Abstract
Purpose:
To compare the visual, refractive, and keratometric outcomes of single-segment conventional and severe keratoconus (SK) types of Intacs for correction of inferior keratoconus (KCN).
Methods:
A total number of 41 consecutive eyes of 23 patients with a diagnosis of inferior KCN underwent Intacs implantation. Eight eyes were excluded due to postoperative complications (4 eyes) and loss to follow-up (4 eyes) and finally 33 eyes underwent statistical analysis. Two groups were created according to Intacs type insertion; conventional group (17 eyes) and SK groups (16 eyes). Intracorneal ring segments (ICRS) implantation was indicated in keratoconic patients with contact-lens intolerance or reduced best spectacle-corrected visual acuity (BSCVA).
Results:
In the conventional group, mean uncorrected distance visual acuity (UCDVA) improved from 0.45 ± 0.41 preoperatively to 0.69 ± 0.39 six months after surgery representing a gain of 2 Snellen lines, and in the SK group mean UCDVA changed from 0.40 ± 0.35 preoperatively to 0.58 ± 0.48 equivalent to two Snellen lines improvement 6 months after operation (P = 0.48). Mean preoperative BSCVA in the conventional group improved from 0.72 ± 0.41 to 0.86 ± 0.39 (2 lines improvement) postoperatively and in the SK group improved from 0.71 ± 0.69 to 0.75 ± 0.45 (0.50 line improvement) (P = 0.29). Mean preoperative spherical equivalent (SE) decreased from −4.86 ± 2.26 D to −3.57 ± 2.21 D (conventional group) and from −4.20 ± 1.82 D to −3.60 ± 1.89 D (P = 0.34), mean astigmatism (AST) decreased from −5.20 ± 2.07 D and −4.50 ± 2.26 D to −4.02 ± 2.57 D and − 3.18 ± 2.14 D in the conventional and SK groups, respectively (P = 0.68). Finally, mean K min decreased from 47.11 ± 2.51 D to 45.40 ± 3.30 D in the conventional group and from 45.05 ± 2.59 D to 44 ± 3.88 D in the SK group (P = 0.63) and mean K max was decreased from 52.82 ± 3.23 D to 50.52 ± 3.57 D and from 49.72 ± 3.17 D to 48.55 ± 4.50 D, respectively (P = 0.48).
Conclusion:
Single-segment implantation of conventional and SK Intacs improved UCDVA and BSCVA, decreased corneal AST and keratometry in both groups with comparable outcomes.
Keywords: Intacs, Keratoconus, Single-Segment
INTRODUCTION
Keratoconus (KCN) is a bilateral noninflammatory, naturally occurring ectatic corneal condition in which the cornea gets thinner and steeper over time leading to myopia, irregular astigmatism (AST), distortion and sometimes corneal scarring which results in loss of best spectacle corrected visual acuity (BSCVA).[1,2,3,4,5,6,7]
Improvement of visual acuity is conventionally achieved by spectacles and hard contact lenses. However, with progression of the disease, spectacles and contact lenses cannot satisfy the keratoconus patient and minimally invasive surgical techniques such as intracorneal ring segment (ICRS) may be offered.[8,9,10]
The first ever approval for an implant to be permanently placed in the human cornea was granted by the Food and Drug Administration (FDA) in 1999. ICRS are small pieces made of synthetic materials which are implanted in the deep corneal stroma in order to make modifications in corneal curvature.[11,12,13,14,15,16,17]
Two types of ICRS have been developed and used for ectatic corneal management: Intacs and Ferrara rings. Intacs consist of a pair of semicircular pieces of poly(methyl methacrylate)(PMMA) with arc length of 150’ and a hexagonal transverse shape, external diameter of 8.10 mm and internal diameter of 6.77 mm with different thicknesses (0.25-0.45 mm) in 0.05 mm increments. There is an additional Intacs design named severe keratoconus (SK) with an inner diameter of 6.00 mm, oval cross section and two different thicknesses (0.40, 0.45 mm).[11,18] Intacs is manufactured by Addition Technology Inc., Des Plaines, IL, USA.
Intacs act as a passive spacing element which shortens the arc length of the corneal anterior surface, thereby flattening the cornea.[13]
In the majority of KCN cases, there is an inferior cone with steepening and superior flattening. Double segments flatten the cornea inferiorly as well as superiorly, but single-segment induce inferior flattening and superior steepening resulting in greater change in I/S ratio and AST, thus reasonable optical result.[7]
There are some studies comparing the effects of single segment and double segment implantation of Intacs in treatment of KCN[10,11,12,13,14,15,16,17,18] however, no study has evaluated outcomes of conventional versus SK Intacs for management of inferior KCN.
Herein, the outcomes of conventional single-segment and SK single-segment implantation for inferior KCN management have been compared.
METHODS
This study was a prospective consecutive randomized interventional case series. All surgeries were performed at Farabi Eye Hospital, Tehran, Iran by a single surgeon since September 2010.
Patients aged ≥ 18 years with KCN with noncentral cone in respect to horizontal line as documented by Orbscan II or Pentacam recording, contact lens intolerance and clear central cornea were enrolled. The corneal thickness should be at least 450 μ at 7 mm optical zone or over the area in which the Intacs were to be inserted. Contact lens intolerance was defined as poor fitting, intolerable foreign body sensation, and visual disturbance such as low vision, glare, diplopia, halos and scatter.
Exclusion criteria included previous ocular surgery, herpetic keratitis and connective tissue disorders. All patients provided written informed consent.
The types of Intacs were selected by block randomized technique. Patients were evaluated preoperatively and 1, 3 and 12 months after surgery. Postoperative examinations included uncorrected distance visual acuity (UCDVA), best spectacle-corrected visual acuity (BSCVA), manifest and cycloplegic refraction, slit lamp biomicroscopy, Goldmann tonometry, indirect ophthalmoscopy, keratomety and Orbscan II or pentacam.
Surgical Procedure
Operations were performed under topical anesthesia, using a diamond knife set at 70% thinnest point. A 1.8 mm radial incision was formed in the marked position, set on the steep axis of the cornea. Corneal inferior pocket were created using Sinskey and Suarez spreader. One inferior tunnel was then formed using dissector under suction created by a vacuum centering guide. The single-segment Intacs (conventional 450 or SK 450) was implanted in the corneal tunnel. Incision was sutured using a single 10/0 nylon stitch. All procedures were uneventful, all eyes received betamethasone and chloramphenicol eye drops 4 times daily. Sutures were removed 4 weeks after surgery.
Statistical Analysis
Data were analyzed for all patients who successfully completed at least 9-months’ follow-up. Statistical comparisons between preoperative and postoperative values were performed using the Wilcoxon test for UCDVA, BSCVA, manifest refraction spherical equivalent, Kflat and Ksteep (SPSS 15, SPSS Inc., Chicago, Illinois, USA).
Changes in all parameters were compared using independent sample t-test and P < 0.05 was considered as statistically significant.
RESULTS
Of a total of 41 eyes in 23 patients successfully implanted with Intacs (Addition Technology Inc., Des Plaines, IL, USA), 33 eyes of 22 patients including 19 male (57.6%) and 14 female (42.4%), 21 OD (63.6%), and 12 OS (36.4%) subjects with mean age of 27.6 ± 5.98 (range 21 to 43) years were enrolled for statistical analysis. In four eyes the Intacs were removed due to segment extrusion including one eye with suture infection not responding to antibiotics 3 weeks after implantation, one eye with incision site vascularization 3 months postoperatively and 2 eyes with surface perforation 4 months after surgery. Four other eyes were excluded because of loss to follow up. Mean follow-up was 13.33 ± 1.94 (range 11 to 180) months. Intacs was 450 μm in conventional and SK type.
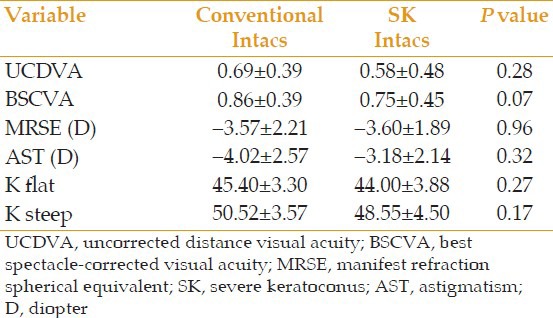
In the conventional group, mean UCDVA improved from 0.45 ± 0.41 preoperatively to better than 0.69 ± 0.39 six months after surgery representing a gain of 2 Snellen lines. In the SK group, mean UCDVA changed from 0.40 ± 0.35 preoperatively to 0.58 ± 0.48 representing two Snellen lines of improvement 6 months after operation (P = 0.48). Mean preoperative BSCVA in the conventional group improved from 0.72 ± 0.41 to 0.86 ± 0.39 (2 lines improvement) postoperatively and in the SK group improved from 0.71 ± 0.69 to 0.75 ± 0.45 (0.50 line improvement) (P = 0.29) [Figures 1–3]. Mean preoperative SE decreased from −4.86 ± 2.26 D to −3.57 ± 2.21 D (conventional group) and from −4.20 ± 1.82 D to −3.60 ± 1.89 D (SK group) (P = 0.34), Mean AST decreased from 5.20 ± 2.07 D and 4.50 ± 2.26 D to 4.02 ± 2.57 D and 3.18 ± 2.14 D in conventional and SK groups, respectively (P = 0.68). Finally, K min (K flat) decreased from 47.11 ± 2.51 D to 45.40 ± 3.30 D in the conventional group and from 45.05 ± 2.59 D to 44 ± 3.88 D in the SK group (P = 0.63) and K max (K steep) reduced from 52.82 ± 3.23 D to 50.52 ± 3.57 D and from 49.72 ± 3.17 D to 48.55 ± 4.50 D in the conventional and SK groups, respectively (P = 0.48) [Tables 1-3].
Figure 1.
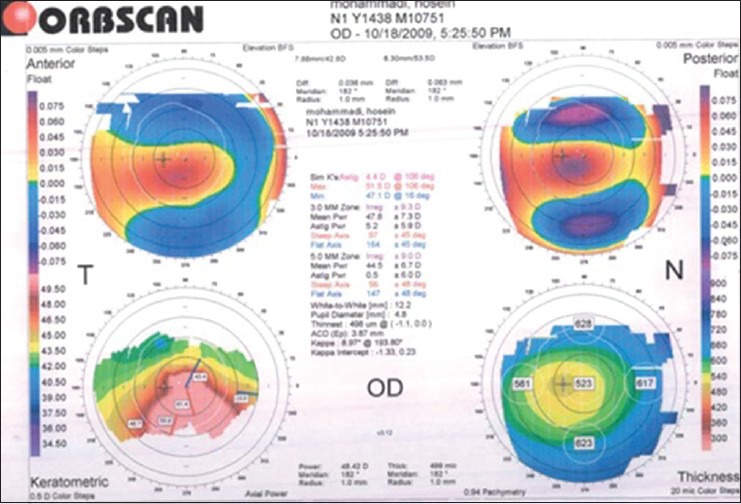
Preoperative Orbsacn of the right eye of a case with inferior keratometry.
Figure 3.

Anterior segment photography of incisional infectious keratitis.
Table 1.
Comparison of preoperative parameters in conventional Intacs group and SK group
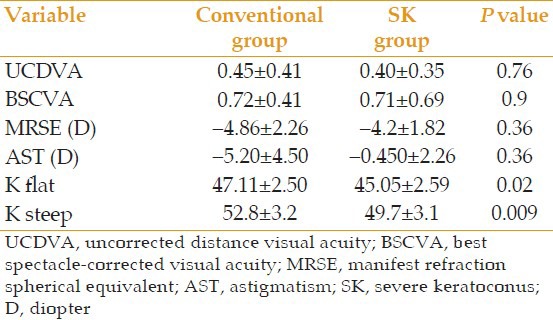
Table 3.
Comparison of variance between conventional Intacs and SK Intacs groups
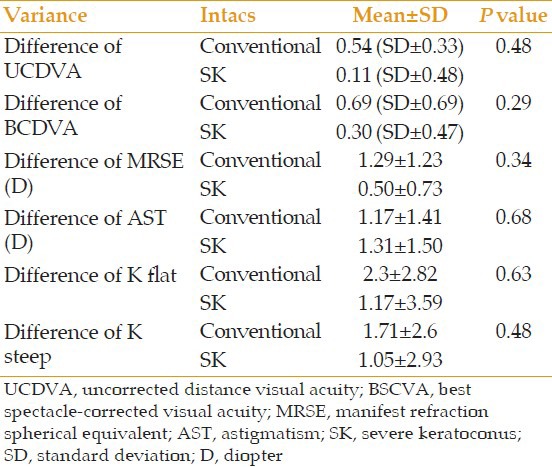
Figure 2.
Postoperative Orbscan of the right eye shows a decrease in keratometry and astigmatism.
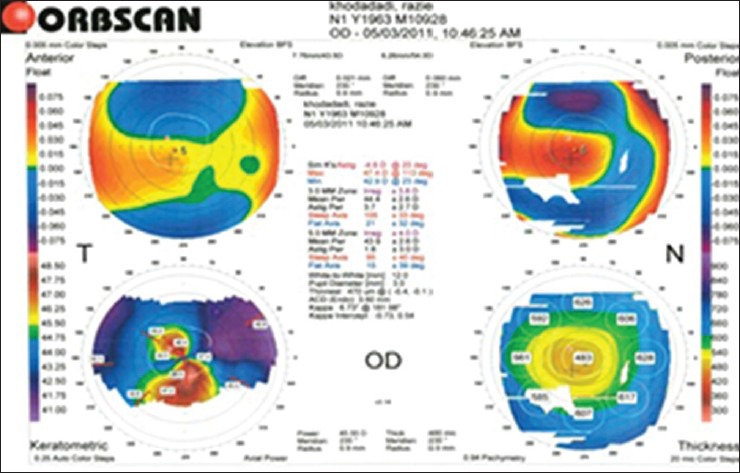
Table 2.
Comparison of postoperative parameters in conventional Intacs and SK Intacs
DISCUSSION
Intacs are relatively new devices for reinforcing the cornea though the arc shortening effect of the corneal lamellae that flattens the central cornea. The keratoconic tissue with thinner structure than normal corneal tissue can be flattened more easily. It is also more logical to reinforce the weak cornea by adding tissue and to avoid further weakening by incisional or ablative measures such as photorefractive keratectomy and laser in situ keratomileusis.[1,2,3,4]
Inserting Intacs for KCN treatment does not eliminate the corneal disease but decreases associated corneal abnormality and improves visual acuity and delays or eliminates the necessity for corneal grafting.
Alió et al[1] evaluated the effect of implanting intracorneal rings on best corrected visual acuity (BCVA) of patients with clear corneal KCN and concluded that 1 or 2 Intacs implantation, according to the preoperative corneal topographic appearance of KCN, safely and effectively reduced corneal steepening and AST in patients with clear corneal KCN along with contact lens intolerance. Mean postoperative UCDVA and BSCVA were significantly improved, and mean keratometric reading was significantly reduced after one year follow-up. The rate of complications reported in their series was low. Implantation of 1 or 2 segments can be performed safely and effectively on the basis of the preoperative corneal topographic aspect of KCN. More ideal outcomes of single-segment implantation may be due to the anatomical change in the keratoconic cornea, which usually occurs asymmetrically in the inferior cornea.
Postoperative results in the current series demonstrated that spherical equivalent error, AST, K steep and K flat significantly decreased and visual acuity improved in almost all cases in both groups. Corneal curvature also decreased in both K steep and K flat parameters, with slightly more reduction in K steep which is consistent with the results of earlier studies.[1,2,3,4,5,6,7,8,9,10,11,12]
In both groups, any line–loss in UCDVA and BSCVA over a period of one year after implantation was not detected as compared to one-month post operation. After the procedure, from 27 eyes with contact lens intolerance 13 eyes including 6 eyes of SK group and 7 eyes of conventional group became contact lens tolerant.
Although the treatment of clear corneal KCN with Intacs seems to be a minimally invasive technique for reducing the corneal steepening, AST and improving the visual acuity, further follow up is required to draw out the ultimate effect of Intacs on the natural progression of KCN and to determine their probable impact on clinical indications and outcomes of penetrating keratoplasty procedure (PKP) or any other surgical procedure which may be performed for involved eyes in the future.[5,6,7,8,9,10,11,12,13,14]
In summary, implanting conventional or SK types of single-segment intracorneal ring is an effective procedure for the treatment of inferior KCN with no significant difference in refraction and visual outcomes and keratometry in two groups.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Alió JL, Artola A, Hassanein A, Haroun H, Galal A. One or 2 Intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005;31:943–953. doi: 10.1016/j.jcrs.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 2.Hellstedt T, Mäkelä J, Uusitalo R, Emre S, Uusitalo R. Treating keratoconus with intacs corneal ring segments. J Refract Surg. 2005;21:236–246. doi: 10.3928/1081-597X-20050501-06. [DOI] [PubMed] [Google Scholar]
- 3.Pokroy R, Levinger S. Intacs adjustment surgery for keratoconus. J Cataract Refract Surg. 2006;32:986–992. doi: 10.1016/j.jcrs.2006.02.032. [DOI] [PubMed] [Google Scholar]
- 4.Rabinowitz YS. Intacs for keratoconus. Curr Opin Ophthalmol. 2007;18:279–283. doi: 10.1097/ICU.0b013e3281fc94a5. [DOI] [PubMed] [Google Scholar]
- 5.Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treating keratoconus: One-year results. Ophthalmology. 2001;108:1409–1414. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 6.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 7.Sharma M, Boxer Wachler BS. Comparison of single-segment and double-segment Intacs for keratoconus and post-LASIK ectasia. Am J Ophthalmol. 2006;141:891–895. doi: 10.1016/j.ajo.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 8.Chan CC, Sharma M, Wachler BS. Effect of inferior-segment Intacs with and without C3-R on keratoconus. J Cataract Refract Surg. 2007;33:75–80. doi: 10.1016/j.jcrs.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Coskunseven E, Jankov MR, 2nd, Hafezi F, Atun S, Arslan E, Kymionis GD. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35:2084–2091. doi: 10.1016/j.jcrs.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Sansanayudh W, Bahar I, Kumar NL, Shehadeh-Mashour R, Ritenour R, Singal N, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–113. doi: 10.1016/j.jcrs.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 11.Pokroy R, Levinger S, Hirsh A. Single Intacs segment for post-laser in situ keratomileusis keratectasia. J Cataract Refract Surg. 2004;30:1685–1695. doi: 10.1016/j.jcrs.2004.02.050. [DOI] [PubMed] [Google Scholar]
- 12.Piñero DP, Alio JL, El Kady B, Coskunseven E, Morbelli H, Uceda-Montanes A, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: Mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009;116:1675–1687. doi: 10.1016/j.ophtha.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Colin J, Malet FJ. Intacs for the correction of keratoconus: Two-year follow-up. J Cataract Refract Surg. 2007;33:69–74. doi: 10.1016/j.jcrs.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 14.Bourcier T, Borderie V, Laroche L. Late bacterial keratitis after implantation of intrastromal corneal ring segments. J Cataract Refract Surg. 2003;29:407–409. doi: 10.1016/s0886-3350(02)01484-0. [DOI] [PubMed] [Google Scholar]
- 15.Colin J. European clinical evaluation: Use of Intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–755. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 16.Alió JL, Shabayek MH, Belda JI, Correas P, Feijoo ED. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006;32:756–761. doi: 10.1016/j.jcrs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Rabinowits YS. Intacs for keratoconus. Int Ophthalmol Clin. 2013;50:63–76. doi: 10.1097/IIO.0b013e3181e21b76. [DOI] [PubMed] [Google Scholar]
- 18.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]


