Abstract
Purpose:
To evaluate changes in the concentration of tear immunoglobulins in contact lens wearers.
Methods:
A total of 45 cases including 23 contact lens wearers (43 eyes) and 22 age and sex matched healthy controls having no ocular pathology were studied for immunoglobulins (IgA, IgG, IgM) in their tears by single radial immunodiffusion method.
Results:
Most of the cases used soft (56.6%) and semi-soft gas permeable (30.4%) contact lenses. Tear IgM was detected in only 17.4% and tear IgG in 43.6% of contact lens wearers, while in controls IgG was detected in 9.1% but none of the controls had IgM. There was a significant rise in total tear IgA (13.17 ± 4.44 mg/dl) in contact lens wearer as compared to controls (8.93 ± 3.79 mg/dl). Rise of tear IgA was more in symptomatic patients (15.38 ± 5.28 mg/dl) and in those wearing hard (19.73 ± 5.43 mg/dl) and semi-soft contact lenses (13.31 ± 5.43 mg/dl). A significant increase in tear IgA was noticed in subjects wearing lenses for >3 years (15.69 ± 5.39 mg/dl). About 43.4% of lens wearers were symptomatic and 80% of their lenses showed deposits and/or haziness. All cases with IgM in tear were symptomatic.
Conclusion:
The relation of immunoglobulin concentration with increasing duration of wear and material of contact lens shows that tear immunoglobulin rise accrues due to mechanical stimulation, hence contact lenses should not be used for a long period and lenses of hard nature should be discouraged. The maintenance, cleaning and deproteinization of the lenses are of high importance to avoid immunostimulation.
Keywords: Contact Lens, Radial Immunodiffusion Method, Tear Immunoglobulins
INTRODUCTION
Contact lenses have several advantages over spectacles and cosmesis is the most common one. There is less peripheral distortion than spectacles, especially with high refractive errors. It decreases the magnification and increases visual fields in uniocular aphakia and anisometropia. Great improvements in contact lens technology have taken place over the past decades through which contact lens material has changed from glass to plastic and from polymethyl cellulose acetate to silicone hydrogel.[1] Gas permeable, disposable, high water content, hydrophilic, and soft even bifocal lenses are the advances in contact lens practice. Wearing contact lens decreases corneal sensitivity,[2] reduces tear secretion, increases evaporation time and leads to concentration of tear film constituent.[3,4,5] However, it can produce furrows, dimples, abrasion, hypoxia of corneal ephithelium[6,7] and vascularization of the cornea.[6] Prolonged wearing of contact lens acts as an immunostimulant interfering with tear immunoglobulin levels[8] and may increase the incidence of microbial keratitis.[9] The present study has been designed to evaluate changes in various immunoglobulins in the tear of contact lens wearers. The study has also attempted to set correlation of tear immunoglobulin with different types of contact lenses and duration of lens wear.
METHODS
In this study, 23 patients wearing various types of contact lenses and 22 controls without any obvious ocular pathology were included. Most of the control cases had slight refractive errors only. Cases with refractive errors were selected from the clinic of Department of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi (U.P.), India. All cases were using their lenses daily but not more than 8 hours in continuation. Detailed history was elicited for the duration of lens wear, average daily time of lens wear, mode of cleaning and disinfection, and features of lens intolerance such as watering, burning, itching, pain in eyes, foreign body sensation and the presence or absence of discharge. Visual acuity was recorded with and without glasses and with contact lens. Refraction and keratometry was done routinely. Detailed ocular examination including slit lamp examination was done to detect ocular changes due to lens wear such as alterations in the conjunctiva (hyperemia and follicular hypertrophy) and alteration in corneal epithelium (furrows, dimples, lens imprints, abrasions, epithelial edema, and corneal vascularization). Patients having ocular diseases such as conjunctivitis, blepharoconjunctivitis, keratomalacia, herpes simplex keratitis, trachoma, and systemic disorders such as diabetes, hypertension, thyroid disease, rheumatoid arthritis, sarcoidosis and scleroderma and so forth as well as subjects who took drugs for systemic diseases, were excluded.
In all cases, tears were collected using a sterile 100 μl micropipette by putting its tip at the margin of lateral canthus after mechanical stimulation by the contact lens itself. In few cases, tear secretion was increased by stimulating the nasal mucosa with swab stick soaked in spirit. After collection, tears were sent to Advanced Immunodiagnostic Training and Research Center of Institute of Medical Sciences Banaras Hindu University where it was stored at −20°C in 0.5 ml tubes. Tear immunoglobulins (IgG, IgA and IgM) were estimated by single radial immunodiffusion method described by Mancini (1965). The low diffusion immunoglobulin agar plates of IgG, IgA and IgM (Biocientifica S.A. Iturri 232(C1427ADD) Buenos Aires, Argentina) supplied by Immunodiagnostic Pvt. Ltd. 1590 Madarsa Road, Kashmere Gate, New Delhi - 110 006 were used for the study.
Data were analyzed by SPSS software (version 17; SPSS, Chicago, IL, USA) employing the Chi-square test and paired t-test. P < 0.05 was considered to be significant.
RESULTS
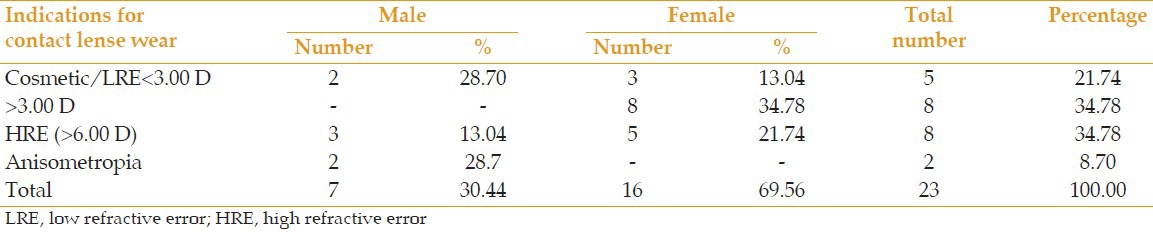
Out of 23 contact lens wearers (43 eyes), 7 (30.4%) were male and 16 (69.6%) were female subjects. Most lens wearers, 12 (52.3%) were in the age group of 21-30 years. Mean age of male and female cases wearing contact lens was 28.8 ± 4 years and 21.6 ± 3 years while in controls it was 25 ± 3.5 and 19.4 ± 3 years, respectively [Table 1]. About 56.5% of the patients were wearing contact lenses for cosmetic reasons or low refractive error (LRE) (21.74%) and refractive error>3.00 D (34.78%), while 34.78% of cases were suffering from high refractive error (HRE) (>6.00 D). Anisometropia was found in 8.7% of cases. Male patients were using contact lenses for high refractive errors (42.3%) and anisometropia (28.6%), whereas the main indication in female patients was refractive errors (>3.00 D) [Table 2].
Table 1.
Age and sex distribution of contact lens wearers and controls
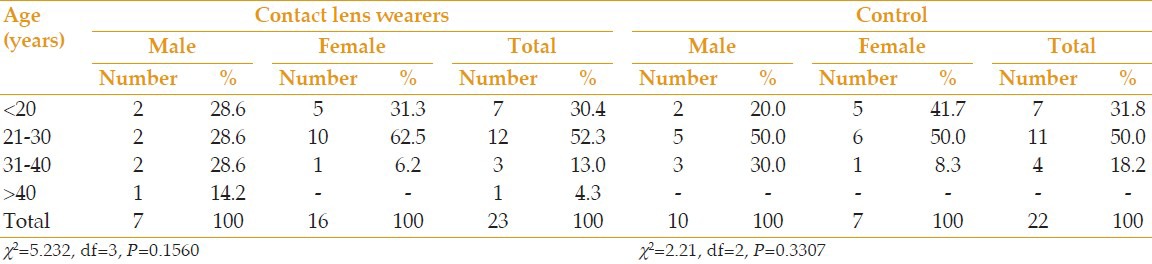
Table 2.
Indication for contact lens wear
About 56.6% of cases used soft contact lenses and 30.4% used semi-soft gas permeable contact lenses, while hard lenses were worn by 13% of patients which included males only. In contrast, most soft contact lenses (75%) were worn by females (75%).
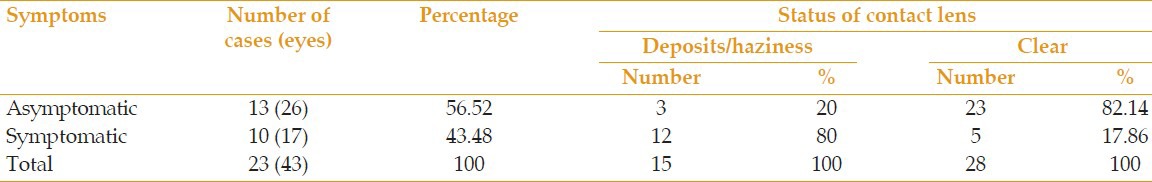
The minimum duration of contact lens wear was observed to be two months, while the maximum duration was 24 years. A large number of patients, 43.5% were wearing contact lens for <1 year, 26.11% were using it between 1 and 3 years, while 30.4% of cases were using it for >3 years. Forty-three contact lenses of 23 cases were examined for their clarity and deposits. Thirteen patients (56.52%) were asymptomatic and 10 patients (43.48%) had symptoms of contact lens related changes in the conjunctiva like hyperemia and hypertrophy and in cornea such as abrasion, edema and vascularization. A total of 80% of the contact lenses of symptomatic patients showed deposits and/or haziness, while in the asymptomatic group only 3 (20%) lenses showed haziness [Table 3].
Table 3.
Contact lens related symptoms and status of contact lens
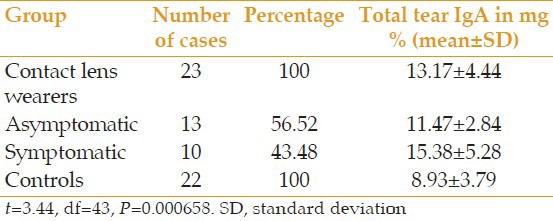
IgA was detected in tears in all lens users. The concentration of tear IgA was significantly higher (13.17 ± 4.44 mg/dl) in contact lens wearers as compared to controls (8.93 ± 3.79 mg/dl) (P < 0.001) [Table 4]. When IgA values were analyzed in relation to symptoms, it was found that symptomatic contact lens wearers had much higher tear IgA (15.38 ± 5.28 mg/dl) than asymptomatic patients (11.47 ± 2.84 mg/dl). This increase was statistically significant (P < 0.05) [Table 4]. Analysis of tear IgA according to the type of lens revealed rising IgA concentrations along with an increase in hardness of lens. Mean value of tear IgA in hard contact lens wearers (19.73 ± 5.43 mg %) was significantly increased as compared to soft (11.58 ± 3.59 mg %, P = 0.003) and semisoft gas permeable (13.31 ± 3.51 mg %, P = 0.029). There was significant increase in total tear IgA with the duration of lens wear. Concentration of tear IgA was more in cases wearing lenses for >3 years in comparison to those with less than one year lens wear.
Table 4.
Mean value of total tear IgA in contact lens wearers and controls
In only four (17.4%) contact lens wearers IgM (13.0 ± 6.0 mg/dl) was detected, whereas there was no IgM detected in 82.6% of cases. In control subjects, no tear IgM was found either [Figure 1]. Correlation of tear IgM with duration of lens wear revealed that out of four cases in which IgM was detected, one patient was wearing lens for <1 year while three patients were wearing contact lenses for >3 years. All four cases were symptomatic and their contact lenses showed deposits.
Figure 1.
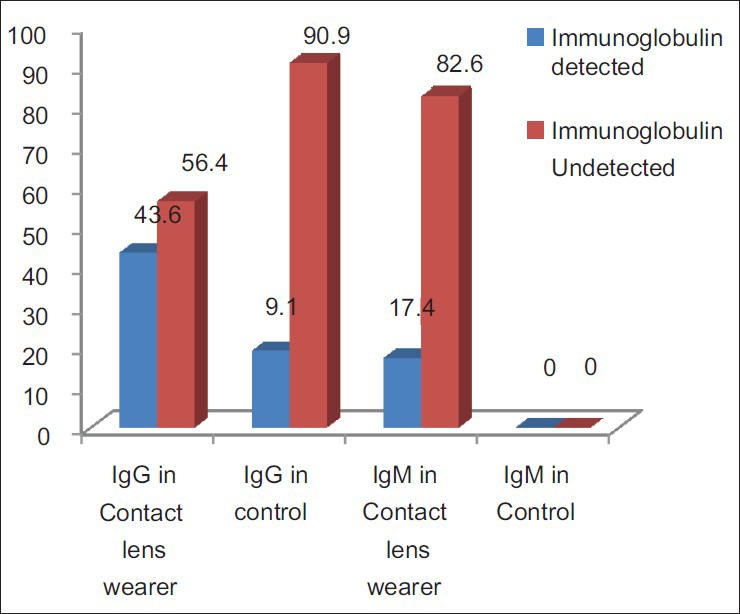
Tear IgM and IgG in contact lens wearers and controls.
Tear IgG was detected in 43.6% of contact lens wearers (ranging from 40-160 mg/dl) and 9.1% of control cases [Figure 1]. About 80% of these patients were symptomatic. Correlation of tear IgG with duration of lens wear revealed that out of 43.61% IgG detected cases, 30% were using contact lenses for <1 year, 20% for 1-3 years and 50% were wearing contact lenses for >3 years.
DISCUSSION
In this study, total tear IgA, IgG, IgM levels were estimated in 23 cases of contact lens wearer and compared with 22 matched controls. Our observation of higher total tear IgA in contact lens wearer is consistent with findings of other studies. Mannucci et al[8] reported very high values of tear IgA (32.8 ± 14.8 mg/dl) in 19 extended contact lens wearers, whereas Temel et al[10] found increased levels of tear IgA (14.0 mg/dl) in only rigid contact lens wearers. Conversely, Vinding et al[11] reported low values of tear secretary IgA in 18 asymptomatic contact lens wearers. They noticed a marked decrease in secretary IgA (mean: 0.72 mg/dl) in contact lens wearers as compared to controls (mean: 2.45 mg/dl) and concluded that absorption of IgA by the contact lenses was responsible for this decrease. Other studies reported similar findings occurring due to IgA absorption by contact lens and lens growing plaques.[12,13,14]
Tear IgA levels in symptomatic patients was significantly higher than asymptomatic cases. Similar to our finding, Temel et al[10] found increased levels of tear IgA (14.0 mg/dl) in rigid lens wearers when compared to soft lens wearers (<9 mg/dl). Tear IgA was significantly increased with extended duration of lens wear. Mannucci et al[8] reported variable results through which, tear IgA level doubled after 1 week of lens wear, decreased after one year similar to that of the control group and again increased after few years. They proposed that changes did not represent a true immunopathological phenomenon, but showed mechanical stimulation of the conjunctiva by permanent lens acting as a foreign body. Pearce et al found reduced concentration of tear secretary IgA epitopes in cases with extended contact lens wear.[15] In other series, no alteration in tear IgA value along with the duration of lens wear were noticed.[10,11]
In our study, tear IgM was detected only in 4 (17.4%) cases. All these cases were symptomatic and showed deposits on the lens. Similar to our results, Sen et al[16] also reported absence of IgM in normal tear. In the present study, tear IgG was detected in only 43.6% of contact lens wearers and 9.1% of controls. The majority of these patients were symptomatic wearing contact lenses for >3 years. Another study reported[17] increased tear IgG (50.7 mg/100 ml) in patients with giant papillary conjunctivitis induced by contact lenses. In addition, progressive increase in IgG concentration which has correlation with the length of lens wear have been reported.[10]
The current study clearly indicates that contact lenses act as a mechanical stimuli and the current study finds the most probable reasons for tear immunoglobulin rise are mechanical stimulation, prolonged wear and hard nature of contact lenses. None of our cases showed any symptom or sign of infection.
In summary, the tear immunoglobulins were increased more in symptomatic cases and symptoms were more marked in patients whose lenses had deposits. In this regard, to avoid deposits on lens and thereby minimize contact lens-related symptoms and tear immunoglobulin rise, the contact lenses should not be worn for long continuous periods and require regular maintenance, cleaning and deproteinization.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Polse KA. Gas-permeable lens materials and designs. Int Ophthalmol Clin. 1986;26:131–148. doi: 10.1097/00004397-198602610-00017. [DOI] [PubMed] [Google Scholar]
- 2.Gilbard JP, Gray KL, Rossi SR. A proposed mechanism for increased tear-film osmolarity in contact lens wearers. Am J Ophthalmol. 1986;102:505–507. doi: 10.1016/0002-9394(86)90081-4. [DOI] [PubMed] [Google Scholar]
- 3.Sota LD, Rastogi A. Update on contact lenses. In: Sovani VB, editor. behalf of FDC Limited; 1992. [Google Scholar]
- 4.Glasson MJ, Stapleton F, Keay L, Sweeney D, Willcox MD. Differences in clinical parameters and tear film of tolerant and intolerant contact lens wearers. Invest Ophthalmol Vis Sci. 2003;44:5116–5124. doi: 10.1167/iovs.03-0685. [DOI] [PubMed] [Google Scholar]
- 5.Campos-Rodríguez R, Oliver-Aguillón G, Vega-Pérez LM, Jarillo-Luna A, Hernández-Martínez D, Rojas-Hernández S, et al. Human IgA inhibits adherence of Acanthamoeba polyphaga to epithelial cells and contact lenses. Can J Microbiol. 2004;50:711–718. doi: 10.1139/w04-057. [DOI] [PubMed] [Google Scholar]
- 6.O’Neal MR, Polse KA, Sarver MD. Corneal response to rigid and hydrogel lenses during eye closure. Invest Ophthalmol Vis Sci. 1984;25:837–842. [PubMed] [Google Scholar]
- 7.Choy CK, Cho P, Benzie IF, Ng V. Effect of one overnight wear of orthokeratology lenses on tear composition. Optom Vis Sci. 2004;81:414–420. doi: 10.1097/01.opx.0000135094.15125.4c. [DOI] [PubMed] [Google Scholar]
- 8.Mannucci LL, Pozzan M, Fregona I, Secchi AG. The effect of extended wear contact lenses on tear immunoglobulins. CLAO J. 1984;10:163–165. [PubMed] [Google Scholar]
- 9.Willcox MD, Lan J. Secretory immunoglobulin A in tears: Functions and changes during contact lens wear. Clin Exp Optom. 1999;82:1–3. doi: 10.1111/j.1444-0938.1999.tb06777.x. [DOI] [PubMed] [Google Scholar]
- 10.Temel A, Kazokoglu H, Taga Y, Orkan AL. The effect of contact lens wear on tear immunoglobulins. CLAO J. 1991;17:69–71. [PubMed] [Google Scholar]
- 11.Vinding T, Eriksen JS, Nielsen NV. The concentration of lysozyme and secretory IgA in tears from healthy persons with and without contact lens use. Acta Ophthalmol (Copenh) 1987;65:23–26. doi: 10.1111/j.1755-3768.1987.tb08485.x. [DOI] [PubMed] [Google Scholar]
- 12.Gachon AM, Bilbaut T, Dastugue B. Adsorption of tear proteins on soft contact lenses. Exp Eye Res. 1985;40:105–116. doi: 10.1016/0014-4835(85)90113-7. [DOI] [PubMed] [Google Scholar]
- 13.Gudmundsson OG, Woodward DF, Fowler SA, Allansmith MR. Identification of proteins in contact lens surface deposits by immunofluorescence microscopy. Arch Ophthalmol. 1985;103:196–197. doi: 10.1001/archopht.1985.01050020048016. [DOI] [PubMed] [Google Scholar]
- 14.Jones B, Sack R. Immunoglobulin deposition on soft contact lenses: Relationship to hydrogel structure and mode of use and giant papillary conjunctivitis. CLAO J. 1990;16:43–48. [PubMed] [Google Scholar]
- 15.Pearce DJ, Demirci G, Willcox MD. Secretory IgA epitopes in basal tears of extended-wear soft contact lens wearers and in non-lens wearers. Aust N Z J Ophthalmol. 1999;27:221–223. doi: 10.1046/j.1440-1606.1999.00206.x. [DOI] [PubMed] [Google Scholar]
- 16.Sen DK, Sarin GS, Mani K, Saha K. Immunoglobulins in tears of normal Indian people. Br J Ophthalmol. 1976;60:302–304. doi: 10.1136/bjo.60.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donshik PC, Ballow M. Tear immunoglobulins in giant papillary conjunctivitis induced by contact lenses. Am J Ophthalmol. 1983;96:460–466. doi: 10.1016/s0002-9394(14)77909-7. [DOI] [PubMed] [Google Scholar]


