Abstract
Purpose:
To assess the refractive and visual outcomes following cataract surgery and implantation of the AcrySof IQ Toric SN6AT2 intraolcular lens (IOL) (Alcon Laboratories, Inc., Fort Worth, TX, USA) in patients with low corneal astigmatism.
Methods:
This study is a retrospective, consecutive, single surgeon series of 98 eyes of 88 patients (with low preoperative corneal astigmatism) undergoing cataract surgery and implantation of the AcrySof IQ Toric SN6AT2 IOL. Postoperative measurements were obtained 1-month postsurgery. Main outcome measures were monocular distance visual acuity and residual refractive astigmatism.
Results:
Mean preoperative corneal astigmatic power vector (APV) was 0.38±0.09 D. Following surgery and implantation of the toric IOL, mean postoperative refractive APV was 0.13±0.10 D. Mean postoperative distance uncorrected visual acuity was 0.08±0.09 logMAR. Postoperative spherical equivalent refraction (SER) resulted in a mean of –0.23±0.22 D, with 96% of eyes falling within 0.50 D of the target SER.
Conclusion:
The AcrySof IQ Toric SN6AT2 IOL is a safe and effective option for eyes undergoing cataract surgery with low levels of preoperative corneal astigmatism.
Keywords: Astigmatism, Cataract, Refractive Errors, Toric Intraocular Lens
INTRODUCTION
Management of corneal astigmatism during cataract surgery is a common scenario in today's clinical practice. The various treatment options for correcting corneal astigmatism include excimer laser refractive procedures such as photorefractive keratectomy and laser in situ keratomileusis, astigmatic keratotomy using corneal relaxing incisions, toric phakic or pseudophakic anterior or posterior chamber intraocular lenses (IOLs), and the conventional use of spectacles and contact lenses.[1]
The implantation of toric IOLs has been shown to be an effective method for reducing refractive astigmatism and postoperative spectacle dependence in patients undergoing cataract surgery.[1,2,3,4] In eyes with lower amounts of preoperative corneal astigmatism (approximately 0.75-1.50 D), numerous studies have confirmed the improved refractive and visual outcomes of the AcrySof Toric SN60T3 IOL (Alcon Laboratories Inc., Fort Worth, TX, USA) over a spherical IOL alternative.[4,5,6] Until recently, this toric IOL with a cylinder power of 1.50 D, approximating to 1.03 D at the corneal plane, was the lowest powered toric IOL in the AcrySof range (Alcon Laboratories Inc., USA).[7]
Over time, with technological advances in surgical techniques, the ability of toric IOLs to accurately correct astigmatism is expected to improve. Recently, Alcon released an addition to its AcrySof IQ Toric range, the AcrySof IQ Toric SN6AT2 (Alcon Laboratories, Inc., Fort Worth, TX, USA), with a cylinder power of 1.00 D at the IOL plane, approximating to 0.68D at the corneal plane. AcrySof single piece IOLs have been designed to achieve maximal IOL stability through its haptics and with the biomaterial of this lens demonstrating adhesive properties that support adherence to the capsular bag.[8] In one study, the rotational stability of this one piece acrylic toric IOL was shown to be significantly better than a plate-haptic silicone IOL.[9] Of late, one study investigated the higher order aberration profile of patients following implantation with the AcrySof IQ Toric IOL and reported that postoperative spherical aberration was significantly higher compared with patients implanted with the Tecnis toric IOL (Abbott Medical Inc., Santa Ana, CA, USA), however this difference had no effect on overall visual quality.[10]
The postoperative refractive benefit of this new, low powered toric IOL in eyes with low levels of corneal astigmatism is yet to be reported. Assessing the performance of this IOL in a clinical setting is particularly pertinent since low levels of corneal astigmatism are common in the population. In one study, approximately 64.4% of patients presenting with cataract had between 0.25 and 1.25 D of corneal astigmatism, whereas higher levels (>2.50 D) were much less common.[11] Another large study of cataractous eyes found that only 4.2% of eyes had no corneal astigmatism, whereas the majority of patients (76.8%) exhibited between 0.25 and 1.50 D of corneal astigmatism.[12]
In this study, we examine the refractive and visual outcomes following cataract surgery and implantation of the AcrySof IQ Toric SN6AT2 IOL in eyes with low corneal astigmatism, in order to assess the performance of this new IOL.
METHODS
This study is a retrospective analysis of consecutive cases undergoing cataract surgery and implantation of the AcrySof IQ Toric SN6AT2 IOL between January 2011 and August 2012, performed by one ophthalmic surgeon (JP) in Bundaberg, Queensland, Australia. Patients with ocular pathology precluding an optimal postoperative outcome were excluded from the study. In all cases, the target spherical equivalent refraction (SER) was for optimal distance vision (target SER range -0.44 to + 0.12 DS). Written informed consent was obtained from all patients prior to cataract surgery and the study was conducted in accordance with the tenets of the Declaration of Helsinki. Follow-up was a minimum of 1-month for inclusion in the study.
All patients underwent a preoperative comprehensive ocular examination. In addition to patient demographics, preoperative data included objective refraction, best corrected distance visual acuity (BCVA) and ocular biometry using the IOLMaster (Carl Zeiss Meditec, Jena, Germany).
Postoperative (1-month) measures included distance uncorrected visual acuity (UCVA), subjective refraction and BCVA. The SRK/T formula was used for lens power calculations. IOL toric power calculations were calculated using the AcrySof IQ Toric IOL online calculator (AcrySof Toric Calculators, (Alcon Laboratories Inc., USA).[13] Surgically induced astigmatism was set at 0.20 D based on internal modeling for the ophthalmologist.
All surgeries were performed at one location, under peribulbar anesthesia, utilizing a standard phacoemulsification technique with 2.2 mm sutureless corneal wounds placed temporally. Prior to surgery the operative eye was marked with reference markings at the desired angle of insertion while the patient was seated upright at the slit-lamp to compensate for cyclorotation. IOL orientation was assessed at the end of surgery. Postoperative topical antibiotics (ofloxacin 0.3%) were prescribed for 14 days and topical steroids (dexamethasone NaCl 0.1%) for 28 days. Postoperative follow-up was scheduled for 1-day, 1-week and 1-month. The postoperative results presented are from the 1-month review visit.
Statistical Analysis
Preoperative keratometry and objective refraction data and postoperative subjective refraction data were converted into power vectors[14] M (spherical equivalent), J0 (90/180 astigmatic power) and J45 (45/135 oblique astigmatic power) using the following formulae where S denotes the spherical component of refraction, C denotes the sign and magnitude of astigmatism and α denotes the axis of astigmatism. The astigmatic power vector (APV) was also calculated for each patient. This metric is a nonsigned scalar, which represents the magnitude, but not direction (axis) of astigmatism.

Refractive power vectors transform conventional sphero-cylindrical components into independent, orthogonal components more appropriate for statistical analysis. Since the data set contained a mixture of right and left eyes, all left eye data was transposed to right eye data to eliminate possible errors as a result of enantiomorphism (mirror symmetry between right and left eyes).[15] Visual acuity data were converted to the logarithm of the minimal angle of resolution (logMAR) for statistical analysis. Data analysis was conducted using SPSS version 19.0 (IBM Inc., NY, USA). Pearson's correlation coefficient was used to examine the association between variables of interest. P<0.05 were considered as statistically significant.
RESULTS
Ninety-eight eyes (50 right and 48 left) of 88 patients were implanted with the AcrySof SN6AT2 IOL. The preoperative characteristics are displayed in Table 1. Mean preoperative corneal APV (a metric of astigmatic magnitude, disregarding orientation) was 0.38±0.09 D, with a mean target SER of –0.20±0.13 D. Postoperative measurements are displayed in Table 2. As expected, following cataract surgery and IOL implantation there was a marked improvement in BCVA (mean improvement: 0.18 logMAR, approximately two lines). Mean postoperative UCVA was 0.08 ± 0.09 logMAR.
Table 1.
Preoperative measurements
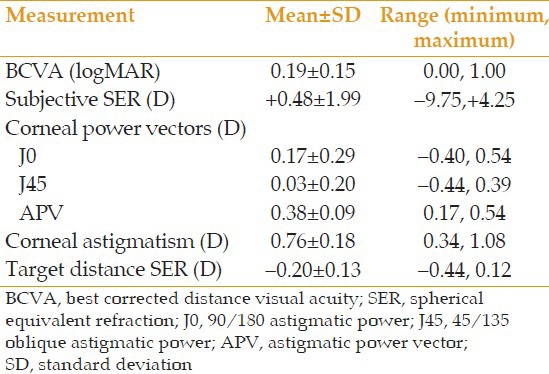
Table 2.
Postoperative measurements
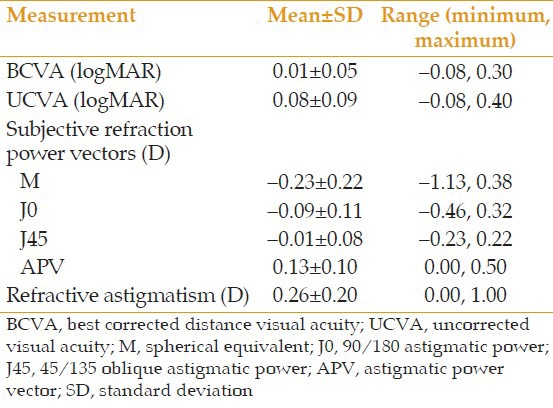
Figure 1 displays the distribution of the difference in postoperative SER from the preoperative target SER for all eyes. Overall, 84% of patients achieved a postoperative SER within 0.25 D of the target, and when extended to within 0.50 D of the target, a 96% success rate was achieved. The mean postoperative SER of –0.23±0.22 D was not significantly different from the target SER calculated prior to surgery (-0.20±0.13 D, P=0.16).
Figure 1.
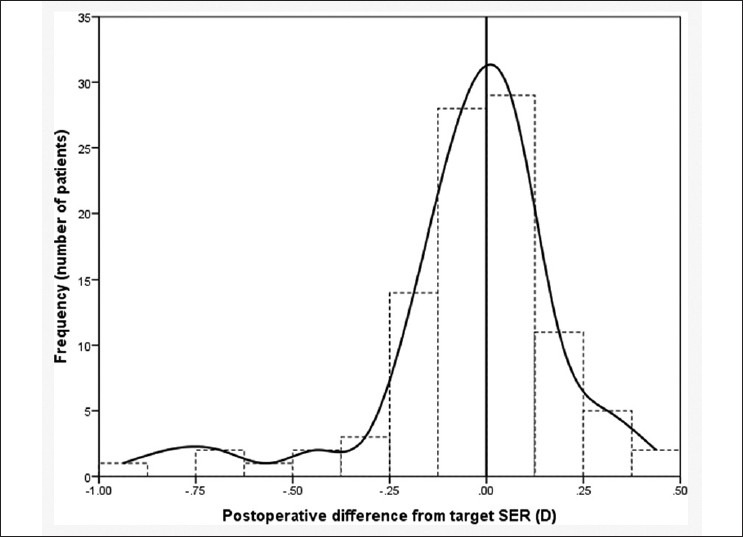
Distribution of the postoperative difference in spherical equivalent refraction (SER) from the preoperative target SER, for 98 eyes implanted with the AcrySof SN6AT2 intraocular lens.
Mean postoperative refractive APV was 0.13 ± 0.10 D, representing a mean reduction of 0.25 D (equivalent to 0.50 D in sphero-cylindrical terminology) from the mean preoperative corneal APV, a statistically significant result (P<0.0001). Figure 2 shows the distribution of preoperative corneal and postoperative refractive APVs J0 and J45 for all cases. The notable clustering of the postoperative data points closer to the origin (i.e. 0 D of J0 and J45) demonstrates the reduction in astigmatism following implantation of the toric IOL. Of note, in our series of cases, no eye suffered an increase in refractive astigmatism post IOL implantation.
Figure 2.
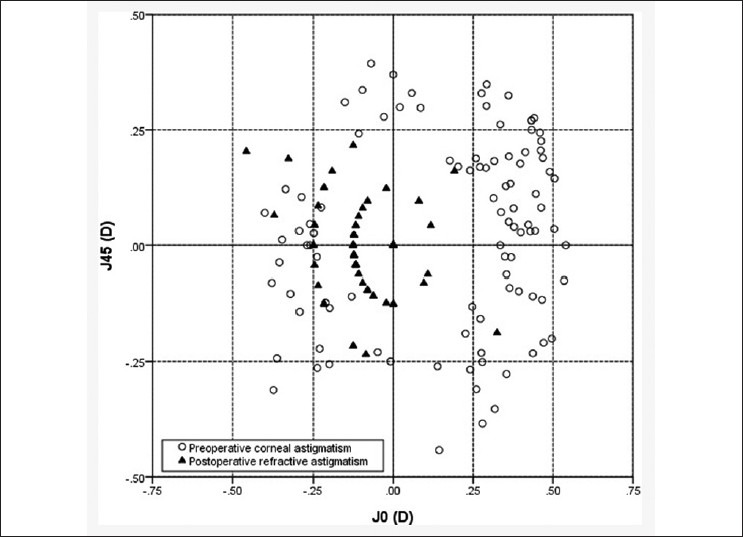
Distribution of preoperative corneal astigmatic power vectors (APV), (open circles, n=98) and postoperative refractive APVs (filled triangles, n=98) for eyes implanted with the AcrySof SN6AT2 intraocular lens. J0 (90/180 astigmatic power), J45 (45/135 oblique astigmatic power).
In our population of patients with minimal postoperative refractive astigmatism, there was a moderate yet significant positive correlation between refractive APV and UCVA (r=0.33, P<0.001), [Figure 3] which suggests that even low levels of residual astigmatism influence visual quality (ignoring the influence of uncorrected spherical refractive error).
Figure 3.

Uncorrected visual acuity (logMAR) as a function of postoperative refractive astigmatic power vector (D) for all patients. Linear regression (solid line) with 95% confidence interval (dashed lines).
At 1-month follow-up, no patient required postoperative IOL adjustments. While measures of IOL axis rotation were not recorded for each individual patient, this was assessed at the follow-up visit, and no patients suffered from a clinically significant rotation of the toric IOL off axis. No patients suffered postoperative complications.
DISCUSSION
This is the first independent study to assess the refractive and visual outcomes following implantation of the AcrySof SN6AT2 IOL in eyes with low preoperative corneal astigmatism. Given the high prevalence of low corneal astigmatism in the population presenting for cataract surgery, with figures of up to 76.8% of patients with between 0.25 and 1.50 D of astigmatism,[11,12] this study provides clinical data, which will be of use to ophthalmic surgeons when determining the most appropriate IOL for their patients.
Previous studies on eyes with relatively low amounts of preoperative corneal astigmatism comparing the AcrySof T3 toric IOL with a spherical IOL have shown definitively favorable results for the toric IOL (reduced residual astigmatism and better UCVA),[5,6] as expected given the higher astigmatic correction with the AcrySof T3 toric IOL (1.50 D). In a small comparison study of 22 patients with preoperative corneal astigmatism around 1.00 D, mean residual refractive astigmatism was significantly lower in patients implanted with the AcrySof T3 toric IOL (0.33 D) compared with the spherical IOL group (0.88 D).[6] These findings were confirmed in a much larger cohort of 323 patients with preoperative corneal astigmatism between 0.75 and 1.38 D. The mean residual refractive astigmatism was significantly lower in the toric IOL group by 0.75 D.[5]
In the current study, we did not design a protocol, which included a spherical IOL control group as our initial impressions through a pilot study with the toric IOL showed clearly better refractive outcomes in comparison; thus, it was deemed to be inconsistent with patient's best interests to continue to implant a spherical IOL in these eyes. Our mean preoperative corneal astigmatism (0.76 D in sphero-cylindrical terminology) was lower than in the aforementioned AcrySof T3 toric IOL studies, in accordance with the manufacturers recommendations for the new toric IOL. The mean postoperative refractive APV significantly reduced from the preoperative corneal APV (P<0.0001). Converting the APV to cylindrical values in the more conventional sphero-cylindrical terminology (equivalent to APV multiplied by 2) revealed a mean residual refractive astigmatism of 0.26 D. Presuming cataract surgery and IOL implantation with a spherical IOL would not significantly compensate for any preoperative corneal astigmatism, the benefit to postoperative refractive astigmatism of implanting this low powered toric IOL according to our data would be around 0.50 D. Notably, this benefit to a patient's refractive outcome following cataract surgery is well within the skills-set of ophthalmic surgeons who currently implant toric IOLs, without an increase in surgical risk, operating time or operating cost.
Measures of postoperative distance UCVA, one indicator of visual performance, revealed a promising mean UCVA of 0.08 logMAR (6/7.5+1) in our study, while BCVA corrected to a mean of 0.01 logMAR (effectively 6/6). Postoperative SER (power vector M) was on average slightly more myopic by 0.03 D than the calculated target SER, however this was not a statistically significant difference (P=0.16). Uncorrected spherical refractive error will influence postoperative UCVA and in cases of low corneal astigmatism may have a greater impact on visual outcomes than the level of residual astigmatism. Nonetheless, Figure 3 highlights the positive correlation between postoperative refractive APV and UCVA, suggesting that low amounts of residual refractive astigmatism are associated with a reduction in UCVA. Overall, with 96% of eyes achieving a postoperative SER result within 0.50 D of the target [Figure 1], this is an encouraging result regarding the predictability of implanting the IOL used in this study.
The results of our study have demonstrated a clear refractive benefit of the toric IOL in eyes with low corneal astigmatism. Using these results to infer a clinical or visual benefit when there are relatively small changes in refractive astigmatism is however a more difficult task. Of note in our study, the postoperative visual acuity measurements were conducted in standard consultation room illumination (i.e., photopic conditions). The benefits of the toric IOL may be more apparent if measured under mesopic/scotopic conditions or for low contrast acuity tasks, where small differences in residual refractive astigmatism may result in more obvious degradation in vision quality as pupil size increases. In addition, we have only measured distance visual acuity. While astigmatism may also degrade the quality of near vision (or a small amount of against the rule astigmatism may enhance near vision), since we only examined eyes with a target SERs for optimal distance vision, we cannot comment on the performance of the toric IOL with respect to near vision. Future studies examining the efficacy of low powered toric IOLs should also take into consideration subjective visual performance following implantation based on spectacle independence and quality of life through patient feedback or validated questionnaires.
A possible limitation of this study includes the 1-month period of follow-up in all patients. We are unable to comment on the long-term postoperative outcomes of patients receiving the toric IOL, in particular regarding IOL stability. However, a large recent randomized trial conducted with an extended 1-year follow-up after cataract surgery in eyes receiving either the AcrySof Toric or AcrySof spherical IOL, found the mean IOL rotation of the AcrySof Toric IOL to be 3.8°, demonstrating good long-term rotational stability.[4]
In summary, the toric IOL investigated in this study is a safe and effective option for implantation during cataract surgery in eyes with low amounts of preoperative corneal astigmatism. The AcrySof SN6AT2 IOL showed a statistically significant reduction in residual refractive astigmatism of around 0.50 D when compared with preoperative corneal astigmatism. Importantly, this benefit can be achieved within the current skills-set of ophthalmic surgeons fitting toric IOLs and comes without detriment to surgical risks, operating time or operating costs-representing a “win-win” scenario from a patient's perspective. Further study of this toric IOL in mesopic or scotopic conditions, including comparisons to a spherical IOL control group would allow for more definitive conclusions on the benefits to vision and spectacle independence.
ACKNOWLEDGMENTS
This work has been presented in part at the Australasian Society of Cataract and Refractive Surgeons annual conference, November 17-19, 2011, Canberra, Australia.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Bauer NJ, de Vries NE, Webers CA, Hendrikse F, Nuijts RM. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg. 2008;34:1483–1488. doi: 10.1016/j.jcrs.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 2.Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007;18:58–61. doi: 10.1097/ICU.0b013e328011f9bf. [DOI] [PubMed] [Google Scholar]
- 3.Lane SS, Ernest P, Miller KM, Hileman KS, Harris B, Waycaster CR. Comparison of clinical and patient-reported outcomes with bilateral AcrySof toric or spherical control intraocular lenses. J Refract Surg. 2009;25:899–901. doi: 10.3928/1081597X-20090617-05. [DOI] [PubMed] [Google Scholar]
- 4.Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117:2104–2111. doi: 10.1016/j.ophtha.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 5.Ernest P, Potvin R. Effects of preoperative corneal astigmatism orientation on results with a low-cylinder-power toric intraocular lens. J Cataract Refract Surg. 2011;37:727–732. doi: 10.1016/j.jcrs.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 6.Statham M, Apel A, Stephensen D. Comparison of the AcrySof SA60 spherical intraocular lens and the AcryS of Toric SN60T3 intraocular lens outcomes in patients with low amounts of corneal astigmatism. Clin Experiment Ophthalmol. 2009;37:775–779. doi: 10.1111/j.1442-9071.2009.02154.x. [DOI] [PubMed] [Google Scholar]
- 7.USA: Alcon Laboratories, Inc; [Last Accessed on 2013 Feb 12]. www.alcon.com . [Google Scholar]
- 8.Linnola RJ, Sund M, Ylönen R, Pihlajaniemi T. Adhesion of soluble fibronectin, laminin, and collagen type IV to intraocular lens materials. J Cataract Refract Surg. 1999;25:1486–1491. doi: 10.1016/s0886-3350(99)00238-2. [DOI] [PubMed] [Google Scholar]
- 9.Chua WH, Yuen LH, Chua J, Teh G, Hill WE. Matched comparison of rotational stability of 1-piece acrylic and plate-haptic silicone toric intraocular lenses in Asian eyes. J Cataract Refract Surg. 2012;38:620–624. doi: 10.1016/j.jcrs.2011.10.037. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira TB, Almeida A. Comparison of the visual outcomes and OPD-scan results of AMO Tecnis toric and Alcon Acrysof IQ toric intraocular lenses. J Refract Surg. 2012;28:551–555. doi: 10.3928/1081597X-20120703-03. [DOI] [PubMed] [Google Scholar]
- 11.Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70–75. doi: 10.1016/j.jcrs.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 12.Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–368. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 13.USA: Alcon Laboratories, Inc; [Last accessed on 2013 Feb 12]. AcrySof Toric Calculators. www.acrysoftoriccalculator.com . [Google Scholar]
- 14.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–375. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Smolek MK, Klyce SD, Sarver EJ. Inattention to nonsuperimposable midline symmetry causes wavefront analysis error. Arch Ophthalmol. 2002;120:439–447. doi: 10.1001/archopht.120.4.439. [DOI] [PubMed] [Google Scholar]


