response to pharmaceutical agents on later effects on bone mineral density/content and fragility fractures: bone turnover markers and fracture risk
BTM may be useful in the assessment of fracture risk. Findings of prospective studies have shown that BTM of resorption predict fracture risk in postmenopausal women and in men (Table 1)( 74 , 83 – 89 ). In five prospective studies of postmenopausal women (Epidemiology of Osteoporosis (EPIDOS), Rotterdam, Os de Femmes de Lyon (OFELY), Hawaii Osteoporosis Study (HOS), and Malmö Osteoporosis Prospective Risk Assessment (OPRA)), there were significant associations of baseline levels of urinary or s-CTX, urinary free deoxypyridinoline, or serum TRAP 5b with fracture risk( 74 , 83 – 87 ) (Table 1). An increase of these markers above the premenopausal range was associated, after adjustment for aBMD, with a twofold increase in risk for hip, vertebral and non-vertebral fractures, over a follow-up period of 1.8 to 5 years. The results for the relationship between bone formation markers and fracture risk are not consistent. In the French cohort study of elderly women (EPIDOS), no significant relationship between OC or BAP and fracture risk could be demonstrated during a 2-year follow-up. In contrast, in younger healthy postmenopausal women (OFELY and HOS cohorts), a significant association was found between increased BAP serum levels and risk of vertebral as well as non-vertebral fracture( 74 , 83 , 84 ).
Table 1.
Relationship between increases in bone resorption rate and fracture risk
| Study | Age (years) | Fracture | RR-BMD* | 95 % CI | Marker | RR-marker† | 95 % CI | |
|---|---|---|---|---|---|---|---|---|
| Women | EPIDOS( 74 ) | >75 | Hip | 2·8 | 1·6, 5·1 | Urinary CTX | 2·2 | 1·3, 3·6 |
| OFELY( 83 ) | 64 (mean) | All | 2·8 | 1·4, 5·6 | Urinary CTX | 2·3 | 1·3, 4·1 | |
| Serum CTX | 2·1 | 1·1, 3·6 | ||||||
| HOS( 84 ) | 69 (mean) | All | 1·6 | 1·2, 2·2 | Urinary CTX | 1·6 | 1·2, 2·0 | |
| Rotterdam( 85 ) | >75 | All | 1·3 | 0·6, 2·8 | Urinary DPD | 1·9 | 1·2, 3·8 | |
| Malmö OPRA( 86 ) | >75 | All | 2·2 | 1·5, 3·1 | TRAP | 2·2 | 1·2, 4·2 | |
| Men | DOES( 87 ) | 72 (mean) | All | 1·8 | 1·4, 2·3 | ICTP | 1·4 | 1·0, 1·9 |
| 2·8‡ | 1·4, 5·4 |
RR, relative risk; BMD, bone mineral density; EPIDOS, Epidemiology of Osteoporosis; CTX, carboxy terminal telopeptide of collagen type I; OFELY, Os de Femmes de Lyon; HOS, Hawaii Osteoporosis Study; DPD, free deoxypyridinoline; OPRA, Osteoporosis Prospective Risk Assessment; TRAP, tartrate-resistant acid phosphatase; DOES, Dubbo Osteoporosis Epidemiology Study; ICTP, C-terminal telopeptide generated by metalloproteinases.
RR-BMD = RR for fracture by 1 sd decrease in BMD.
RR-marker = RR for fracture by 1 sd increase in marker above the premenopausal normal range.
For the highest quintile.
These results suggest that a combined approach, with both aBMD and indices of bone turnover, could improve fracture prediction in postmenopausal women. In fact, calculating the absolute risk of fracture by combining clinical risk factor (i.e. previous fracture), low aBMD and increased bone turnover (high CTX) resulted in a better hip fracture probability at 10 years than with low aBMD alone( 90 ). In elderly men high bone resorption was also associated with an increased risk of osteoporotic fracture( 87 ).
Bone turnover markers and treatment monitoring
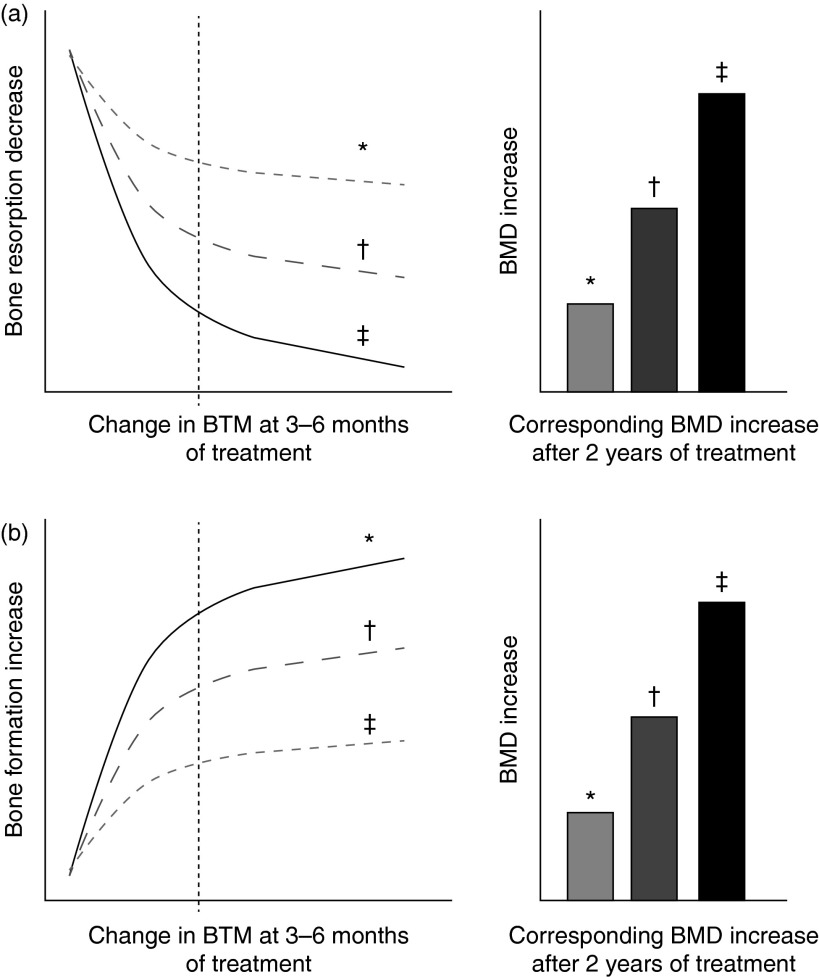
The main domain for the clinical use of BTM is the monitoring of osteoporosis therapy. The ultimate goal in treating patients with osteoporosis is to reduce their fracture risk. However, the short-term incidence of osteoporotic fractures is low, and the absence of fracture during treatment does not necessarily mean that the treatment is effective. Consequently, serial measurements of changes in aBMD as a surrogate marker of therapeutic efficacy are currently the standard approach to monitor osteoporosis therapy. Yet, changes in aBMD occur slowly and therapeutic effects are usually not detectable before 1–2 or more years of treatment( 80 , 91 – 94 ). In contrast, BTM levels change much faster than aBMD in response to therapeutic interventions( 80 ). Antiresorptive treatment generates a rapid decrease in bone resorption markers after only 2–4 weeks, reaching a plateau after 3 to 6 months of treatment( 80 , 95 ) (Fig. 3(a)). The decrease in bone formation markers, reflecting the physiological coupling of bone formation to bone resorption, is delayed and reaches a plateau after 6–12 months. The magnitude of the decreases varies according to the type and dose of the drug and the marker used to assess the effect (Table 2).
Fig. 3.
Schematic representation of changes in bone turnover markers (BTM) at 3–6 months and corresponding increase in bone mineral density (BMD) during treatment of osteoporosis. (a) Bone antiresorptive treatment (i.e. bisphosphonate): a more pronounced decrease in bone resorption marker at 3–6 months is associated with larger increases in BMD. (b) Bone formation-stimulating treatment (i.e. recombinant parathyroid hormone): a greater increase in bone formation marker is associated with a larger increase in BMD. * Mild response in changes in BTM and BMD. † Moderate response in changes in BTM and BMD. ‡ Pronounced response in changes in BTM and BMD. The diagrams show the relationship between early changes (3–6 months) in BTM and changes in BMD after 2 years of either bone resorption inhibition (a) or bone formation stimulation (b). Fig. 3(a) is based on quantitative data obtained by antiresorptive treatment with alendronate, documenting tertile changes at 6 months of the bone resorption marker urinary N-terminal telopeptide (u-NTX) and the changes in BMD as assessed by dual-energy X-ray absorptiometry (DXA) in total hip, trochanter and spine at 3 years in postmenopausal women( 98 ). Fig. 3(b) is based on quantitative data obtained by anabolic treatment with parathyroid hormone documenting tertile changes at 3 months of the bone formation marker N-terminal procollagen I propeptide (PINP) and the change in areal and volumetric BMD at 12 months, as assessed in the spine by DXA and quantitative computed tomography in postmenopausal women( 98 , 113 ).
Table 2.
Changes from baseline in serum tartrate-resistant acid phosphatase (s-TRAP), carboxy terminal telopeptide of collagen type I (s-CTX) and procollagen type I N-terminal propetide (s-PINP) in response to antiresorptive and bone formation-stimulating treatments*
| Change from baseline (%) | ||||
|---|---|---|---|---|
| Compound | Dose and route of administration | s-TRAP | s-CTX | s-PINP |
| Ca + vitamin D | 500–1000 mg +10–20 μg/d (p.o.) | − 20 to − 25 | − 20 to − 30 | − 10 to − 20 |
| Alendronate | 70 mg/week (p.o.) | − 30 to − 40 | − 70 to − 80 | − 60 to − 70 |
| Risedronate | 35 mg/week (p.o.) | − 50 to − 60 | − 40 to − 50 | |
| Ibandronate | 150 mg/month (p.o.) | |||
| 3 mg/3 months (i.v.) | − 60 to − 80 | − 60 to − 70 | ||
| Zoledronate | 5 mg/year (i.v.) | − 50 to − 60 | − 50 to − 60 | |
| Raloxifene | 60 mg/d (p.o.) | − 10 to − 15 | − 20 to − 50 | − 30 to − 40 |
| Denosumab | 60 mg/6 months (s.c.) | − 70 to − 90 | − 60 to − 70 | |
| PTH 1–34 (teriparatide) | 20 μg/d (s.c.) | Up to 80 | Up to 200 | |
| PTH 1–84 | 100 μg/d (s.c.) | 10–100 | 90–150 |
Evidence from interventional drug trials, where the placebo groups received Ca and vitamin D, as well as in nutritional interventions with fortified food, shows a reduction in bone resorption markers of 20–30 % (as outlined in more detail in the ‘Study designs to test the effects of food products on bone metabolism’ section). The decrease in BTM during antiresorptive treatment is inversely related to the subsequent increase in aBMD, predominantly at the lumbar spine( 80 , 81 ). Several studies of postmenopausal women treated with antiresorptive agents (hormone replacement therapy, raloxifen, bisphosphonates) have indicated that the degree of short-term reduction in BTM (after 3 to 6 months) correlates with the observed long-term increase in aBMD after 1 to 3 years of treatment( 79 , 81 , 95 – 99 ). Reduction in fracture risk is only partially explained by the documented changes in aBMD (4–28 %)( 91 , 100 – 104 ). There is also some evidence that even a modest decrease in bone mass is nevertheless associated with some fracture risk reduction( 105 ). There is thus substantial evidence that bone mass or changes thereof does not explain satisfactorily either the skeletal fragility of osteoporosis or the effects of bone active agents( 106 ). It is therefore possible that changes in other determinants of bone strength, including the rate of bone turnover, may be more predictive of anti-fracture efficacy than changes in aBMD. In fact, several studies confirmed that short-term reductions in bone turnover were associated with a reduction in vertebral and/or non-vertebral fracture risk in women treated with hormone replacement therapy, raloxifene, risedronate and alendronate( 88 , 102 , 107 – 109 ).
In contrast to antiresorptive agents, PTH fragments administered intermittently in low doses increase bone remodelling, stimulating bone formation preferentially over bone resorption, and resulting in net gain of bone and reducing fracture risk( 110 – 112 ). Increases in BTM indicate a skeletal response to PTH. There is evidence that early measurement of bone formation markers (OC, BAP and particularly PINP) correlates positively with the subsequent BMD response to PTH (Fig. 3(b))( 113 – 116 ). These data suggest that serial BTM measurements could become useful in identifying skeletal responders to an anabolic therapy with PTH. Based on results from clinical studies and improved technical performance on automated platforms, several national and international guidelines recommend these markers in the follow-up of patients treated for postmenopausal osteoporosis( 32 , 117 , 118 ).
Usefulness of biomarkers of bone turnover in clinical nutrition research
In the process of generating scientific support for claims on foods, BTM were deemed as not sufficiently indicative of bone health to provide evidence for enhanced function or reduced osteoporosis risk( 29 ). However, over the last 10 years there have been improvements in analytical performance and new knowledge of how biochemical markers can be of great utility in osteoporosis management. Because BTM measurement can assess response to anti-osteoporotic medications, the time has come to use BTM levels to reflect bone formation and resorption in response to foods and nutrients.
Influence of foods or nutrients on bone turnover markers
Several studies have examined the response of BTM levels and related hormonal factors to varying food or nutrient consumption in postmenopausal women or in elderly individuals. These studies illustrate how BTM can be important in establishing food and nutrient health claims.
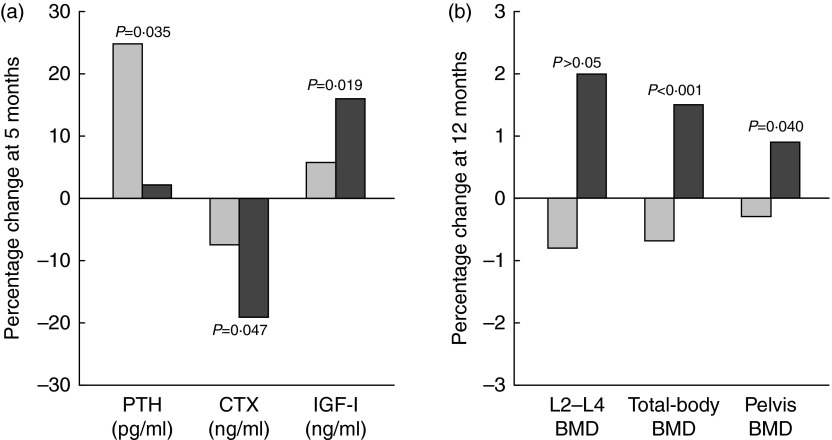
Postmenopausal women
In a 12-month intervention involving postmenopausal women (mean age 60–62 years), the consumption of Ca- and vitamin D-fortified milk and yogurt favourably influenced vitamin D status and bone metabolism, as expressed by changes in serum 25(OH)D, PTH, CTX and IGF-I, as compared with a control group maintaining their usual diet or a group receiving equivalent Ca as lactate–gluconate and bicarbonate salts( 119 ) (Fig. 4). A prospective cross-over trial in postmenopausal women (mean age 59 years) found that supplementation with non-fortified milk for 6 weeks induced a decrease in serum PTH and BTM, including CTX, and a non-significant increase in IGF-I( 120 ). In a randomised study of postmenopausal women (mean age 57 years), consumption of a vitamin D- and Ca-fortified soft white cheese significantly reduced the sensitive biochemical marker of bone resorption TRAP 5b and increased serum IGF-I levels( 121 ).
Fig. 4.
Changes (%) in serum biochemical indexes at 5 months (a) and in bone mineral density (BMD) at 12 months (b) in response to fortified dairy products (▓) for 12 months as compared with controls (░) in postmenopausal women. Data are adapted from Manios et al. ( 119 ). PTH, parathyroid hormone; CTX, carboxy terminal telopeptide of collagen type I; IGF-I, insulin-like growth factor-I. P= Probability level for treatment × time interaction effect as compared with the control group.
Elderly individuals
Favourable effects of milk, fortified or not with vitamin D or Ca, on bone turnover in elderly individuals have been documented in several intervention studies( 42 , 120 , 122 – 124 ).
Interventions with dairy products such as yogurts( 125 , 126 ) or soft white cheese( 126 – 128 ) have shown reductions in bone turnover. In institutionalised elderly individuals with vitamin D deficiency and secondary hyperparathyroidism, an 8-week consumption of vitamin D- and Ca-fortified yogurts saw increases in serum 25(OH)D, associated with a reduction in the BTM CTX and TRAP 5b, and a normalisation of previously high serum PTH( 126 ). Elderly patients hospitalised for an osteoporotic fracture of the proximal femur often present with signs of undernutrition, particularly protein malnutrition( 129 ). In a randomised study, protein repletion by the daily consumption of a 20 g casein-enriched food v. an isoenergetic non-protein supplement led to a significant elevation in serum IGF-I by the end of the 6-month dietary intervention( 58 ). The serum IGF-I response to 20 g/d protein repletion in patients with a recent hip fracture was observable by 7 d, with no further rise in serum IGF-I( 130 ). Thus, in hip fracture patients, the long-term effects of various protein preparations on IGF-I can be predicted from changes observed as early as 1 week following protein supplementation( 130 ).
Bone turnover markers in clinical research on eating disorders
Several nutrition-related disorders can lead to bone loss and increased risk of osteoporotic fracture. Their pathophysiology and clinical expression in relation to the application of biochemical markers are relevant to the present review.
Anorexia nervosa
In young women with anorexia nervosa, aBMD is reduced at several skeletal sites( 131 ). Body weight, but not oestrogen use, is a significant predictor of aBMD in these patients. Together with low endogenous oestrogen levels and Ca deficiency, a low protein intake very probably also contributes to the bone deficit observed in anorexia nervosa. However, low Ca intake has not been consistently reported and 25(OH)D serum levels are usually normal( 132 ). The BTM of bone formation, serum OC and BAP, are significantly reduced in adolescents whereas in adults with anorexia nervosa, the markers of bone resorption are elevated while those of formation are suppressed( 133 , 134 ). The serum level of IGF-I is low in anorexia nervosa( 135 , 136 ), an observation quite compatible with insufficient protein intake( 135 ) although low protein intake has not been consistently recorded. Nutritional rehabilitation reversed the uncoupling of bone remodelling( 137 ) and led to a significant increase in BTM of formation followed by increases in aBMD in as little as 3 months( 134 ). This reversibility occurs before oestrogen levels rise and menses return, suggesting that nutritional factors are of paramount importance( 132 , 134 ).
The serum level of IGF-I was reported to increase rapidly after the onset of intravenous hyperalimentation, followed by a progressive elevation in serum osteocalcin( 136 ). IGF-I level changes were dependent on variations in the nutritional state( 133 ). Increased GH levels accompanied by decreased IGF-I are seen in anorexia nervosa, suggesting an acquired resistance to GH that reversed with refeeding( 132 ). The administration of recombinant IGF-I alone has only a small bone-sparing effect( 138 ). This is not surprising, since the anabolic effects of IGI-I on bone formation are tempered by poor nutrition, particularly by insufficient protein intake( 139 ).
Intensive exercise
In female athletes or ballet dancers, intensive exercise in the absence of appropriate nutrition can lead to hypothalamic dysfunction with delayed menarche and disruption of menstrual cyclicity, bone loss and increase risk of fracture( 140 – 142 ). Nutritional restriction, more common when leanness confers advantages for performance, can play an important role in the disturbance of the female reproductive system when combined with intense physical activity. Insufficient energy intake with respect to energy expenditure impairs the secretion of gonadotropin-releasing hormone and thereby leads to a state of hypo-oestrogenism. This hormonal disturbance is reversed by nutritional rehabilitation leading to an increase in both luteinising hormone and follicle-stimulating hormone. These changes occur well before oestrogen rises and menses return, suggesting the dominant effect of nutritional factors( 132 ). However, the relative contribution of insufficient protein intake with low IGF-I remains to be assessed since it is often associated with reduced energy intake. The consequence on bone metabolism of acute experimental energy restriction has been investigated in young exercising female volunteers( 143 ). This study indicated that severe reduction in energy availability rapidly induces a negative uncoupling between bone formation and bone resorption( 143 ). The resulting bone loss may become irreversible with persistence of such a negative uncoupled remodelling, explaining the increased risk of fragility fractures in anorexia nervosa( 132 , 144 ) as well as in certain athletes and ballet dancers( 140 , 142 ).
Induced weight loss in overweight/obese subjects
Reduction in energy balance induced by energy restriction is often associated with bone loss that varies according to sex, age, ovarian function and initial fat mass (for a recent review, see Shapses & Sukumar( 145 )). The degree of bone loss also depends upon the kind of diet accompanying the energy restriction. Bone mineral loss during body-weight reduction may not be fully recovered with weight regained, at least in postmenopausal women( 146 ). Hence, it is important to understand the underlying pathophysiological mechanisms and thereby define the best strategies to prevent bone loss during energy restriction in overweight/obese individuals. Several studies have used bone health biomarkers, particularly with the objective to identify the key implicated nutrients.
Ca intake typically decreases with energy-restriction diets. In this condition, the reduced Ca intake is associated with elevation in both serum PTH and biochemical markers of bone remodelling( 147 , 148 ). Consumption of Ca salt supplements can suppress the rise in both serum PTH and BTM( 147 , 149 – 151 ).
Dairy products may prevent bone loss during energy restriction not only by providing Ca but also by supplying proteins. Weight-reducing diets that are high in dairy products can suppress the rise in bone turnover and prevent bone loss( 152 , 153 ). In postmenopausal women, a randomised 12-month controlled study showed that higher dietary protein intake (86 v. 60 g/d) during weight reduction increased serum IGF-I and attenuated loss of aBMD at several skeletal sites and volumetric BMD at the distal tibia( 154 ). The additional consumed proteins were from various food sources including dairy products, with a whey supplement providing 6 g protein/d( 154 ). Combining dairy foods with physical exercise( 155 , 156 ) might be appropriate to prevent bone loss during weight loss in overweight/obese human adults( 157 ). In a recent study, hypo-energetic diets higher in dairy Ca and protein combined with daily exercise favourably affected bone health biomarkers as follows: decrease in PTH; increase in bone formation markers (OC and PINP) with no change in bone resorption markers (CTX and N-terminal telopeptide (NTX)); increment in osteoprotegerin:receptor activator of NFκB ligand (RANKL) ratio( 157 ).
Study designs to test the effects of food products on bone metabolism
In order to provide information on medical practice, the needed evidence-based criteria differ for foods and nutrients as compared with drugs. The development of drugs requires a very high level of rigour, more for safety concerns than for providing evidence of efficacy( 18 , 24 , 25 ). The present review essentially considers the rationale for using BTM in clinical research on foods or nutrients that influence bone mineral economy and/or metabolism.
Issues with randomised controlled trials in osteoporosis
An RCT is the clinical study design that best permits strong causal inference between a tested drug or nutrient and a given outcome( 18 , 20 ). Previous reviews or position papers have emphasised the distinct differences in the evidence that can be obtained by using RCT in the context of drug testing, as compared with the development of nutrient requirement or dietary guidelines( 18 , 23 , 24 , 158 , 159 ). In the osteoporosis context, in order to demonstrate the efficacy of a new medication, regulatory agencies usually require RCT of 3 years’ duration, with fracture as the primary endpoint. In the nutrition field, all types of research are useful in setting dietary recommendations: observational studies, to document prevalence and generate hypotheses; preclinical experiments to identify physiological and biochemical pathways; qualitative studies to understand the human condition; and, finally, RCT, to establish a relationship of causality( 18 , 24 , 25 , 160 ).
Ethical consideration in randomised controlled trials and sample size
The demonstration that a drug is efficacious for reducing the burden of fragility fractures necessitates the design of RCT with very large sample sizes. It is especially the case when, for ethical reasons, the new therapy is tested in so-called ‘active comparator trials’, i.e. when the recently developed medication is compared with an approved drug with convincing antifracture efficacy in patients at high risk of fragility fractures( 161 ). Moreover, a placebo-controlled trial can neither be considered ethically acceptable when the new drug is tested in patients at low risk of fractures. This study design requires a much larger number of subjects, as compared with previous RCT conducted in patients at high risk of fragility fractures( 161 ). Thus, proper design and execution of long-duration large RCT aimed at demonstrating the antifracture efficacy of a drug impose requirements that are difficult to meet( 158 ). This difficulty also encompasses both the narrow response due to the placebo effect and the non-random loss of enrolled subjects that convert a randomised trial into a cohort study( 158 ). It can be expected to be magnified in long-duration RCT aimed at testing the antifracture efficacy of foods or nutrients in osteoporotic patients( 18 , 158 ).
Surrogate endpoints for antifracture efficacy of new drugs
Therefore, the development of surrogate endpoints for antifracture efficacy of new drugs has been considered not only for foods and nutrients( 158 , 159 ), but also for drugs( 161 ). Taking into account not only the large sample size but also the very long duration of conducting RCT with fragility fracture as the primary outcome, it is worth considering the measurement of fracture-related data that can be obtainable within a few weeks or months after the onset of the intervention. In clinical investigation, it is recognised that the early bone remodelling response is a good predictor of fragility fracture( 158 , 159 ). Effective pharmaceutical agents, whether acting via anticatabolic or anabolic mechanisms, very promptly influence bone remodelling, as biochemically expressed by measuring BTM changes( 158 ). These pharmoco-kinetic and -dynamic characteristics, that combine an early response to intervention with a reliable predictability of fragility fractures, make BTM tools better suited to assess the effects of foods or nutrients in clinical research on osteoporosis than the delayed changes in DXA-measured aBMD or bone mineral content. Furthermore, the effect size is usually larger with BTM after a few months than the changes in BMD/bone mineral content that can be observed after 1, or more frequently, 2 years of intervention.
Short-duration randomised controlled trials in nutrition clinical research
In adulthood, the effects of foods on BTM can be assessed in appropriately designed RCT. Examples of such studies are described in the ‘Study designs to test the effects of food products on bone metabolism’ section. The short duration of these RCT limits the number of non-compliant participants. Furthermore, one may also expect that few subjects will be completely lost, i.e. without outcome measurement. This makes the ‘intention-to-treat’ data analysis more valuable for comparison with the ‘per protocol’ analysis that will only include treatment-adhering participants, and thereby provides an estimate of the effect size, some sort of ‘dose–response’, of the intervention.
A physiologically meaningful set of biochemical variables can be selected and assessed at several time points. For instance, when nutritional products are evaluated for their capacity to improve vitamin D status and bone metabolism, changes in serum 25(OH)D, PTH, bone formation and resorption markers should provide information on the dynamic interrelationships between these variables. Measuring the circulating level of IGF-I can assess the response to an increase in protein intake. These short-term RCT studies should provide not only qualitative information on the response but also quantitative data on both the magnitude and the pharmacokinetics of the effects.
The advantage of cross-over design in nutritional investigation
A powerful methodology is the cross-over design, also called ‘n of 1 RCT’( 162 , 163 ). Herein there are two intervention periods, separated by a ‘washout’ period, the duration of which depends upon how long the effect of the intervention lingers after its discontinuation. For some anti-osteoporotic agents such as bisphosphonate compounds, the effect can last months or years. For foods and nutrients acting on bone, the effects may be ‘washed out’ much more rapidly, i.e. within a few days or weeks, with the exception of large doses of vitamin D. Within a trial, each participant acts as his or her own control, and permits comparison between and within groups( 164 ). This design eliminates any genetic influence and reduces bias associated with imbalance in known and unknown confounding variables, as compared with randomised parallel-group controlled trials enrolling two unrelated groups of subjects( 164 ).
Comparative effectiveness research
An important recent trend in medical research is to apply ‘comparative effectiveness research’ (CER)( 165 ). CER is a marked departure from the efficacy standard that any new intervention should outperform placebo or randomised controls. There is particular emphasis placed on the leading question regarding clinical effectiveness of care. A CER study is aimed at determining the value of an intervention over another. It answers two relevant questions: (1) how effective is the intervention, if enrolled subjects follow it as prescribed?; (2) how likely is it that the enrolled participants follow it as prescribed?( 166 ). In a classically designed study, the answers to these two questions would be given by comparing the results computed by ‘intention to treat’ with those analysed ‘per protocol’. CER is a recommended priority for nutrition research( 165 ). Although CER will pose challenges for medical and nutritional industries, it will present numerous opportunities to improve the information base supporting nutritional products, especially when they are integrated into other medical interventions( 166 ). Recent CER nutrition studies have been reported on the bone effects of several vitamin D and Ca supplement regimens( 167 , 168 ).
Conclusions
Osteoporosis is a major health problem for an increasing number of adults as they age. Nutrition plays a substantial role in the primary and secondary prevention of osteoporosis. Several nutrients exert reproducible beneficial effects on bone metabolism, reducing the acceleration of bone loss that occurs after the menopause and in the elderly. The supply in vitamin D, Ca, Pi and protein affects levels of bone-trophic hormones as well as resorption of the bony organic matrix and its subsequent formation and mineral deposition. Some foods and nutrients positively influence bone metabolism by either reducing bone resorption or increasing bone formation, or both. Measurement of several biochemical components in blood facilitate the delineation of the impact of nutrients and food factors on bone-trophic hormones such as vitamin D metabolites, PTH and IGF-I, and on BTM that reflect bone resorption and/or matrix formation and mineralisation. Cross-over randomised trials appear to be the optimal way to evaluate the influence of nutrients and food factors on bone metabolism. Using such a study design, which is considered near the top of the hierarchy of evidence for nutritional studies, biologically significant insight can be gained into the potential influence of food products on bone metabolism and osteoporosis prevention within a relatively short time.
Acknowledgements
The authors are grateful to Flore Dontot, scientific collaborator of Yoplait France, for her administrative contribution by facilitating the coordination of the six co-authors.
Yoplait France had no role in the design, analysis or writing of this article.
J.-P. B., S. W. and M. K. were in charge of drafting the manuscript; W. K., R. L. and M. W. revised the first drafts. M. K. and J.-P. B. designed the figures. The manuscript was English proofed by S. W. All authors critically reviewed the manuscript and approved the final version. J.-P. B. took the responsibility of the final version.
J.-P. B. is clinical consultant for Yoplait France. The remaining authors have no conflict of interest regarding the content of the present review.
Abbreviations: 25(OH)D, 25-hydroxyvitamin D; aBMD, areal bone mineral density; BAP, bone alkaline phosphatase; BMD, bone mineral density; BTM, bone turnover marker; CER, comparative effectiveness research; CTX, carboxy terminal telopeptide of collagen type I; DXA, dual-energy X-ray absorptiometry; GH, growth hormone; IGF, insulin-like growth factor; OC, osteocalcin; Pi, inorganic phosphate; PINP, procollagen type I N-terminal propeptide; PTH, parathyroid hormone; RCT, randomised controlled trial; s-CTX, serum carboxy terminal telopeptide of collagen type I; TRAP 5b, tartrate-resistant acid phosphatase isoenzyme 5b
References
- 1.Rizzoli R & Bonjour JP (2006) Physiology of calcium and phosphate homeostasis. In Dynamics of Bone and Cartilage Metabolism: Principles and Clinical Applications, 2nd ed., pp. 345–360 [Seibel MJ, Robins SP and Bilezikian JP, editors]. San Diego: Academic Press. [Google Scholar]
- 2.Lensmeyer GL, Binkley NC & Drezner MK (2006) New horizons for assessment of vitamin D status in man. In Dynamics of Bone and Cartilage Metabolism: Principles and Clinical Applications, 2nd ed., pp. 513–527 [Seibel M, Robins SP and Bilezikian JP, editors]. San Diego: Academic Press. [Google Scholar]
- 3.Souberbielle JC, Friedlander G & Cormier C (2006) Practical considerations in PTH testing. Clin Chim Acta 366, 81–89. [DOI] [PubMed] [Google Scholar]
- 4.Jüppner H & Fulehan GE-H (2006) Measurement of parathyroid hormone. In Dynamics of Bone and Cartilage Metabolism: Principles and Clinical Applications, 2nd ed., pp. 507–512 [Seibel M, Robins SP and Bilezikian J.P., editors]. San Diego: Academic Press. [Google Scholar]
- 5.Hjortebjerg R & Frystyk J (2013) Determination of IGFs and their binding proteins. Best Pract Res Clin Endocrinol Metab 27, 771–781. [DOI] [PubMed] [Google Scholar]
- 6.Kraenzlin ME & Seibel MJ (2006) Measurements of biochemical markers of bone resorption. In Dynamic Bone and Cartilage Metabolism: Principles and Clinical Applications, 2nd ed., pp. 541–563 [Seibel MJ, Robins SP and Bilezikian J.P., editors]. San Diego: Academic Press. [Google Scholar]
- 7.Lee J & Vasikaran S (2012) Current recommendations for laboratory testing and use of bone turnover markers in management of osteoporosis. Ann Lab Med 32, 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naylor K & Eastell R (2012) Bone turnover markers: use in osteoporosis. Nat Rev Rheumatol 8, 379–389. [DOI] [PubMed] [Google Scholar]
- 9.Vasikaran S, Cooper C, Eastell R, et al. (2011) International Osteoporosis Foundation and International Federation of Clinical Chemistry and Laboratory Medicine position on bone marker standards in osteoporosis. Clin Chem Lab Med 49, 1271–1274. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization (2007) Assessment of Osteoporosis at the Primary Health Care Level. Report of a WHO Scientific Group. Geneva: WHO. [Google Scholar]
- 11.Harvey N, Dennison E & Cooper C (2008) Epidemiology of osteoporotic fractures. In Primer of the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 7th ed., pp. 198–203 [Rosen CJ, Compston JE and Lian J.B., editors]. Washington, DC: The American Society of Bone and Mineral Metabolism. [Google Scholar]
- 12.Hopkins RB, Goeree R, Pullenayegum E, et al. (2011) The relative efficacy of nine osteoporosis medications for reducing the rate of fractures in post-menopausal women. BMC Musculoskelet Disord 12, 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murad MH, Drake MT, Mullan RJ, et al. (2012) Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J Clin Endocrinol Metab 97, 1871–1880. [DOI] [PubMed] [Google Scholar]
- 14.Downey TW, Foltz SH, Boccuzzi SJ, et al. (2006) Adherence and persistence associated with the pharmacologic treatment of osteoporosis in a managed care setting. South Med J 99, 570–575. [DOI] [PubMed] [Google Scholar]
- 15.Rossini M, Bianchi G, Di Munno O, et al. (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17, 914–921. [DOI] [PubMed] [Google Scholar]
- 16.Silverman S & Gold DT (2010) Compliance and persistence with osteoporosis medications: a critical review of the literature. Rev Endocr Metab Disord 11, 275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schousboe JT (2013) Adherence with medications used to treat osteoporosis: behavioral insights. Curr Osteoporos Rep 11, 21–29. [DOI] [PubMed] [Google Scholar]
- 18.Blumberg J, Heaney RP, Huncharek M, et al. (2010) Evidence-based criteria in the nutritional context. Nutr Rev 68, 478–484. [DOI] [PubMed] [Google Scholar]
- 19.Heaney RP (2008) Nutrients, endpoints, and the problem of proof. J Nutr 138, 1591–1595. [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH (1998) Evidence-based management of patients with osteoporosis. J Clin Densitom 1, 395–402. [DOI] [PubMed] [Google Scholar]
- 21.Harris RP, Helfand M, Woolf SH, et al. (2001) Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 20, 21–35. [DOI] [PubMed] [Google Scholar]
- 22.Woolf SH, DiGuiseppi CG, Atkins D, et al. (1996) Developing evidence-based clinical practice guidelines: lessons learned by the US Preventive Services Task Force. Annu Rev Public Health 17, 511–538. [DOI] [PubMed] [Google Scholar]
- 23.Biesalski HK, Aggett PJ, Anton R, et al. (2011) 26th Hohenheim Consensus Conference, September 11, 2010. Scientific substantiation of health claims: evidence-based nutrition. Nutrition 27, S1–S20. [DOI] [PubMed] [Google Scholar]
- 24.Fenton TR & Fenton CJ (2011) Nutrition science mustn't accept a lower level of evidence. Nutr Rev 69, 413–414. [DOI] [PubMed] [Google Scholar]
- 25.Heaney RP & Blumberg J (2011) Author reply: nutrition science mustn't accept a lower level of evidence. Nutr Rev 69, 415–416. [DOI] [PubMed] [Google Scholar]
- 26.Woodside JV, Koletzko BV, Patterson CC, et al. (2013) Scientific standards for human intervention trials evaluating health benefits of foods, and their application to infants, children and adolescents. World Rev Nutr Diet 108, 18–31. [DOI] [PubMed] [Google Scholar]
- 27.Bonjour JP, Ammann P & Rizzoli R (1999) Importance of preclinical studies in the development of drugs for treatment of osteoporosis: a review related to the 1998 WHO guidelines. Osteoporos Int 9, 379–393. [DOI] [PubMed] [Google Scholar]
- 28.Bruyere O, Rizzoli R, Coxam V, et al. (2012) Assessment of health claims in the field of bone: a view of the Group for the Respect of Ethics and Excellence in Science (GREES). Osteoporos Int 23, 193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prentice A, Bonjour JP, Branca F, et al. (2003) PASSCLAIM – bone health and osteoporosis. Eur J Nutr 42, Suppl. 1, I28–I49. [DOI] [PubMed] [Google Scholar]
- 30.Sibai T, Morgan EF & Einhorn TA (2011) Anabolic agents and bone quality. Clin Orthop Relat Res 469, 2215–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Syed FA & Melim T (2011) Rodent models of aging bone: an update. Curr Osteoporos Rep 9, 219–228. [DOI] [PubMed] [Google Scholar]
- 32.Kanis JA, McCloskey EV, Johansson H, et al. (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24, 23–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schuit SCE, van der Klift M, Weel AEAM, et al. (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34, 195–202. [DOI] [PubMed] [Google Scholar]
- 34.Sornay-Rendu E, Munoz F, Garnero P, et al. (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20, 1813–1819. [DOI] [PubMed] [Google Scholar]
- 35.Siris ES, Chen YT, Abbott TA, et al. (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164, 1108–1112. [DOI] [PubMed] [Google Scholar]
- 36.Boutroy S, Bouxsein ML, Munoz F, et al. (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90, 6508–6515. [DOI] [PubMed] [Google Scholar]
- 37.Eastell R, Arnold A, Brandi ML, et al. (2009) Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab 94, 340–350. [DOI] [PubMed] [Google Scholar]
- 38.Tannenbaum C, Clark J, Schwartzman K, et al. (2002) Yield of laboratory testing to identify secondary contributors to osteoporosis in otherwise healthy women. J Clin Endocrinol Metab 87, 4431–4437. [DOI] [PubMed] [Google Scholar]
- 39.Lips P, Duong T, Oleksik A, et al. (2001) A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trial. J Clin Endocrinol Metab 86, 1212–1221. [DOI] [PubMed] [Google Scholar]
- 40.Boonen S, Bischoff-Ferrari HA, Cooper C, et al. (2006) Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcif Tissue Int 78, 257–270. [DOI] [PubMed] [Google Scholar]
- 41.Tang BM, Eslick GD, Nowson C, et al. (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370, 657–666. [DOI] [PubMed] [Google Scholar]
- 42.Tenta R, Moschonis G, Koutsilieris M, et al. (2011) Calcium and vitamin D supplementation through fortified dairy products counterbalances seasonal variations of bone metabolism indices: the Postmenopausal Health Study. Eur J Nutr 50, 341–349. [DOI] [PubMed] [Google Scholar]
- 43.Kanellakis S, Moschonis G, Tenta R, et al. (2012) Changes in parameters of bone metabolism in postmenopausal women following a 12-month intervention period using dairy products enriched with calcium, vitamin D, and phylloquinone (vitamin K1) or menaquinone-7 (vitamin K2): the Postmenopausal Health Study II. Calcif Tissue Int 90, 251–262. [DOI] [PubMed] [Google Scholar]
- 44.Cavalier E, Rozet E, Gadisseur R, et al. (2010) Measurement uncertainty of 25-OH vitamin D determination with different commercially available kits: impact on the clinical cut offs. Osteoporos Int 21, 1047–1051. [DOI] [PubMed] [Google Scholar]
- 45.Eddington H, Hudson JE, Oliver RL, et al. (2013) Variability in parathyroid hormone assays confounds clinical practice in chronic kidney disease patients. Ann Clin Biochem 51, 228–236. [DOI] [PubMed] [Google Scholar]
- 46.Mason RS (2010) Vitamin D: a hormone for all seasons. Climacteric 14, 197–203. [DOI] [PubMed] [Google Scholar]
- 47.Ross AC, Manson JE, Abrams SA, et al. (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96, 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96, 1911–1930. [DOI] [PubMed] [Google Scholar]
- 49.Ginde AA, Wolfe P, Camargo CA Jr, et al. (2012) Defining vitamin D status by secondary hyperparathyroidism in the U.S. population. J Endocrinol Invest 35, 42–48. [DOI] [PubMed] [Google Scholar]
- 50.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. (2012) Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab 97, 1153–1158. [DOI] [PubMed] [Google Scholar]
- 51.Rosen CJ, Abrams SA, Aloia JF, et al. (2012) IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab 97, 1146–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bischoff-Ferrari HA, Willett WC, Wong JB, et al. (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293, 2257–2264. [DOI] [PubMed] [Google Scholar]
- 53.Boonen S, Lips P, Bouillon R, et al. (2007) Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. J Clin Endocrinol Metab 92, 1415–1423. [DOI] [PubMed] [Google Scholar]
- 54.Bischoff-Ferrari HA (2010) Vitamin D and fracture prevention. Endocrinol Metab Clin North Am 39, 347–353. [DOI] [PubMed] [Google Scholar]
- 55.Warriner AH & Saag KG (2013) Osteoporosis diagnosis and medical treatment. Orthop Clinics North Am 44, 125–135. [DOI] [PubMed] [Google Scholar]
- 56.Macdonald HM, Wood AD, Aucott LS, et al. (2013) Hip bone loss is attenuated with 1000 IU but not 400 IU daily vitamin D3: a 1-year double-blind RCT in postmenopausal women. J Bone Miner Res 28, 2202–2213. [DOI] [PubMed] [Google Scholar]
- 57.Clemmons DR (2011) Consensus statement on the standardization and evaluation of growth hormone and insulin-like growth factor assays. Clin Chem 57, 555–559. [DOI] [PubMed] [Google Scholar]
- 58.Schürch MA, Rizzoli R, Slosman D, et al. (1998) Protein supplements increase serum insulin-like growth factor-I levels and attenuate proximal femur bone loss in patients with recent hip fracture. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 128, 801–809. [DOI] [PubMed] [Google Scholar]
- 59.Thissen JP, Ketelslegers JM & Underwood LE (1994) Nutritional regulation of the insulin-like growth factors. Endocr Rev 15, 80–101. [DOI] [PubMed] [Google Scholar]
- 60.Bonjour JP, Ammann P, Chevalley T, et al. (2003) Nutritional aspects of bone growth: an overview. In Nutritional Aspects of Bone Health, pp. 111–127 [New S and Bonjour JP, editors]. Cambridge, UK: The Royal Society of Chemistry. [Google Scholar]
- 61.Giustina A, Mazziotti G & Canalis E (2008) Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev 29, 535–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bonjour JP, Schürch MA, Chevalley T, et al. (1997) Protein intake, IGF-1 and osteoporosis. Osteoporos Int 7, Suppl. 3, S36–S42. [DOI] [PubMed] [Google Scholar]
- 63.Perrini S, Laviola L, Carreira MC, et al. (2010) The GH/IGF1 axis and signaling pathways in the muscle and bone: mechanisms underlying age-related skeletal muscle wasting and osteoporosis. J Endocrinol 205, 201–210. [DOI] [PubMed] [Google Scholar]
- 64.Sugimoto T, Nishiyama K, Kuribayashi F, et al. (1997) Serum levels of insulin-like growth factor (IGF) I, IGF-binding protein (IGFBP)-2, and IGFBP-3 in osteoporotic patients with and without spinal fractures. J Bone Miner Res 12, 1272–1279. [DOI] [PubMed] [Google Scholar]
- 65.Garnero P, Sornay-Rendu E & Delmas PD (2000) Low serum IGF-1 and occurrence of osteoporotic fractures in postmenopausal women. Lancet 355, 898–899. [DOI] [PubMed] [Google Scholar]
- 66.Vasikaran S, Eastell R, Bruyere O, et al. (2011) Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 22, 391–420. [DOI] [PubMed] [Google Scholar]
- 67.Henriksen K, Tanko LB, Qvist P, et al. (2007) Assessment of osteoclast number and function: application in the development of new and improved treatment modalities for bone diseases. Osteoporos Int 18, 681–685. [DOI] [PubMed] [Google Scholar]
- 68.Halleen J, Hentunen TA, Karp M, et al. (1998) Characterization of serum tartrate-resistant acid phosphatase and development of a direct two-site immunoassay. J Bone Miner Res 13, 683–687. [DOI] [PubMed] [Google Scholar]
- 69.Halleen J, Alatalo SL, Janckila AJ, et al. (2001) Serum tartrate-resistant acid phosphatase 5b is a specific and sensitive marker of bone resorption. Clin Chem 47, 597–600. [PubMed] [Google Scholar]
- 70.Kraenzlin ME, Lau KHW, Liang L, et al. (1990) Development of an immunoassay for human serum osteoclastic tartrate-resistant acid phosphatase. J Clin Endocrinol Metab 71, 442–451. [DOI] [PubMed] [Google Scholar]
- 71.Hannon R, Clowes J, Eagleton AC, et al. (2004) Clinical performance of immunoreative tartrate resistent acid phosphatase isoform 5b as a marker of bone resorption. Bone 34, 187–194. [DOI] [PubMed] [Google Scholar]
- 72.Garnero P, Borel O & Delmas P (2001) Evaluation of a fully automated serum assay for C-terminal cross-linking teleopeptide of type I collagen in osteoporosis. Clin Chem 47, 694–702. [PubMed] [Google Scholar]
- 73.Garnero P, Sornay-Rendu E, Chapuy MC, et al. (1996) Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J Bone Miner Res 11, 337–349. [DOI] [PubMed] [Google Scholar]
- 74.Garnero P, Hausherr E, Chapuy MC, et al. (1996) Markers of bone resorption predict hip fracture in elderly women: the EPIDOS Prospective Study. J Bone Miner Res 11, 1531–1538. [DOI] [PubMed] [Google Scholar]
- 75.Henriksen K, Leeming DJ, Christiansen C, et al. (2011) Use of bone turnover markers in clinical osteoporosis assessment in women: current issues and future options. Womens Health (Lond Engl) 7, 689–698. [DOI] [PubMed] [Google Scholar]
- 76.Stepan J (2000) Prediction of bone loss in postmenopausal women. Osteoporos Int 11, Suppl. 6, 45–54. [DOI] [PubMed] [Google Scholar]
- 77.Delmas P, Eastell R, Garnero P, et al. (2000) The use of biochemical markers of bone turnover in osteoporosis. Committee of Scientific Advisors of the International Osteoporosis Foundation. Osteoporos Int 11, Suppl. 6, S2–S17. [DOI] [PubMed] [Google Scholar]
- 78.Garnero P & Delmas PD (2004) Contribution of bone mineral density and bone turnover markers to the estimation of risk of osteoporotic fracture in postmenopausal women. J Musculoskelet Neuronal Interact 4, 50–63. [PubMed] [Google Scholar]
- 79.Garnero P, Sornay-Rendu E, Duboeuf F, et al. (1999) Markers of bone turnover predict postmenopausal forearm bone loss over 4 years: the OFELY study. J Bone Miner Res 14, 1614–1621. [DOI] [PubMed] [Google Scholar]
- 80.Delmas P (2000) Markers of bone turnover for monitoring treatment of osteoporosis with antiresorptive drugs. Osteoporos Int 11, Suppl. 6, S66–S76. [DOI] [PubMed] [Google Scholar]
- 81.Delmas PD, Hardy P, Garnero P, et al. (2000) Monitoring individual response to hormone replacement therapy with bone markers. Bone 26, 553–560. [DOI] [PubMed] [Google Scholar]
- 82.Rosen C, Chesnut CH & Mallinak NJ (1997) The predictive value of biochemical markers of bone turnover for bone mineral density in early postmenopausal women treated with hormone replacement or calcium supplementation. J Clin Endocrinol Metab 82, 1904–1910. [DOI] [PubMed] [Google Scholar]
- 83.Garnero P, Sornay-Rendu E, Claustrat B, et al. (2000) Biochemical markers of bone turnover, endogenous hormones and risk of fractures in postemenopausal women: the OFELY study. J Bone Miner Res 15, 1526–1536. [DOI] [PubMed] [Google Scholar]
- 84.Ross PD, Kress BC, Parson RE, et al. (2000) Serum bone alkaline phosphatase and calcaneus bone density predict fractures: a prospective study. Osteoporos Int 11, 76–82. [DOI] [PubMed] [Google Scholar]
- 85.van Daele P, Seibel M, Burger H, et al. (1996) Case-control analysis of bone resorption markers, disability and hip fracture: the Rotterdam Study. Br Med J 312, 482–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gerdhem P, Ivaska KK, Alatalo SL, et al. (2004) Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res 19, 386–393. [DOI] [PubMed] [Google Scholar]
- 87.Meier C, Nguyen TV, Center JR, et al. (2005) Bone resorption and osteoporotic fractures in elderly men: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 20, 579–587. [DOI] [PubMed] [Google Scholar]
- 88.Bauer DC, Black DM, Garnero P, et al. (2004) Change in bone turnover and hip, non-spine, and vertebral fracture in alendronate-treated women: the fracture intervention trial. J Bone Miner Res 19, 1250–1258. [DOI] [PubMed] [Google Scholar]
- 89.Garnero P & Delmas PD (2006) Laboratory assessment of osteoporosis. In Dynamics of Bone and Cartilage Metabolism: Principles and Clinical Applications, 2nd ed., pp. 611–628 [Seibel M, Robins S and Bilezikian J, editors]. San Diego: Academic Press. [Google Scholar]
- 90.Johnell O, Odén A, De Laet C, et al. (2002) Biochemical indices of bone turnover and the assessment of fracture probability. Osteoporos Int 13, 523–526. [DOI] [PubMed] [Google Scholar]
- 91.Bonnick SL & Shulman L (2006) Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med 119, S25–S31. [DOI] [PubMed] [Google Scholar]
- 92.Briot K & Roux C (2005) What is the role of DXA, QUS and bone markers in fracture prediction, treatment allocation and monitoring? Best Pract Res Clin Rheumatol 19, 951–964. [DOI] [PubMed] [Google Scholar]
- 93.Miller PD (2005) Bone density and markers of bone turnover in predicting fracture risk and how changes in these measures predict fracture risk reduction. Curr Osteoporos Rep 3, 103–110. [DOI] [PubMed] [Google Scholar]
- 94.Roux C, Garnero P, Thomas T, et al. (2005) Recommendations for monitoring antiresorptive therapies in postmenopausal osteoporosis. Joint Bone Spine 72, 26–31. [DOI] [PubMed] [Google Scholar]
- 95.Garnero P, Shih WJ, Gineyts E, et al. (1994) Comparison of new biochemical markers of bone turnover in late postmenopausal osteoporotic women in response to alendronate treatment. J Clin Endocrinol Metab 79, 1693–1700. [DOI] [PubMed] [Google Scholar]
- 96.Delmas PD (2000) How does antiresorptive therapy decrease the risk of fracture in women with osteoporosis? Bone 27, 1–3. [DOI] [PubMed] [Google Scholar]
- 97.Rosen C, Chesnut CHIII & Mallinak NJS (1997) The predictive value of biochemical markers of bone turnover for bone mineral density in early postmenopausal women treated with hormone replacement or calcium supplementation. J Clin Endocrinol Metab 82, 1904–1910. [DOI] [PubMed] [Google Scholar]
- 98.Greenspan SL, Resnick NM & Parker RA (2005) Early changes in biochemical markers of bone turnover are associated with long-term changes in bone mineral density in elderly women on alendronate, hormone replacement therapy, or combination therapy: a three-year, double-blind, placebo-controlled, randomized clinical trial. J Clin Endocrinol Metab 90, 2762–2767. [DOI] [PubMed] [Google Scholar]
- 99.Ravn P, Hosking D, Thompson D, et al. (1999) Monitoring of alendronate treatment and prediction of effect on bone mass by biochemical markers in the early postmenopausal intervention cohort study. J Clin Endocrinol Metab 84, 2363–2368. [DOI] [PubMed] [Google Scholar]
- 100.Cummings SR, Karpf DB, Harris F, et al. (2002) Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med 112, 281–289. [DOI] [PubMed] [Google Scholar]
- 101.Hochberg M (2000) Preventing fractures in postmenopausal women with osteoporosis: a review of recent controlled trials of antiresorptive agents. Drugs Aging 17, 317–330. [DOI] [PubMed] [Google Scholar]
- 102.Hochberg MC, Greenspan S, Wasnich RD, et al. (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87, 1586–1592. [DOI] [PubMed] [Google Scholar]
- 103.Wasnich RD & Miller P (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85, 231–236. [DOI] [PubMed] [Google Scholar]
- 104.Watts NB, Geusens P, Barton IP, et al. (2005) Relationship between changes in BMD and nonvertebral fracture incidence associated with risedronate: reduction in risk of nonvertebral fracture is not related to change in BMD. J Bone Miner Res 20, 2097–2104. [DOI] [PubMed] [Google Scholar]
- 105.Chapurlat RD, Palermo L, Ramsay P, et al. (2005) Risk of fracture among women who lose bone density during treatment with alendronate. The Fracture Intervention Trial. Osteoporos Int 16, 842–848. [DOI] [PubMed] [Google Scholar]
- 106.Heaney RP (2003) Is the paradigm shifting? Bone 33, 457–465. [DOI] [PubMed] [Google Scholar]
- 107.Bjarnason NH, Sarkar S, Duong T, et al. (2001) Six and twelve month changes in bone turnover are related to reduction in vertebral fracture risk during 3 years of raloxifene treatment in postmenopausal osteoporosis. Osteoporos Int 12, 922–930. [DOI] [PubMed] [Google Scholar]
- 108.Eastell R, Barton I, Hannon RA, et al. (2003) Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate. J Bone Miner Res 18, 1051–1056. [DOI] [PubMed] [Google Scholar]
- 109.Reginster JY, Sarkar S, Zegels B, et al. (2004) Reduction in PINP, a marker of bone metabolism, with raloxifene treatment and its relationship with vertebral fracture risk. Bone 34, 344–351. [DOI] [PubMed] [Google Scholar]
- 110.Cranney A, Papaioannou A, Zytaruk N, et al. (2006) Parathyroid hormone for the treatment of osteoporosis: a systematic review. CMAJ 175, 52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hodsman A, Papaioannou A & Cranney A (2006) Clinical practice guidelines for the use of parathyroid hormone in the treatment of osteoporosis. CMAJ 175, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kraenzlin ME & Meier C (2011) Parathyroid hormone analogues in the treatment of osteoporosis. Nat Rev Endocrinol 7, 647–656. [DOI] [PubMed] [Google Scholar]
- 113.Bauer DC, Garnero P, Bilezikian JP, et al. (2006) Short-term changes in bone turnover markers and bone mineral density response to parathyroid hormone in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 91, 1370–1375. [DOI] [PubMed] [Google Scholar]
- 114.Chen P, Satterwhite JH, Licata AA, et al. (2005) Early changes in biochemical markers of bone formation predict BMD response to teriparatide in postmenopausal women with osteoporosis. J Bone Miner Res 20, 962–970. [DOI] [PubMed] [Google Scholar]
- 115.Eastell R, Krege JH, Chen P, et al. (2006) Development of an algorithm for using PINP to monitor treatment of patients with teriparatide. Curr Med Res Opin 22, 61–66. [DOI] [PubMed] [Google Scholar]
- 116.Lane NE, Sanchez S, Genant HK, et al. (2000) Short-term increases in bone turnover markers predict parathyroid hormone-induced spinal bone mineral density gains in postmenopausal women with glucocorticoid-induced osteoporosis. Osteoporos Int 11, 434–442. [DOI] [PubMed] [Google Scholar]
- 117.Bergmann P, Body JJ, Boonen S, et al. (2009) Evidence-based guidelines for the use of biochemical markers of bone turnover in the selection and monitoring of bisphosphonate treatment in osteoporosis: a consensus document of the Belgian Bone Club. Int J Clin Pract 63, 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Swiss Association against Osteoporosis (2010) Osteoporosis: prevention, diagnosis and treatment. Recommendation 2010 http://www.SVGO.ch.
- 119.Manios Y, Moschonis G, Trovas G, et al. (2007) Changes in biochemical indexes of bone metabolism and bone mineral density after a 12-mo dietary intervention program: the Postmenopausal Health Study. Am J Clin Nutr 86, 781–789. [DOI] [PubMed] [Google Scholar]
- 120.Bonjour JP, Brandolini-Bunlon M, Boirie Y, et al. (2008) Inhibition of bone turnover by milk intake in postmenopausal women. Br J Nutr 100, 866–874. [DOI] [PubMed] [Google Scholar]
- 121.Bonjour JP, Benoit V, Rousseau B, et al. (2012) Consumption of vitamin D- and calcium-fortified soft white cheese lowers the biochemical marker of bone resorption TRAP 5b in postmenopausal women at moderate risk of osteoporosis fracture. J Nutr 142, 698–703. [DOI] [PubMed] [Google Scholar]
- 122.Heaney RP, McCarron DA, Dawson-Hughes B, et al. (1999) Dietary changes favorably affect bone remodeling in older adults. J Am Diet Assoc 99, 1228–1233. [DOI] [PubMed] [Google Scholar]
- 123.Palacios S, Castelo-Branco C, Cifuentes I, et al. (2005) Changes in bone turnover markers after calcium-enriched milk supplementation in healthy postmenopausal women: a randomized, double-blind, prospective clinical trial. Menopause 12, 63–68. [DOI] [PubMed] [Google Scholar]
- 124.Manios Y, Moschonis G, Panagiotakos DB, et al. (2009) Changes in biochemical indices of bone metabolism in post-menopausal women following a dietary intervention with fortified dairy products. J Hum Nutr Diet 22, 156–165. [DOI] [PubMed] [Google Scholar]
- 125.Heaney RP, Rafferty K & Dowell MS (2002) Effect of yogurt on a urinary marker of bone resorption in postmenopausal women. J Am Diet Assoc 102, 1672–1674. [DOI] [PubMed] [Google Scholar]
- 126.Bonjour JP, Benoit V, Payen F, et al. (2013) Consumption of yogurts fortified in vitamin D and calcium reduces serum parathyroid hormone and markers of bone resorption: a double-blind randomized controlled trial in institutionalized elderly women. J Clin Endocrinol Metab 98, 2915–2921. [DOI] [PubMed] [Google Scholar]
- 127.Bonjour JP, Benoit V, Pourchaire O, et al. (2009) Inhibition of markers of bone resorption by consumption of vitamin D and calcium-fortified soft plain cheese by institutionalised elderly women. Br J Nutr 102, 962–966. [DOI] [PubMed] [Google Scholar]
- 128.Bonjour JP, Benoit V, Pourchaire O, et al. (2011) Nutritional approach for inhibiting bone resorption in institutionalized elderly women with vitamin D insufficiency and high prevalence of fracture. J Nutr Health Aging 15, 404–409. [DOI] [PubMed] [Google Scholar]
- 129.Bonjour JP, Schurch MA & Rizzoli R (1996) Nutritional aspects of hip fractures. Bone 18, 139S–144S. [DOI] [PubMed] [Google Scholar]
- 130.Chevalley T, Hoffmeyer P, Bonjour JP, et al. (2010) Early serum IGF-I response to oral protein supplements in elderly women with a recent hip fracture. Clin Nutr 29, 78–83. [DOI] [PubMed] [Google Scholar]
- 131.Grinspoon S, Thomas E, Pitts S, et al. (2000) Prevalence and predictive factors for regional osteopenia in women with anorexia nervosa. Ann Intern Med 133, 790–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Warren MP (2011) Endocrine manifestations of eating disorders. J Clin Endocrinol Metab 96, 333–343. [DOI] [PubMed] [Google Scholar]
- 133.Soyka LA, Misra M, Frenchman A, et al. (2002) Abnormal bone mineral accrual in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 87, 4177–4185. [DOI] [PubMed] [Google Scholar]
- 134.Dominguez J, Goodman L, Sen Gupta S, et al. (2007) Treatment of anorexia nervosa is associated with increases in bone mineral density, and recovery is a biphasic process involving both nutrition and return of menses. Am J Clin Nutr 86, 92–99. [DOI] [PubMed] [Google Scholar]
- 135.Soyka LA, Grinspoon S, Levitsky LL, et al. (1999) The effects of anorexia nervosa on bone metabolism in female adolescents. J Clin Endocrinol Metab 84, 4489–4496. [DOI] [PubMed] [Google Scholar]
- 136.Hotta M, Fukuda I, Sato K, et al. (2000) The relationship between bone turnover and body weight, serum insulin-like growth factor (IGF) I, and serum IGF-binding protein levels in patients with anorexia nervosa. J Clin Endocrinol Metab 85, 200–206. [DOI] [PubMed] [Google Scholar]
- 137.Caillot-Augusseau A, Lafage-Proust MH, Margaillan P, et al. (2000) Weight gain reverses bone turnover and restores circadian variation of bone resorption in anorexic patients. Clin Endocrinol (Oxf) 52, 113–121. [DOI] [PubMed] [Google Scholar]
- 138.Grinspoon S, Thomas L, Miller K, et al. (2002) Effects of recombinant human IGF-I and oral contraceptive administration on bone density in anorexia nervosa. J Clin Endocrinol Metab 87, 2883–2891. [DOI] [PubMed] [Google Scholar]
- 139.Bourrin S, Ammann P, Bonjour JP, et al. (2000) Dietary protein restriction lowers plasma insulin-like growth factor I (IGF-I), impairs cortical bone formation, and induces osteoblastic resistance to IGF-I in adult female rats. Endocrinology 141, 3149–3155. [DOI] [PubMed] [Google Scholar]
- 140.Warren MP & Perlroth NE (2001) The effects of intense exercise on the female reproductive system. J Endocrinol 170, 3–11. [DOI] [PubMed] [Google Scholar]
- 141.Gremion G, Rizzoli R, Slosman D, et al. (2001) Oligo-amenorrheic long-distance runners may lose more bone in spine than in femur. Med Sci Sports Exerc 33, 15–21. [DOI] [PubMed] [Google Scholar]
- 142.Warren MP, Brooks-Gunn J, Fox RP, et al. (2002) Osteopenia in exercise-associated amenorrhea using ballet dancers as a model: a longitudinal study. J Clin Endocrinol Metab 87, 3162–3168. [DOI] [PubMed] [Google Scholar]
- 143.Ihle R & Loucks AB (2004) Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res 19, 1231–1240. [DOI] [PubMed] [Google Scholar]
- 144.Misra M & Klibanski A (2011) The neuroendocrine basis of anorexia nervosa and its impact on bone metabolism. Neuroendocrinology 93, 65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shapses SA & Sukumar D (2012) Bone metabolism in obesity and weight loss. Annu Rev Nutr 32, 287–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Villalon KL, Gozansky WS, Van Pelt RE, et al. (2011) A losing battle: weight regain does not restore weight loss-induced bone loss in postmenopausal women. Obesity (Silver Spring) 19, 2345–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Jensen LB, Kollerup G, Quaade F, et al. (2001) Bone minerals changes in obese women during a moderate weight loss with and without calcium supplementation. J Bone Miner Res 16, 141–147. [DOI] [PubMed] [Google Scholar]
- 148.Ricci TA, Heymsfield SB, Pierson RN Jr, et al. (2001) Moderate energy restriction increases bone resorption in obese postmenopausal women. Am J Clin Nutr 73, 347–352. [DOI] [PubMed] [Google Scholar]
- 149.Ricci TA, Chowdhury HA, Heymsfield SB, et al. (1998) Calcium supplementation suppresses bone turnover during weight reduction in postmenopausal women. J Bone Miner Res 13, 1045–1050. [DOI] [PubMed] [Google Scholar]
- 150.Shapses SA, Von Thun NL, Heymsfield SB, et al. (2001) Bone turnover and density in obese premenopausal women during moderate weight loss and calcium supplementation. J Bone Miner Res 16, 1329–1336. [DOI] [PubMed] [Google Scholar]
- 151.Riedt CS, Schlussel Y, von Thun N, et al. (2007) Premenopausal overweight women do not lose bone during moderate weight loss with adequate or higher calcium intake. Am J Clin Nutr 85, 972–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bowen J, Noakes M & Clifton PM (2004) A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr 134, 568–573. [DOI] [PubMed] [Google Scholar]
- 153.Thorpe MP, Jacobson EH, Layman DK, et al. (2008) A diet high in protein, dairy, and calcium attenuates bone loss over twelve months of weight loss and maintenance relative to a conventional high-carbohydrate diet in adults. J Nutr 138, 1096–1100. [DOI] [PubMed] [Google Scholar]
- 154.Sukumar D, Ambia-Sobhan H, Zurfluh R, et al. (2011) Areal and volumetric bone mineral density and geometry at two levels of protein intake during caloric restriction: a randomized, controlled trial. J Bone Miner Res 26, 1339–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ryan AS, Nicklas BJ & Dennis KE (1998) Aerobic exercise maintains regional bone mineral density during weight loss in postmenopausal women. J Appl Physiol 84, 1305–1310. [DOI] [PubMed] [Google Scholar]
- 156.Silverman NE, Nicklas BJ & Ryan AS (2009) Addition of aerobic exercise to a weight loss program increases BMD, with an associated reduction in inflammation in overweight postmenopausal women. Calcif Tissue Int 84, 257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Josse AR & Phillips SM (2012) Impact of milk consumption and resistance training on body composition of female athletes. Med Sport Sci 59, 94–103. [DOI] [PubMed] [Google Scholar]
- 158.Heaney RP, et al. (2008) Design considerations for clinical investigations of osteoporosis. In Osteoporosis, 3rd ed., pp. 1598–1620 [Marcus M, Feldman D and Nelson DA, editors]. Amsterdam: Elsevier, Inc. [Google Scholar]
- 159.Heaney RP, et al. (2008) Nutrition and risk for osteoprosis. In Osteoporosis, pp. 799–836 [Marcus M, Feldman D and Nelson DA, editors]. Amsterdam: Elsevier, Inc. [Google Scholar]
- 160.Mann JI (2010) Evidence-based nutrition: does it differ from evidence-based medicine? Ann Med 42, 475–486. [DOI] [PubMed] [Google Scholar]
- 161.Bouxsein ML & Delmas PD (2008) Considerations for development of surrogate endpoints for antifracture efficacy of new treatments in osteoporosis: a perspective. J Bone Miner Res 23, 1155–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Montori VM & Guyatt GH (2001) What is evidence-based medicine and why should it be practiced? Respir Care 46, 1201–1214. [PubMed] [Google Scholar]
- 163.Dawson B & Trapp RG (2001) Basic and Clinical Biostatistics, 3rd ed. New York: Lange Medical Books/McGraw-Hill. [Google Scholar]
- 164.Mills EJ, Chan AW, Wu P, et al. (2009) Design, analysis, and presentation of crossover trials. Trials 10, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Iglehart JK (2009) Prioritizing comparative-effectiveness research – IOM recommendations. N Engl J Med 361, 325–328. [DOI] [PubMed] [Google Scholar]
- 166.Kaats GR, Preuss HG & Leckie RB (2009) Comparative effectiveness research (CER): opportunities and challenges for the nutritional industry. J Am Coll Nutr 28, 234–237. [DOI] [PubMed] [Google Scholar]
- 167.Kaats GR, Preuss HG, Croft HA, et al. (2011) A comparative effectiveness study of bone density changes in women over 40 following three bone health plans containing variations of the same novel plant-sourced calcium. Int J Med Sci 8, 180–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Michalek JE, Preuss HG, Croft HA, et al. (2011) Changes in total body bone mineral density following a common bone health plan with two versions of a unique bone health supplement: a comparative effectiveness research study. Nutr J 10, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]