Abstract
Background
The aim of this study was to assess whether high-resolution impedance-manometry (HRIM) could be utilized to assess bolus retention similar to the timed barium esophagram (TBE).
Method
20 achalasia patients [10 males, ages 21–79] were prospectively evaluated with HRIM and TBE to determine the correlation between barium column height and the impedance bolus height (IBH). The TBE protocol utilized a 200 ml barium challenge and the HRIM protocol utilized a 200 ml saline challenge protocol. Both protocols were performed in an upright position and the heights of the barium and impedance columns were measured at 1 and 5 minutes. Analysis of IBH was performed with a topographic technique and a spatial impedance variation plot.
Results
There was no significant difference between the median IBH and barium column at 1 minute [IBH 12.0 cm (IQR, 8.0–18.0), TBE 12.0 cm (IQR, 7.0–19.0), P=0.90] or 5 minutes [IBH 11.0 cm (IQR, 1.0–17.0), TBE 9.0 cm (IQR, 4.0–12.0), P=0.47]. Additionally, the correlation between the two measurements at 1 and 5 minutes was 0.60 and 0.86, respectively. Using a barium column or impedance height of >5.0 as a definition of bolus retention was associated with 75% concordance at 1 minute and 95% concordance at 5 minutes.
Conclusion
There was excellent agreement between TBE and HRIM for assessing bolus retention at 5 minutes. Thus, HRM with impedance may be utilized as a single test to assess bolus retention and motor function in the management of achalasia.
Keywords: Achalasia, manometry, esophagram, impedance
INTRODUCTION
Achalasia is diagnosed by demonstrating dysfunction of lower esophageal sphincter relaxation and aperistalsis in the absence of a mechanical obstruction. The major diagnostic modalities utilized to establish the diagnosis and manage the disease are endoscopy, timed barium esophagram (TBE) and esophageal manometry. Although each of these tests have unique attributes that make them valuable, there is significant overlap in the information acquired and many patients eventually end up having all three tests performed. Endoscopy is essential as it provides a method for ruling out obstruction or pseudoachalasia and thus, it is required before definitive therapy can be rendered. On the other hand, manometry or barium esophagram can both be diagnostic and therapy could be instituted when either of these tests are abnormal. However, current guidelines still emphasize that manometry is the “gold standard” and that this should be obtained to confirm the diagnosis as it is defined by abnormal motor function1.
In terms of follow up, there is less evidence supporting the use of manometry and previous data using a TBE protocol have shown it to be helpful in evaluating treatment success2, 3. Bolus retention on TBE is a useful metric in assessing treatment outcome in that it can identify patients at risk for requiring further treatment. Although an EGJ pressure after treatment of <10 mmHg has also been identified as a predictor of good outcome4, there are conflicting reports regarding the utility of this measurement in the evaluation of patients after treatment5. Thus, the standard follow up for achalasia is not well defined.
Given recent advances in manometric techniques, we hypothesized that high resolution manometry combined with impedance could be leveraged to provide a more comprehensive assessment of outcome than TBE or manometry alone. Recently, our group reported that high resolution manometry could complement other functional studies in assessing achalasia treatment outcomes6. However, bolus retention on TBE still appeared to be an important outcome measure as it did not always correlate with manometric findings. Previous studies have attempted to utilize impedance to assess bolus retention and outcomes in achalasia. However, the methodology and analysis was hampered by the low baseline impedance value and confounding air entrapment7, 8. Hence, our aim was to develop and validate a new strategy to assess bolus retention with a modified esophageal pressure-impedance topography protocol using 200 milliliters of saline and assessing impedance bolus height (IBH) at the same time intervals as utilized in the standard TBE protocol.
MATERIALS AND METHODS
Subjects
20 achalasia patients (11 males; 21–79 years of age) were prospectively studied. All 20 patients underwent endoscopy, HRIM, TBE, and symptom assessment using the Impaction Dysphagia Questionnaire (IDQ). The endoscopy, TBE and standard HRIM protocol were part of the clinical evaluation, while the questionnaire was part of our ongoing prospective study assessing the correlation between manometric variables and symptom outcomes. Given that we were testing the agreement between HRIM and TBE, a heterogeneous patient population was recruited to enrich the data set with untreated and treated achalasics; ten had no previous treatment, while ten were previously treated with Botulinum toxin, pneumatic dilation, Heller myotomy or per-oral endoscopic myotomy. HRM and TBE studies were done within 1 month of each other and the temporal variability was based on scheduling availability. All subjects gave written informed consent. The Northwestern University Institutional Review Board approved the study protocol.
Symptom Assessment
Symptoms of dysphagia, chest pain and regurgitation were assessed with the IDQ using a cumulative score as a descriptor of difficulty eating, pain with swallowing and food impaction. Ten questions with a 6-point Likert score (0–5) rating the frequency (none to daily) and severity (none to severe) of symptoms was utilized with a scoring range of 0 to 50.
High-resolution impedance-manometry
High-resolution impedance-manometry studies were conducted after a six-hour fast. The HRIM catheter was a 4.2 mm outer diameter solid-state assembly with 36 circumferential sensors spaced 1 cm apart (Given Imaging, Duluth GA, USA). The catheter also incorporated 19 metal rings spaced 2 cm apart to facilitate 18 impedance recordings. Impedance rings were located between pressure sensors such that there were two pressure sensors contained within each ring pair. The HRM assembly was calibrated at 0 and 300 mmHg using externally applied pressure and placed transnasally, positioned to record from the hypopharynx to the stomach with at least three intragastric sensors. The manometric protocol included a 2 min baseline recording and ten 5 ml swallows, 5 upright swallows and the IBH protocol of a 200 ml saline challenge followed by a 5-minute observation period (Figure 1).
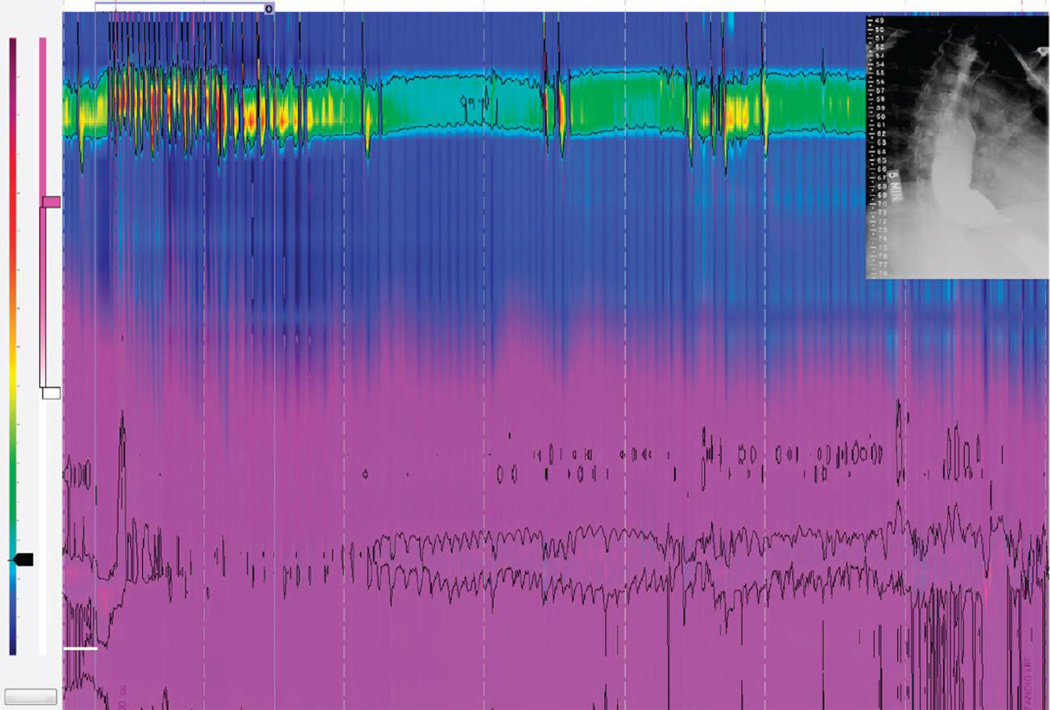
Figure 1.
Methodology and protocol for assessing Impedance Bolus Height (IBH) on HRM with impedance (HRIM) at the 5-minute time-point. The IBH protocol starts with the patient ingesting 200 ml of saline and recording for 5 minutes once the swallow challenge is complete. The height of the bolus retained after a swallow can be visualized using the impedance topography color plot highlighted by the purple color. The impedance range for the impedance topography plot is determined by the nadir impedance value that is calculated as a mean value of the first 3 swallows at the distal esophagus 3 cm above the EGJ. The impedance range is set at the nadir impedance (0.35 kOhms) plus 1000 Ohms to highlight an interface between liquid and mucosa/air. The yellow circles represent measurements of the IBH at 30 second intervals. The timed barium esophagram (TBE) image at 1 and 5 minutes are shown in the same patient to highlight the correlation between TBE and IBH.
Manometric Analysis
Manometry studies were analyzed using ManoView analysis software 3.0 (Given Imaging, Duluth GA, USA). Key pressure topography metrics analyzed were: integrated relaxation pressure (IRP), the peristaltic integrity using the 20 mmHg isobaric contour, the distal contractile integral, contractile front velocity and the distal latency9. The central metric in cases of achalasia is the IRP, which quantifies EGJ relaxation both in completeness and persistence. Additional measures of EGJ function analyzed were the mean resting EGJ pressure during expiration during the 2 minute baseline recording and the mean nadir EGJ relaxation pressure among the 10 swallows measured using the isobaric contour tool of the ManoView software.
Pressure patterns within the esophagus were characterized according to Chicago Classification metrics9. The criteria used for defining type I achalasia in untreated patients were an IRP ≥10 mmHg and 100% failed peristalsis10. Pretreatment type II achalasia was defined by an IRP ≥15 mmHg and panesophageal pressurization in ≥20% of test swallows. The presence of premature contractions with ≥20% of test swallows and no normal peristalsis was consistent with type III achalasia while swallows associated with some degree of preserved peristalsis not exhibiting premature contractions was considered an EGJ outflow obstruction11. With post-treatment patients, the same definitions were utilized with the caveat that patients were no longer categorized as having an achalasia subtype if the post-treatment IRP was <10 mmHg12. Hence, after treatment, patients were categorized as persistent achalasia pattern (Type I, II or III) or resolved achalasia pattern with a description of the current manometric profile using the Chicago Classification definitions. We emphasize that persistent or resolved achalasia patterns do not mean a resolution of the achalasia disease process.
Impedance Bolus Height analysis
The IBH was measured using two methods (Figure 2) that differed in how they calibrated the impedance signal for bolus presence and absence. The first method (Impedance Topography) utilized the average impedance nadir measured 3 cm proximal to the EGJ during the first three swallows of the 200 ml saline challenge using the impedance topography format. This nadir impedance value was then used as the lower limit for liquid presence in the color scale. The upper limit for liquid presence was then arbitrarily set at the nadir impedance plus 1000 Ohms, visually evident by loss of the purple color. The 1000 Ohm value was chosen because it clearly distinguished liquid from mucosa or air. The height of the impedance bolus was then measured with the smart mouse tool from the proximal aspect of the EGJ high-pressure zone to the top of the purple topographic signal. The second method (Spatial Impedance Variation Plot) for measuring IBH also utilized an average impedance nadir measured 3 cm proximal to the EGJ during the first three swallows of the 200 ml saline challenge. However, the average nadir impedance was utilized as a threshold for liquid using a spatial impedance variation plot that displayed impedance change along the luminal axis. This is analogous to assessing bolus presence on conventional impedance tracings using a 50% change in impedance value as the indication of liquid clearance. Both methods of IBH measurement were performed at 1 and 5 minutes during expiration.
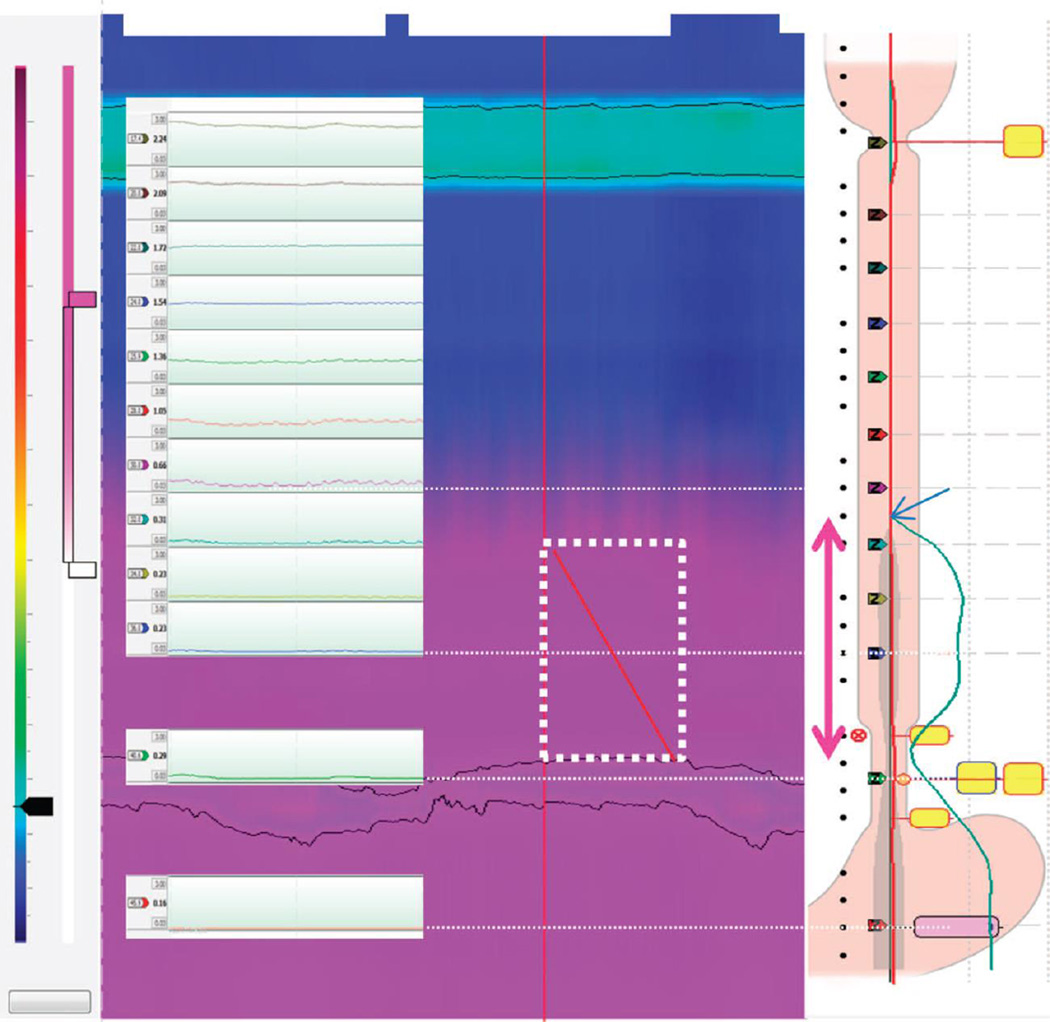
Figure 2.
Techniques utilized for measuring Impedance Bolus Height (IBH). The HRIM catheter is oriented to have impedance recording sites spaced 2 cm apart and positioned through the EGJ and UES. The impedance tracing format is overlaid on top of the HRIM topography plot to illustrate the 2 cm incremental changes in impedance data through the body of the esophagus. The two HRIM impedance techniques utilized to measure the IBH utilize the nadir impedance to highlight the interface using the impedance color topography contour plot (Method 1) and the spatial impedance variation plot (Method 2). The impedance topography method (middle) utilizes a smart mouse tool to measure the distance from the proximal aspect of the EGJ to the top of the topographic color change during end-expiration (white dashed box). In this example, the measurement is 9.0 cm. The spatial impedance variation plot is shown on the right and presents the instantaneous impedance change along the axial length of the esophagus (green line). Interpolation is utilized to smooth out the curve and the range for the impedance measure is set at the nadir impedance to delineate the inflection point where the liquid interface occurs. The IBH is measured by determining the location along the catheter where the nadir impedance inflection occurs to signify the top of the bolus. The height is measured using the catheter sensors as a measurement reference and in this case the height is 9.0 cm.
The IBH measurement was also used to quantify the rate of esophageal emptying. A unique metric was devised by plotting the impedance bolus height over time at 30-s intervals and calculating the area above the proximal aspect of the EGJ consistent with liquid presence (impedance bolus area (IBA). We also calculated the time to half IBH reduction to distinguish subjects with slow emptying from those who have bolus retention with no evidence of emptying.
Timed barium esophagram
Timed barium esophagrams were performed in the upright position to obtain frontal spot films of the esophagus at baseline, 1 minute, and 5 minutes after ingestion of 200 ml (sometimes limited by patient tolerance) of low-density (45% weight to volume) barium sulphate. The height of the barium column, measured vertically from the axial position of the EGJ, was made using a standard reference scale placed directly on patient and rounded up to whole centimeters. The maximal esophageal diameter was measured along the esophageal body perpendicular to the axial plane of the esophagus. All measurements were made by a blinded investigator (JEP) and confirmed by the official radiology report.
Statistical analysis
Data from the HRIM assessment were analyzed separately (no knowledge of TBE results) by two reviewers in a blinded fashion to assess the inter-observer reproducibility. The mean value of the two reviewers for the HRIM measurement of impedance bolus height was utilized for the comparison with TBE. All continuous variables were expressed as median (25th – 75th percentile). Two sample comparisons utilized the Mann Whitney test with significance set at p<0.05 for both. Categorical variables were compared using the Chi Square test. Correlation between the various pressure topography and TBE metrics was calculated using Pearson correlation. The agreement between the HRIM measure of IBH and TBE was assessed by two sample comparisons. The data for IBH and TBE height was presented as whole centimeters based on the fact that the heights measured were completed as whole centimeters.
RESULTS
The study population consisted of 10 untreated patients (age range 33–79 years; 8 male) and 10 post-treatment patients (age range 21–67; 3 male). The demographic, symptoms scores and baseline manometric features of the untreated and treated patients are presented in Table 1. The treatments rendered were pneumatic dilation (n=2), laparoscopic Heller myotomy (n=3), and per-oral endoscopic myotomy (n=5). There was a significant difference in the median IRP, expiratory EGJ pressure and sex distribution between the untreated and treated patients (Table 1).
Table 1.
| Untreated (n=10) | Treated (n=10) | P value | |
|---|---|---|---|
| Ages | 50 (35–76) | 56 (32–60) | P=0.67 |
| Sex | 8 male / 2 female | 3 male/ 7 female | P< 0.05 |
| Subtype* | type I-2, type II-4, type III-4 | absent peristalsis-3, DES-2, type I-5 | |
| IRP | 30.0 (17.0–40.1) | 10.9 (4.5–12.7) | P<0.01 |
| Expiratory EGJ Pressure | 21.0 (10.0–38.8) | 5.5 (2–14) | P=0.02 |
| IDQ | 18 (11–29) | 14.0 (5–25) | P=0.34 |
Subtype comparisons between untreated and treated patients was not performed due to the obvious changes that occur after the EGJ is disrupted.
DES distal esophageal spasm]
Impedance Bolus Height
The median nadir impedance value utilized for both methods to assess IBH was 0.27 kOhms (IQR, 0.19 – 0.45). There was excellent correlation of this measurement with a second blinded investigator (0.91) and the median disagreement was 0.0 kOhms (IQR, −0.03 to 0.05 kOhms). Similarly, applying this value to the calculation of IBH using the impedance topography method, there was an excellent correlation between the two reviewers at 1 minute (r=0.97) and 5 minutes (r=0.99). The median disagreement between the two reviewers was minimal (1 minute, 1.0 cm (range, 0–3.0 cm); 5 minutes, 0 cm, 0–2.0 cm). The calculation of IBH using the spatial impedance variation plot technique also found an excellent correlation at 1 minute (r=0.99) and 5 minutes (r= 0.99). The median inter-observer disagreement with this method was also minimal (1 minute, 1.0 cm (range, 0–1.0 cm); 5 minutes, 1.0 cm, 0–1.0 cm). The correlation between the impedance topography method (method 1) and the spatial impedance variation plot approach (method 2) for measuring IBH was excellent at both the 1 minute (R=0.99) and the 5 minute (R=0.99) time point. The range of discrepancy at 1 minute was 0 to 2.0 cm and at 5 minutes was 0 to 2.0 cm.
Agreement between Impedance Bolus Height and TBE
There was no significant difference between the median IBH and barium column height at 1 minute [IBH 12.0 cm (IQR, 8.0–18.0), TBE 12.0 cm (IQR, 7.0–19.0), P=0.90] or 5 minutes [IBH 11.0 cm (IQR, 1.0–17.0), TBE 9.0 cm (IQR, 4.0–12.0), P=0.47]. The correlation between the IBH and barium column at 1 minute was moderate with an R value of 0.60. However, the correlation between the IBH and the barium column at 5 minutes was excellent with an R value of 0.86.
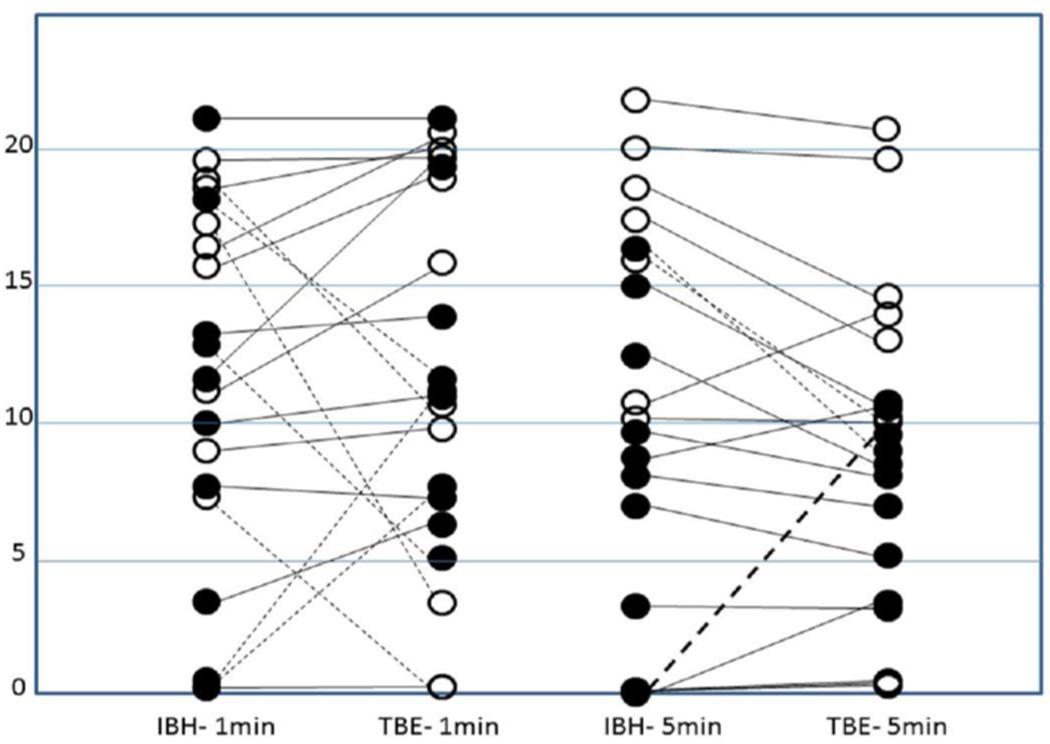
The variability between IBH and barium column height at 1 and 5 minutes is illustrated in Figure 3. At 1 minute, there were 7 values that differed by greater than 5 cm between the two measures and 5 of these would have resulted in non-concordant data for bolus retention using a 5 cm cutoff. At 5 minutes, only 3 measures differed by more than 5 cm and there was 95% concordance using 5 cm as a cutoff value for bolus retention.
Figure 3.
Comparison of the IBH and the barium column height during the 1 and 5 minute measurement time-point. The open circles represent untreated patients and the filled circles are treated patients. There was more disagreement between the two techniques at 1 minute compared to 5 minutes. The dashed lines indicate patients whose measures differed by more than 5 cm. There were 7 such instances for 1-minute values and 3 at 5 minutes. There was only one subject with a discordant value at 5 minutes that would have represented a good outcome on IBH and a poor outcome on TBE (bold dashed line). This patient had severe esophagitis (Los Angeles C) and a very good effect from his myotomy with an IRP of 5 mmHg and an EGJ expiratory pressure of 2 mmHg suggesting that the bolus retention on the 5 minute TBE may have been reflux related.
Correlation between Impedance Bolus Height and outcome measures
The correlation between IBH at 5 minutes and IDQ score was fair to moderate with an R value of 0.49. The correlation between IBH at 5 minutes and measures of EGJ function on HRM was fair (IBH-IRP, R=0.39; IBH-EGJ expiratory pressure, R=0.40). The correlation between IDQ score and barium column at 5 minutes was fair with an R value of 0.35. The correlation between barium column height at 5 minutes and IRP was also fair (r=0.36), however, the correlation between barium column at 5 minutes and EGJ basal pressure was weak (R=0.15).
Impedance topography as a surrogate for bolus emptying
Assessing impedance bolus height as a function of time provided an estimate of bolus emptying rate. Of the 20 patients, 8 achieved a half reduction in IBH during the 5 minutes and the median IDQ scores for these patients showed a trend toward a lower IDQ score compared to those who did not achieve a half reduction in IBH (t-1/2 less than 5 minutes, IDQ = 9 (IQR, 2.8–15.5; t-1/2 greater than 5 minutes, IDQ 21 (IQR, 13.8–27.8); p=0.08). The correlation of t-1/2 IBH and IDQ was fair with an R value of 0.40. However, this was likely limited by the fact that the study was conducted for only 5 minutes.
The IBA after the 200 ml saline challenge was also assessed to determine the dynamics of bolus retention. The median value for the IBA was 3264 cm-s (IQR, 1680–5100 cm-s). There was a fair to moderate correlation between IBA and IDQ with an R value of 0.48.
DISCUSSION
The aim of this study was to assess whether new metrics devised for HRIM could be utilized to assess bolus retention comparable to barium retention on TBE. The major finding was that IBH at 5 minutes had good agreement with barium column height measured at 5 minutes using fluoroscopy during a standard TBE protocol. Additionally, IBH was significantly correlated with both symptoms and other manometric predictors of successful treatment outcome within a range that was similar to TBE. Hence, IBH obtained during a standard HRIM protocol can be utilized to simultaneously assess bolus retention and manometric parameters in achalasia.
Although this is not the first study to evaluate impedance or high volume swallows in achalasia, it is the first to combine the two techniques into a standardized measurement tool that provides important functional and clinical outcome data. Previously, Tutuian and colleagues reported that abnormal bolus transit was found uniformly in achalasia13. Similarly, that same group of investigators reported that low baseline impedance was associated with chronic fluid retention and elevated intra-esophageal pressure8. Conchillo et al utilized simultaneous impedance and fluoroscopy to assess concordance of barium clearance time and impedance depiction of height and showed a modest correlation at 10 minutes with an r value of 0.65. Paralleling this in time, HRM was becoming increasingly widespread in clinical application. Using HRM, Fox et al reported on the utility of using free water swallows at the end of the standard protocol to assess bolus stasis and esophageal pressurization in achalasia14. Thus, it was a natural progression that HRM would be combined with impedance to assess esophageal function in achalasia as investigators began looking into the mechanism of esophageal emptying in type II achalasia15, 16.
We sought to combine the novel observations found using impedance and manometry by previous investigators into a combined objective measurement that would complement both techniques. Given the previous work by Vaezi et al demonstrating that bolus retention on TBE was an important clinical outcome measure2, 3, it was logical to attempt to simulate a clinical TBE protocol using HRIM. Thus, we developed new measurement tools focused on impedance bolus height after a 200-ml saline challenge (IBH). We found good agreement between the two techniques despite differences in density between the saline and barium bolus and also determined that IBH can be performed easily with good reproducibility. The 5-minute measurement point was more concordant between IBH and TBE suggesting that the 5-minute time point is much more stable and that emptying may be more variable during the initial few minutes after the swallow. Additionally, we found that the prolonged monitoring of the IBH could be leveraged to assess the rate of esophageal emptying similar to a gastric empty study by determining the time at which the impedance column would be reduced to half of the initial height.
There has been a longstanding debate regarding the optimal test to evaluate treatment outcomes in achalasia. Both TBE and HRM are extremely helpful and complementary in terms of the information that they provide; however, both tools have limitations. Barium esophagram requires radiation exposure and does not provide quantitative information regarding the contractile activity within the esophagus. Manometry may be difficult to perform in a dilated esophagus and data on bolus retention is difficult to ascertain. HRIM circumvents some of these limitations and provides a more global assessment of esophageal function that could be utilized as a single test. This technique provides the important manometric data utilized to assess treatment effect during the standard protocol and this is complemented by data on bolus retention following the 200-ml saline challenge. Our previous findings suggest that resolution of the achalasia pattern on pressure topography was an important predictor of treatment outcome and that this was complementary to TBE and standard HRM variables12, 17. Additionally, an evaluation of contractile activity during the 200-ml bolus challenge provides additional information regarding mechanisms of emptying and potential reflux as the cause of ongoing symptoms. In our dataset, there were two instances in which the IBH changed due to reflux events during the 5-minute protocol and these two patients were noted to have esophagitis on endoscopy.
There are certain limitations to using impedance in achalasia and these were highlighted by Conchillo et al7. The precise location of the liquid column can be difficult to ascertain on impedance as there is air trapping and pooling of saliva in the esophagus. However, the nadir impedance method improved confidence that liquid was present and resulted in very good correlation with the TBE height at 5 minutes. Additionally, the accuracy of the impedance component is limited by the 2-cm electrode spacing thereby limiting the resolution of the measurement. However, the relevance of a 1 to 2 cm difference on a TBE study is unlikely to be clinically important.
In conclusion, our findings suggest that HRM with impedance using a 200-ml saline challenge can be leveraged to provide a global assessment of esophageal function in achalasia before and after treatment. This tool can be utilized to assess most of the clinically important parameters associated with achalasia outcome: 1) EGJ relaxation pressure, 2) expiratory EGJ pressure, 3) intraesophageal pressure, 4) contractile pattern, 5) achalasia subtype and 6) bolus retention at 5 minutes. Although assessment of dilatation and sigmoid deformity by TBE are important in clinical decisions, this information is typically most crucial during the initial evaluation and can be largely obtained during endoscopy. Future studies focused on determining whether applying this HRIM protocol is more effective than obtaining a single TBE or HRM are warranted to provide further evidence of which strategy is most effective.
Current Knowledge.
Manometry is the gold standard for diagnosing achalasia.
Barium esophagram is an important tool in the evaluation and management of achalasia.
Obtaining bolus retention data using a timed barium esophagram protocol is helpful in assessing treatment outcome and requirement for further intervention
What is new here
A novel technique for assessing impedance bolus height has been developed to standardize assessment of bolus retention by combining high-resolution manometry and impedance.
Impedance bolus height has an excellent correlation with barium column height on timed barium esophagram when using a 200-ml protocol at 5 minutes.
Impedance bolus height has an equivalent correlation with symptoms and manometric variables when compared to barium column height on timed barium esophagram.
Acknowledgements
This work was supported by R01 DK079902 (JEP) and R01 DK56033 (PJK) from the Public Health Service
Abbreviations
- HRM
high resolution manometry
- TBE
timed barium esophagram
- EGJ
esophagogastric junction
- IRP
integrated relaxation pressure
- IBH
impedance bolus height
- IDQ
Impaction Dysphagia Score
Footnotes
Author contributions
John Pandolfino obtained funding, contributed to the conception and study design, study supervision, data collection, analysis and interpretation, statistical analysis, manuscript drafting, editing, critical revision and final approval.
Frederic Nicodeme contributed to data analysis and interpretation, and manuscript final approval.
Yu K. Cho contributed to the conception of the study design, performed analysis and interpretation, critical revision and final approval.
Anna Lipowska contributed to data collection and analysis, and final approval.
Elyse R. Johnston contributed to data collection and analysis, and final approval.
Andrew Gawron contributed to data collection and analysis, and final approval.
Ezra N. Teitelbaum contributed to data collection and analysis, and final approval.
Eric S. Hungness contributed to the conception and study design, data interpretation, critical revision and final approval.
Peter J. Kahrilas contributed to the conception and study design, obtained funding, data interpretation, editing, critical revision and final approval.
References
- 1.Pandolfino JE, Kahrilas PJ. AGA technical review on the clinical use of esophageal manometry. Gastroenterology. 2005;128:209–224. doi: 10.1053/j.gastro.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Vaezi MF, Baker ME, Richter JE. Assessment of esophageal emptying post-pneumatic dilation: use of the timed barium esophagram. Am J Gastroenterol. 1999;94:1802–1807. doi: 10.1111/j.1572-0241.1999.01209.x. [DOI] [PubMed] [Google Scholar]
- 3.Vaezi MF, Baker ME, Achkar E, et al. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50:765–770. doi: 10.1136/gut.50.6.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–1738. doi: 10.1016/0016-5085(92)91428-7. [DOI] [PubMed] [Google Scholar]
- 5.Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011;8:311–319. doi: 10.1038/nrgastro.2011.68. [DOI] [PubMed] [Google Scholar]
- 6.Nicodeme F, Pandolfino JE. Esophageal Disorders Not Yet Addressed by High-resolution Manometry. J Neurogastroenterol Motil. 2013;19:114–115. doi: 10.5056/jnm.2013.19.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conchillo JM, Selimah M, Bredenoord AJ, et al. Assessment of oesophageal emptying in achalasia patients by intraluminal impedance monitoring. Neurogastroenterol Motil. 2006;18:971–977. doi: 10.1111/j.1365-2982.2006.00814.x. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal A, Hila A, Tutuian R, et al. Manometry and impedance characteristics of achalasia. Facts and myths. J Clin Gastroenterol. 2008;42:266–270. doi: 10.1097/01.mcg.0000248013.78020.b4. [DOI] [PubMed] [Google Scholar]
- 9.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin Z, Kahrilas PJ, Roman S, et al. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–e363. doi: 10.1111/j.1365-2982.2012.01952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandolfino JE. Uncovering hidden information in achalasia using esophageal pressure topography. Gastroenterology. 2013;144:681–684. doi: 10.1053/j.gastro.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 12.Roman S, Kahrilas PJ, Mion F, et al. Partial recovery of peristalsis after myotomy for achalasia: more the rule than the exception. JAMA Surg. 2013;148:157–164. doi: 10.1001/2013.jamasurg.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tutuian R, Castell DO. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am J Gastroenterol. 2004;99:1011–1019. doi: 10.1111/j.1572-0241.2004.30035.x. [DOI] [PubMed] [Google Scholar]
- 14.Fox M. Multiple rapid swallowing in idiopathic achalasia: from conventional to high resolution manometry. Neurogastroenterol Motil. 2007;19:780–781. doi: 10.1111/j.1365-2982.2007.00980.x. author reply 782. [DOI] [PubMed] [Google Scholar]
- 15.Tutuian R, Pohl D, Castell DO, et al. Clearance mechanisms of the aperistaltic oesophagus: the "pump gun" hypothesis. Gut. 2006;55:584–585. doi: 10.1136/gut.2005.085423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong SJ, Bhargava V, Jiang Y, et al. A unique esophageal motor pattern that involves longitudinal muscles is responsible for emptying in achalasia esophagus. Gastroenterology. 2010;139:102–111. doi: 10.1053/j.gastro.2010.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicodeme F, de Ruigh A, Xiao Y, et al. A comparison of symptom severity and bolus retention with Chicago classification esophageal pressure topography metrics in patients with achalasia. Clin Gastroenterol Hepatol. 2013;11:131–137. doi: 10.1016/j.cgh.2012.10.015. quiz e15. [DOI] [PMC free article] [PubMed] [Google Scholar]