Abstract
Purpose:
To assess the agreement among ultrasonic pachymetry, the Galilei dual Scheimpflug analyzer, and Orbscan II for central and peripheral (Galilei vs. Orbscan) corneal thickness (CCT and PCT) measurement in normal and keratoconic eyes.
Methods:
In this prospective study, CCT and PCT were measured in 88 eyes of 88 refractive surgery candidates and 128 eyes of 69 keratoconic patients with ultrasonic pachymetry, the Galilei, and Orbscan II. The readings by the three instruments were compared using one-way analysis of normal variance. Agreement among the three devices was assessed using Pearson and intraclass correlation coefficients, and Bland–Altman plots. The same analyses were employed to evaluate agreement between Galilei and Orbscan II for PCT measurement.
Results:
In the normal group, mean CCT was 551.0±39.4, 566.9±33.5, and 565.5±40.9 μm measured by ultrasonic pachymetry, the Galilei, and Orbscan II, respectively (P<0.001). The corresponding figures in the keratoconus group were 492.0±61.7, 502.0±42.1, and 470.6±56.9 μm, respectively (P<0.001). Mean PCT was 612.5±35.3 and 640.9±38.0 μm in the normal group (P<0.001) and 567.6±35.2 and 595.1±41.4 μm in the keratoconus group (P<0.001) by the Galilei and Orbscan II, respectively. CCT and PCT measurements obtained by different devices were significantly correlated in both groups.
Conclusion:
To measure CCT, the Galilei and Orbscan II can be used interchangeably in normal eyes, but not in keratoconic eyes. For PCT, there is a systematic error between measurements obtained by the Galilei and Orbscan II. However, it is possible to change optical pachymeter readings into those obtained by ultrasonic pachymetry using a constant.
Keywords: Central Corneal Thickness, Galilei, Keratoconus, Orbscan II, Peripheral Corneal Thickness, Ultrasonic Pachymetry
INTRODUCTION
Central corneal thickness (CCT) measurements are important for monitoring corneal endothelial function, assessing the cornea before and after keratorefractive surgery, accurate intraocular pressure measurements, and diagnosis, follow-up, and planning for surgical intervention in corneal pathologies such as keratoconus.[1,2]
A perfect pachymetry device should be safe and precise with good repeatability and reliability. Ultrasonic pachymetry has been considered a benchmark in measuring corneal thickness.[3,4,5] However, the major drawbacks of this technique are discomfort and occasionally infection transmission through corneal contact, which can also interfere with subsequent evaluations such as topography.[6] In addition, the accuracy of ultrasonic pachymetry may be adversely influenced by alteration of the ultrasonic wave propagation speed through tissue (resulting from variations in corneal hydration) and nonperpendicular or decentered position of the probe in relation to the cornea, making it dependent on operator expertise.[7]
Recently, several noncontact optical technologies such as slit-scanning and rotating Scheimpflug imaging have been developed to compensate for limitations posed by ultrasonic pachymetry. With these modalities, there is no need for anesthesia and no risk of corneal contamination. Besides, the center of the cornea can objectively be determined which would result in higher precision and convenience. In addition, they provide corneal topographic mapping including the thinnest-point as well as peripheral corneal thickness (PCT), which is valuable for preoperative planning for refractive surgery, collagen cross-linking, implantation of intrastromal corneal ring segments, and femtosecond laser-assisted keratoplasty.
Orbscan II (Bausch and Lomb, Rochester, NY, USA) uses a horizontally moving slit beam to produce slit images of the anterior segment and provides data for corneal topography, corneal thickness and anterior chamber depth. A conventional Placido ring-based topography is combined with a scanning-slit topography in the Orbscan II system to assess the curvature of the anterior and posterior corneal surface, hence calculating corneal thickness indirectly.[8]
The recently introduced Galilei topographer (Ziemer Ophthalmic System AG, Zurich, Switzerland), uses a double Scheimpflug system in combination with a Placido disk. Slit images are captured from opposite sides of the illuminated slit by 2 cameras situated 180° apart to overcome errors associated with scans at an oblique angle, as well as to compensate for micromovements during the examination and provide direct anterior and posterior elevation and pachymetry measurements from the cornea.[9]
It is not yet clear, however, whether the results of these methods are comparable to ultrasonic pachymetry and whether they can be used interchangeably in normal and abnormal corneas. Herein, the agreement of three methods of CCT measurement including ultrasonic pachymetry, the Galilei, and Orbscan II in normal and keratoconic eyes is evaluated. PCT measurements and agreement between the Galilei and Orbscan II are also compared.
METHODS
In this prospective comparative study, consecutive patients with keratoconus as well as normal subjects who were scheduled for refractive surgery were included. The initial diagnosis of keratoconus was based on clinical slit-lamp findings (stromal thinning, conical protrusion, Fleischer ring, and Vogt striae) and associated characteristic Placido-based topographic patterns. Eyes with previous acute corneal hydrops or a history of corneal surgery were excluded. Keratoconus severity was classified according to corneal curvature using the same system used in the Collaborative Longitudinal Evaluation of Keratoconus study.[10] According to this system, disease severity is classified with respect to the curvature of the steepest corneal meridian as follows: mild, <45 D; moderate, 45–52 D; severe, >52 D.
In the normal group, the only ocular problem was refractive error. Any history or diagnosis of ocular pathology (such as dry eye, keratoconus, glaucoma and retinal disease), ocular surgery or systemic diseases such as diabetes and connective tissue disorders led to subject exclusion. Only the right eyes of the normal group were enrolled.
All participants were asked to stop wearing soft contact lenses for at least 2 weeks and rigid gas permeable contact lenses for at least 4 weeks before the measurements. A signed informed consent was obtained after explaining the purpose of the study and the Institutional Review Board of the Ophthalmic Research Center approved the study.
A complete ocular examination was performed including slit-lamp biomicroscopy, cycloplegic refraction, best spectacle-corrected visual acuity (BSCVA) using the Snellen acuity chart, intraocular pressure measurement, and dilated funduscopy. To avoid the effect of sleeping and diurnal variation on corneal thickness measurements, all subjects were examined in the morning, at least 3 h after awakening, when the post-awakening decline had already occurred.
For Orbscan II measurements, an acoustic equivalent factor of 0.92 was preset. This custom factor was previously derived from an independent set of normal subjects. Subjects were seated in front of the device: their chin placed on a chin rest and asked to keep both eyes open. The participant's eye was aligned along the visual axis by a central fixation light and the corneal image was brought into focus with the help of two reflected and inverted half circles. Orbscan II was set up to obtain central 2 mm corneal thickness and to create eight circles (1.5 mm diameter each) within the 5 to 7 mm zone to measure the average PCT.
For measurements with the Galilei dual Scheimpflug analyzer, the participants were seated with their chin on a chin rest and forehead against the forehead strap. The device was brought into focus and the subject's eye was aligned along the visual axis by a central fixation light. The appropriateness of alignment was checked by using an initial Scheimpflug image formed on the monitor. Measurements were repeated until a good quality image was captured. The measurements were collected at 0.0-mm and between 4 and 7-mm to calculate central and average PCT, respectively.
The noncontact assessments (Orbscan II and Galilei) were performed with no order of preference. Additionally, they were used to determine the thinnest-point corneal thickness in both normal and keratoconic eyes.
The last examination was ultrasonic pachymetry to prevent corneal irregularities caused by this contact technique from interfering with other measurements. The ultrasonic pachymeter US-10000 (Nidek, Kamagori, Japan) was calibrated at the beginning of each reading. The cornea was anesthetized using tetracaine 0.5%. The probe of the pachymeter was aligned perpendicular and central to the pupil as precisely as possible, whereas the patient was instructed to fixate on a distant target, and five consecutive measurements within ±2 μm were averaged to obtain a single result. All measurements were taken by a single experienced operator.
Statistical Analysis
Data were analyzed using SPSS (version 17; SPSS Inc., IL, USA) for Windows XP. MEDCALC software (version 13.2.2; Acacialaan, Ostend, Belgium) was used to draw Bland–Altman plots. Mean and standard deviation (SD) were used to express quantitative values with normal distributions such as age, mean keratometry, spherical equivalent refractive error, CCT, and PCT. Single way repeated measure analysis of variance was used to compare the means of CCT in each group. Peripheral and thinnest-point corneal thickness obtained with the Galilei and Orbscan II were compared in each group using the paired t-test. Regression analysis and intraclass correlation coefficient (ICC) and its 95% confidence interval (CI) were utilized to quantify the correlation between CCT readings by ultrasonic pachymetry and the Galilei, by ultrasonic pachymetry and Orbscan II, and by the Galilei and Orbscan II. Bland–Altman plots and the 95% limits of agreement (LoA) (95% LoA = mean difference ± 1.96 SD) were applied to find the agreement between each pair of devices. The same analyses were used to determine the correlation and agreement between PCT readings by the Galilei and Orbscan II.
RESULTS
In this prospective comparative study, 88 right eyes of 88 refractive surgery candidates and 128 (49 right) eyes of 69 keratoconic patients were included. In the latter group, 20 eyes had mild, 51 had moderate, and 57 had severe keratoconus. Table 1 compares the two study groups in terms of demographic data, BSCVA, and refractive and keratometric readings.
Table 1.
Demographic, visual, and refractive characteristics of the study groups
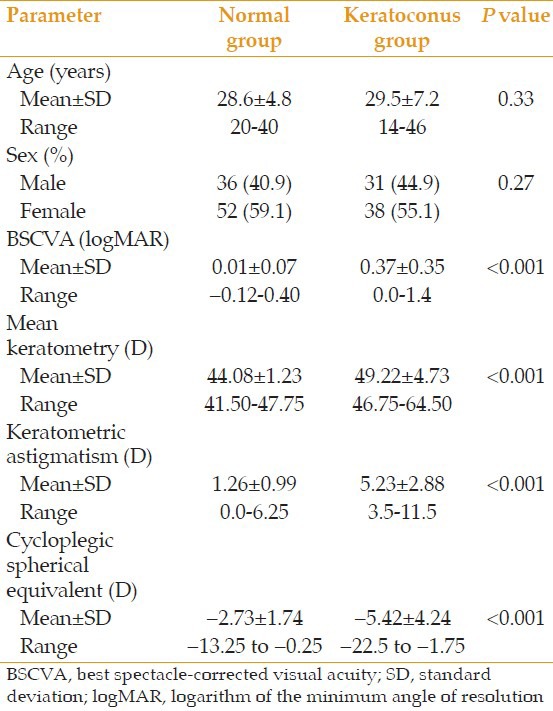
Table 2 demonstrates mean CCT measurements by ultrasonic pachymetry, Orbscan II, and Galilei systems as well as mean PCT measurements by the two latter systems. In the normal group, CCT measured by ultrasonic pachymetry was significantly lower than by the Galilei and Orbscan II (both P < 0.001), while the two latter instruments yielded comparable results (P = 0.99). The mean difference in CCT was the highest between ultrasonic pachymetry and the Galilei (–16.0 ± 19.6 μm; 95% CI, –20.14 to –11.82 μm) and between the Orbscan II and Galilei (–1.5 ± 17.0 μm; 95% CI, –5.07 to 2.14 μm). The mean difference between ultrasonic pachymetry and Orbscan II was –14.5 ± 22.9 μm (95% CI, –19.37 to –9.66 μm).
Table 2.
Central corneal thickness measurements by ultrasonic pachymetry, Galilei and Orbscan II and peripheral corneal thickness by the two latter pachymeters
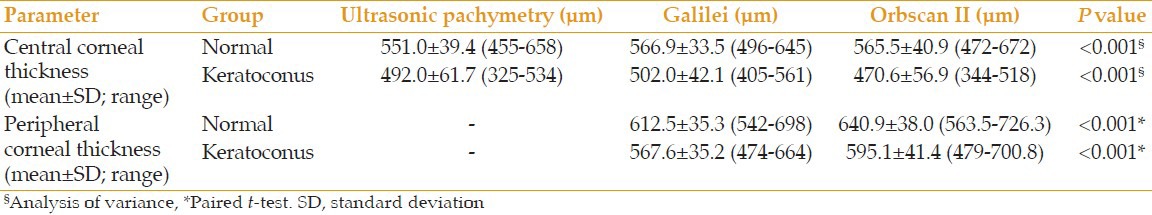
In the keratoconus group, CCT measured by the Galilei was significantly higher than by ultrasonic pachymetry (P=0.01) and Orbscan II (P<0.001). In addition, the results obtained by ultrasonic pachymetry were significantly higher than those obtained by the Orbscan II (P<0.001). The mean difference between the Orbscan II and Galilei was the highest (–31.96±24.99 μm; 95% CI, –36.63 to −27.27 μm) and that between ultrasonic pachymetry and the Galilei was the lowest (–9.9±42.0 μm; 95% CI, –17.69 to –2.02 μm). The mean difference between ultrasonic pachymetry and Orbscan II was 22.4±44.1 μm (95% CI, 14.07–30.81 μm).
Averages of mean measurements of PCT by the Galilei were significantly lower than those by Orbscan II in both study groups [Table 2]. The mean difference in PCT between the Orbscan II and Galilei was 28.93±10.86 μm (95% CI, 26.52–31.35 μm) in the normal group and 27.77±15.80 μm (95% CI, 24.70–30.85 μm) in the keratoconus group. The difference in PCT did not differ significantly in the normal group from that in the keratoconus group (P=0.57).
There was no significant difference in the thinnest-point corneal thickness measured by the Galilei and Orbscan II in the normal group [556.4±34.4 μm (95% CI, 548–564 μm) versus 558.6±40.8 μm (95% CI, 548-567 μm), respectively, P=0.19]. However, the Galilei yielded significantly higher values than Orbscan II in the keratoconus group (473.6±54.6 μm; 95% CI, 462-483 μm vs. 448.8±63.5; 95% CI, 436–459 μm, respectively, P<0.001).
In the keratoconus group, the maximum difference in CCT, PCT, and thinnest-point corneal thickness measurements between the three devices was observed in severe cases.
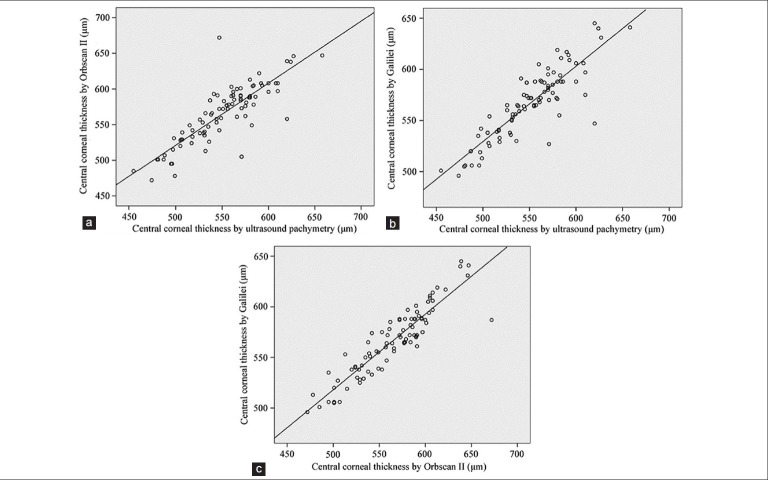
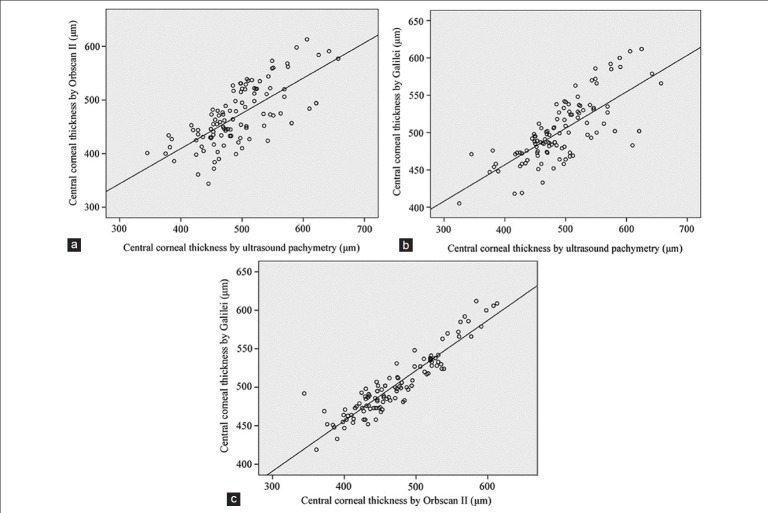
Linear regression analysis showed a significant correlation among the central thickness measurements by the three instruments in both groups [Figures 1 and 2]. The strongest association was observed between the Galilei and Orbscan II, indicating that the results by these two optical systems are better correlated, especially in the normal group [Table 3]. The correlation between central thickness measurements by ultrasonic pachymetry (U) and Galilei (G) was expressed by the equation: U = 1.02 × G –27.63 in the normal group and U = 1.11 × G –63.78 in the keratoconus group. The correlation between ultrasonic pachymetry (U) and Orbscan II (O) was expressed by the equation: U = 0.81 × O + 95.0 in the normal group and U = 0.76 × O + 134.70 in the keratoconus group.
Figure 1.
Scatter plot of central corneal thickness in the normal group measured with ultrasonic pachymetry against the Orbscan II system (a), ultrasonic pachymetry against the Galilei system (b), and Orbscan II against the Galilei system (c). The solid lines represent the fit and the dotted lines represent the 45° angle.
Figure 2.
Scatter plot of central corneal thickness in the keratoconus group measured with ultrasonic pachymetry against the Orbscan II system (a), ultrasonic pachymetry against the Galilei system (b), and Orbscan II against the Galilei system (c). The solid lines represent the fit and the dotted lines represent the 45° angle.
Table 3.
Correlation measured with Pearson (R) and ICC between the different instruments in the two study groups
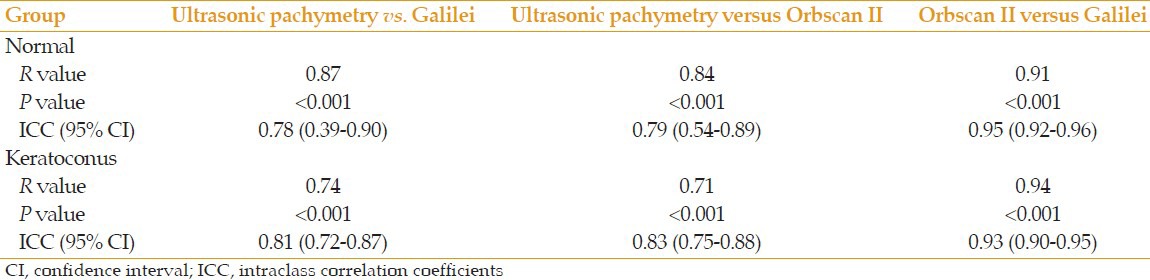
Furthermore, a significant correlation was found between PCT measurements taken by Orbscan II and the Galilei in the normal group (R=0.96, P<0.001, ICC=0.96) as well as in the keratoconus group (R=0.93, P<0.001, ICC=0.91) [Figure 3].
Figure 3.
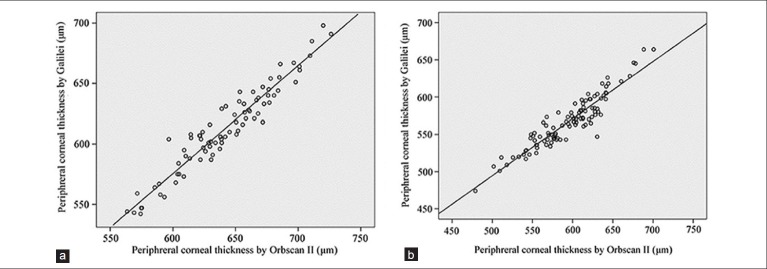
Scatter plot of peripheral corneal thickness in the normal (a) and keratoconus (b) groups measured with the Galilei system against the Orbscan II system.
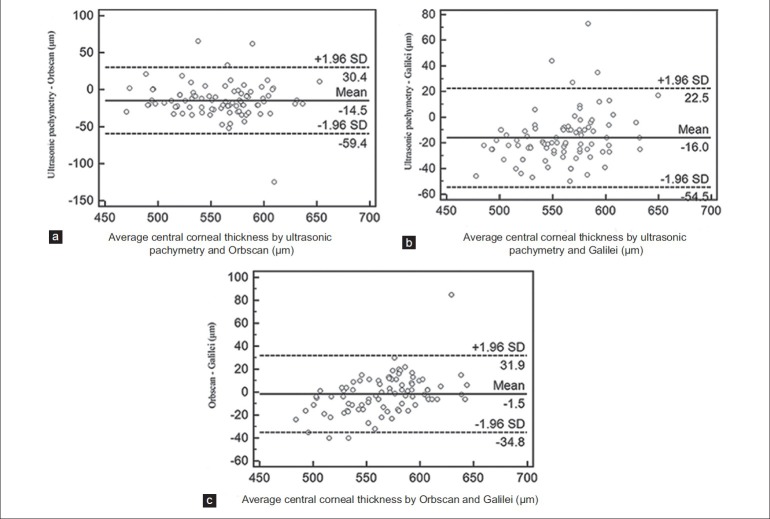
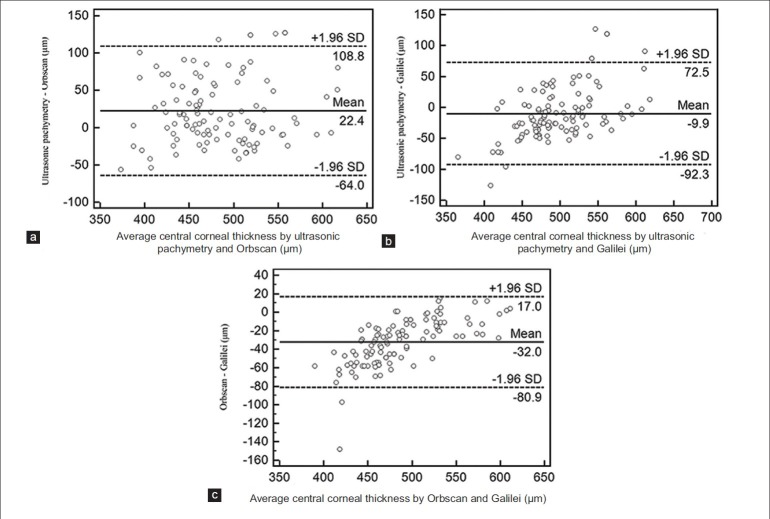
Bland–Altman plots demonstrated that 95% LoA for CCT was –54-22 μm between ultrasonic pachymetry and the Galilei, –35-32 μm between the Orbscan II and Galilei, and −59-30 μm between ultrasonic pachymetry and Orbscan II in the normal group [Figure 4]. In the keratoconus group, 95% LoA was −92-73 μm, −17-81 μm, and −64-109 μm, respectively [Figure 5].
Figure 4.
Bland–Altman plots in the normal group; difference of central corneal thickness against mean central corneal thickness measured with the Orbscan II system and ultrasonic pachymetry (a), with the Galilei system and ultrasonic pachymetry (b), and with the Galilei and Orbscan II systems (c). The solid (middle) lines indicate the mean difference and the dotted (side) lines represent the upper and lower borders of the 95% limits of agreement.
Figure 5.
Bland–Altman plots in the keratoconus group; difference of central corneal thickness against mean central corneal thickness measured with the Orbscan system and ultrasonic pachymetry (a), with the Galilei system and ultrasonic pachymetry (b), and with the Galilei and Orbscan II systems (c). The solid (middle) lines indicate the mean difference and the dotted (side) lines represent the upper and lower borders of the 95% limits of agreement.
About 95% LoA for PCT between the Orbscan II and Galilei was 8-50 μm in the normal group and −3-59 μm in the keratoconus group [Figure 6].
Figure 6.
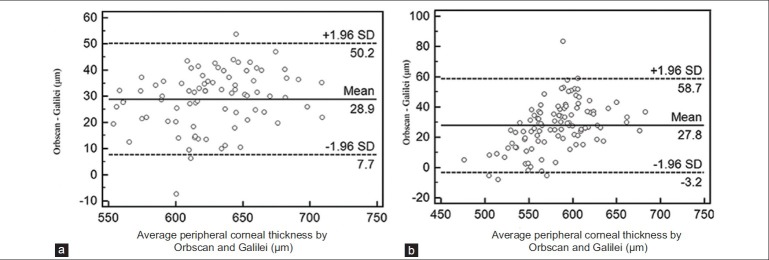
Bland–Altman plots in the normal (a) and keratoconus (b) groups; difference of peripheral corneal thickness against mean peripheral corneal thickness measured with the Orbscan II and the Galilei systems.
DISCUSSION
Previous studies evaluated CCT and PCT in normal and keratoconic eyes. Using ultrasonographic pachymetry, Lotfi Sedigh and Shenasi[11] compared CCT and PCT between eyes with and without keratoconus and found that mean CCT and PCT were significantly lower in eyes with keratoconus. Prospero Ponce et al[12] measured CCT and PCT using ultrasonic pachymetry, Scheimpflug imaging, and high-speed optical coherence tomography (OCT) and compared the results among normal, keratoconus-suspect, and postlaser in situ keratomileusis (LASIK) eyes. They reported that CCT measurements by Scheimpflug and OCT were reproducible but always thinner than ultrasonic pachymetry in normal and keratoconus-suspect eyes. In post-LASIK eyes, OCT pachymetry maps were more accurate than Scheimpflug maps. Uçakhan et al[13] suggested that while Pentacam and ultrasonic pachymetry may be used interchangeably in normal eyes in the clinical setting for the measurement of CCT, one should be cautious interpreting corneal thickness data from Pentacam and ultrasonic pachymetry in eyes with keratoconus. Additionally, they demonstrated that although in normal and mildly keratoconic eyes, Pentacam and ultrasonic pachymetry revealed very high and comparable reproducibility, in moderately keratoconic eyes, Pentacam readings showed better reproducibility than ultrasonic pachymetry. Haque et al[14] compared corneal thickness measurements in individuals with keratoconus using OCT, Orbscan II, and ultrasonic pachymetry and reported that Ultrasonic pachymetry produced the highest corneal thickness readings in the center and apex, compared with Orbscan II and OCT.
Although ultrasonic pachymetry has been the gold standard for CCT measurement,[3,4,5] other noncontact optical techniques can be considered as promising alternatives. Several studies have reported good agreement between the Orbscan system and ultrasonic pachymetry in normal eyes.[15,16,17] However, some studies reported that Orbscan II significantly overestimates CCT values ranging from 23 to 54 μm as compared with ultrasonic pachymetry in normal eyes.[18,19] This reported discrepancy is supported by the results of the current study. The accuracy of ultrasonic pachymetry readings is dependent on operator expertise.[7] Any excessive pressure of the probe on the cornea can displace the 7 to 30-μm-thick precorneal tear film and compress the anterior corneal stroma in addition to the fact that a noncentral nonperpendicular position of the probe can hamper the accuracy of readings by ultrasonic pachymetry.[20] That explains why there is a significant difference between Orbscan II and ultrasonic pachymetry values in normal patients of the current study, in spite of acoustic factor adjustment.
As the Galilei and Orbscan II are both optical pachymeters, their measurements are expected to be comparable as was the case in the normal group in the current study. Supporting our results, Menassa et al[21] have reported that CCT measurements by the Galilei and Orbscan II were comparable in normal eyes. In the keratoconus group, however, we observed that CCT measurements made with Orbscan II were significantly lower than those made with the other two pachymeters. It was previously found that the discrepancy between the Orbscan II system and other pachymeters varies as a function of corneal thickness. For thin corneas, Orbscan II tends to underestimate corneal thickness, while for thick corneas it tends to overestimate it, when compared to the results by the Gailei.[21] Therefore, it may not be appropriate to use the same Orbscan correction factors over a wide range of corneal thicknesses for this purpose.
Another explanation for the discrepancy between the two optical pachymeters observed in the keratoconus, but not in the normal group could be the method used to determine the corneal center. In Scheimpflug imaging, the center of the cornea is detected automatically and measurement alignment is not examiner dependent; however, appropriate alignment in the Orbscan is operator dependent. Therefore, the examiner's skill and the patient's cooperation contribute equally to a reliable Orbscan II measurement, whereas the accuracy of the Galilei measurement depends almost entirely on patient cooperation.[21] The distorted corneal shape in eyes with keratoconus can make it difficult to determine the real position of the corneal center by the optical pachymeters. One testimony to this speculation is the statistically different values for thinnest-point thickness. This value was comparable in normal corneas, while the Galilei yielded significantly higher values in keratoconic eyes than did the Orbscan II.
With regard to PCT, Orbscan imaging gave a value that was approximately 28 μm greater than the Galilei in both study groups. There is no satisfactory explanation for the systematic measurement difference between these two optical systems. The reason for the difference might be explained by the region of measurement. In the Galilei dual Scheimpflug analyzer, the PCT is the mean value of all points within a segment of the circumference between the 4- and 7-mm diameter centered circles. With Orbscan II, corneal thickness was measured in 8 circles in the 5- to 7-mm zone and then averaged. Another explanation is the distinct methodologies of the devices. Because the Galilei analyzer averages data from the left camera and right camera, independent of the inclined surface, it can correct biases derived from decentered measurements and provide a more accurate measurement. On the other hand, it has been shown that peripheral data repeatability from Orbscan can be poorer than CCT measurements due to more incomplete or erroneous slit image acquisition at the periphery.[16,18]
Highly specialized imaging devices are essential in ocular diagnosis and treatment of patients, especially when screening them for refractive surgery.[22] Moreover, with the wide array of available treatment options, including intrastromal corneal ring segments, collagen cross-linking, deep anterior lamellar keratoplasty, and femtosecond laser-assisted corneal transplantation, both CCT and PCT are of utmost importance, not only in the diagnosis of keratoconus, but also in its management.[23] In this study, three different devices gave significantly different CCT and PCT with an unacceptably wide range of 95% LoA. Therefore, we cannot infer as to which of them is the most accurate pachymeter in keratoconic eyes. Clinicians should be aware of this difference when measuring corneal thickness using different devices. A keratoconic patient who is eligible for collagen cross-linking by the Galilei analyzer, for example, may have a thinnest-point corneal thickness <400 μm by Orbscan II, and hence be excluded.
In conclusion, based on the data in our study, the Galilei and Orbscan II provide very similar CCT measurements and can be used interchangeably in normal corneas. However, agreement between these two optical pachymeters profoundly decreases in keratoconic eyes. Additionally, the comparable range of LoA and presence of a fixed systematic bias for PCT measurements may allow appropriate conversion equations to be derived so that measurements from these two optical devices can be interchangeable in both normal and keratoconic eyes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Rabinowitz YS, Rasheed K, Yang H, Elashoff J. Accuracy of ultrasonic pachymetry and videokeratography in detecting keratoconus. J Cataract Refract Surg. 1998;24:196–201. doi: 10.1016/s0886-3350(98)80200-9. [DOI] [PubMed] [Google Scholar]
- 2.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 3.Giasson C, Forthomme D. Comparison of central corneal thickness measurements between optical and ultrasound pachometers. Optom Vis Sci. 1992;69:236–241. doi: 10.1097/00006324-199203000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Miglior S, Albe E, Guareschi M, Mandelli G, Gomarasca S, Orzalesi N. Intraobserver and interobserver reproducibility in the evaluation of ultrasonic pachymetry measurements of central corneal thickness. Br J Ophthalmol. 2004;88:174–177. doi: 10.1136/bjo.2003.023416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rainer G, Petternel V, Findl O, Schmetterer L, Skorpik C, Luksch A, et al. Comparison of ultrasound pachymetry and partial coherence interferometry in the measurement of central corneal thickness. J Cataract Refract Surg. 2002;28:2142–2145. doi: 10.1016/s0886-3350(02)01533-x. [DOI] [PubMed] [Google Scholar]
- 6.Kawana K, Tokunaga T, Miyata K, Okamoto F, Kiuchi T, Oshika T. Comparison of corneal thickness measurements using Orbscan II, non-contact specular microscopy, and ultrasonic pachymetry in eyes after laser in situ keratomileusis. Br J Ophthalmol. 2004;88:466–468. doi: 10.1136/bjo.2003.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.González-Méijome JM, Cerviño A, Yebra-Pimentel E, Parafita MA. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg. 2003;29:125–132. doi: 10.1016/s0886-3350(02)01815-1. [DOI] [PubMed] [Google Scholar]
- 8.Cairns G, McGhee CN. Orbscan computerized topography: Attributes, applications, and limitations. J Cataract Refract Surg. 2005;31:205–220. doi: 10.1016/j.jcrs.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 9.Savini G, Carbonelli M, Barboni P, Hoffer KJ. Repeatability of automatic measurements performed by a dual Scheimpflug analyzer in unoperated and post-refractive surgery eyes. J Cataract Refract Surg. 2011;37:302–309. doi: 10.1016/j.jcrs.2010.07.039. [DOI] [PubMed] [Google Scholar]
- 10.Zadnik K, Barr JT, Gordon MO, Edrington TB. Biomicroscopic signs and disease severity in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Cornea. 1996;15:139–146. doi: 10.1097/00003226-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Lotfi Sedigh A, Shenasi A. Central and peripheral corneal thicknesses in cases with and without keratoconus. Pak J Biol Sci. 2011;14:138–141. doi: 10.3923/pjbs.2011.138.141. [DOI] [PubMed] [Google Scholar]
- 12.Prospero Ponce CM, Rocha KM, Smith SD, Krueger RR. Central and peripheral corneal thickness measured with optical coherence tomography, Scheimpflug imaging, and ultrasound pachymetry in normal, keratoconus-suspect, and post-laser in situ keratomileusis eyes. J Cataract Refract Surg. 2009;35:1055–1062. doi: 10.1016/j.jcrs.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 13.Uçakhan OO, Ozkan M, Kanpolat A. Corneal thickness measurements in normal and keratoconic eyes: Pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J Cataract Refract Surg. 2006;32:970–977. doi: 10.1016/j.jcrs.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 14.Haque S, Simpson T, Jones L. Corneal and epithelial thickness in keratoconus: a comparison of ultrasonic pachymetry, Orbscan II, and optical coherence tomography. J Refract Surg. 2006;22:486–493. doi: 10.3928/1081-597X-20060501-11. [DOI] [PubMed] [Google Scholar]
- 15.Rainer G, Findl O, Petternel V, Kiss B, Drexler W, Skorpik C, et al. Central corneal thickness measurements with partial coherence interferometry, ultrasound, and the Orbscan system. Ophthalmology. 2004;111:875–879. doi: 10.1016/j.ophtha.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 16.Buehl W, Stojanac D, Sacu S, Drexler W, Findl O. Comparison of three methods of measuring corneal thickness and anterior chamber depth. Am J Ophthalmol. 2006;141:7–12. doi: 10.1016/j.ajo.2005.08.048. [DOI] [PubMed] [Google Scholar]
- 17.Amano S, Honda N, Amano Y, Yamagami S, Miyai T, Samejima T, et al. Comparison of central corneal thickness measurements by rotating Scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology. 2006;113:937–941. doi: 10.1016/j.ophtha.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 18.Marsich MW, Bullimore MA. The repeatability of corneal thickness measures. Cornea. 2000;19:792–795. doi: 10.1097/00003226-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Yaylali V, Kaufman SC, Thompson HW. Corneal thickness measurements with the Orbscan Topography System and ultrasonic pachymetry. J Cataract Refract Surg. 1997;23:1345–1350. doi: 10.1016/s0886-3350(97)80113-7. [DOI] [PubMed] [Google Scholar]
- 20.Tam ES, Rootman DS. Comparison of central corneal thickness measurements by specular microscopy, ultrasound pachymetry, and ultrasound biomicroscopy. J Cataract Refract Surg. 2003;29:1179–1184. doi: 10.1016/s0886-3350(02)01921-1. [DOI] [PubMed] [Google Scholar]
- 21.Menassa N, Kaufmann C, Goggin M, Job OM, Bachmann LM, Thiel MA. Comparison and reproducibility of corneal thickness and curvature readings obtained by the Galilei and the Orbscan II analysis systems. J Cataract Refract Surg. 2008;34:1742–1747. doi: 10.1016/j.jcrs.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: A review and meta-analysis approach. Surv Ophthalmol. 2000;44:367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 23.Gherghel D, Hosking SL, Mantry S, Banerjee S, Naroo SA, Shah S. Corneal pachymetry in normal and keratoconic eyes: Orbscan II versus ultrasound. J Cataract Refract Surg. 2004;30:1272–1277. doi: 10.1016/j.jcrs.2003.11.049. [DOI] [PubMed] [Google Scholar]